Chapter 7: Bone Tissue
1/134
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
135 Terms
functions of the skeleton
support
protection
movement
electrolyte balance
acid-base balance
blood formation
hormone secretion
osseous tissue
connective tissue in which the matrix is hardened by the deposition of calcium phosphate and other minerals
no
No
what makes up the bone
osseous tissue, blood, bone marrow, cartilage, adipose tissue, nervous tissue, fibers
what kind of bones do cranial bones form? where else do these kind of bones form
flat bones (thin curved plats)
sternum (breast)
scapula (shoulder blades)
ribs
hips
what are the most important bones in movement? where can you find them
long bones that serve as a lever
limbs
digit bones
short bone and irregular bones. where can you find them
bones that don’t fit the long or flat bone groups
wrist, ankle (short)
vertebrae, some skull bones (irregular)
compact, dense, cortical bone
outer shell of dense white osseous tissue that encloses the marrow cavity
marrow (medullary cavity)
contains bone marrow
spongy bone
ends of bone where the central spacy is occupied by a more loosely organized form of osseous tissue
what is the ratio of compact bone to spongy bone
¾ : ¼
No
No
diaphysis
provides leverage
epiphysis
enlarged to strengthen the joint and provide added surface area for the attachment of tendons and ligaments
what is unique about mature bone
exhibits epiphyseal line of slightly dense spongy bone between the epiphysis and diaphysis (remnant of a childhood growth zone aka epiphyseal plate)
articular cartilage
a hyalin cartilage that covers the joint surface where one bone meets another
articular cartilage along what what enables a joint to move easily
lubricating fluid
nutrient foramina
minute holes in the bone where blood vessels can penetrate
periosteum
sheath that covers the bone that provides strong attachment and continuity from muscle to tendon to bone
what is the periosteum made of
outer fibrous layer, inner osteogenic layer
What are 2 pathways of the outer fibrous layer
collagen fibers penetrate into the bone matrix as perforating fibers
continuous with the tendons that bind muscle to bone
endosteum
thin layer of reticular connective tissue that lines the internal marrow cavity, covers surfaces of spongy bone, and lines a canal system in compact bone
function of flat bone
shield like plates that protect delicate organs (brain and heart), and form broad surfaces for muscle attachment (scapula, hip)
2 layers of flat bone
inner and outer tables (sandwiching spongy bone)
diploe definition and function
spongy layer in the cranium
absorb the impact
what does the epiphyseal line mark
site of epiphyseal plate that has ossified (closed). once closed, growth in length no longer occurs at the site
4 types of bone cells
osteogenic
osteoblasts
osteoblasts
osteoclasts
osteogenic cells
stem cells that give rise to other bone types from mesenchyme
where do you find osteogenic cells
endosteum, inner layer of periosteum, central canals
what is unique about osteogenic cells
only cells capable of dividing continually and producing more bone cells
what do osteogenic cells become
osteoblasts
osteoblasts
bone forming cells that synthesize the organic matter of the bone to promote mineralization (formation of the organic bone matrix)
osteogenesis
bone-building activity
what do osteoblasts from
rows in the endosteum and inner layer of the periosteum
what tissue do osteoblasts resemble
cuboidal epithelium on the bone surface
What do osteoblasts consist of
mitochondria, rough ER, and secretory vessicles
What stimulates the acceleration of osteogenic mitosis
stress and fractures
osteocyte
former osteoblasts that are embedded in the matrix
what % of bone cells do osteocytes make up? how long do they live?
