N245: Disorders of Leukocytes & Lymphoid Tissues
1/120
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
121 Terms
How much blood do humans have?
5 liters (1.3 gallons)
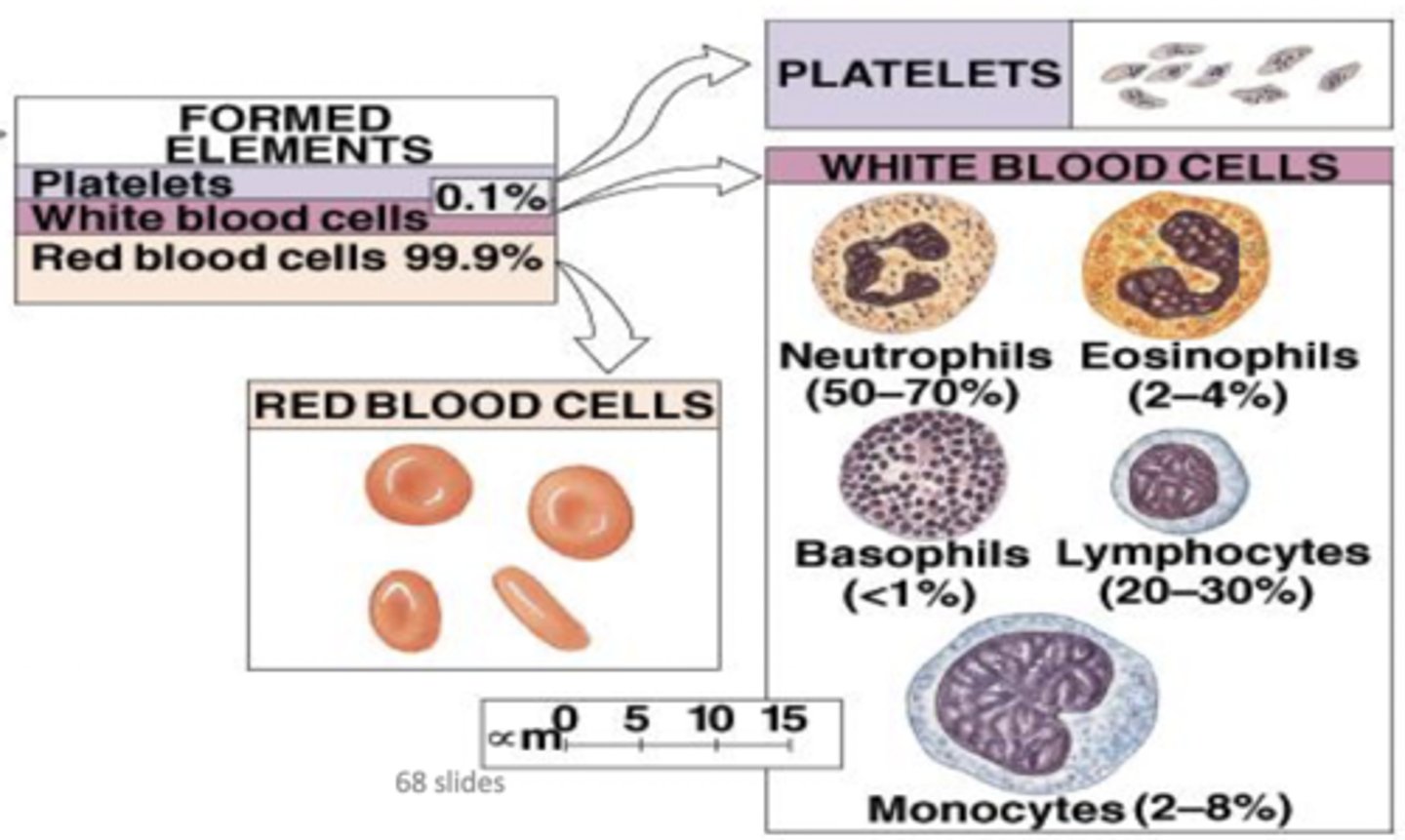
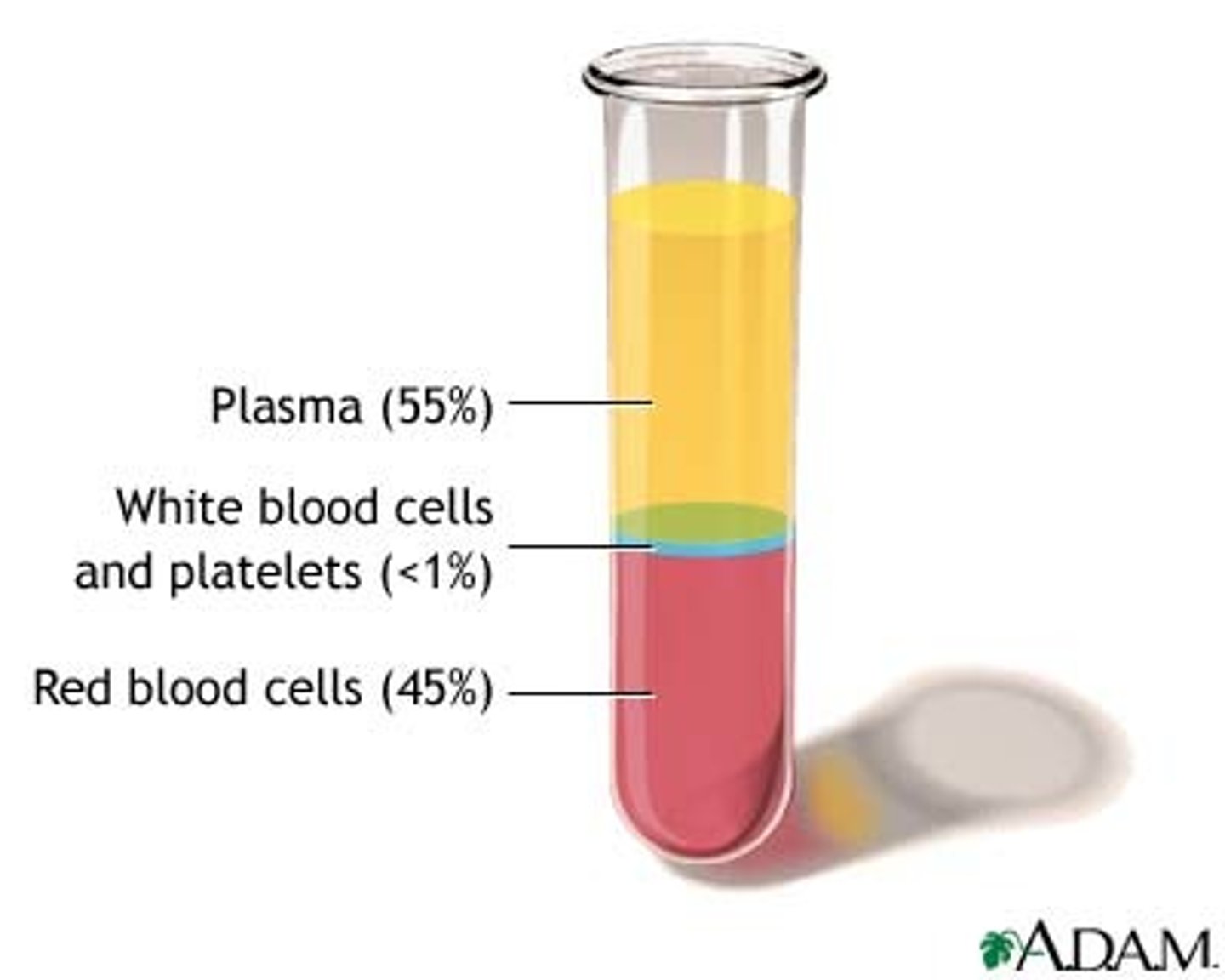
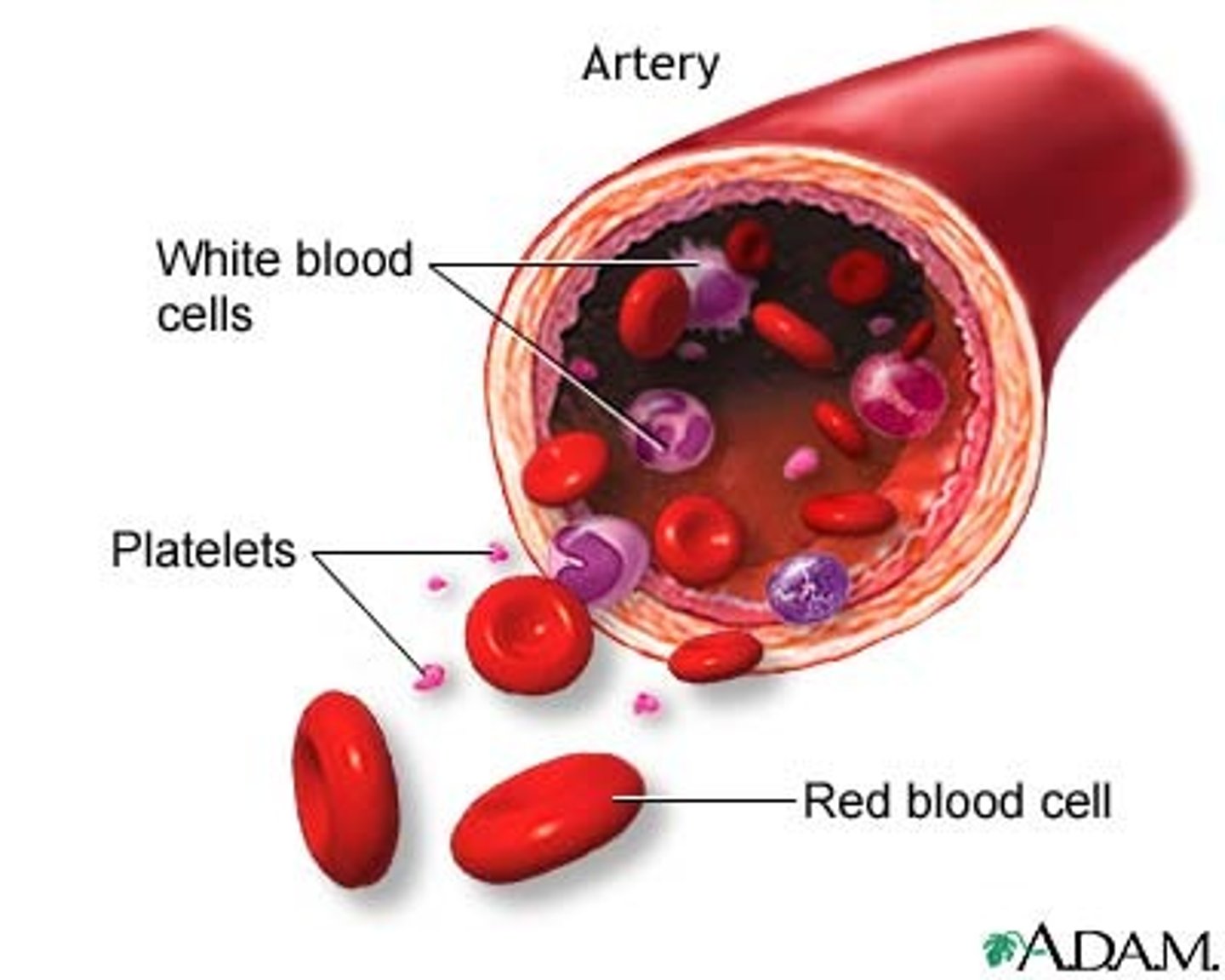
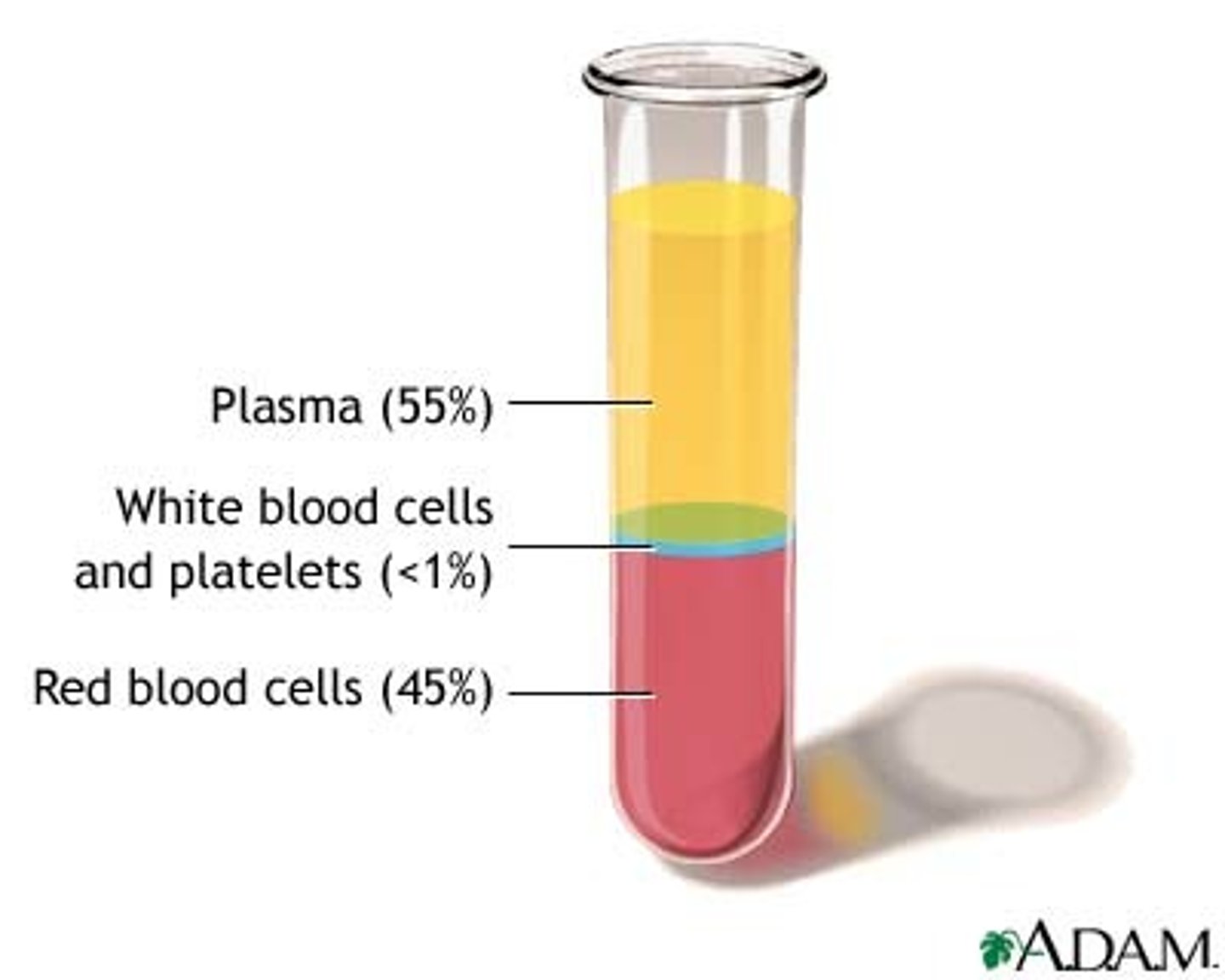
What is the cellular component of blood?
