Physio Exam IV
1/281
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
282 Terms
what are the layers of the heart from inside out?
endocardium
myocardium
visceral pericardium
paricardial cavity
parietal pericardium
What is Beck’s Triad? what is diagnosis?
becks triad: low BP, distension of jugular veins, muffled heart sounds
acute cardial tamponade → build-up of fluid, blood, or air in pericardial sac that compresses the heart
what is the order of vessels in the heart?
arteries, arterioles, capillaries, venules, veins
where is the site of greatest vascular resistance?
arterioles
Which vessels use high pressure system and have elastic walls to maintain BP?
arteries
which vessels use a low pressure system and is affected more by gravity?
Veins
what does capacitance vessels refer to?
the systemic veins that contain the largest volume of blood
which vessels use:
1) skeletal muscle as a pump
2) changes in intrathoracic pressure due to breathing as a pump
veins
what are central venous sinuses?
aka dural sinuses
these sinuses have rigid walls and do not collapse
in the brain
what are the bends?
decompression sickness
caused by increased pressure pushing nitrogen gas into the blood
what is the driving force of blood pressure?
the difference in pressure between the aorta and the large central veins
Flow = what?
Ohm’s Law (pressure)
Flow = difference in pressure between 2 points/Resistance
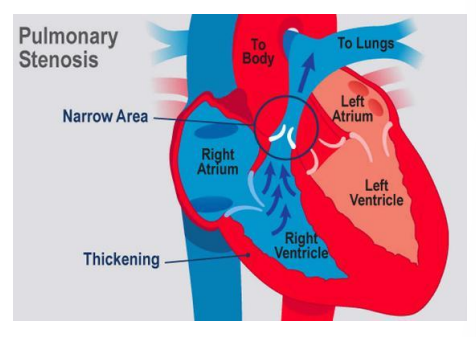
Stenosis = increased ________ = _________ flow
resistance
decreased
what is pulmonary hypertension?
excessive pressure in the pulmonary arteries
this can result in right-sided heart failure
results in fluid backing up into the legs, veins in the neck, liver, and so on.
what causes resistance to go up?
increased length
increased viscosity
decreased radius
The longer the straw → the ______ it takes to drink
The thicker the fluid → the _______ it takes to drink
the larger the diameter of the straw → the _______ it takes to drink
longer
longer
faster
why do capillaries have low resistance?
when in parallel, resistance decreases
bc there is a network of capillaries, the resistance is very low
T/F low compliance = stiff
True
what is the equation for compliance?
change in volume/change in pressure = compliance
lymph have ____-____ capillaries
blind-ended
what percent of the total circulating protein is returned via lymph?
25-50%
what lymphatic duct drains the right side of the head, right arm, and right side of chest? what drains everything else?
right lymphatic duct
thoracic duct
what controls capillaries?
recapillary sphincters
how are proteins taken up in cappilaries?
through endocytosis
T/F gasses and lipid-soluble substances readily diffuse
true
T/F formed elements in the blood do not diffuse
True
what is the MOST important mechanism for exchange in the capillaries ?
diffusion
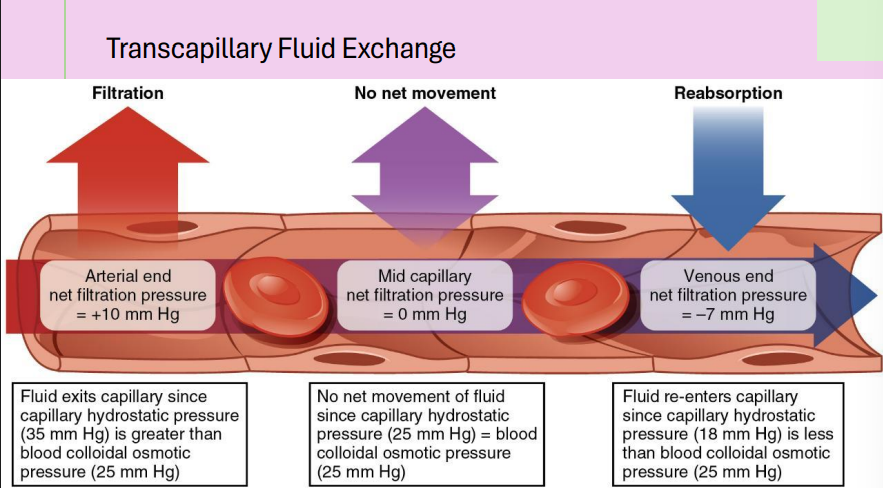
explain the transcapillary fluid exchange
when hydrostatic pressure is greater than blood colloidal osmotic pressure, there is filtration because fluids exit the capillaries.
