26. coughing
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
coughing
what is it triggered by
what is the mechanism
what is an acute vs chronic cough
what do we have to rule out when we see cough
Cough reflex triggered by stimulating cough receptors in the larynx, trachea or bronchi
Draw air into the lungs to augment force of expulsion
Different from expiratory reflex where there is NO draw in of air
Acute cough = <3wk duration
Greater than = chronic
Describe the animal’s cough, history, environment
RULE OUT CARDIAC DISEASE
canine infectious respiratory disease (CIRD, tracheobronchitis)
how is it classified
is acute
2 categories of etiology
Any contagious, acute-onset respiratory infection of dogs, typically involving upper respiratory tract
Acute and highly contagious
Etiology
Bacterial and/or viral
Synergistic infections
Viral | Bacterial |
|
|
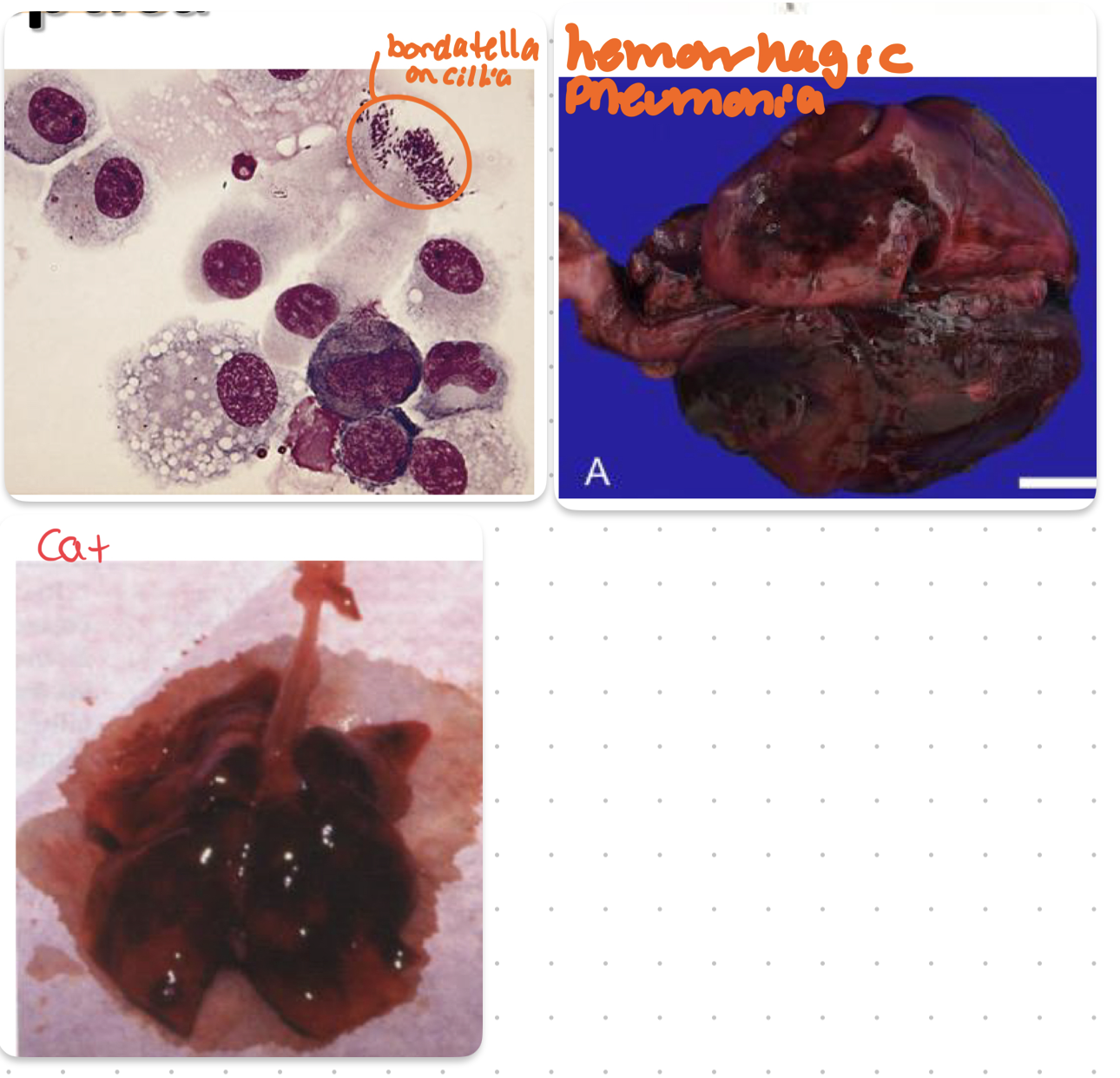
bordetella bronchiseptica
is it a commensal
what morbidity and mortality
often seen with what virus
incubation period
transmission route
hallmark clinical signs
2 major mechanisms that help it infect
how does this present in cats
Can be a normal inhabitant of resp tract
Gram negative aerobic bacillus
More commonly a ‘2ndary’ pathogen, but can
cause severe primary infections
High morbidity, low mortality
Often seen with CPIV
Incubation 2-10 days, may be shed for months
Variable presentation: mild upper-respiratory signs, to severe
bronchopneumonia
Transmission via inhalation/airborne route, highly contagious
CS: Dry paroxysmal cough, nasal discharge;
In severe cases: depression, pneumonia and death
Mechanisms
Unknown stimuli can lead to bacteria attaching to and
colonizing respiratory epithelium
Initiates ciliostasis
Express exo/endotoxins to promote cellular injury & bacterial survival (lipopolysaccharide, adenylate cyclase haemolysin, dermonecrotic toxin, tracheal toxin)
Adhere to respiratory cilia via adhesins(fimbriae, filamentous hemagglutinin, pertactin)
Cats
Can be a primary pathogen in cats!
Incidence: Overcrowding, stress, age
More upper respiratory signs in adults
Sneezing, nasal discharge