Erythrocytes, leukocytes, thrombocytes (45% of blood)
What is blood plasma?
Liquid part of blood, mostly water and proteins (55% of blood)
What are the functions of blood?
Transportation of nutrients, protections against pathogens, regulation of homeostasis
Blood fractionation
The process of separating blood into its component parts using a centrifuge
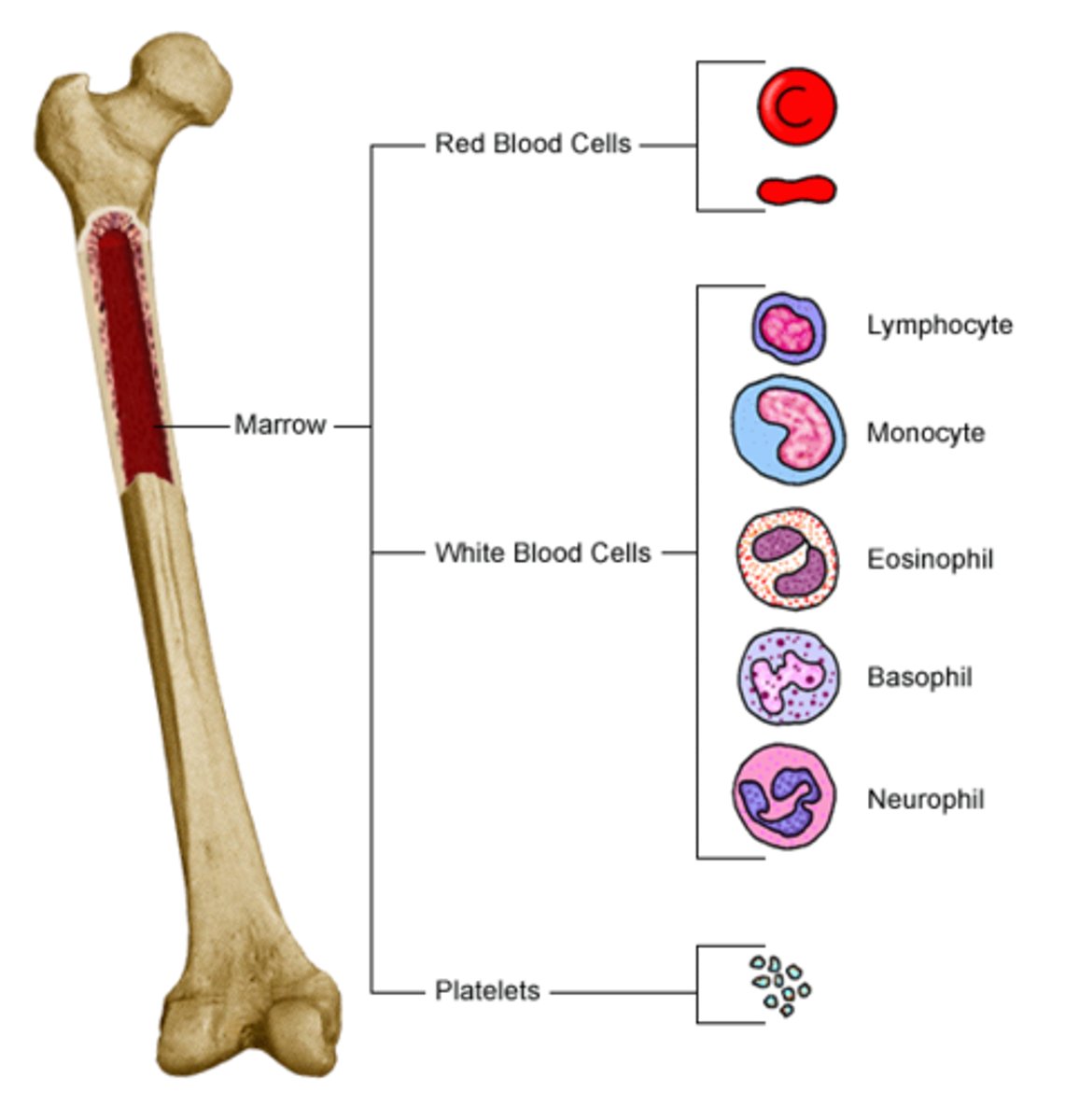
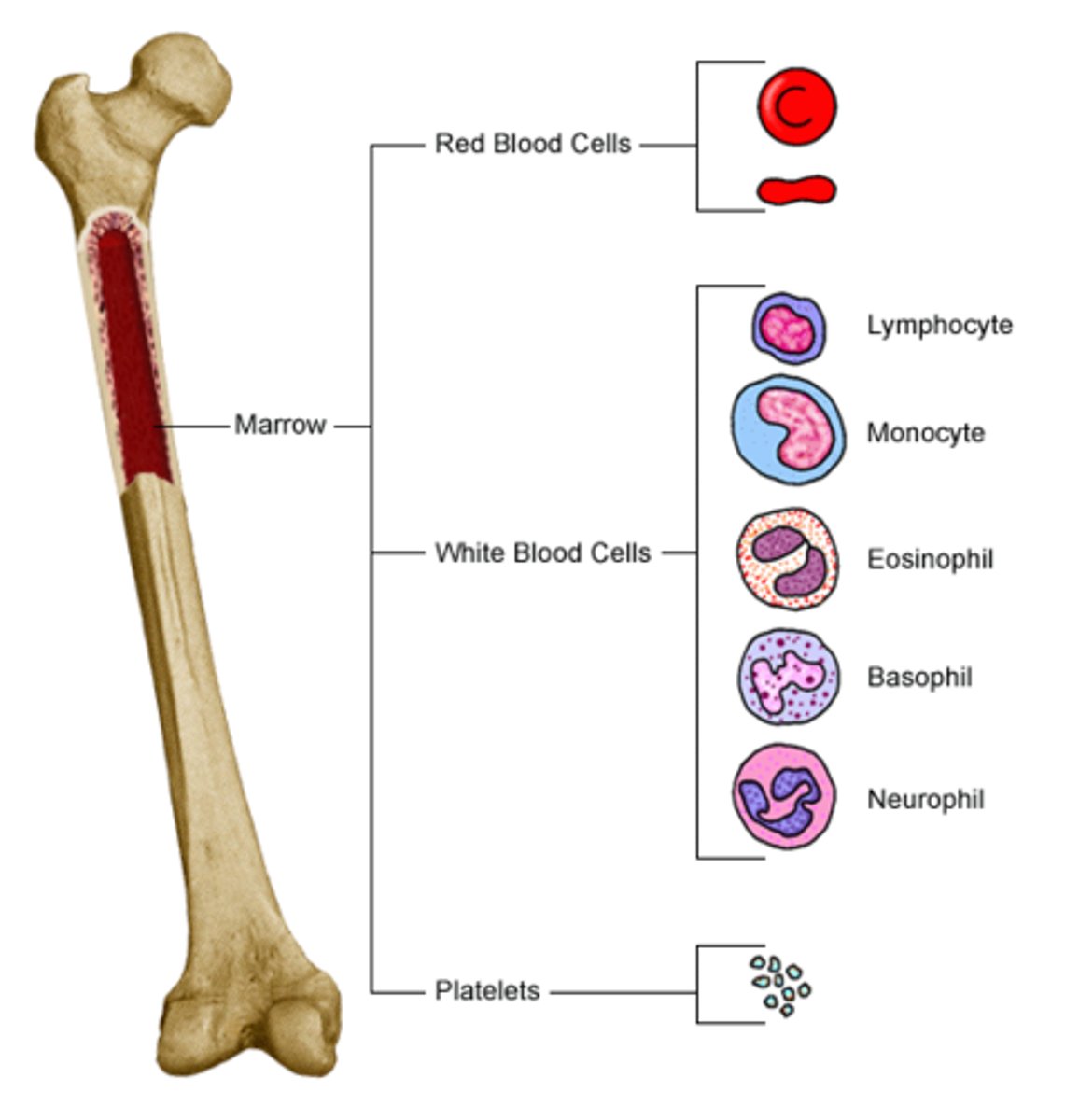
Hematopoiesis
The formation of blood cells from stem cells in the bone marrow
What are pluripotent cells?
Stem cells that can differentiate into each of the different types of blood cells

Lymphoid stem cell
Differentiates into the 3 types of lymphocytes (T cells, B cells, NK cells)
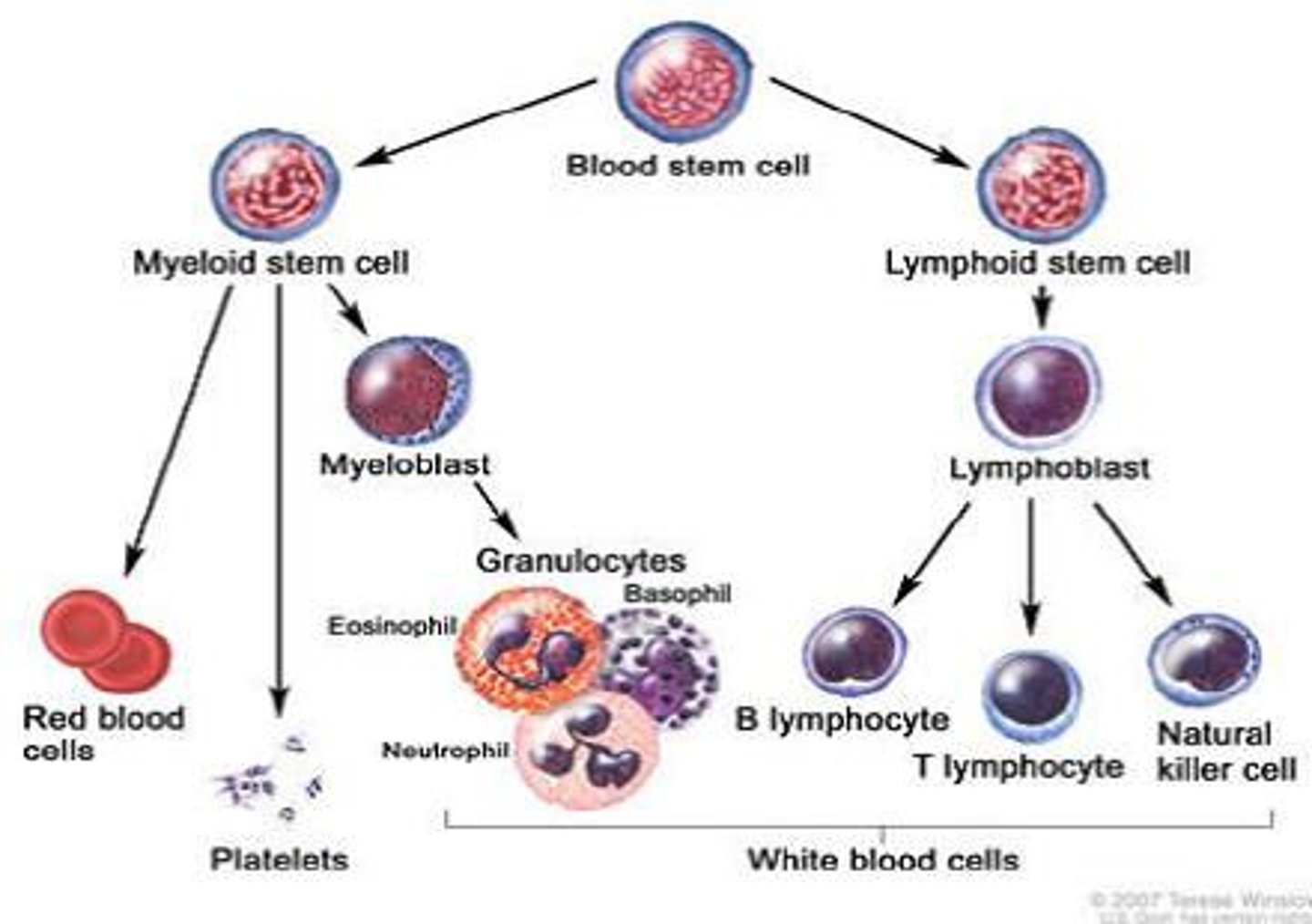
Myeloid stem cell
Differentiates into erythrocytes/platelets, and granulocytes/monocytes
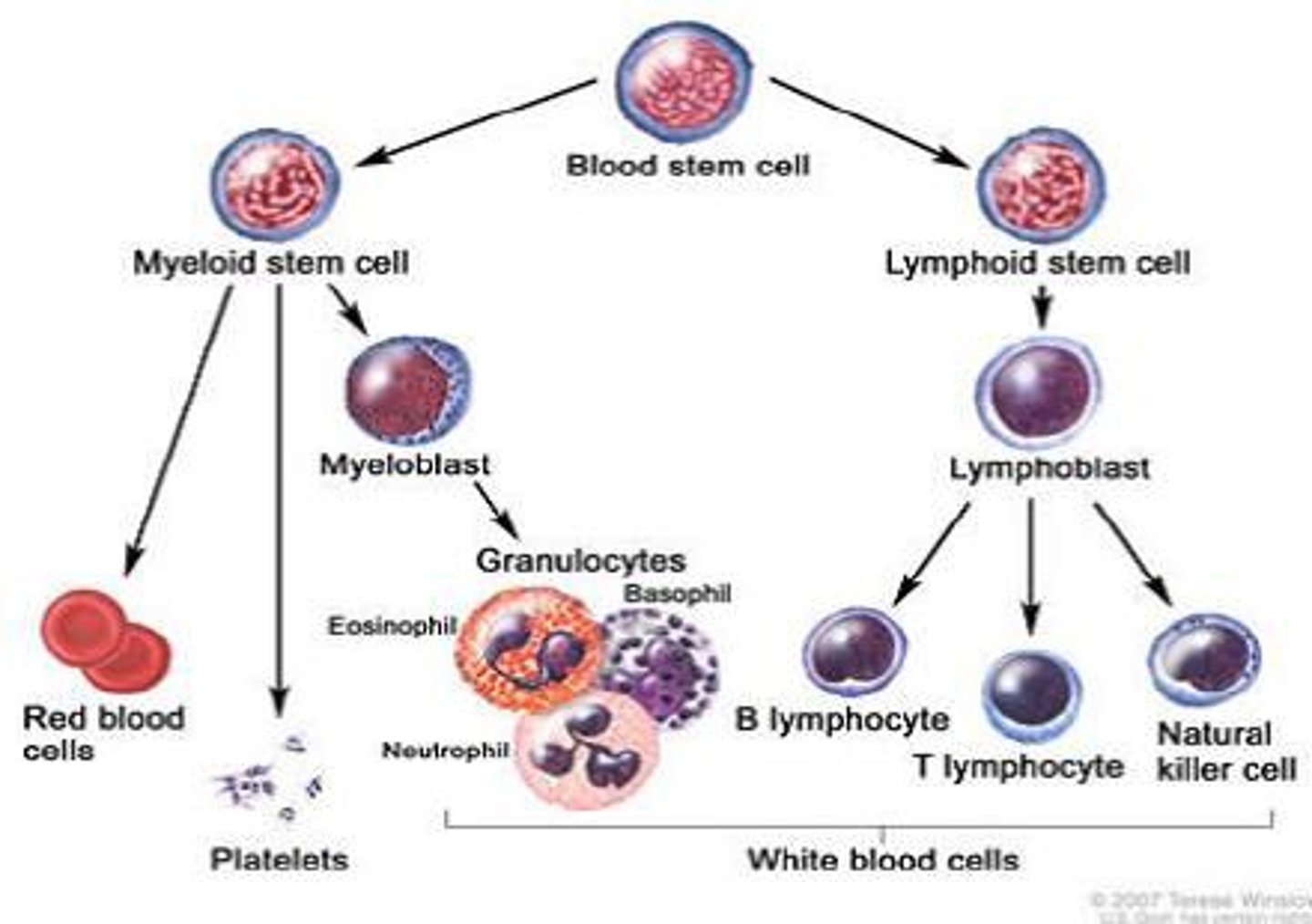
Hematopoietic growth factors
