Chapter 8 and Lecture 6: Diet, exercise, and obesity
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
48 Terms
The Obesity Epidemic
Since the mid-late 20th century, obesity has increased significantly (in North America and around the world)
Weight concerns prevalence
Start in childhood and adolescence.
Overweight ppl are often judged negatively by society.
Overweight in teens (esp girls) at risk for depression and anxiety disorders.
Girls' self-esteem related to weight typically declines sharply and consistently from ages 10 to 16.
The desirability of weight is judged by attractiveness and healthfulness.
Individuals who stay within certain weight ranges have lower rates of chronic illness and longer lifespans.
Obesity
Having a very high amount of body fat in relation to lean body mass, or BMI 30 or higher. (Overweight is 25 or higher)
Declared a disease by the AMA in 2013 and by the CMA in 2015 (to help them gain access to treatment)
More in developed countries (but lower SES in developed countries)
Body Mass Index (BMI)
A measure of an adult’s weight in relation to their height; weight over height (BMI = kg / m²)
Inaccuracy in defining “healthy/unhealthy” cuz it doesn’t directly measure the amount of body fat
Doesn’t work for ppl who are rlly tall or rlly short
Obesity trends among US adults
42% of American adults were obese, 73% overweight (10-19% older than 90)
No diff by sex or age
So many Mcdonalds
Obesity trends in Canada
Similar trends (but not as severe) as US
65%: 35% overweight, 30% obese (In 1978, 14% of Canadian adults were obese)
Rates of obesity highest between 55 and 64 years
Obese/overweight high across country. Highest in men: Newfoundland and Labrador. Highest in women: Nunavut
Weight gain occurs when
Calorie intake > energy spent
Excess calories are stored as fat in adipose tissue → increases in number if fat cell size becomes excessive
Reasons for adult weight gain
Accumulation of unlost weight from life events (e.g., holidays, pregnancy).
Decline in physical activity and metabolism with age
Metabolism
Fat tissue is less metabolically active than lean tissue, which contributes to continued weight gain in overweight individuals even without increased caloric intake.
Heredity/Genetics
Specific genes are linked to obesity.
Heredity is not destiny: Physical activity may overcome a genetic predisposition to be overweight (e.g., active people with the FTO gene were no heavier than others)
Set-Point Theory
The body has a "set" weight it strives to maintain via a thermostat-like mechanism in the hypothalamus. This explains why people often return to their original weight after dieting
Fat cells
The number of fat cells increases mainly in childhood and adolescence.
Too many fat cells can doom individuals to struggle against a high set-point.
When fat cells shrink during weight loss, the body responds with metabolic signals similar to starvation (increased hunger, decreased metabolism) to maintain fat stores
Central adiposity
Fat collected in the abdominal region ("rounded in the middle"), is associated with higher rates of hypertension, diabetes, and coronary heart disease compared to fat stored on the thighs, hips, and buttocks
Psychosocial factors in weight control
Emotion and Eating: Negative emotions (like stress or boredom) can induce eating.
Hunger hormone increases with stress
Cultural thing (like US), or weight gain in socially contagious (immigrate to US → eat more), larger portion makes you eat more
Comfort Foods: Foods eaten during stress tend to be sweet and high in fat.
Risk Factors: Chronic stress or depression increases the risk for binge eating and subsequent obesity.
Binge Eating: Is a common feature of individuals seeking treatment for obesity
To change a behavior effectively, you have to focus on…
Habits, not goals!
(Focus on going to sleep and waking up at the same time every day, instead of focusing on getting 8 hours of sleep)
Childhood Obesity and Prevention
Childhood obesity is a powerful predictor of adult obesity. (An obese infant = 15% chance of becoming an obese adult, an obese 10-13-year-old = 70% chance
Prevention: Preventing obesity must begin early. Parents play a crucial role by modeling and encouraging healthy eating and activity, restricting TV, avoiding food rewards, and providing healthy breakfasts
Childhood obesity Interventions (not effective & effective)
Not effective: School nutrition programs
More effective approaches: Comprehensive efforts to improve diets and physical activity, involving school cafeterias, staff, and parental cooperation.
Societal policies, such as mandating calorie labels on restaurant menus, can also encourage healthier choices.
A Systems Approach
Obesity is an end result of the intricate interactions of biology, behavior, and environment
The obesity epidemic is driven largely by environmental & lifestyle factors rather than biological ones (stressful lifestyle, high energy/fat food)
Obesity is heritable. But in most cases of genetic predisposition, risk of obesity is increased by 20-30%
Healthwashing
No regulation of the ingredient when the packaging say “natural”
How companies exaggerate the labelling or advertize products as “healthier” (ex. like diet coke — they don’t put extra sugar, but just ad to look better)
Green washing is same but focus more on eco-friendly (“composable” “eco-friendly”)
(Health washing) Food is considered healthier when…
It is labeled “low-calorie”, “organic”, or “all-natural”
It comes from a restaurant seen as healthier (e.g., Subway)
The Health Halo Effect
The tendency to judge an entire food item as healthier based on one or more narrow traits that are perceived as healthy.