May progress to dyspnea, cyanosis, death especially in kittens
Can transmit dog → cat
mycoplasma
pathogenic species
commensal species
what does this lack
where does it colonize
how is it transmitted
how long does it persist
Many Mycoplasma spp are commensal
Likely a pathogenic role of M. cynos and a commensal role of M. canis and M. edwardii in lower respiratory tract in dogs
Lack a cell-wall, fastidious
Colonizes ciliated & non-ciliated epithelium
Genital, GI, resp
M cynos can persist in lungs for 3 wks following infection and be transmitted via aerosols
Streptococcus equi subsp zooepidemicus
how do dogs get it
what is hallmark CS in dogs
β-hemolytic, Lancefield C streptococcus
Contact with horses has been identified in some, but not all infected dogs
Acute, severe bronchopneumonia in dogs
Initially mild signs, progresses rapidly over 24-48 hours
Severe, fibrinosuppurative, necrotizing, hemorrhagic bronchopneumonia
Disease course may be similar to strep. exotoxin-induced toxic shock syndrome in people
Overexuberant immune response from pyrogenic exotoxins = superantigens?
TNF-a, IL6,8 → necrosis and hemorrhage in lungs
Lungs from infected dogs had much higher mRNA levels of proinflammatory cytokines than controls
viral etiologies of coughing (6)
canine parainfluenza
canine adenovirus 2
canine coronavirus
canine influenza H3N8
canine influenza H3N2
canine distemper
canine parainfluenza
what are 2 key features of this virus
shedding period
what is hallmark CS
Paramyxoviridae, enveloped RNA virus (disinfectant works)
Most common viral isolate of CIRD
Very contagious; sheds 8-10 days
Pure viral - mild signs; high pitched ‘honking’ cough from vocal fold swelling (dry, stridor)
Does not survive well in environment
canine adenovirus 2
incubation period
where do we isolate it from
generally CS
can it survive in environment
Adenoviridae, non-enveloped double-stranded DNA virus
Incubation: 1 week
Frequently isolated in upper respiratory disease
Mild signs; usually with other agents
Very contagious, survives in environment for months
canine coronavirus
is it attached to CIRD
is it similar to the enteric form
species specific?