"Hormones" that promote and regulate the differentiation and proliferation of blood cells
AKA colony stimulating factors
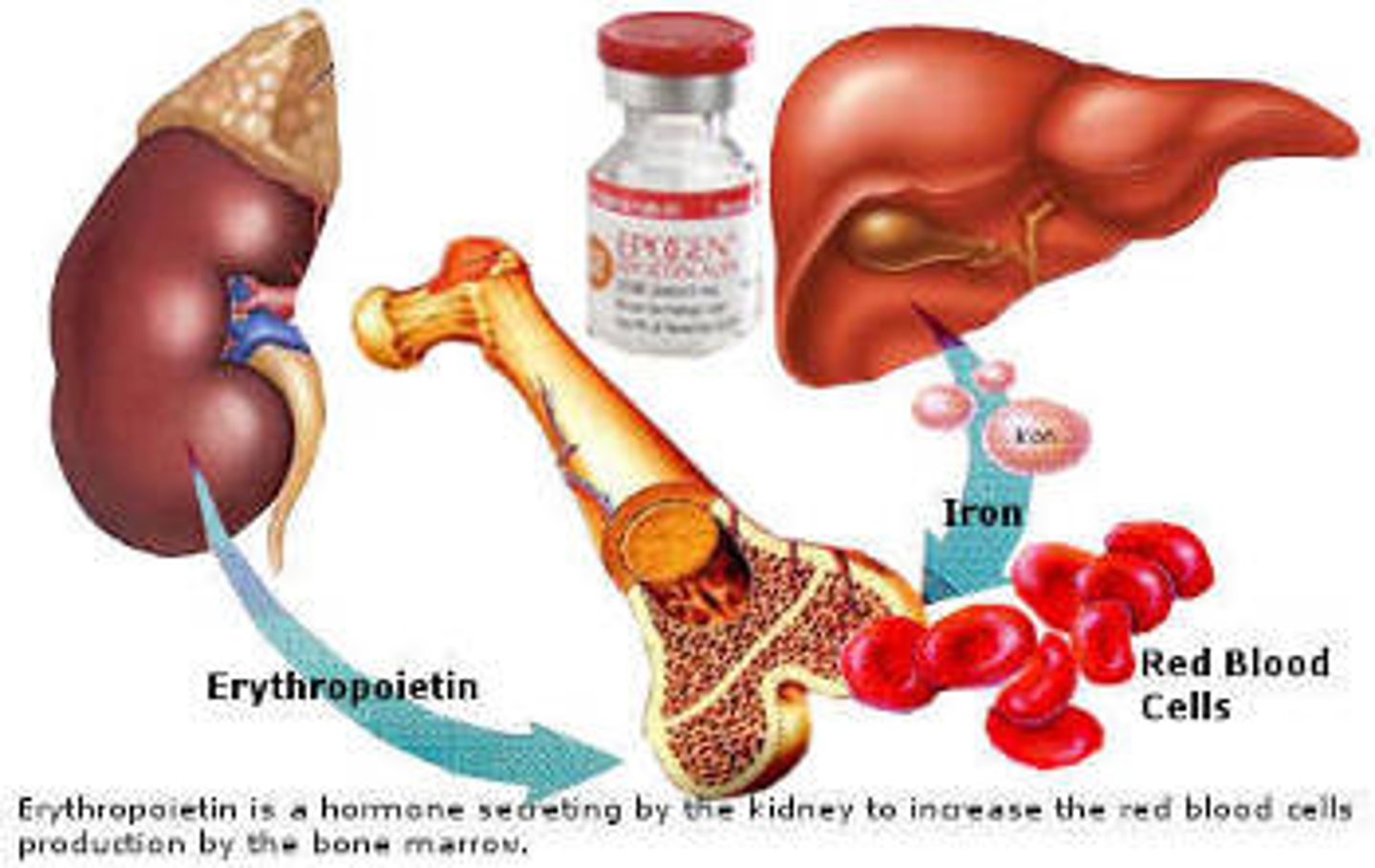
EPO
Erythropoietin; promotes growth of red blood cells
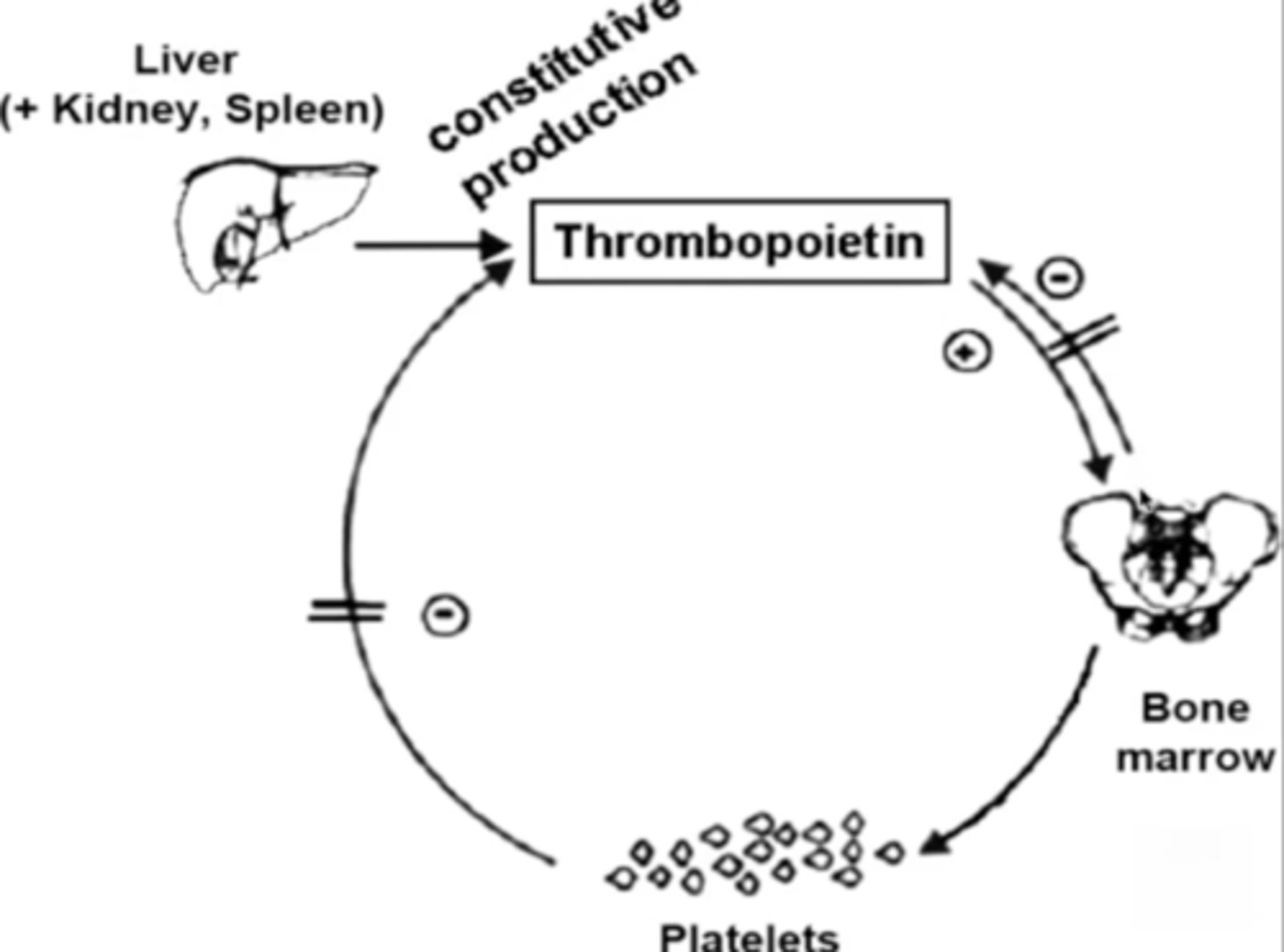
TPO
Thrombopoietin; stimulates platelet production
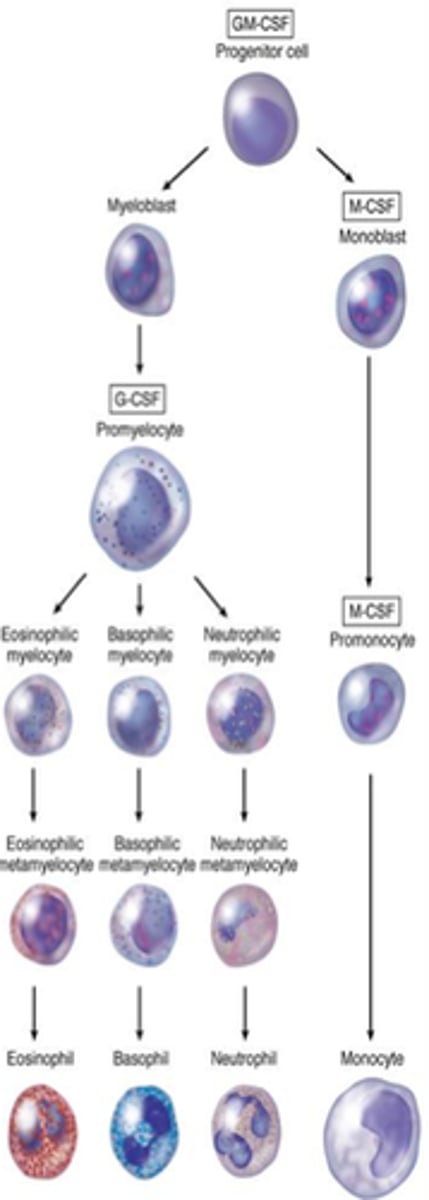
GM-CSF
Granulocyte-macrophage colony-stimulating factor; stimulates granulocytes and monocytes
Hematology
The study of blood and blood disorders
Hematology nurses
These nurses specialize in caring for patients with blood disorders

Leukocytes
White blood cells

Granular leukocytes
Neutrophils, eosinophils, basophils
PHILLED (filled) with granules (enzymes)
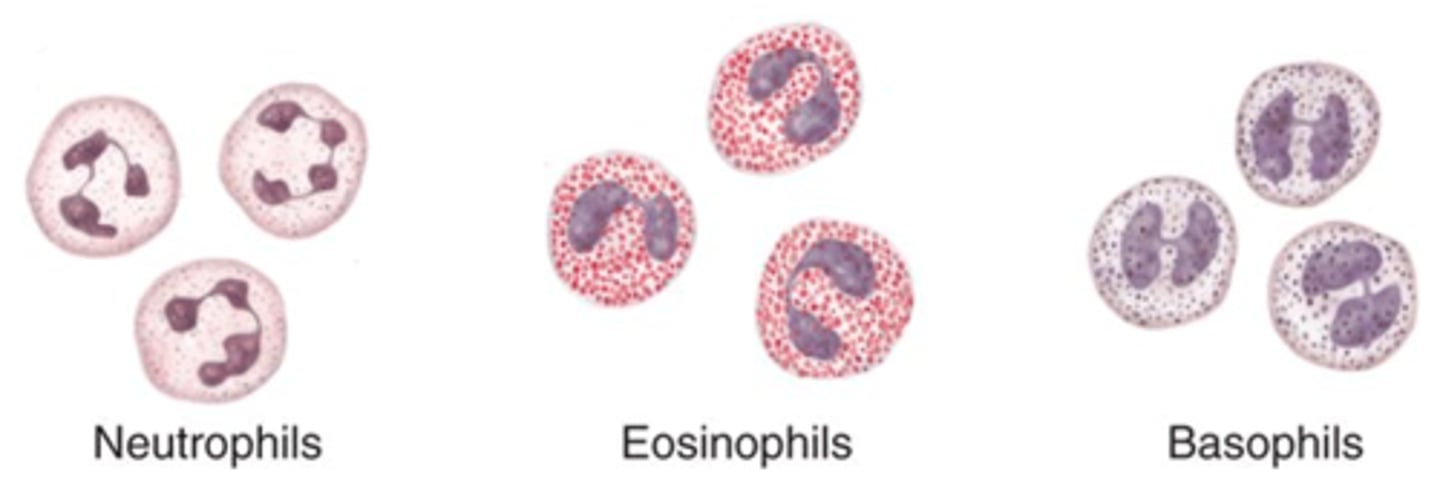
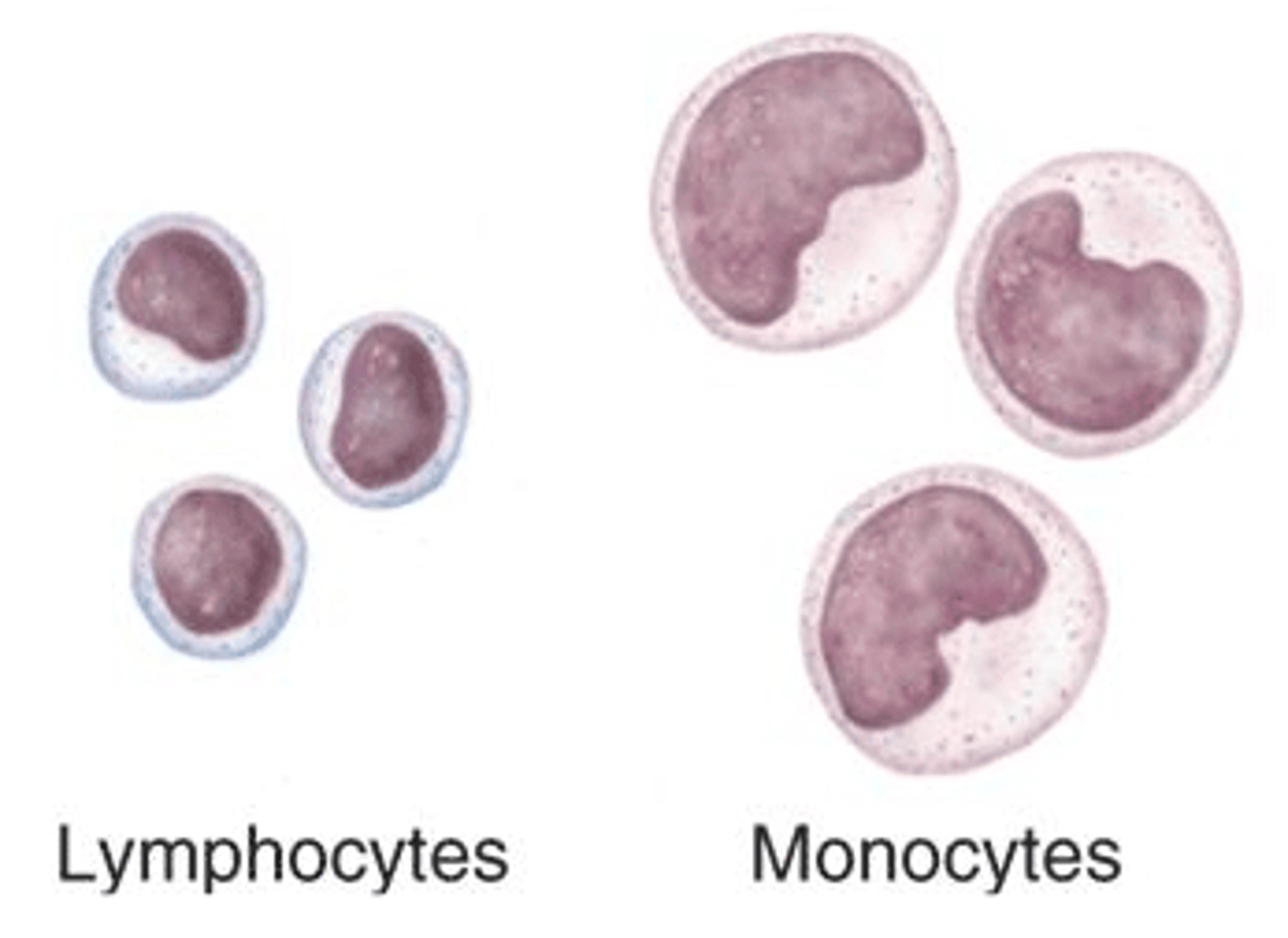
Agranular leukocytes
Lymphocytes and monocytes
No granules
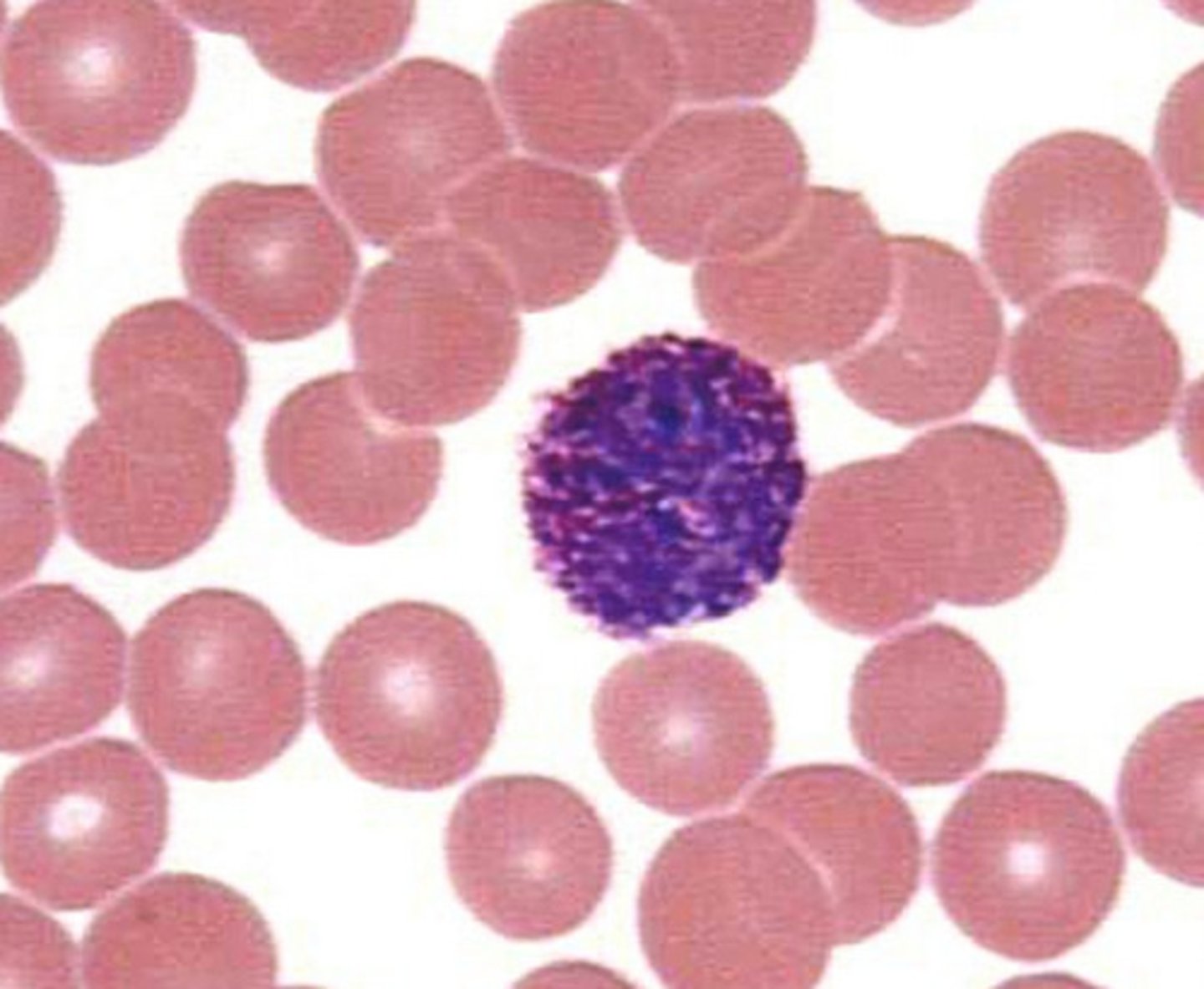
What is unique about lymphocytes?