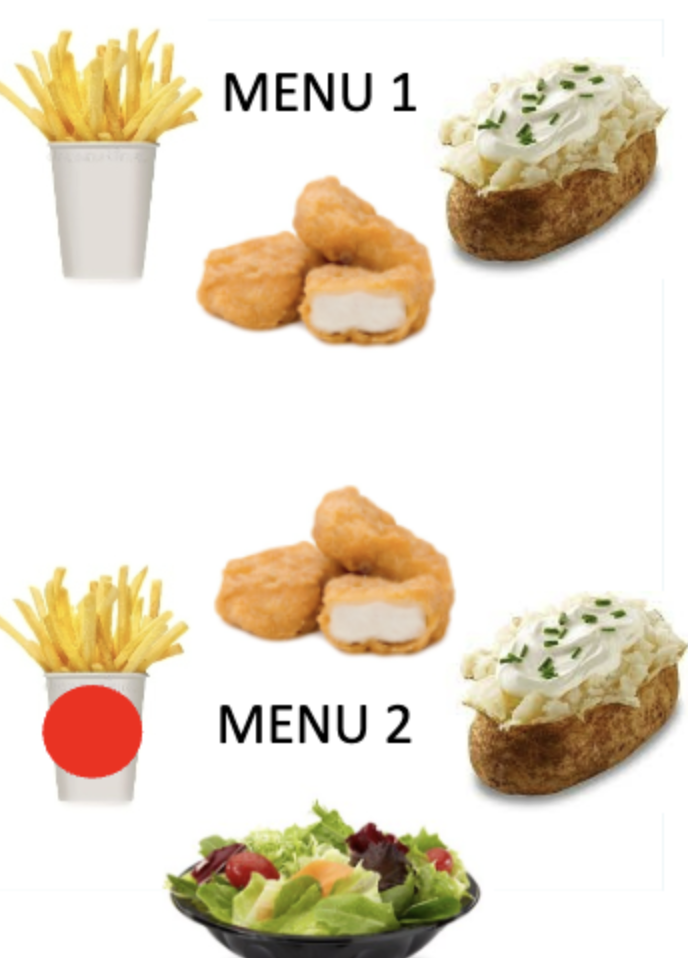
Study: Comes from a restaurant. Side as no salad option vs. there’s salad option
Individuals more likely to make indulgent food choices (ex. french fries) when a healthy item is available compared to when it is not
The more options that are given, the more likely one will go with the “status-quo” (familiar, unhealthy) option
Can be explained by
Status quo bias
Vicarious nutritional goal fulfilling
Status quo bias
People tend to stick with what feels familiar, easy, normative, or default, even when a better alternative exists
The more options, the more this bias
Vicarious nutritional goal fulfilling
“I could have had the salad… but I’ll get the fries this time.”
Simply seeing a healthy option activates your health goals momentarily. Just considering being healthy, your brain feels a small sense of moral satisfaction, as if you’ve already made progress
Community-level factors associated with higher risk of obesity...
lower SES
lower percentage of college/university graduates
lower grocery stores and farmers’ markets
lower satisfaction with safety and public transportation
lower accessibility to sports facilities
Behaviours implicated in obesity across the lifespan
unhealthy diet
physical inactivity
poor sleep
screen time
stress (cortisol)
interpersonal factors
What diet is the best
Sustainable, balanced diets that provide optimal amounts of all essential nutrients for the body’s metabolic needs
Problematic diet
Fat or “crash” diets (premature death and lower level of serotonin for ppl on low carbs diet)
Added/processed sugar appears to be more predictive of both poor health and obesity than most dietary fat
Does non-celiac gluten sensitivity exist?
2011 study: non-celiac gluten sensitivity “may exist” (ppl who believe they have sensitivity to gluten might become actually sensitive)
2013 study: There’s no such effects
2018 study: It could be Fructans (instead of gluten) that induce symptoms of gluten sensitivity
Also nocebo effect
Long-term gluten-free in adults without celiac disease (allergic to gluten) and risk of coronary heart disease
not encouraged
Avoiding whole grains/fiber is asso w higher risk of cardiovascular disease
This diet population is driven by “health halo effect”
Lifestyle Interventions for weight control: Behavioral methods
Programs, based on behavioral and cognitive methods, are highly effective.
Nutrition and exercise counseling
Self-monitoring: Keeping records of food intake and body weight
Managing environmental cues (e.g., shopping with a list).