Enveloped RNA virus; Coronaviridae
No evidence it is a primary CIRD pathogen (usually secondary)
First detected in UK in 2003
Now identified in US and worldwide
Different than the enteric virus (enteric is more common)
Species specific
Signs typically mild; strains can mutate
canine influenza H3N8
what are general signs
what percentage are asymptomatic vs fatal
incubation period
viral shedding period
2 methods of dx
First identified in Greyhounds in 2004 -horse origins
Now recognized in many states and many dogs – community acquired (breeding)
CS: upper respiratory disease – cough, nasal discharge
Up to 20% are asymptomatic; 1-5% may have fatal hemorrhagic pneumonia
Incubation is 2 – 4 days
Virus shedding 7 – 10 days
CS: Cough, nasal discharge, bronchopneumonia (< 20%)
Dx
Paired serology
virus detection by PCR (nasal swabs); should be done early in disease
canine influenza H3N2
what animal did it OG effect
where was it discovered
Identified first in 2007 in South Korea
Mutated avian influenza virus that has now adapted to the dog
Identified in USA in 2015
how to treat and prevent canine influenza
how long in environment
prevention
what is tx
what should we not use
Tx: very contagious
Supportive care
Virus persists in env. 2 days
Prevention: vaccine available
Oseltamivir (tamiflu) not been investigated, not recommended
canine distemper
what family
is it enveloped
what is infection and disease rate relative to reach other
what percent are subclinical and clear it
when is incidence highest
what age has it more severe
Morbillivirus, family Paramyxoviridae
Single negative stranded RNA, enveloped
Infection rate > disease rate
Approximately 25 - 75% of susceptible dogs are subclinically infected and clear
Temporal infection: high incidence in winter
Puppies are more severe dz than older dogs
canine distemper transmission
2 methods of spread
what is the main way
how long is it excreted post infection
what 3 factors that determine infection
Spread by aerosol: contact between animal is main method of spread
Excreted up to 60 - 90 days post infection
Don’t forget about racoons
Direct
Indirect (hygiene)
Factors:
Infectious dose
Strain virulence
Host defenses
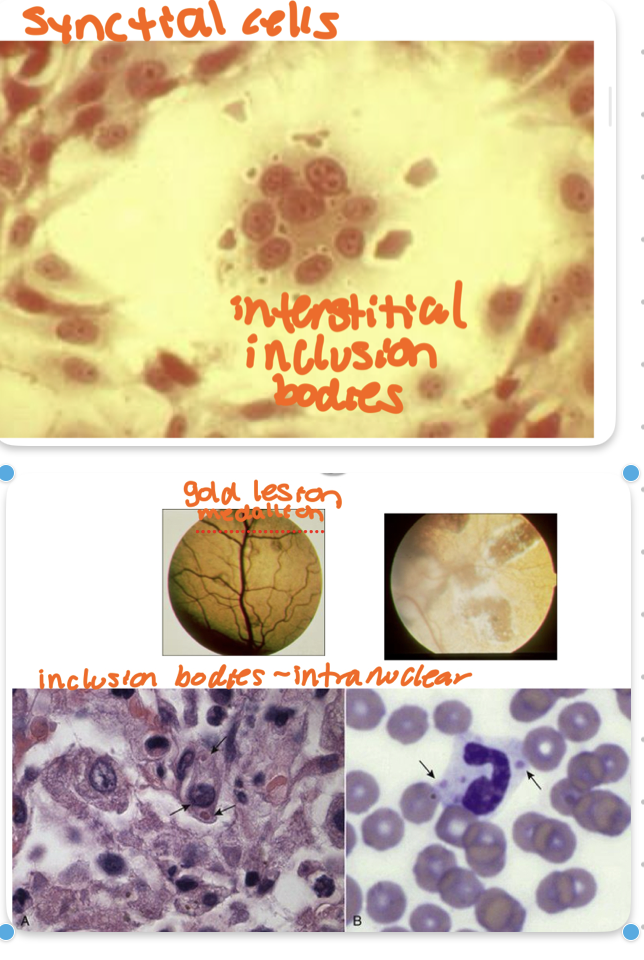
canine distemper CS
what 4 organ systems does it affect
what 2 diseases is it often confused for
what is the 2 hallmark signs
what do you see on histopath
what CS = poor prognosis
Respiratory tract is not the primary target of CDV
Varies with virulence of strain, age of host, immunocompetence, body systems affected
Neuro, GI, upper resp, conjunctivitis (eye)
Vx against CDV was associated with lower risk of CIRDC and severe respiratory signs.