They can move between blood and lymphatic tissue, whereas all others only circulate in blood
That's why they're called LYMPHocytes you silly goose
What are the two most common leukocytes?
Neutrophils and lymphocytes
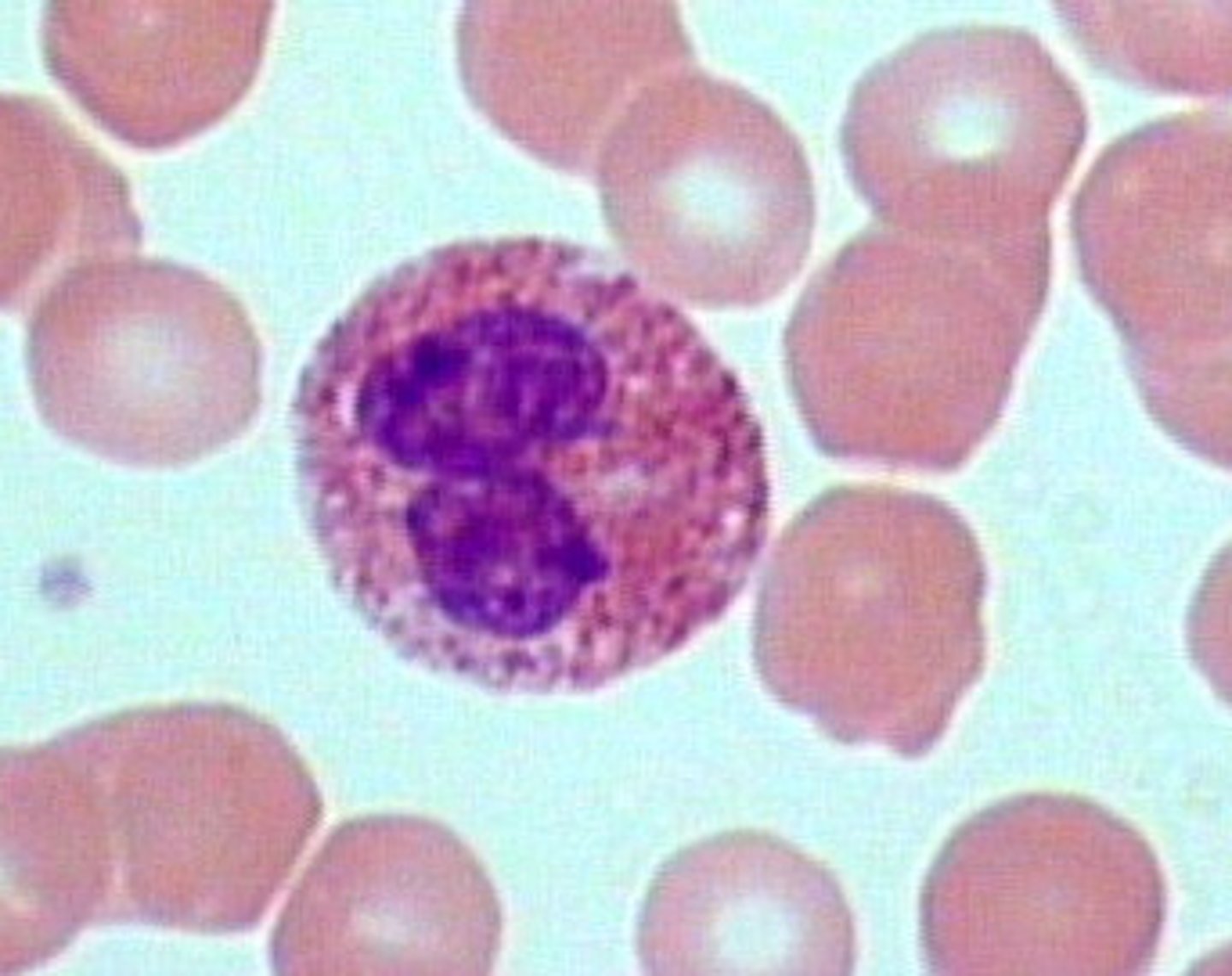
Neutrophils structure
Nuclei has three or more lobes, granules stain light pink

Neutrophils function
most common WBC; fights bacterial infections by engulfing bacteria by phagocytosis (innate immunity)
Where does the name neutrophils come from?
Their granules do not stain with acid OR basic dye -- they are neutral
Other name for neutrophils
Polymorphonuclear leukocytes (bc they have many lobes)
Eosinophils structure
Nuclei has two lobes, granules stain bright red
Eosinophils function
A WBC that digests and destroys parasitic worms, they also play a role in allergy and immune response (innate immunity)
Where does the name eosinophils come from?