when hydrostatic pressure=blood colloidal osmotic pressure, there is no net movement
when the hydrostatic pressure is less than blood colloidal osmotic pressure, reabsorption takes place
what is the equation for net fluid flux in capillaries?
Net fluid flux= (capillary hydrostatic pressure - interstitial hydrostatic pressure) - (capillary oncontic pressure - interstitial oncotic pressure)
what are some reasons for edema?
can be due to increased venous pressure due to a clot
can be due to lack of oncotic pressure
inflammation/sepsis
or lymphatic obstruction
what is cardiac muscle like?
innvoluntary
striated
have intercalated discs with gap junctions
electrical stimulation of heart muscles uses what ion?
Ca2+
define contractility
the ability of a muscle to contract in response to stimuli
force of contraction is dependent on regulation of calcium
What is the SA node?
collection of specialized myocytes that spontaneously depolarize to generate action potentials
what is the only electrical communication between the atria and the ventricles?
AV node
what are the branches of the Bundle of His?
right bundle branch
left bundle branch
divides into two fascicles:
anterior fascicle
posterior fascicle
right vagus input goes directly into which node of the heart? left vagus?
right: SA node
left: AV
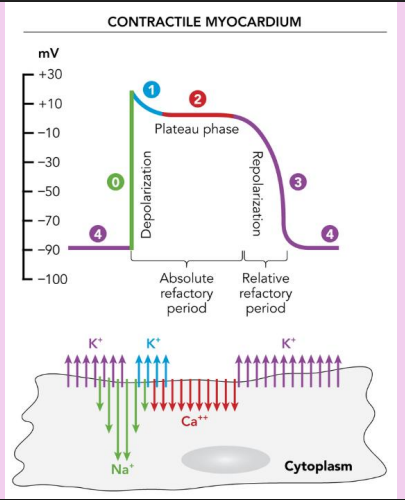
when the heart is going through contraction, what is happening in each phase?
phase 0: deopolarization, channels rapid upstroke immediately after stimulation, Na+ quickly exits the cell into cytoplasm
phase 1: partial repolarization, K+ is entering the heart
phase 2: plateue phase, dramatic slowing of repolarization, Ca 2+ is exiting ot cytoplasm
phase 3: repolarization back to -90mV, relative refractory period, K+ re-enters the cell
phase 4: reaches resting membrane potential
why do Nodal cells spontaneously generate action potentials during phase 4 of contraction?
their maximum membrane potential difference is -60 mV and their phase 0 triggers about -40 mV
what do the class I-class IV antiarrhythmics block?
class I: sodium channel blockers
class II: beta blockers
class III: potassium channel blockers
class IV: calcium channel blockers
why do calcium channel blockers work for arrhythmias?
help heart relax and keeps calcium out which decreases contractility and increases compliance. this also lowers blood pressure
why are refractory periods important?
they protect against rapid atrial arrythmias
what is a positive chronotropic effect?
increases heart rate
uses norepi and beta adrenergic receptors
sympathetic innervation
what is a negative chronotropic effect?
slows heart rate
parasympathetic innervation
ACh acts on muscarinic receptors
what are signs of sympathetic nervous stress?
tachycardia
pale, cool skin
sweating
dilated pupils
what are intrinsic causes of sympathetic nervous stress?