Many can be subclinical
Confused with kennel cough and sometimes parvovirus if GI signs predominate
Syncytial cells predominant + interstitial inclusion bodies
Severe systemic infection
Most common in puppies
Initial fever, depression, anorexia
Conjunctivitis, cough
Vomiting/diarrhea/dehydration
Sudden death
Pneumonia
Neuro
chewing gum seizures, myoclonus
Poor prognosis

canine distemper dx
what do you see on fundic exam
what do see on histopath
what are 2 testing methods we use in combo to dx
what globulin do we want to see to dx
CS
Ophthalmologic exam
Gold medallion lesion
CBC, biochem
Intranuclear inclusion bodies
Radiology? - not pathognomonic
Serology - IgG & IgM
IgG - more vx
IgM - acute and will rise and fall
+ PCR - urine
Positive for unknown amount of time post vx
Virus isolation - difficult, more for research
canine distemper tx
main thing you should do to prevent spread
how do we prevent disease
how do we treat symptoms of canine distemper
what vx should we use and not use
ISOLATION
Supportive
Tx secondary infections
Nutritional support
Seizures - anticonvulsants
Maternal immunity - colostrum
Modified live vx or recombinant
Attenuated live → encephalitis if immunocompromised and <6 wks age
CDV involvement in CIRDC rare due to vx
uncomplicated infectious tracheobronchitis (CIRDC) clinical findings
incubation period
hallmark CS
duration of dz
tx
Usually a mild self-limiting disease
All ages susceptible
Incubation: 3 - 10 days
Dry, harsh, non-productive cough +/- discharge
Duration: 7 - 10 days (or longer)
No other clinical findings
Tx: supportive care
complicated infectious tracheobronchitis (CIRDC) clinical findings
what age group affected
hallmark CS
what do you seen on rads
duration
is it severe?
tx
Young puppies, immunocompromised
Productive cough → pneumonia
Fever, depression, anorexia
Naso-ocular discharge
Thoracic rads: signs of infection
Lasts 1 - 3 weeks, may be fatal
Tx: antibiotics if bacterial
dx of infectious tracheobronchitis (CIRDC)
what does bloodwork look like
when do we do C&S
what samples do we submit
when do we consider PCR and serology
History of exposure?
May have normal blood work and radiographs
Culture and sensitivity (TTW, ETW)
usually done in complicated cases
Nasal swab bacterial culture is not representative of 1º etiology
Submit all samples: conjunctiva, thorat, nose
PCR panels: interpret and use with caution, serology +/-
Consider if rapid progression, CS > 10 days or outbreak
tx of infectious tracheobronchitis (CIRDC)
does everyone needs antibiotics
what 2 drugs could potentially be helpful
collar or harness
how long does bordetella shed
how long is bacterial CIRDC course
Complicated or uncomplicated?
Treat specific infection
Bordetella or Mycoplasma cynos?
Not everyone needs antibiotics!!!