Their granules stain bright pink/red with acidic dye called eosin
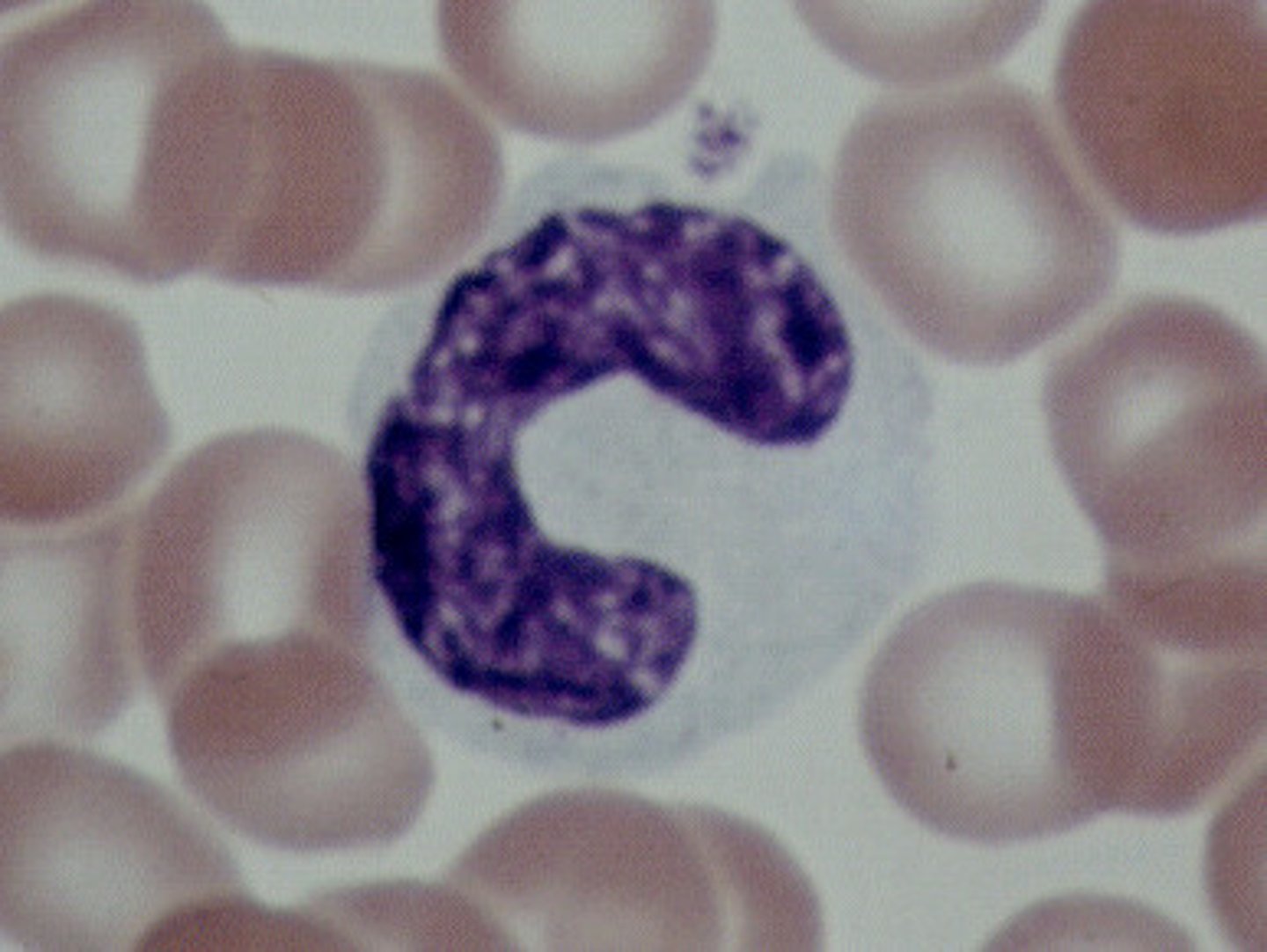
Basophils
Nuclei is U or S shaped but is obstructed by HUGE blue granules
Basophil function
A WBC that produces histamine --> causing inflammation during an immune response (innate immunity)
Where does the name basophils come from?
Their granules stain blue with BASic dye called hematoxylin dye
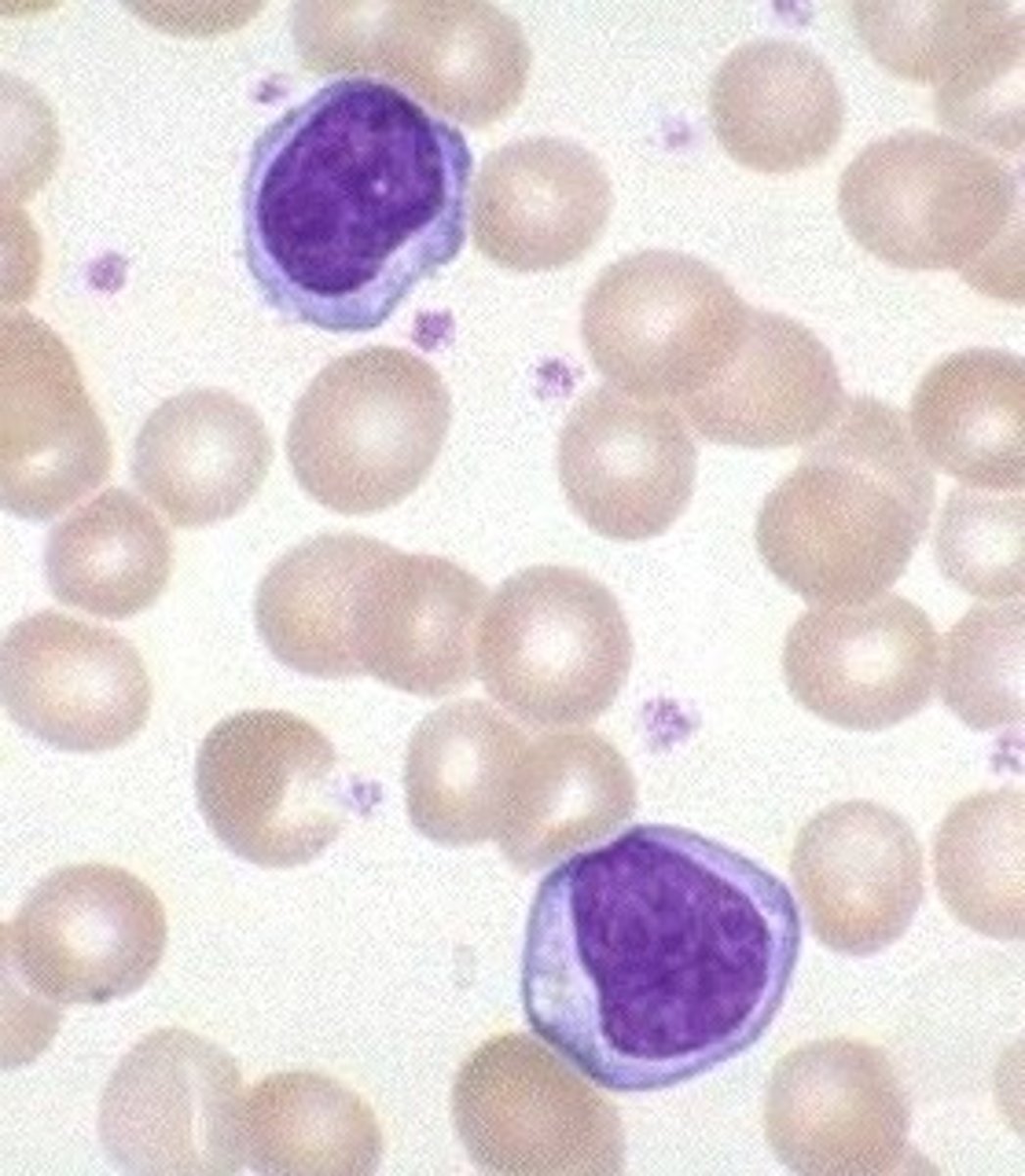
Monocytes structure
Largest WBCs, U shaped nucleus
Monocytes function
A large WBC that transform into macrophages(outside blood stream) to fight off viruses and chronic infections (innate immunity)
Lymphocytes structure
Has a large, dark purple nucleus that takes up most of the cell volume
Lymphocytes function
Fight off viral infections B & T cells provide acquired immunity, NK cells provide innate immunity
B cells
A type of lymphocyte that are created and mature in the bone marrow; creates antibodies that isolate and destroy pathogens, provide humoral acquired immunity
Naive B cells
A B cell that has not been exposed to an antigen yet
Effector B cells
Active B cells that have been exposed to antigens
Plasma cells
A type of effector terminally differentiated B cells, they produce and secrete antibodies
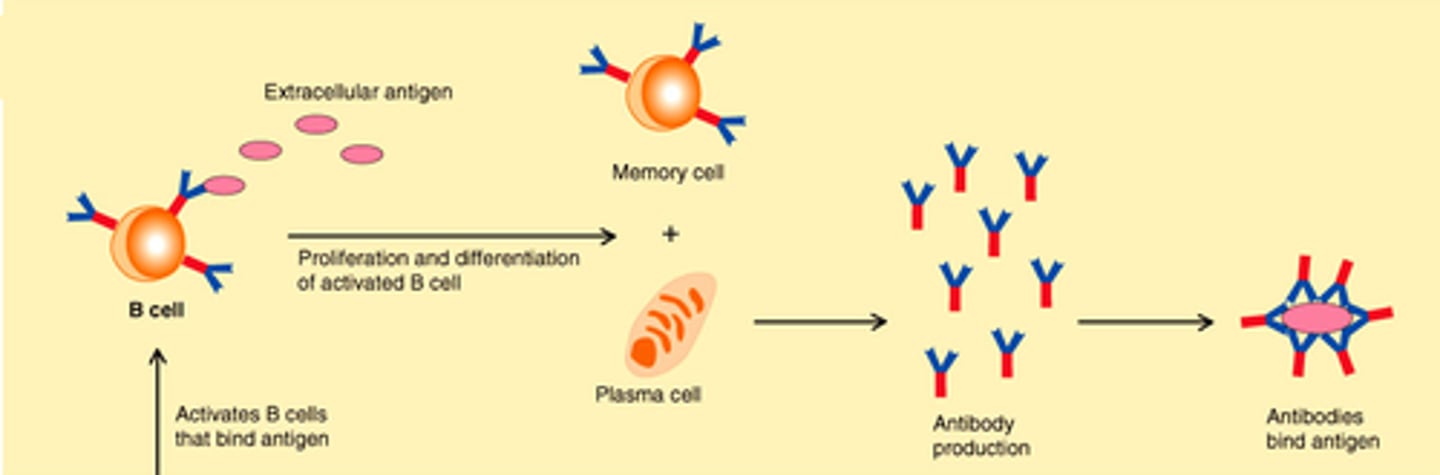
Memory B cells
A type of effector B-cell that memorizes the characteristics of the pathogen antigen; it remains dormant until reactivated by the same antigen
An elephant never forgets.

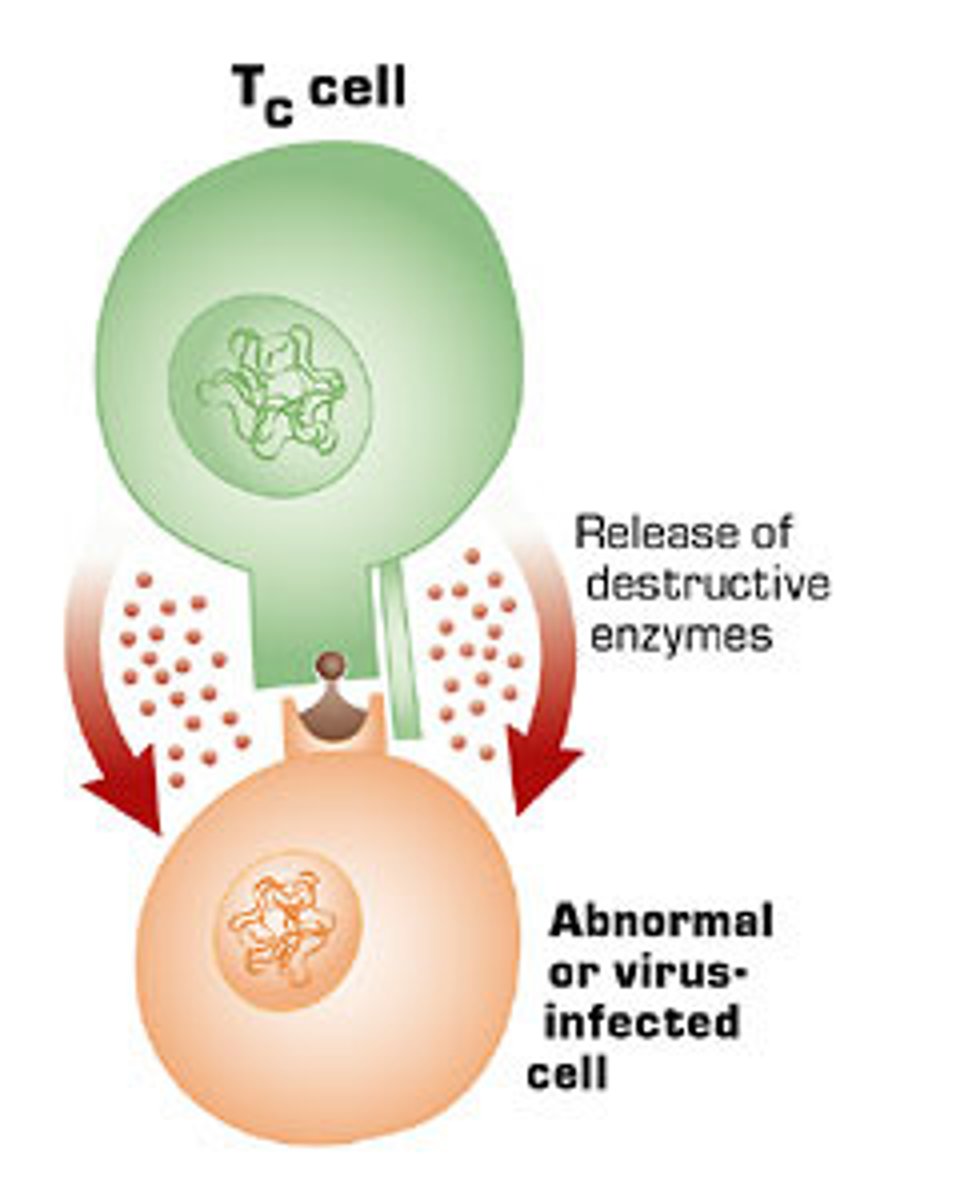
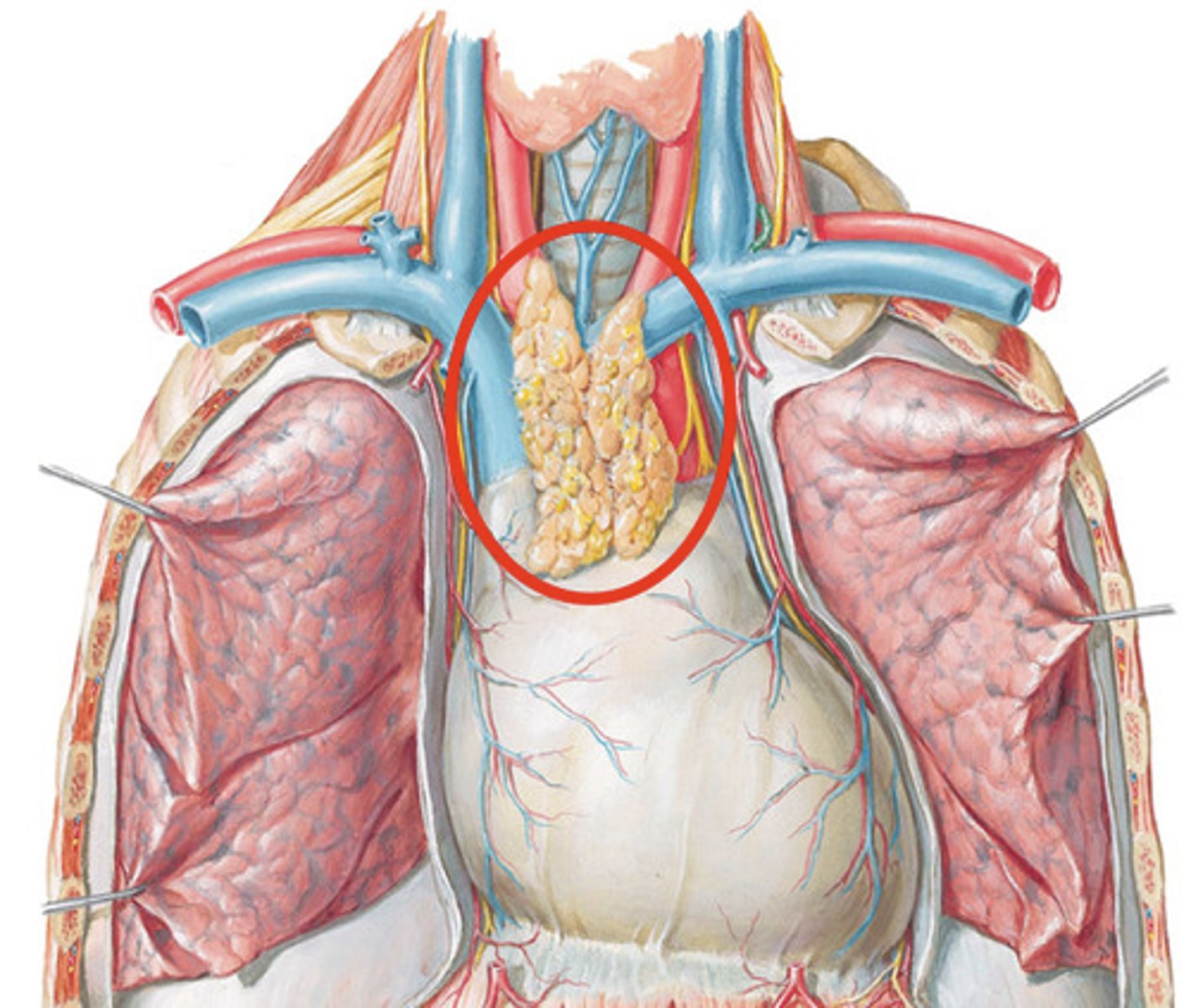
T cells
A type of lymphocyte that is created in the thymus; produce substances that attack infected cells in the body, provide acquired immunity
CD8 T cells
Cytotoxic T cells
A type of effector T-cell; they target and kill invading pathogens and cancer cells
CD4 T cells
Helper T cells
A type of effector T-cell that, when activated, stimulates activity of B cells and cytotoxic T cells, help plasma cells produce and secrete antibodies

Memory T cells
A T cell that remembers antigens and quickly stimulates the immune response upon re-exposure
A crow never forgets.

