Body Fluids
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
State the time frame for testing a body fluid, and how body fluid specimens are stored.
Processed within 4 hours
body fluids are stored in the Micro fridge for several days
State how to process a body fluid, list reasons why the test might need to be cancelled, and list the frequent testing done on body fluids.
mix well
observe for volume, clots, mucus, consistency
fluids are observed for color and clarity, have cell counts done, and evaluate the WBCs present
fluids often have chemical exam and cultures done
Define CSF. Name the functions of CSF, where it is produced and function of the blood brain barrier.
clear, colorless fluid that surrounds the brain and spinal cord
produced by the choroid plexuses in the brain
used to evaluate the central nervous system
functions
cushion for brain
lubricant for CNS
supplies nutrients and removes waste
Name the procedure used to collect CSF. List indications for collection, and which tubes are used for each area of testing
procedure: lumbar puncture
indications
CNS malignancy
demyelinating diseases
meningeal infection
subarachnoid hemorrhage
Collection (4 tubes)
1: send outs
2: chemistry
3: microbiology
4: hematology
Describe what normal and abnormal CS looks like and correlate what conditions it may indicate.
Normal: clear and colorless
Abnormal: cloudy or hazy
WBCs or RBCs
increased lipids and proteins
microorganisms (infection)
Blood
Traumatic tap: contaminated with blood by a nicked vessel
Subarachnoid hemorrhage: leakage of blood from vessels to spaces inside the body
Define traumatic tap, hemorrhage, and xanthochromia. Describe how to differentiate between a traumatic tap and hemorrhage
Traumatic tap
lumbar puncture contaminated with blood by a nicked vessel or vertebrae
blood concentration will decrease across 4 tubes
clear, colorless supernatant
clotting
Hemorrhage
the leaking of blood from blood vessels to spaces inside the body
yellowish/pink
uniform bloodiness
no clotting
xanthochromia
yellowish discoloration
Explain how RBCs are counted (when automated count is <1000 cells/uL). List the equation and be able to calculate total RBCs using a hemocytometer.
RBCs initially counted by the sysmex
if <1000 then you use hemocytometer'
Calculated RBCs = (average number of cells counted x dilution) / (squares counted x 0.1) = cells/uL
Ex: sample not diluted, first count was 22 RBCs and second count was 24 RBCs. answer ~ 26 cells/uL
Hemocytometer
10uL injected to each side
placed in humidity chamber 5-10min
both sides need to be counted and match within 10%
List the normal range of CSF protein. List causes of elevated and decreased total protein .
15-45 mg/dL
Abnormal values may indicate
disruption or permeability to the blood-brain barrier
increased production or metabolism due to pathological conditions
Elevated
meningitis
hemorrhage
Decreased
CSF leakage/trauma
recent puncture
Name an excellent indicator of the blood brain barrier.
Albumin
<9 = no impairment
Describe how glucose enters CSF and the normal values. List reasons for increased and decreased CSF glucose.
