Renal Function: Acid Base Regulation
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
What three main systems does the body use to achieve acid base balance?
1) Intra- and extra-cellular buffers - RAPID
2) Lungs/respiratory system (volatile acids)
3) Kidneys (SLOW - relatively speaking)
Only system for removal of non-volatile acids formed during metabolism
How do we regulate acid / base production in the kidney?
production/reabsorption of HCO3- (Combatting acidosis)
excretion of H+ (Combatting acidosis)
excretion of HCO3- (Combatting alkalosis)
What is the typical urinary pH?
4.5 - 8.5
Where is the majority of tubular HCO3- reabsorbed?
Where else is it absorbed?
In the PCT
Restores HCO3 to plasma, NO net change in H+ (cycles between tubular lumen and cell) Tm/saturable, excess excreted
TAL reabsorbs ~15% of filtered using a similar mechanism
In conditions of acidosis, the body might need to produce more HCO3-, how is this done?
Where plasma HCO3- is low…
Production of HCO3-, by tubular walls in the DCT and CD
Intercalated cells of CD
Can secrete HCO3- into the capillaries and absorb Cl- into the tubular cells
H+ also actively pumped into filtrate to be excreted
K+ / H+ ATPase pump also actively pumps H+ into filtrate
Both serve to decrease pH, net gain of HCO3
The active transport of H+ at the level of the collecting duct can increase luminal H+ by how much?
900 fold
Renal Net Acid Excretion (NAE)
Under acidic conditions H+ is excreted into the filtrate, however H+ is low because most is buffered. What is the predominant buffer and what happens when the body needs to reabsorb this specific compound?
Predominant buffer in the filtrate is HCO3-, but as most HCO3-, is reabsorbed........
Two additional tubular buffers…
Titratable Acids:
Phosphate
(НРО42- - H2РО4-) (dietary source, tubular concentration determined by filtration / reabsorption)
Limited amount of phosphate in tubular fluid
Ammonia (NH3 → NH4+ (Ammonium)) - regulated production in kidney allows for control of H+
What are titratable acids?
Filtered solutes, in base form, that therefore can bind protons
Excreted titratable acids are formed from secreted protons.
Where are these hydrogen ions mainly secreted?
What transporters allow them to be secreted?
PCT
Via the Na+ / H+ exchanger (Secondary Active Transport)
H+ ATPase (Active transport of intracellular H+ across apical membrane) (Small Amount)
TAL
Via the Na+ / H+ exchanger
CD
H+ ATPase (Active transport of intracellular H+ across apical membrane)
K+ / H+ ATPase pump
Once H+ is inside the tubular filtrate, it can cause weak bases such as phosphate to form…
Why is this done and what does it prevent?
H+ in the tubule fluid…
Combines with filtered weak bases e.g. HPO42- (Which is lipid soluble, and permeable), to form H2PO4 (Which is impermeable)
H2PO4- is lipid insoluble, SO bound protons are excreted
H+ can also be excreted bound to creatinine and/or citrate (urates in birds).
Once H+ is inside the tubular filtrate, it can join weak bases such as ammonia to form…
Where does this occur?
What is it formed from?
H+ can join ammonia (NH3) - (lipid soluble) which is a weak base to form NH4+ (A weak acid → Transported) (not lipid soluble)
Main sites
PCT (Production and secretion), CD regulation of excretion
Most NH4+ is formed from amino acids (particularly glutamine).
During acidosis, how much does NH4+ excretion increase?
Up to 10 fold
Ammoniagenesis and ammonium excretion, account for 60-90% of net acid excretion in mice, rats, dogs, chickens and humans (not, cats, rabbits).
How is ammonia produced?
In the proximal tubule → Glutamine broken into NH3 + H+ and HCO3-
HCO3- absorbed with Na+ into the capillaries (Cotransporter)
NH3 joins with H+ forming NH4+
NH4+ enters filtrate, Na+ enters tubular cell (Counter transporter)
Describe what happens once NH4+ is produced in the PCT.
Passes through the descending loop, to the ascending loop of henle.
Na+ / K+ / 2 Cl- channel (Originally all into the tubular cell) can be used to transport NH4+ (Substitutes K+)
NH4+ and Na+ transported into the tubular cell, 2 Cl- can be transported into the filtrate
NH4+ transported into interstitial space
Can break down into ammonia and hydrogen ions again
High medullary [NH4+] maintained by counter current multiplication
Some of which is absorbed by the collection duct as H+ and NH3
Describe how ammonium and ammonia enter the collecting duct to be excreted.
Basolateral Membrane
NH4+ and Na+ Cotransporter
Transports NH4+ into tubule cells
NH4+ can break down into ammonia and H+
NH3 Channels
Transports NH3 into the tubule cells
Apical Membrane
NH3 Channel
Transports NH3 into the filtrate
H+ and K+ Channel
H+ joins with NH3 to form NH4+
During acidosis, how can ammonia channels be regulated?
During acidosis, NH3 and NH4+ channels are up-regulated
Promoting NH4+ formation in the collecting duct to be excreted
What effect does angiotensin II have on acid/base regulation?
Stimulates absorption of bicarbonate into capillaries
Via Na+ and HCO3- Cotransporter
What effect does corticosteroids / endothelin have on acid/base regulation?