Natural Killer (NK) cells
A type of lymphocyte found in the blood/lymph nodes/spleen --> they kill cancer cells and cells infected with viruses (innate immunity)

What enzymes do NK cells secrete?
perforins and granzymes
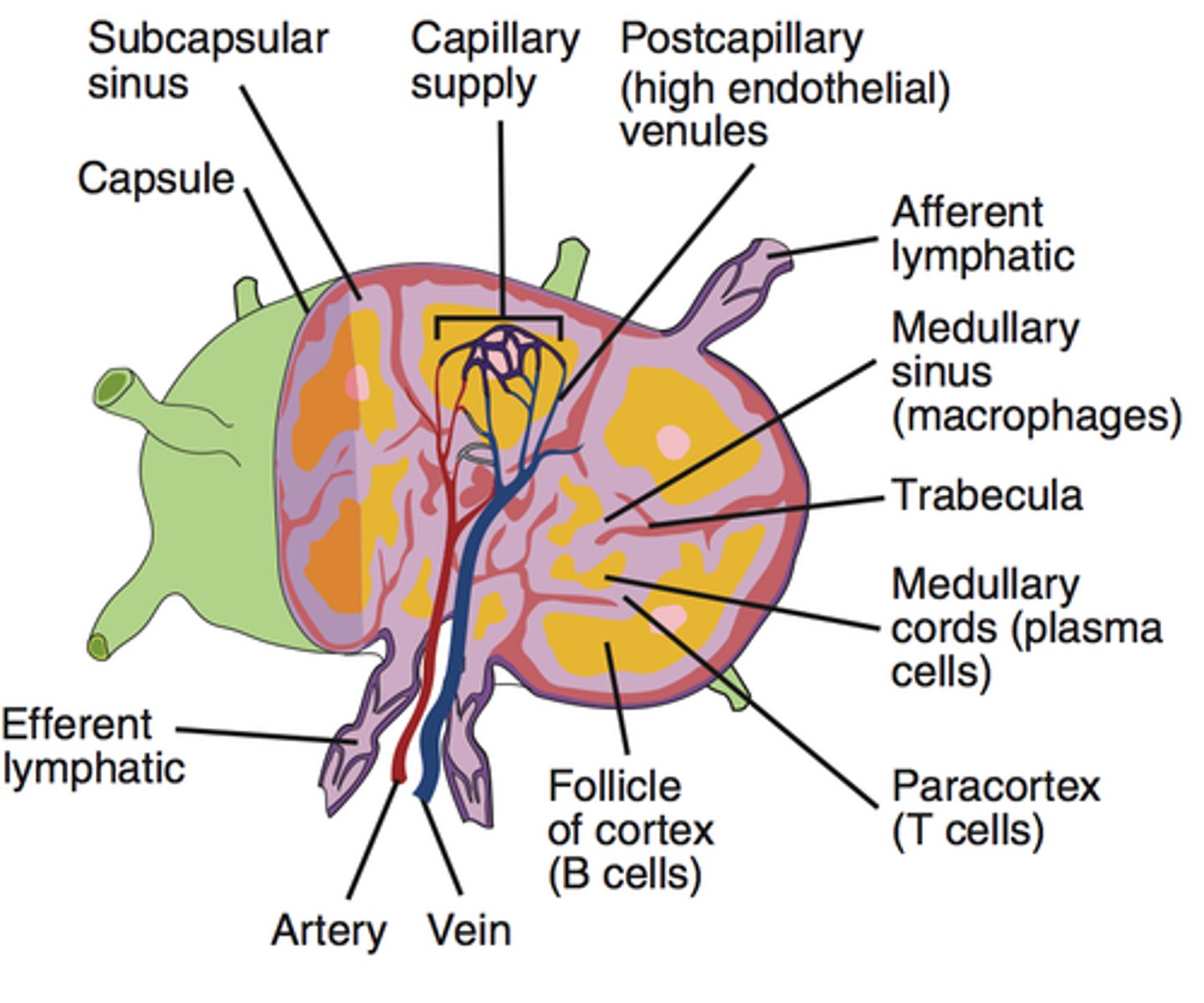
Lymphoid tissues
organized structures that support the immune system
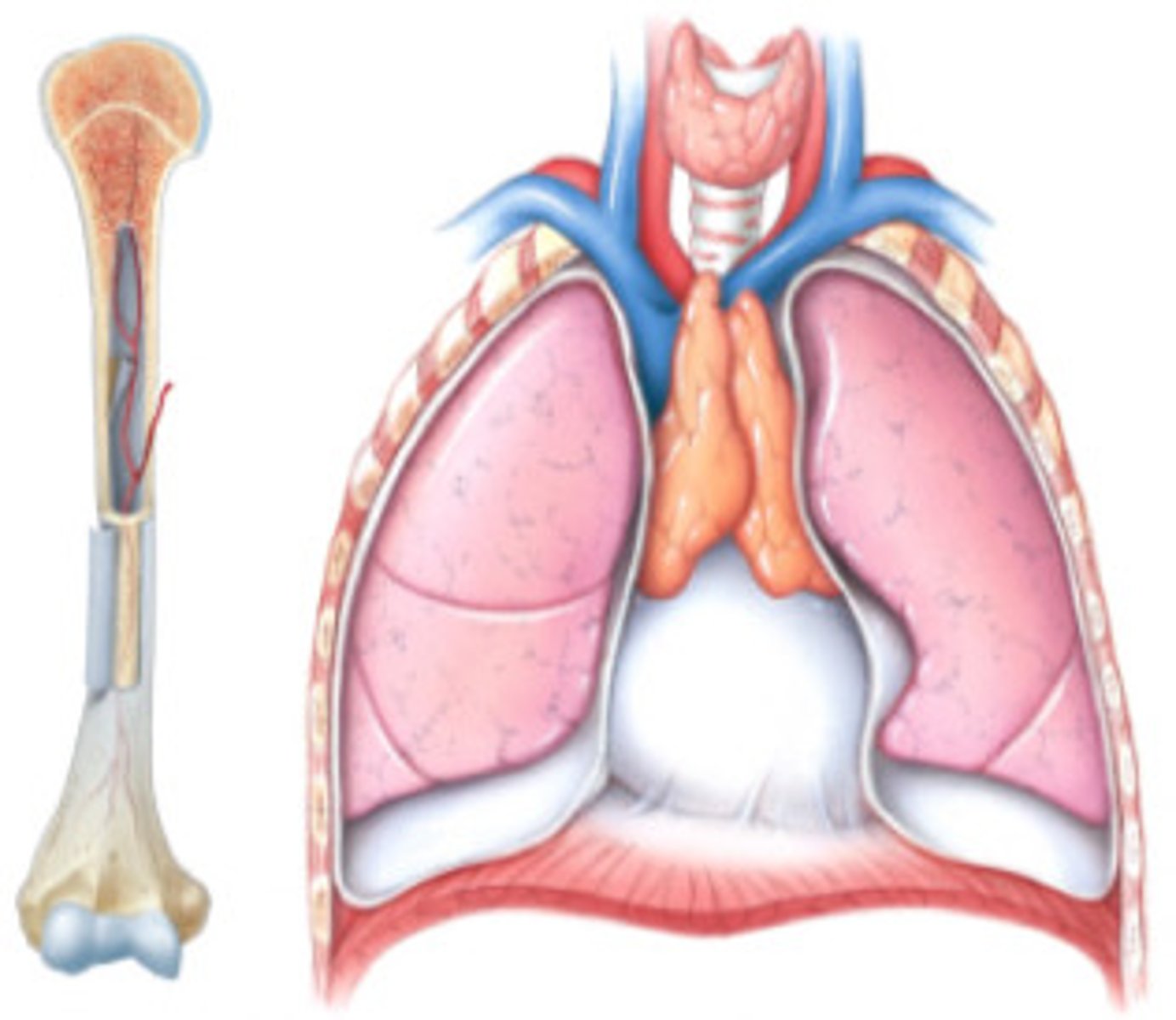
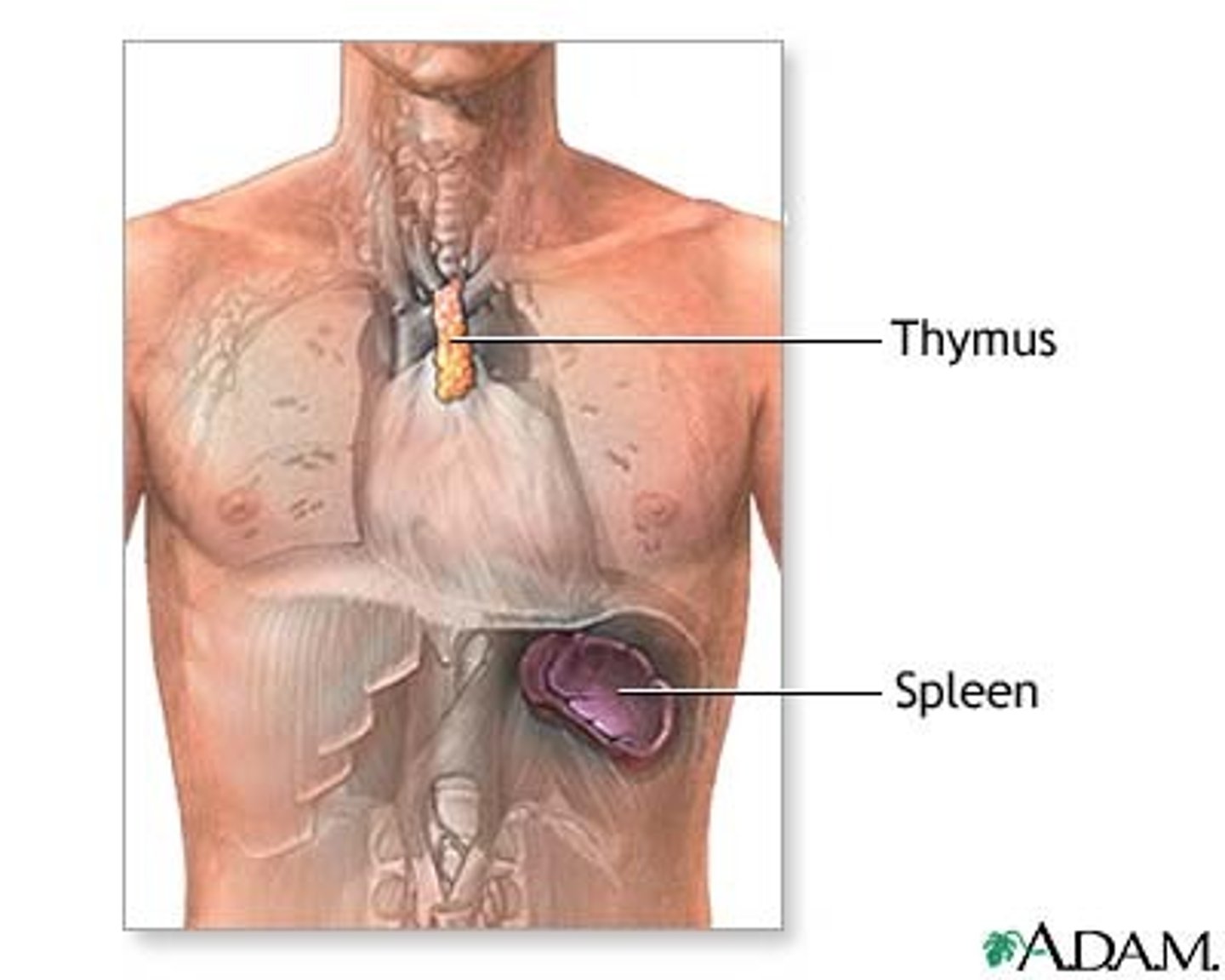
Central (primary) lymphoid tissues
where lymphocytes are formed and mature, bone marrow and thymus
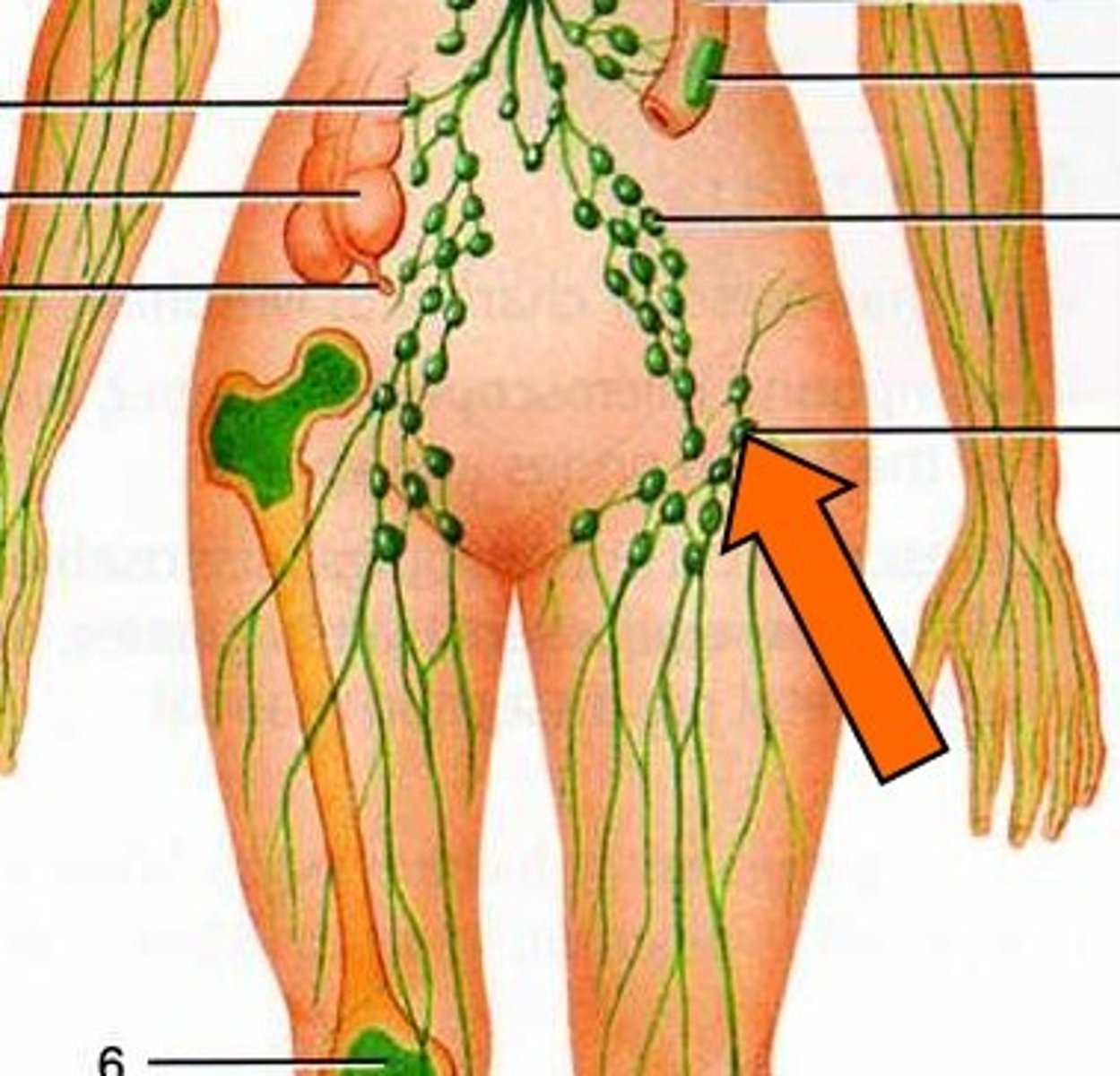
Peripheral (secondary) lymphoid tissues
where lymphocytes are activated by antigens, lymph nodes, spleen, and mucosa-associated lymphoid tissue (MALT)
What does the bone marrow do?
Produces blood cells
What does the thymus do?
Site of T cell differentiation and maturation
What do the lymph nodes do?
Filter lymph --> trap pathogens for destruction by white blood cells
What does the spleen do?
Filters blood and removes damaged blood cells --> THE RED BLOOD CELL GRAVEYARD
Red pulp vs white pulp
white pulp has B cells and T cells, red pulp has venous sinuses that filter blood by removing pathogens and senescent erythrocytes
Mucosa-associated lymphoid tissue (MALT)
Lymphatic tissue without a connective tissue capsule (salivary glands, eyes, breast tissue)

Non-neoplastic
Not cancerous
What kind of non-neoplastic leukocyte disorders are the most common?
Those that involve neutrophils and lymphocytes
What kind of non-neoplastic disorders are the least common?
Those that involve monocytes, eosinophils, and basophils
Neutropenia
Abnormally low number of neutrophils
Neutropenia etiology
Chemotherapy, inherited genetic disorders, septicemia that deplete neutrophils faster than they can be produced
Neutropenia S&S
Recurrent infections, absence of pus formation at sites of infection and/or lack of inflammation
Neutropenia treatments
Antimicrobial meds, hematopoietic growth factors
Agranulocytosis
Severe neutropenia (deficiency in neutrophils appears as if there is just an elevated number of the agranular cells --> hence the name)