pain, fear, anxiety, and hypotension
pts experiences MI’s and abdominal aortic aneurysms have these symptoms
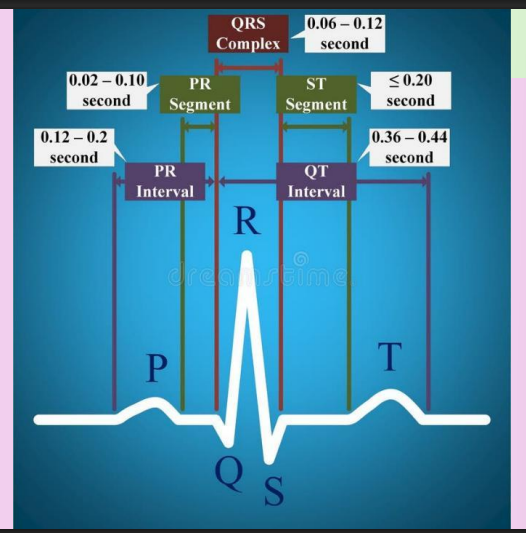
what is occurring during the different phases of the EKG?
P wave: atrial depolarization - atria contract
PR segment: AV node gets input from SA node
QRS: ventricular depolarization begins and atrial repolarization occurs - ventricles contract
ST segment: ventricular depolarization is complete
T wave: ventricular repolarization begins - ventricles relax
what is a normal heart rate?
60-100 bpm
what is a normal heart axis?
between -30 to 110 degrees
what can cause right axis deviation?
right ventricular hypertrophy
what causes left axis deviation?
indicate heart is bein pushed up → pregnancy, hypertrophy, or obesity
what will Lead 1 and Lead aVF tell you about the axis?
if both are positive, it indicates a normal axis
if both are negative it is an extreme axis
if one is positive and one is negative it is a left or right axis deviation
on an EKG paper, 5mm is how long?
0.2 seconds
how many squares in an EKG in normal for P wave? (atrial depolarization)
3 small squares
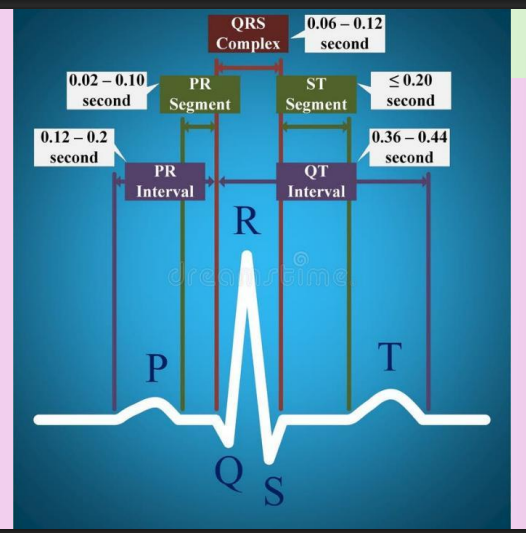
how many squares is normal for a PR interval in an EKG?
3-5 small squares
if PR interval is greater than 200 ms (greater than 5 squares) then it is a 1st-degree heart block
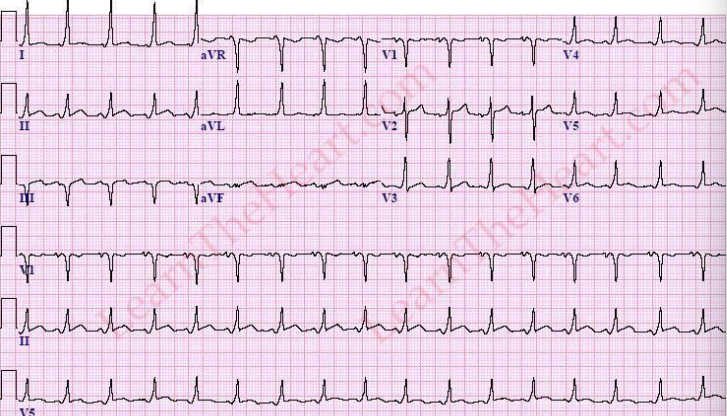
what causes a delta wave/slurring upstroke in an EKG?
when there is a bundle of Kent that conducts more quickly than the AV node which excites one ventricle early
short PR interval and longer QES with slurred upstroke
what is a normal QRS width?