Humidify air
Cough suppressants +/-, Bronchodilators +/- (can be helpful)
Rest/ no collars (harness)
Isolation for at least 2 weeks
Shedding of bordetella: at least a month and sometimes several months
Bacterial CIRDC CS resolve quickly (1-2 wks)
Prevention of infectious tracheobronchitis (CIRDC)
what vaccines are core
what vaccines are non-core
what to avoid in the environment
Avoid contaminated areas
Decrease stress and overcrowding
Vx
No vx completely prevents disease
Maternal antibodies present
Core vx
DA2PP
Rabies
Non-core
Bordetella
Canine influenza (H3N8/H3N2)
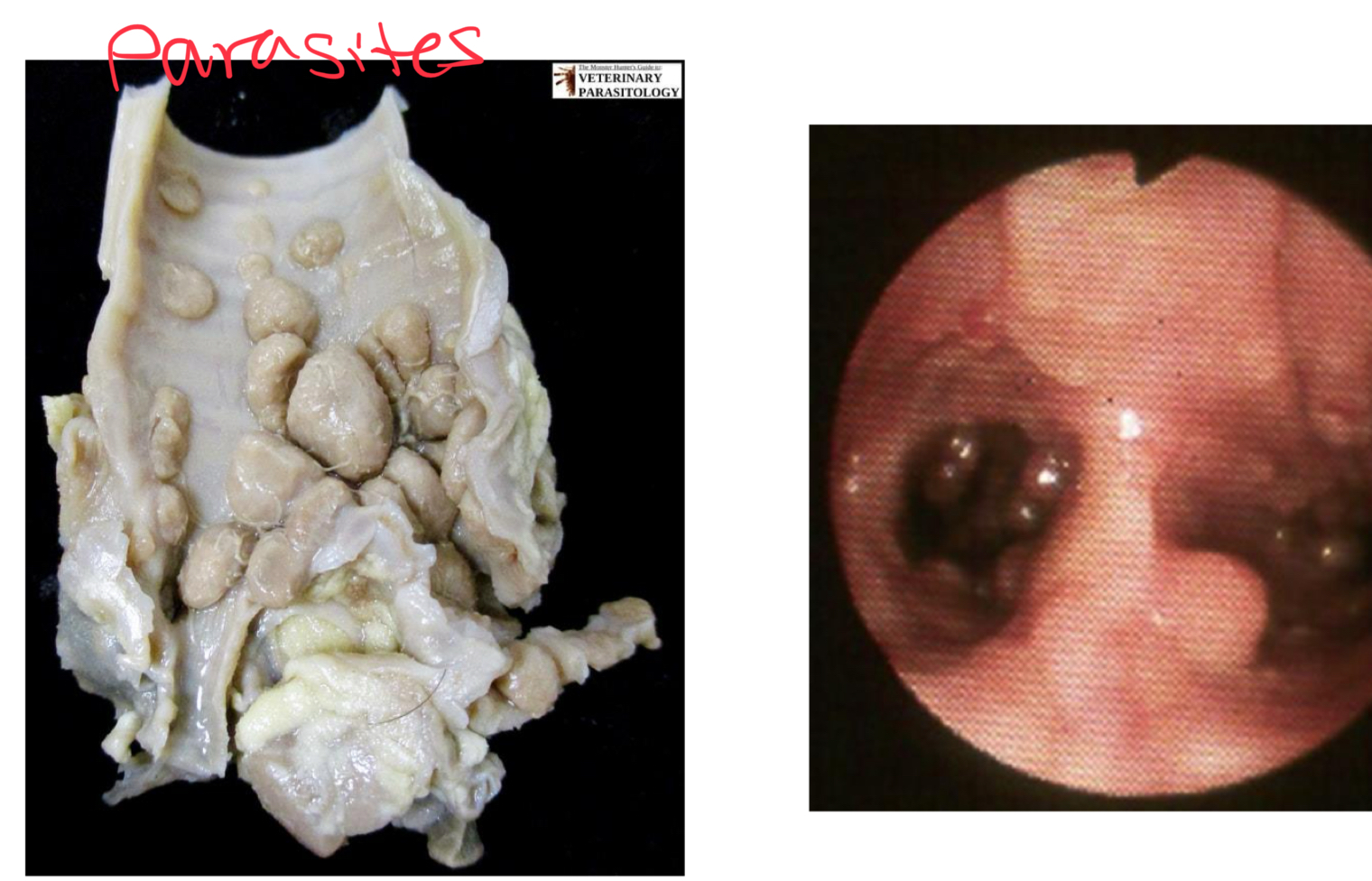
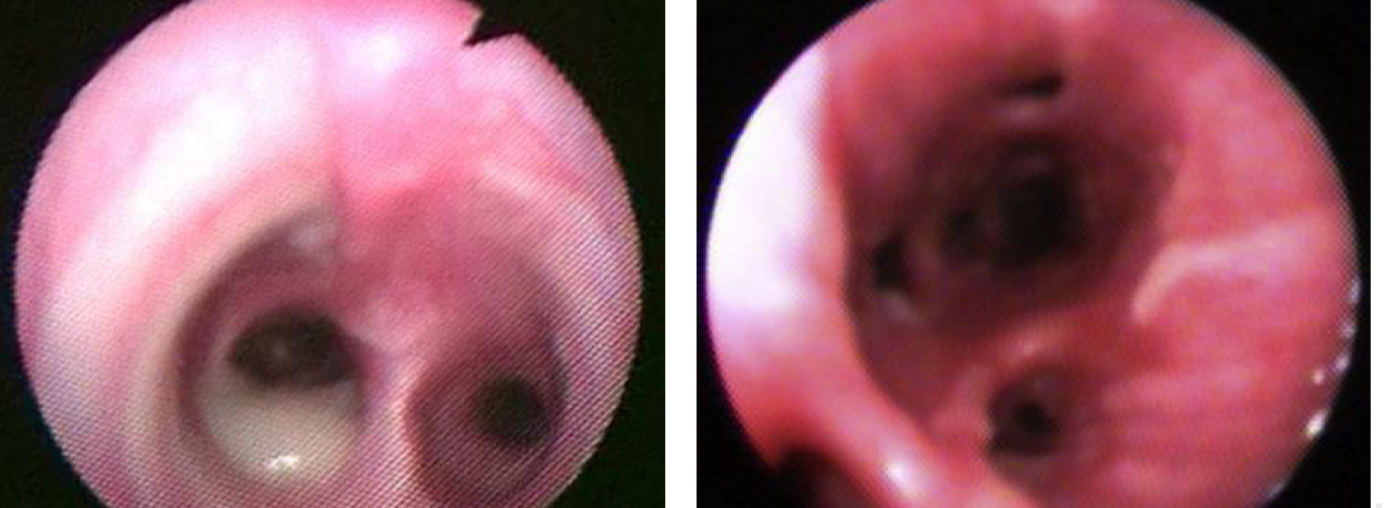
3 Etiologies of upper respiratory coughs
Parasitic
Filaroides osleri
Crenosoma vulpi
Capillaria aerophilia
(aka Eucoleus aerophilus)
Dx: baermann (not 100%)
Tx: prophylactically
Foreign body
Rocks, toys, grass awn, teeth
Irritant
Chemical (bleach)
mechanical
chronic bronchitis in canines
what is hallmark resp sign
what can we auscultate
7 etiologies
Incurable with insidious onset
Chronic and persistent cough
No identifiable or persistent primary cause found
Syndrome not necessarily a final dx
PE:
Normal BCS (usually)
Auscult wheezes, crackles, and increased airway
Persistent cough often with terminal retch (gag) often the primary complaint
Etiologies
Defect in muco-ciliary function
Airway parasites
Infections (previous damage)
Kennel cough
Inhaled irritants
Smokers, air freshener
Allergy
Aerodigestive disorders
Inhale stomach acids from primary GI dz
5 differential dx for chronic bronchitis
what must we rule out
which one is regional
Left atrial enlargement
MUST RULE OUT CARDIAC DISEASE
Heartworm disease
Collapsing trachea
Neoplasia
Fungal → SE
dx of chronic bronchitis
it is a diagnosis of ____
what dx is typically normal
what is a more objective test
what rad pattern do we see
what might we see on washes
what makes prognosis worse
Diagnosis
Exclusion of all potential primary or secondary causes = frustrating & inconclusive
Rule out contributing dz