Neutrophilic Leukocytosis
Abnormally high number of neutrophils
Neutrophilic Leukocytosis etiology
early response to a bacterial or fungal infection, acute inflammation, certain meds, physical/emotional stress
Neutrophilic Leukocytosis treatment
Solve underlying cause of infection/injury
Invasive Candidiases
infection caused when candida albicans enters blood and circulates to organs other than skin and GI tract, treated by IV antifungal agents
Pathogenesis of Invasive Candidiasis
Immune cells (macrophages, NK cells) recognize PAMPs (pathogen-associated molecular patterns) on fungal cell walls —> Start producing pro-inflammatory cytokines (e.g. IL-1, IL-6) and GM-CSF —> GM-CSF stimulates the bone marrow to produce neutrophils
Lymphocytopenia
Abnormally low number of lymphocytes
Lymphocytopenia etiology
inherited genetic disorders, chemo/radiation, prolonged periods of malnutrition, viral infections (HIV)
Lymphocytopenia S&S
Recurrent infections, decreases in B, T, or NK cells
Lymphocytopenia treatments
Antimicrobial meds, IV immunoglobulins (artificial antibodies)
Lymphocytic leukocytosis
Abnormally high number of lymphocytes (B cells, T cells, or NK cells)
Lymphocytic leukocytosis etiology
early response to viral infection, chronic inflammation
Lymphocytic leukocytosis treatment
Solve underlying cause of infection/injury
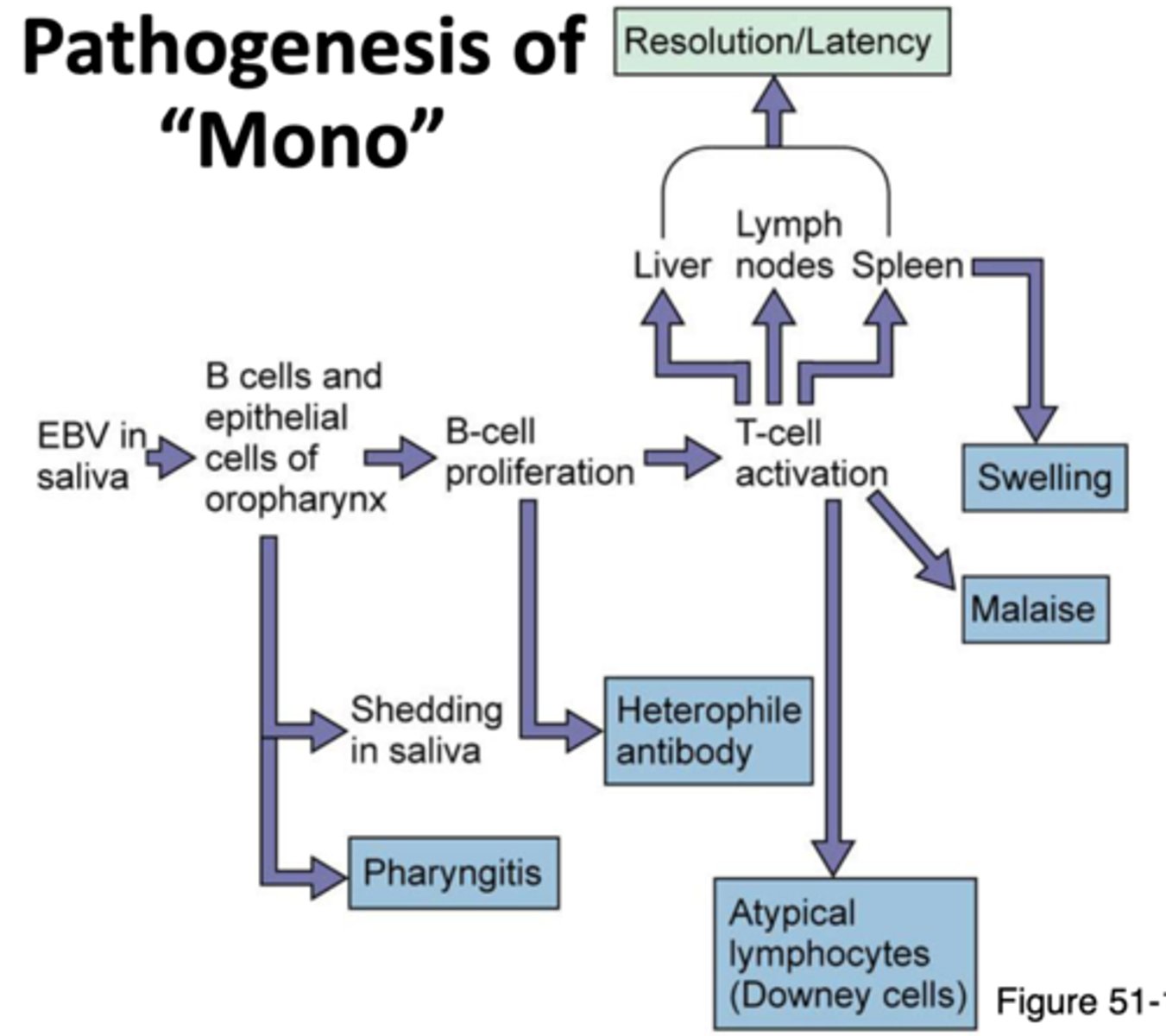
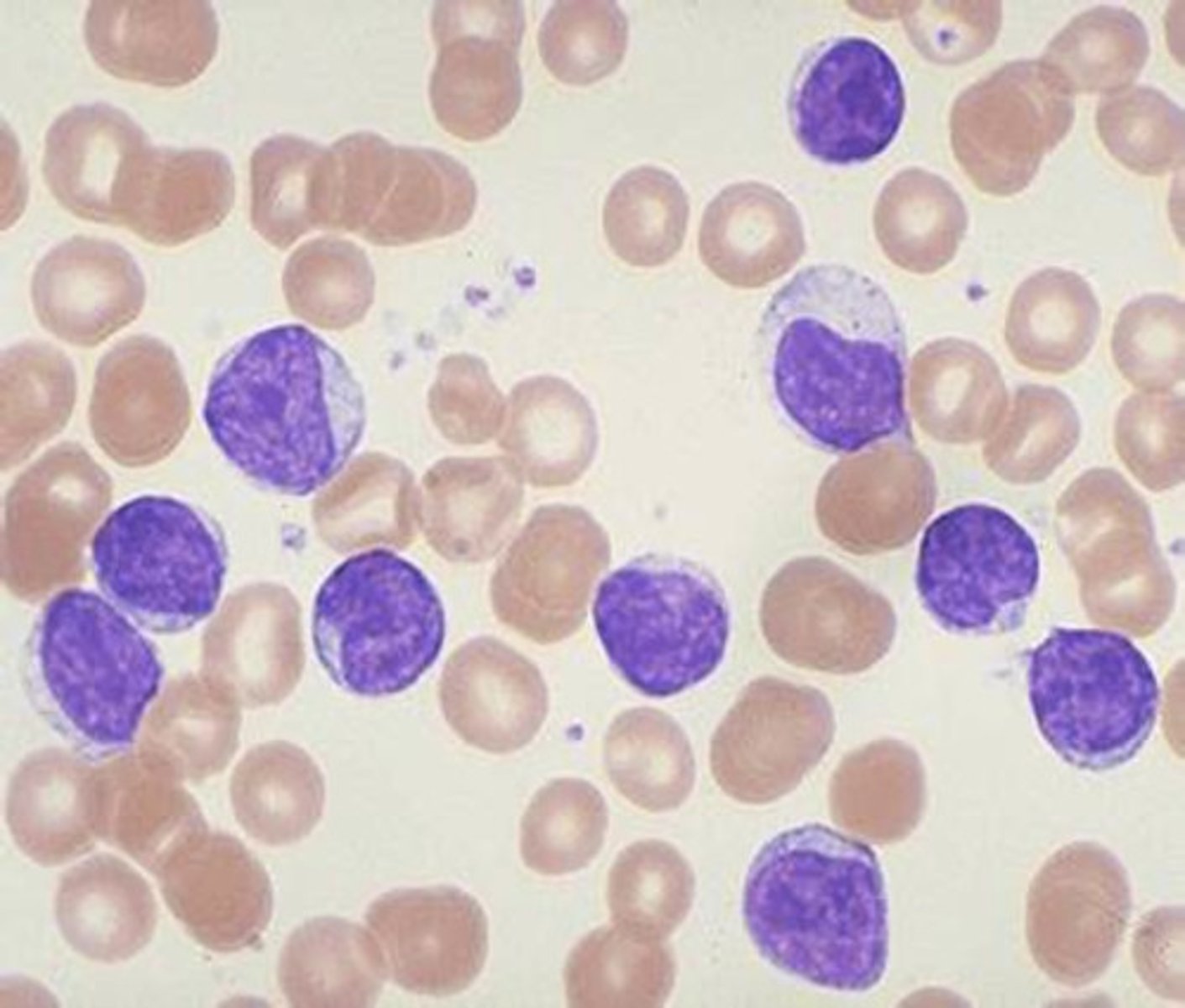
Infectious mononucleosis
Kissing disease
Sore throat, fatigue, fever, enlarged spleen, large number of BIG lymphocytes

Infectious mononucleosis etiology
Epstein-Barr virus (EBV)
Infectious mononucleosis treatment
Rest + no exercise
Pathogenesis of mono
EBV enters and multiplies in epithelial cells in mouth --> Spreads to B cells in the throat --> Infected B cells multiply --> Signs and symptoms --> Cytotoxic T cells and NK cells destroy infected B cells --> Recovery
Leukemias
Cancers of the hematopoietic stem cells in the bone marrow
Where does the name leukemia come from?