enters CSF by selective transport across blood-brain barrier
normal values
60-70% of serum values
Elevated glucose
increased serum glucose (hyperglycemia)
traumatic tap
decreased glucose
alterations to the glucose transport mechanism across the blood-brain barrier or increased use of glucose in the brain
CNS infections (meningitis)
CNS damage
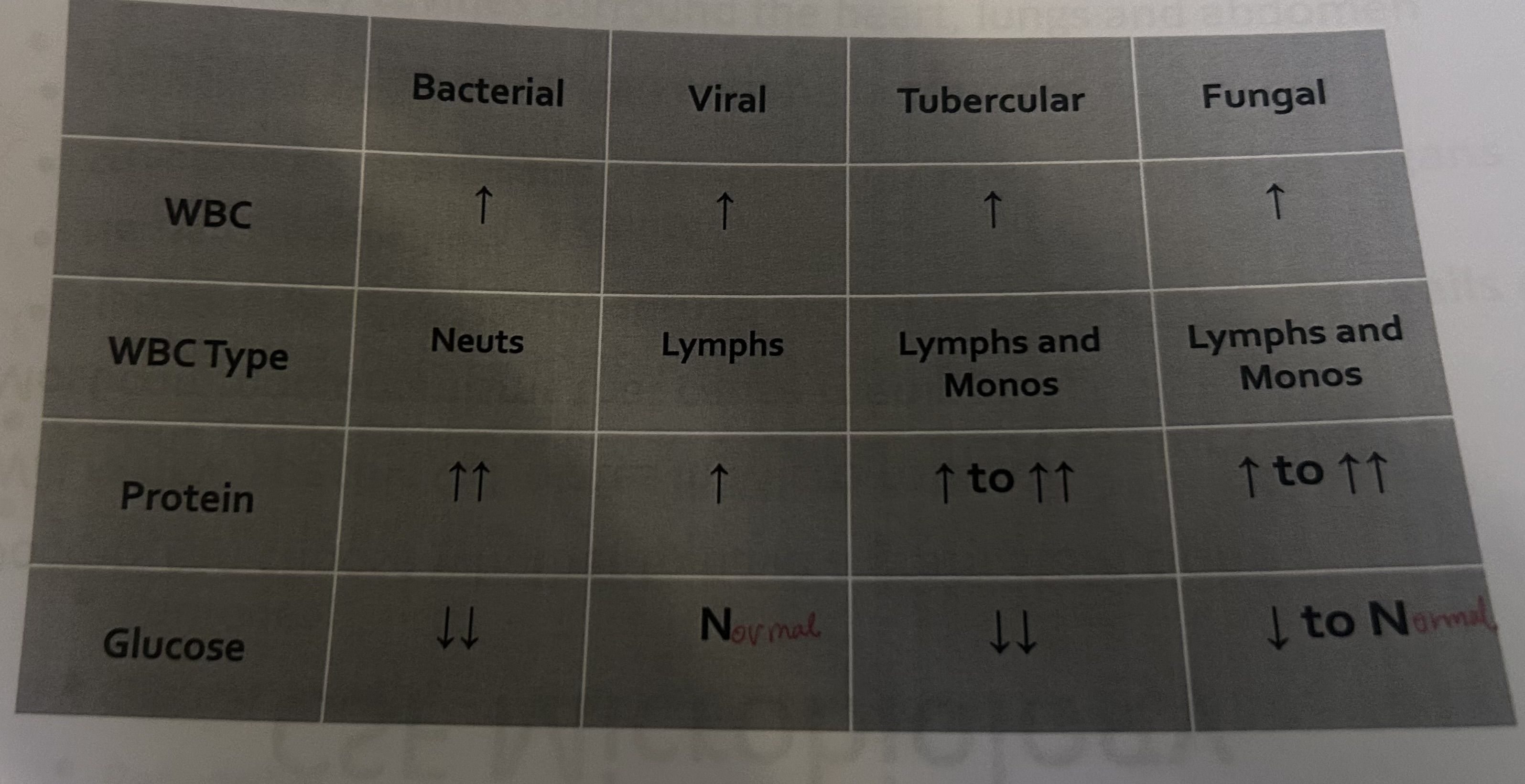
Correlate WBC count, differential results, and protein and glucose levels in bacterial, viral, tubercular and fungal meningitis.
Define serous body cavity, visceral membrane, parietal membrane.
Serous Body Cavity
surrounds the heart, lungs, and abdomen
Visceral membrane
serous membrane covering the organs contained within a cavity
Parietal membrane
serous membrane that lines the walls of the lung, heart and abdomen cavities
Define effusion, transudate, exudate and list disease states for each.
Effusion
an accumulation of fluid between the serous membranes
Transudate
serous effusion produced as a result of systemic disruption of fluid production and regulation between the serous membranes
congestive heart failure
hepatic cirrhosis
nephrotic syndrome
Exudate
serous fluid effusion caused by conditions producing damage to the serous membranes at the site of fluid production
infections
inflammation
hemorrhage
malignancy
Differentiate between transudates and exudates based on lab results.