70-100 ms → electrical impulse came from atria
if it is longer, the electrical impulse came from the ventricles
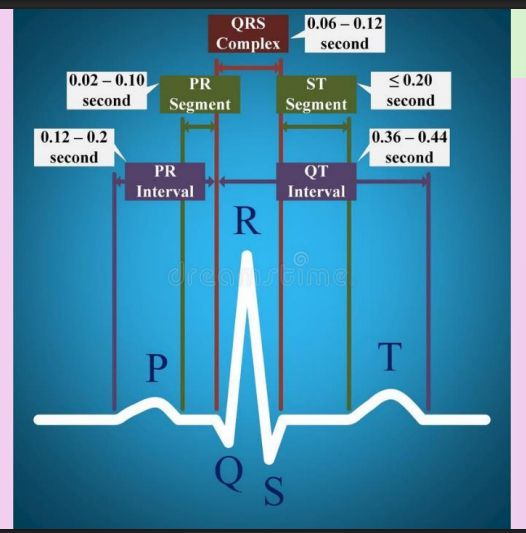
what is a normal QT interval?
360-440 ms
increases in slower HRs and decreases in faster HRs
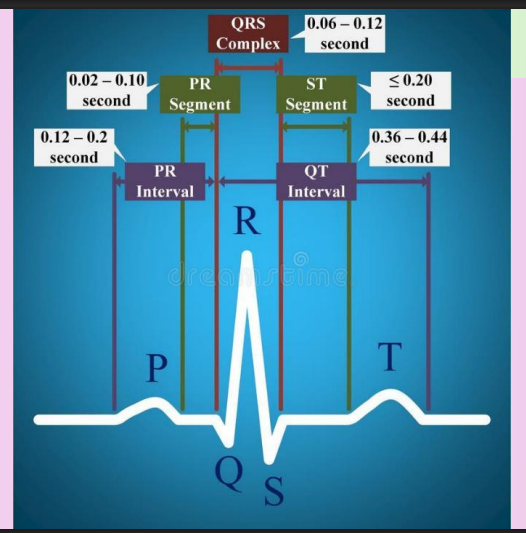
ST segment (Ventricule Completed Depolarizing)
what does an elevated or depressed ST segment indicate?
Elevated: concerning for MI
depressed: concerning for ischemia
flat is normal
T wave (ventricular repolarization
is an inverted T wave normal?
it can be, but if it is persistently inverted it can be an indication of a prior MI
what is the U wave?
it is a rare wave after the T wave. it is small and can sometimes be seen in electrolyte abnormalities and medication overdoses
what are the 4 types of heart block?
1st degree: PR interval is greater than 0.2ms
2nd degree (Mobitz I): progressive PR + dropped beat
2nd degree (Mobitz II): Fixed PR interval + Dropped beat
3rd degree: No relation between P waves + QRS
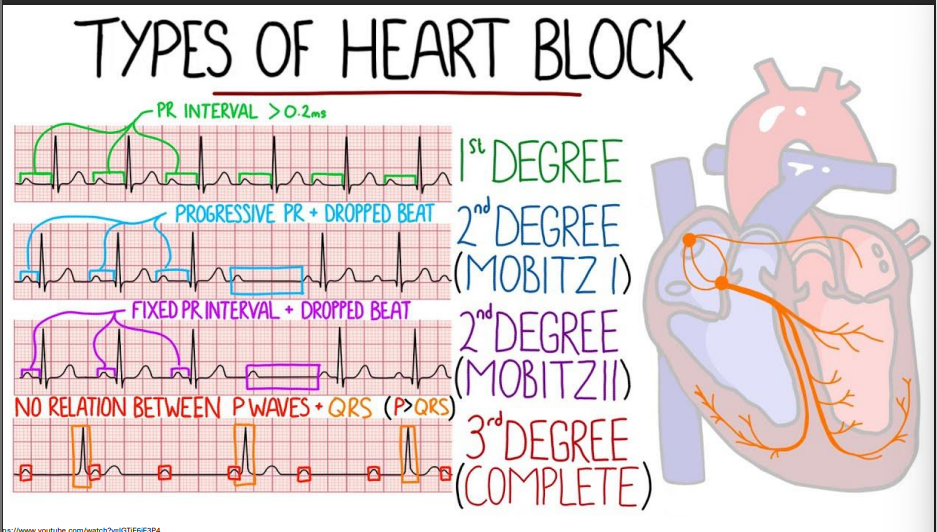
in a first degree block, what is happening with conduction?