There is a reversal of the normal RBC to WBC ratio --> now more WBCS than RBCS --> "white blood"
What 2 factors are used to classify leukemias?
Based on
1. Whether they are acute or chronic
2. Affected cell type (lymphoid or myeloid)
Lymphocytic leukemia
Leukemia involving cells that originate from lymphoid stem cells
Myelocytic leukemia
Leukemia involving cells that originate from myeloid stem cells
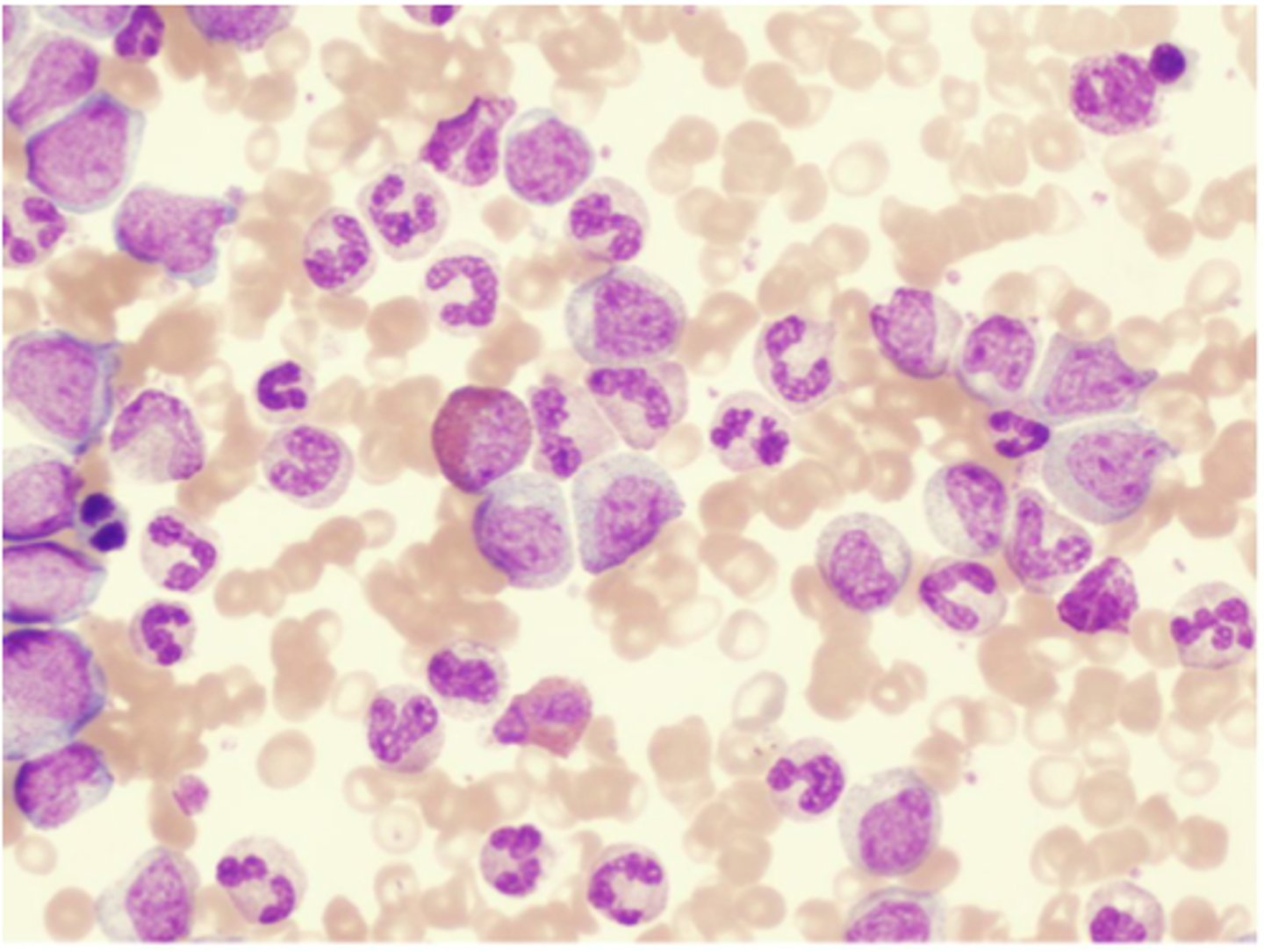
Acute Leukemias
Large numbers of immature BLAST leukocytes in the blood and bone marrow (rapid onset and progression)

Acute lymphocytic leukemia (ALL)
Acute leukemia of lymphoid stem cells that occurs in children and adolescents
Acute myelocytic leukemia (AML)
Acute leukemia of myeloid stem cells that occurs in older adults
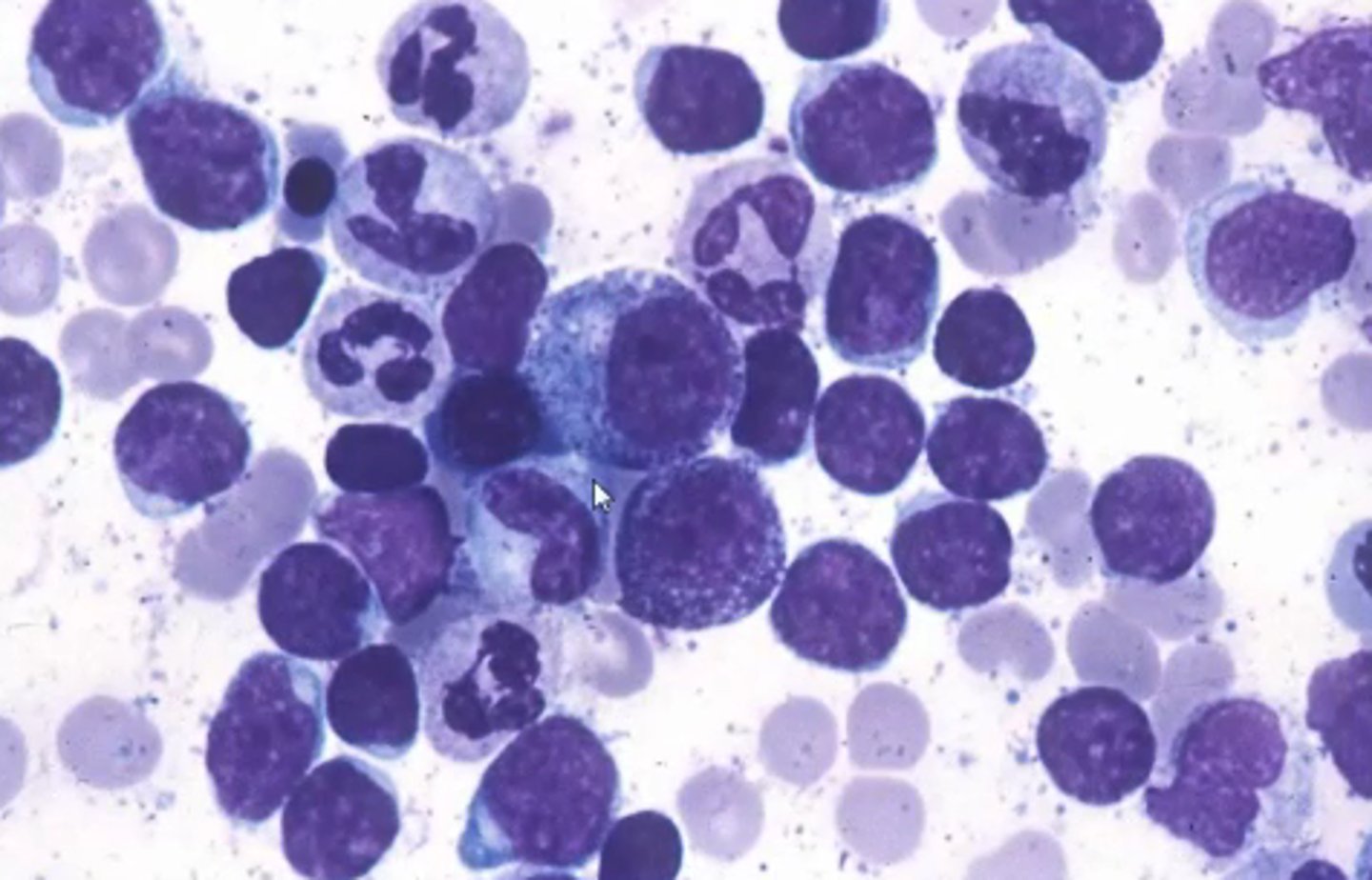
Chronic Leukemias
Large numbers of mature, differentiated leukocytes in the blood and bone marrow (slow onset and progression)
Chronic lymphocytic leukemia (CLL)
Chronic leukemia of lymphoid stem cells that occurs in older adults
Chronic myelocytic leukemia (CML)
Chronic leukemia of myeloid stem cells that occurs in older adults
S+S of leukemias
Fever, chills and night sweats, loss of appetite, weight loss, bone pain, enlarged lymph nodes, spleen, and liver

Why is fatigue a symptom of leukemia?
Anemia occurs due to the lack of RBCs --> fatigue
Why is bleeding a symptom of leukemia?
Decreased platelet count occurs due to the lack of thrombocytes --> bleeding
Why is recurrent infections a symptom of lymphocytic leukemias?
Neutropenia occurs as a result of too many lymphocytes --> more prone to infections
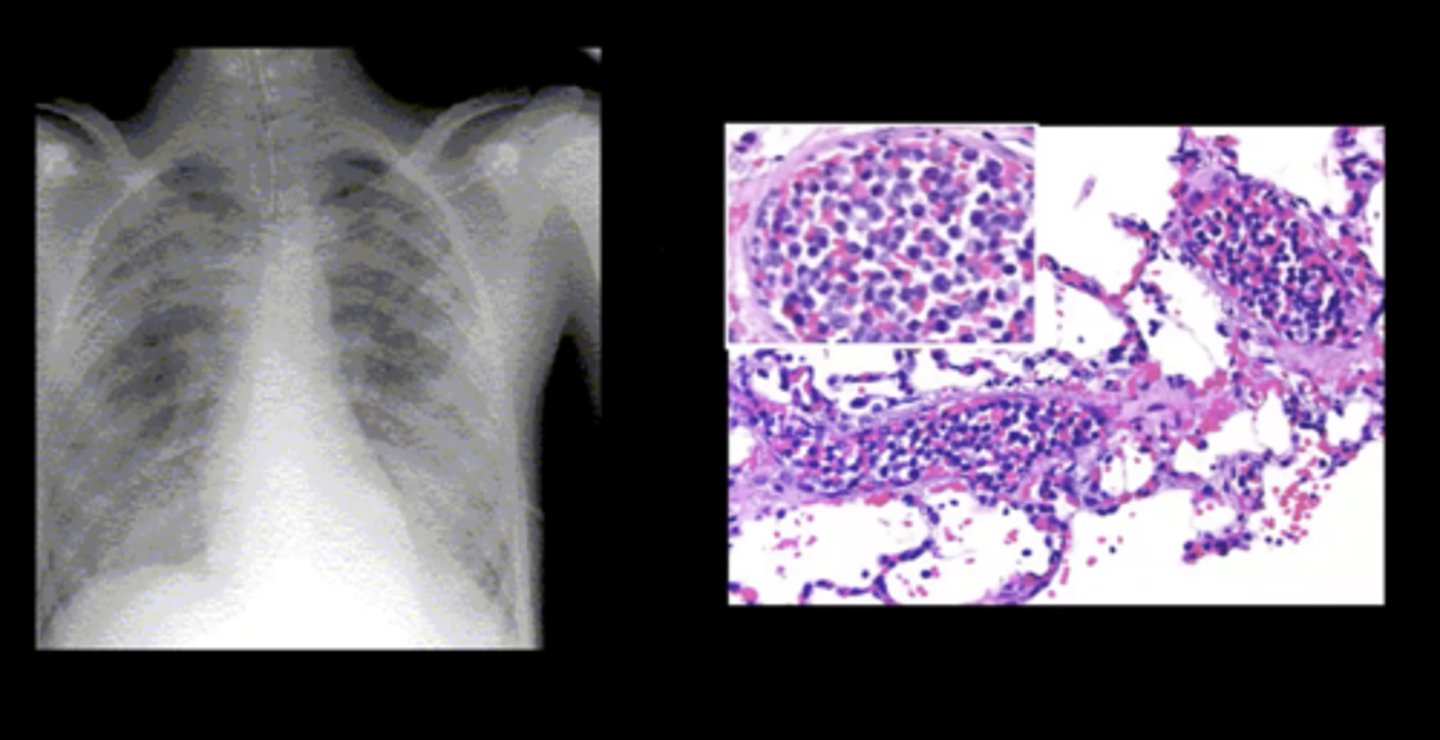
Leukostasis
Complication of acute leukemia; a severely elevated circulating immature WBC count --> blood is more viscous --> clot development
Pulmonary leukostasis
Sudden shortness of breath and progressive dyspnea; caused by a WBC clot
Cerebral leukostasis
Severe headache which can progress to confusion and coma; caused by a WBC clot
Genetic factors that increase the likelihood of leukemia
Down Syndrome --> high risk of acute leukemias
Family history --> high risk of CLL
Philadelphia chromosome --> high risk of CML
Environmental factors that increase the likelihood of leukemia
Exposure to chemicals, chemotherapy
How are leukemias diagnosed?
Leukocyte count, bone marrow biopsy, genetic tests
How are leukemias treated?
Chemo, radiation, bone marrow transplants, antimicrobial meds