Baseline bloodwork; typically normal, but pay attention to eosinophilia
Fecal for lungworms (baermann), heartworm testing
Arterial blood gas and pulse oxygenation
6 minute walk test < 400 m = sick
Consider pet lifestyle and environment as potential triggers
Rads
Prominent bronchial structures (donuts, tramlines)
Interstitial infiltrate
Bronchiectasis
Rubbery and blown out
Secondary
Overall not super specific
TTW, ETW
Inflammation - neutrophils and mucus
Culture, +/- bacteria (lungs are not sterile)
Bronchoscopy
Collapse of intrathoracic airway has worse prognosis
4 tx goals for chronic bronchitis
Reduce inflammation
Limit cough
Improve exercise stamina
Slow progression of disease and reduce airway remodeling
6 tx for chronic bronchitis
is this curable
what is a first choice abx
Reduce env. Contamination
Smoking, scented candles/cleaners
Avoid dog parks, groomers, public areas to reduce infectious disease contribution
Reduce obesity and modify behaviors
Consider consult nutritionist
Harness instead of collar, curtail excessive barking (anxiety tx)
Corticosteroids
Anti-inflammatory
↑ receptor sensitivity to beta-agonists
↓ sensitivity to allergens
Inhaled glucocorticoids can be effective
Fluticasone
Oral → wean oral start inhaled → wean both
Aerodog
Bronchodilators
Antitussives - judgement call
Antibiotics
Suspect concurrent infection
Reserve for acute exacerbation, infectious encounters
Doxycycline and azithromycin = reasonable 1st line choice
Various therapies necessary for control (lifelong) - not curable
Signs may wax and wane and therapeutic adjustments will be necessary
7 ways to treat a cough
cough suppressants
antitussive therapy
hydrocodone
maropitant (cerenia)
neuromodulators
mucokinetic drugs
antihistamines
indications and contraindications for cough suppressants
Indications:prevent coughing
When nonproductive, exhausting, painful or potential for lung damage
Contraindications:
Cough defense mechanism is very important
Productive cough?
The cough is needed to remove possible infectious fluids and secretions from lung