Chewing food thoroughly
Behavioural contracting: Setting up rewards for sticking to the diet
Social support
Lifestyle Interventions for weight control: Cognitive methods
Motivational interviewing
Problem-solving training
Medically supervised methods for obesity
Self-help group
Medication: Orlistat reduces intestinal absorption of fat
Bariatric surgery: for severely obese (BMI 35 or higher w significant medical condition)
Effective in reducing weight, cardiovascular events and mortality!
Liposuction is a cosmetic procedure, not a weight loss method
Protein-sparing modified fast: Eat less than 800 cal a day (short term, quick, for severely obese)
Effective methods to prevent relapse
Only the minority who lose 5% of weight succeed in maintaining weight after years
Frequent therapist contact
Ongoing problem-solving training
Permanent low-calorie diet
Consistent exercise
Good social support
The “Health At Every Size” Approach and goals
An alternative to the weight-centered/weight control approach; focuses on weight-neutral outcomes (e.g., healthy behaviours)
Goals:
Promote size acceptance
End weight discrimination
reduce the cultural obsession with weight loss and thinness.
Some evidence of effectiveness
A factor in both weight gain and poor health; stigma predicts mortality
Numerous mechanisms, including increased stress & poor coping.
Weight stigma and anti-fat bias in health care also lead to poorer treatment and inadequate care for patients with obesity.
Internalization of weight biases interfere with weight management interventions
The solution: We need to change the attitudes and behaviours of those who stigmatize
Sedentary behaviour
Any activity involving sitting, reclining, or lying down that has a very low energy expenditure. (Bed-rotting)
May be a distinct risk factor for premature death and adverse health independent of low physical activity (they are measured differently).
Mortality is predicted by sedentary behavior itself, this measure doesn’t include low physical exercise
In other words, being highly physically active doesn’t mean you will have low sedentary behavior (sitting, lying down)
Associated with risk of depression (associated w smth like staying at home
Sedentary behavior and studies
High metabolic, cardiovascular, diabetes if high sedentary behavior
Study: Have ppl do more of unsedentary behav just 3 mins more a day (standing, walking) → greatly reduce these health risks!
Watching TV for an hour lifespan by 22 mins (on avg), whereas smokers shorten their lives by 11 mins on avg per cig
Premature death and adverse health independent of low physical activity
Depression risk
How much exercise do you need?
Adults should get at least 2.5 hrs of more than moderate physical activity each week
Ppl are more likely to be successful w any exercise program by making physical activity a permanent part of their lifestyle
Health behavior of lower SES, indigenous ppl, and other minorities
Lower rates of health enhancing behavior
Poorer health habits (high smoking, alcohol, obesity, low exercise, healthy eating)
Poorer knowledge about risk factors for disease; living in environments that do not encourage healthy behaviours; barriers to accessing health services; etc.
Eating disorders
Anorexia Nervosa: Not eating, distorted body image, high mortality (More resistant to treatment, goal is to get them to normal weight)
Bulimia Nervosa: Cycle of binge eating and purging to prevent weight gain
Affect 2% of popul in western. 90% is female
Psychological traits: Perfectionism, cultural factors (media-driven ideal female body)
Benefits of exercise
Psychosocial benefits: Lower stress and anxiety, improve cognitive processes and self-concept
Physical benefits: Slow down the natural decline in functioning, strength, cardiovascular function. Protection against premature death and other diseases
Cardiovascular benefits from exercising
BP: less risk of hypertension, lower BP
Reduce inflammation
Reactivity to stress
Barriers to exercise
Lack of time, environment (weather, no convenient place), personal (stress, fatigue, low self-efficacy), and low income & education
Activity declines sharply from adolescence to early adulthood
Key Strategies for Promoting Exercise
Pre-assessment: Determine purposes, benefits, and health status before starting.
Exercise Selection: Tailor exercises to needs and interests.
Determine where and when to exercise. Make it safe and convenient.
Specific, measurable goals in a behavioural contract.
Use reinforcement, both tangible (early on) and intrinsic (enjoyment, physical benefits).
Exercise with a partner or in a group
Record Keeping (enhance motivation)
Interventions are most effective when they are tailored specific to indv
Gets enough exercise
Exercised a lot in the past
Rural area
Childhood
Don’t rlly exercise:
Middle-age women: Underestimate their inactivity, Concern about getting old
Low activity, busy adults
Decreases in university
Strategies for starting and continuing to exercise
Pre-assessment: Health status, benefit
Exercise selection
Exercise condition: When, where you’re exercising
Goals and consequences (rewards)
High social support
Keep track
In precontemplation tends to stick w exercise
For sedantary: Frequency > intensity (so start small is better, start walking > HIT workout)
Better mental health (less depressed)
Compensatory belief
Thinking you can compensate unhealthy behaviors for doing healthy behaviors
Ex. I went to gym today, I can eat a cake
(You’re not likely to lose weight)