Increases H+ secretion into filtrate via Na+ and H+ Cotransporter
What effect does PTH have on acid/base regulation?
Inhibits angiotensin II and corticosteroid/endothelin effects
How does the collecting duct determine final urine pH?
By H+ and HCO3- secretion
What is the pH of initial CD filtrate?
7.4
What purpose do the type A intercalated cells have and where are they found?
Found in CD - Most active under conditions of acidosis
Type A intercalated Cells produce HCO3- and H+
Can directly secrete hydrogen ions using H+ ATPase pump or H+ / K+ ATPase channel (On Apical Surface)
H+ in filtrate, K+ in tubule cell
Basolaminar surface has HCO3- / Cl- channels to move bicarbonate back into interstitial space
Apical surface also has NH3 channels to move ammonia into filtrate
How are the Type A Intercalated Cells regulated during acidodis?
Increased NH3 channels
Up-regulate K+ / H+ and H+ channels
What purpose do the type B and C intercalated cells have and where are they found?
Found in CD, most active under alkalosis-conditions
Mirror image of acid secreting cells
Move bicarbonate out into filtrate (HCO3- and Cl- transporter)
HCO3- into filtrate
Cl- into tubular cell
Move hydrogen ions into interstitial space
Activity increased by alkalosis and inhibited by acidosis
Increased by aldosterone and angiotensin II
If there is an increased production/consumption of H+, results in a reduction in…
If there is an excess amount of bases, results in..
Will use and result in a reduction in buffers, including HCO3-
Reabsorb HCO3-, (matched by 1:1 H+ excretion)
Produce HCO3- (matched by 1:1 H+ excretion)
Kidney excretes HCO3-
What hormones will chronic metabolic acidosis activate and what effects will it have?
Angiotensin II, Endothelin, PTH
Level of PCT
Reabsorb HCO3-
H+ Secretion
Generation of NH4+
Generation of HCO3-
Level of CD
AND H+ Secretion, NH4+ entry/H+ secretion
Glucocorticoids
Reabsorb HCO3-
H+ Secretion
Generation of NH4+
Generation of HCO3-
What are possible causes of chronic metabolic acidosis?
Increase non-volatile acids e.g. lactic acid
Ketosis
Increased B-hydroxybutyric acid
Increased Acetoacetic acid
Increased loss of HCO3-
Prolonged starvation
Diabetes mellitus
Rumen acidosis
Renal failure
Faecal HCO3- loss
Diarrhoea
Respiratory acidosis (severe)
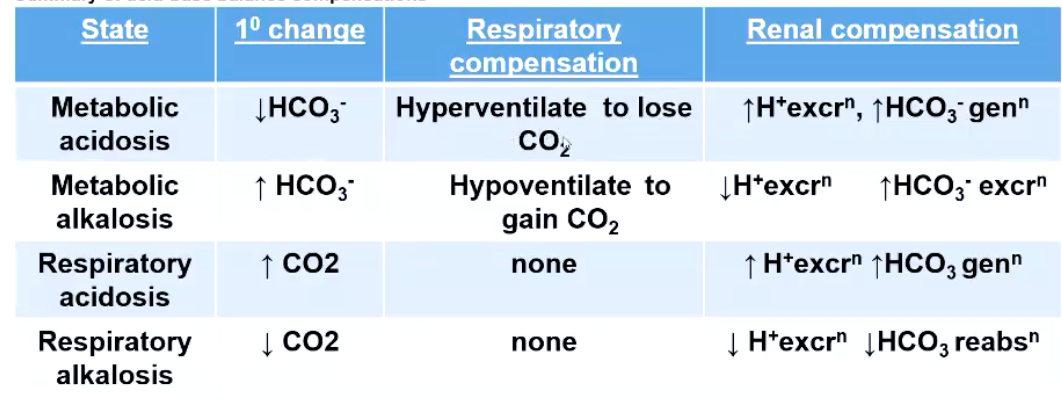
Describe the renal acid base regulation occuring in concert with the respiratory system. For each describe…
10 Change
Respiratory Compensation
Renal Compensation
Metabolic acidosis
Metabolic alkalosis
Respiratory acidosis
Respiratory alkalosis
What is proteinuria or albuminuria caused by?
alteration in filtration barrier (Glomerulus)
What is haemoglobinuria caused by?
Exceeding binding capacity of haptoglobulin to Hb present in filtrate
What is glucosuria caused by?
exceeded Tm for glucose, secondary increase in water loss due to osmotic potential of the filtrate
What is water diuresis caused by?
increased volume of excreted urine due to low concentrations of ADH in plasma
What is polyuria caused by?
abnormally large volume of urine, could be water diuresis or osmotic challenge, e.g. secondary to glucosuria
Reminder, where do the following drugs act and how do they affect renal function?
Loop Diuretics
Potassium sparing diuretics
Osmotic Diuretics
Loop diuretics - act on ascending limb of LOH to inhibit transport proteins that mediate cotransport of Na+ (Cl- and K+).
Potassium sparing diuretics - act in cortical CD to inhibit Na+ reabsorption and K+ secretion, by either inhibition of aldosterone or epithelial Na+ channel
Osmotic diuretics - filtered but not reabsorbed.