90-95%, decades
where do osteocytes live and define that
lacunae (cavities in a bone)
canaliculi
slender channels that interconnect lacunae
describe the dendrite process for osteocytes
dendrites of Osteocytes go through the canaliculi to reach other Osteocytes, blood vessels and other osteoblasts
how do osteocytes pass nutrients and how do they dispose of waste
gap junctions where their processes meet to pass nutrients and signals
pass their metabolic wastes to blood vessels
what is unique about osteocytes
resorb or deposit bone matrix that contributes to homeostasis of bone density and blood concentrations
strain sensors
why are osteoblasts and osteocytes important for endocrine cells
secretes osteocalcin (responsible for fight-or-flight)
osteocalcin
inhibits the parasympathetic nervous system and allows the sympathetic system to work unopposed
stimulates the pancreas to make insulin
increase the insulin sensitivity of fat cells
acts on skeletal muscles to promote energy availability and capacity for exercise
influence brain dev and function and male fertility
osteoclasts
bone dissolving cells on the bone surface
osteolysis
osteoclasts dissolves bone
where do osteoclasts develop
bone marrow stem cells as blood cells (independent of blast, clast, and cytes)
What is the reason behind the large size of osteoclasts
several stem cells fuse together to form osteoclast (150 micrometer and 3-4 nuclei)
ruffled border
side of osteoclast facing the bone surface with many deep infoldings of the plasma membrane that increase surface area and efficiency of bone resorption
resorption bays
etched pits in the bone where osteoclast reside
what cells perform osteogenesis? what bone cell performs osteolysis
osteocytes and osteoblasts
osteoclast
lacunae
Spaces between lamellae that contain osteocytes
matrix (bone)
stony matter that surrounds the osteocytes and lacunae
what percent of the matrix is organic? what is it synthesized by? what are these organic substances
1/3 organic
osteoclasts
collagen, protein-carb complexes
what makes up the majority of the inorganic matter in the matrix
85% hydroxyapatite (crystallized calcium phosphate)
compact bone contains
concentric lamellae
central (haversian) canal
osteon (haversian system)perforating canals
concentric lamellae
onion like layers of matrix arranged around the central canal
osteon (haversian system)
basic structural unit of compact bone
cylinder of tissue surrounding a central call
made up of central canal and its lamellae
perforating canals
connects central canals of 2 neighboring osteons
what are central and perforating canals lined with
endosteum
what separates each osteon
cement line that blocks microfractures from spreading
how do the central canals get fed and dispose of waste
foramina open into the perforating canals that cross the matrix
waste is removed by the blood stream
circumferential lamellae
inner and outer boundaries of dense bone hat run parallel to the bone surface
interstitial lamellae
irregular regions, remains of old osteons that broke down
spongy bone consists of
spicules (rods or spines) and trabeculae (thin plates or beams)
bone marrow
soft tissue that occupy the marrow cavity
red bone marrow (myeloid tissue)
hematopoietic tissue (tissue that produce blood cells) that fills the marrow cavity
yellow bone marrow
fatty bone marrow that replaces red marrow in adults
where is red marrow limited to in adults
skull, vertebrae, ribs, sternum, hip, and proximal heads of the humerus and femur
Does yellow marrow produce blood
no, but if needed it can turn back into red marrow
ossification (osteogenesis)
bone formation
2 method of ossification
intramembranous and endochondral
intramembranous ossification
produces flat bones of the skull, clavicle, and part of the mandible