delayed conduction in the atria
what is happening with conduction in a 2nd degree heart block?
fatigue with resultant filure or intermittent failure of the bundle of His/Purkinje fibers
what is happening with conduction in a 3rd degree heart block?
complete failure of the His/Purkinje fibers
list out the diastoles and systoles in the cardiac cycle
ventricular diastole: AV valves open and ventricles fill passively (70%) of filling is passive
atrial systole: Atrial kick, a small amount of extra blood is pumped into the ventricles
isovolumic ventricular contraction: volume remains the same, but the contraction of the ventricle closes the AV valves and increases the pressure
ventricular ejection: semilunar valves open as the ventricular pressure exceeds the aorta/pulmonary artery’s pressure and blood is pumped into these vessels
isovolumic relaxation: volume remains the same, semilunar valves close as ventricular pressure decreases. The atria fill passively with blood.
at what point do the atrioventricular valves open?
when the atrial pressure exceeds the ventricular pressure
A _______ is a pressure wave that expands the arterial walls
pulse
what causes the dicrotic notch?
when the aortic valve closes - it is a quick dip in aortic pressure
what is Chordae tendineae’s job?
anchor the AV valves to the papillary muscles
when ventricles contract, the muscle pulls on the papillary muscles and the chordae tendineae to close the AV valves.
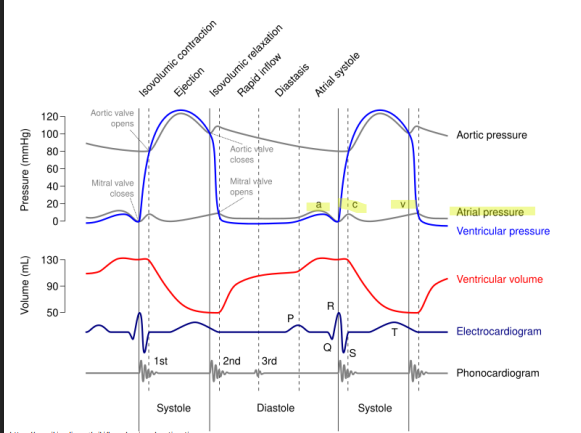
Explain the a, c, and v waves in the atrial pressure line of Wiggers diagram
a wave : atrial systole
c wave: bulge of the mitral valve into the atria - increasing the pressure
v wave: passive atrial filling
In a 3rd degree heart block why can the jugular vein look distended?
the atria can be going through systole at the same time as the ventricles → pumps against a closed AV valve causing a back flow of blood up into the jugular veins
in the phonocardiogram portion of the diagram, what does the 1, 2 and 3 refer to? (S1, S2, S3)
S1: closing of the AV valves
S2: closing of the SL valves
S3: rapid ventricular filling
T/F turbulent flow is more likely with increased velocity
True
Laminar flow is what?
normal and smooth flow
it is related to the diameter of the vessel, and to the viscosity of hte blood
what is Reynold’s number?
a number used to compare laminar and turbulent flow
when taking blood pressure, you are forcing what kind of flow?
turbulent flow → causes korotkoff sounds when compressing brachial artery and slowly releasing it
what is trasnmural pressure? what is the equation?
the pressure gradient across the wall of a membrane
determines if vessel expands or collapses
Transmural Pressure = internal pressure - external pressure
for example, a decrease in external pressure would allow increased internal pressure and increased blood flow (if transmural pressure is constant)
Blood flow creates a force on the endothelium called what?
sheer stress
this stimulates cilia on endothelial cells
Law of Laplace
Tension ________ with the size of the vessel thickness
increase in radius (aka thickness) of a cylinder = _________ tension
Tension decreases with the size of the vessel → why capillaries don’t collapse
increase in radius of a cylinder = increased tension
what is bernoulli’s equation? how does it relate to blood vessels?