4 drugs that make up antitussive therapy
Central acting - narcotics
Hydrocodone (#1), butorphanol, lomotil, atropine
Dextromethorphan - not really central
NMDA receptor antagonist
Maropitant +/-
Substance P inhibitor
Bronchodilators
hydrocodone
often combined with what other drug
2 atropine effects
Hydrocodone combined with atropine (homatropine)
Atropine does exert significant effects (vagal suppress = bronchodilation)
Atropine limits dosing, so discourages abuse
Suspected action is based on binding to 𝜇-opioid receptor
maropitant
what receptor does it act on
what binds to that receptor
what 3 effects does it have on bronchial epithelial cells
is it suitable for chronic canine bronchitis
NK1 receptor antagonist
Substance P (SP) is a potent NK1 agonist, maropitant is a SP inhibitor
SP from immune cells can induce bronchoconstriction, chemotaxis, and neutrophil adhesion to bronchial epithelial cells
Perceived clinical improvement but not decrease airway inflammation (not suitable tx for CCB)
neuromodulators
2 examples
for what type of cough
Gabapentin, amitriptyline
Chronic, idiopathic cough
Sensory neuropathy, laryngeal irritability
Optimal dose, length, true benefit not yet determined
mucokinetic drugs
mechanism
2 examples
Help eliminate resp secretions by changing viscosity
Acetylcysteine
Destroys mucoprotein disulfide bonds, creates smaller, less viscous molecules
Antioxidant properties
Administered via nebulization – this can lead to bronchospasm in cats (avoid) - good for dog
Guaifenesin
antihistamines
indicators
mechanism
May be useful if cough is suspected to have allergic component
Direct effects occur by blocking H1 receptors in the central and peripheral nervous systems
Indirect effects include reduced mucus secretion and sedation
coughing in cats
are cats specifically treated for cough
what is often the underlying pathology
what does it resemble
Not as common as dogs
Cats not tx specifically for coughing
Often caused by chronic lower airway inflammatory dz (paroxysmal coughing, resembles coughing up hairballs)