what are the 4 steps to intramembranous ossification
mesenchyme (soft tissue w/ blood vessels) condenses. mesenchymal cells —> osteoblasts and secrete osteoid tissue (prebone)
osteoblasts deposit minerals on osteoid, hardening it. osteoblasts —> osteocytes
periosteum and trabeculae forms
osteoblasts deposit bone on surfaces, creating thick compact bone
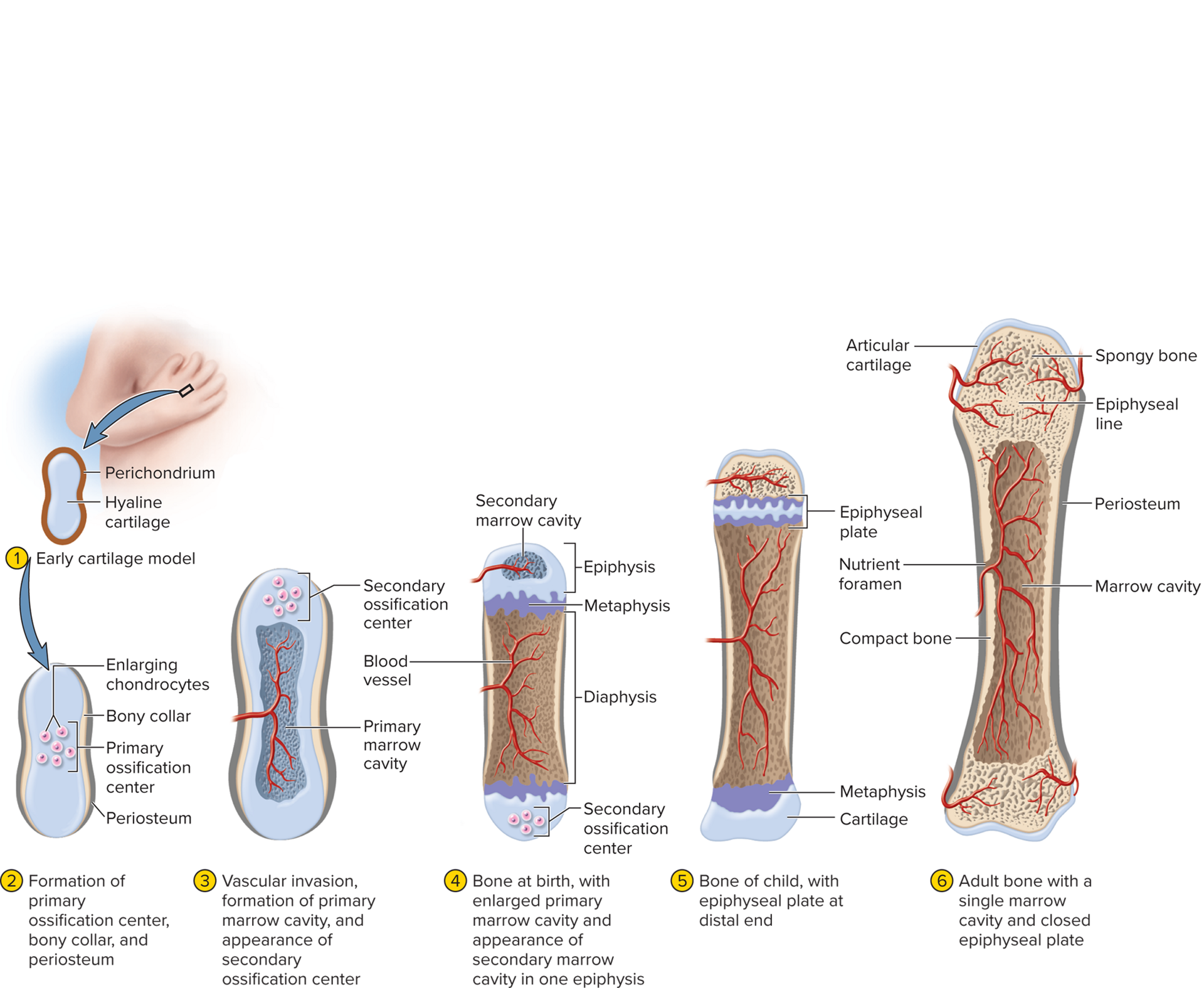
endochondral ossification
bone develops from preexisting model composed of hyalin cartilage
when does endochondral ossification begin
sixth week of fetal development
6 steps of endochondral ossification
cartilage model: hyaline cartilage covered with fibrous perichondrium forms
primary ossification center: walls calcify, osteoblasts forms a bone collar around the cartilage
marrow cavity formation: cells digest the cartilage and osteoblasts deposit bone layers
secondary ossification centers: epiphyses, forms secondary ossification centers and marrow cavities
epiphyseal plate: cartilage remains at the ends a articular cartilage and in the epiphyseal plate
adult bone: epiphyseal plate disappears, marrow cavities join to make adult bone
metaphysis
where epiphysis and diaphysis meets
trabeculae
thin plates of bone found in spongy bone
zone of reserve cartilage
furthest from the marrow cavity
consists of: hyalin cartilage w/ resting chondrocytes
zone of cell proliferation
chondrocytes multiply and arrange themselves into columns of lacunae
accounts for child growth in height
zone of cell hypertrophy
mitosis stops, cells begin hypertrophy (enlarge), walls of the matrix between the lacunae become thin
accounts for child growth in height
zone of calcification
minerals are deposited in the matrix between the columns of lacunae and calcify cartilage for temporary support
zone of bone deposition
walls between the lacunae break down and chondrocytes die, forming channels. blood vessels invade those channels, osteoblasts create bone layers, and osteoclasts dissolve cartilage, resulting in spongy bone
epiphyseal line
slightly denser spongy bone
appositional growth (in mature bones only!!!)
the deposition of new tissue at the surface (widening of the bone) that occurs by intramembranous ossification at the bone surface
only in mature bones
what is the process of appositional growth
osteoblasts in the inner layer deposit osteoid tissue on the bone surface, calcify it, and become trapped in the osteocytes
circumferential lamellae
surface layers of bone
as bone diameter increases, _____ _____ widens. why does this happen?
marrow cavity
osteoclasts dissolve tissue on the inner bone surface
flat bones develop by ____ ossification, where as long bones develop what?
intramembranous ossification
intramembranous, endochondral ossification, appositional
Wolff’s law of bone
architecture of a bone in determined by the mechanical stresses placed upon it
Where does the calcium and phosphate used to mineralize bone come from?
osteoblasts
resorption
dissolving bone and releasing minerals
explain the relationship between osteoclasts and osteoblasts in bone remodeling.
if the bone is used a little, osteoclasts function to get rid of extra mass. if the bone is heavily used, osteoblasts deposits new osseous tissue and thickens it.
mineral deposition (mineralization)
crystallization process in which calcium, phosphate, and other ions are taken from the blood plasma and deposited in bone tissue, mainly as hydroxyapatite
what are the steps to mineralization
osteoblasts lay down collagen fibers
collagen fibers attact the minerals from the blood
hydroxyapatite forms on the fibers
accumulation of hydroxyapatite hardens the bone
more crystals attract more minerals
ectopic ossification
abnormal calcification of tissues, occurs in the lungs, brain, eyes, muscles, tendons, arteries, and other organs