in a tube, total energy is constant
this means that if a vessel is scarred, causing increased velocity, there is a corresponding decreased pressure so vessel maintains itself and isn’t ruptured.
what are some reasons for murmurs?
due to stenosis of valves
or regurgitation
or increased flow such as pregnancy and anemia
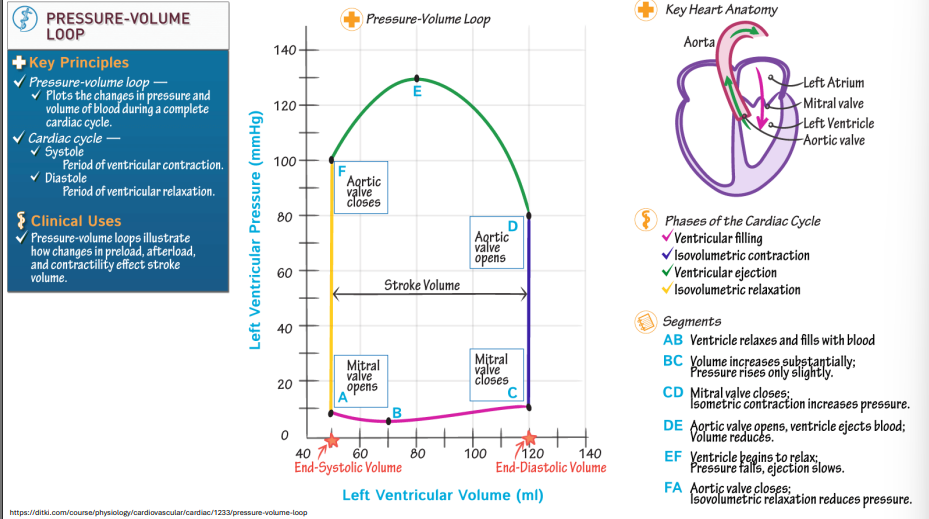
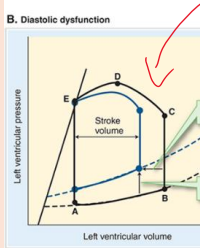
draw out and understand the pressure-volume loop
Point A = end systolic volume mitral valve opens
Point B = passively filling volume
Point C = mitral valve closes
Point D = aortic valve opens
Point F = valve closes because pressure is too much
Cardiac output is what?
the volume of blood (L) pumped by each ventricle per minute
why is low Cardiac output concerning?
inadequate tissue perfusion → shock!
Cardiac output equation
CO = (SV x HR)/1000
CO= cardiac output
SV= stroke volume
HR= heart rate
if cardiac rate is controlled by ANS, what controls stroke volume?
partially ANS control
ionotropic?
increase force of contraction
increasing preload OR decreasing afterload does what do stroke volume?
increases it
what is the Ejection fraction?
the percentage of blood pumped out of each ventricle in one beat
EF= SV/EDV x 100%
what range is ejection fraction (EF) normal? when is it heart failure?
normal EF: 55-70%
heart failure: <40%
how does loss of contractility impact ejection fraction?
it decreases it
how does left sided heart failure present?
restlessness
confusion
tachycardia
cyanosis
pulmonary congestion
exertional dyspnea
how does right sided heart failure present?
fatigue
increased peripheral venous pressure
ascites
enlarged liver and spleen
edema
distended jugular veins
what is cardiac index?
cardiac index= cardiac output/body surface area
normal is 2.5-4 L/min/m2 at rest
what is Frank-Starling’s principle? (the relationship between left ventricle EDV and SV). What would he say are the main factors affecting stroke volume?
increased diastolic filling=increased SV
preload, force of contraction, afterload
what increases preload?
increasing blood volume
rhythmic skeletal muscle contraction
deep inspiration
atrial systole
venoconstriction
what increases afterload?
increased resistance to blood flow
decreased compliance of an SL valve or the great vessels themselves
what does a left-ward shift in the Frank-starling curve indicate?
greater contractility
what does an upward shift in the loop indicate?
decreased compliance