Transudates
pale yellow
clear
SG: <1.016
cell count: <1000
glucose: equal to serum
no clotting
LD: <200
protein: <3
Exudates
abnormal color
bloody, cloudy, etc
SG: >1.016
cell counts: >1000
glucose: less than serum level
possible clotting
LD: >200
protein: >3
Define Chylous and Pseudochylous effusions
Chylous
a milky lymphatic fluid that contains triglycerides and chylomicrons
Pseudochylous
milky effusion that does not contain chylomicrons
List normal and abnormal cells found in serous fluid and what they may indicate.
Normal
lymphocytes
macrophages
mesothelial cells: cavity lining cells
Abnormal
neutrophils
eosinophils/basophils
lupus erythematosus (LE) cells
malignant cells
Describe normal peritoneal fluid. List abnormal colors and clarity and what it may indicate.
paracentesis
surgery to obtain fluid
Normal
pale yellow, clear
Abnormal
turbid: infection
green: bile, gallbladder, pancreatic disorders
bloody: trauma, infection, or malignancy
milky: lymphatic trauma or blockage
List causes for transudates and exudates in peritoneal fluid and describe how albumin can be used to differentiate.
Transudates
cirrhosis
hypoproteinemia
Exudates
Infections
neoplasms
pancreatitis
trauma
Albumin can be used to help differentiate between transudates and exudates
serum and fluid albumin is measured
serum albumin - fluid albumin
a difference of >1.1 = transudate
List the normal WBC count for peritoneal fluid and list causes for an increased count.
Normal WBC counts
<350 cells/uL
Increased count is seen in bacterial peritonitis and cirrhosis
an absolute neutrophil count >250 cells/uL or >50% of the total WBC count indicates infection
List what decreased glucose levels may indicate. (peritoneal fluid)
glucose decreased below serum levels may indicate
bacterial and tubercular peritonitis
malignancy
Define pleural fluid and thoracentesis.
Pleural fluid
fluid around the lungs
Thoracentesis
surgical puncture into the thoracic cavity to collect pleural fluid
Describe normal pleural fluid. List other colors and clarity and what it may indicate.
Normal
pale yellow, clear
Abnormal
turbid, white: infection, tuberculosis
bloody: hemothorax, hemorrhagic effusion, pulmonary embolism, tuberculosis, malignancy
Milky: chylous material from thoracic duct leakage, pseudochylous material from chronic inflammation
Brown: rupture of amoebic liver abscess
black: aspergillus
Viscous: malignant mesothelioma
List causes for transudates and exudates in pleural fluid
Transudates
hypoproteinemia
peritoneal dialysis
postoperative
postpartum
venous obstruction
congestive heart failure
Exudates
neoplasma
post myocardial infarct
pulmonary emboli or infarct
trauma
bile peritonitis
Describe what abnormal cell types in a pleural fluid may indicate.
neutrophils are indicative of bacterial infection such as pneumonia
leukocytes are normally present in transudates and exudates
elevated lymphocyte counts are seen in effusions resulting from:
tuberculosis
viral infections
malignancy
autoimmune disorders (RA and SLE)
Eosinophil levels >10% may be associated with trauma resulting in a pneumothorax or hemothorax in the pleural cavity
Define pericardial fluid and pericardiocentesis.
pericardial fluid
accumulation of fluid around the heart
Pericardiocentesis
removal of fluid from pericardium
dangerous and rarely performed
done if infection or malignancy are suspected
Describe what pericardial effusions are caused by.
Pericardial effusions are caused by damage to the mesothelium and not by mechanical factors, therefore they are usually exudate
Transudate
metabolic and autoimmune disorders
Exudate
cardiovascular disease
coagulation disorders
infections
metabolic diseases
neoplasma
trauma
Describe normal pericardial fluid. List other colors and clarity and what they may indicate.
Normal
pale yellow, clear
Abnormal
blood-streaked: infection, malignancy
grossly bloody: cardiac puncture, anticoagulant, medications
milky: chylous or pseudochylous material
List causes of transudates and exudates in pleural fluid.
Transudates
metabolic and autoimmune disorders
Exudates
cardiovascular disease
coagulation disorders
collagen vascular disorders
infections
metabolic diseases
neoplasms
trauma
Describe synovial fluid and arthrocentesis. What makes it viscous?
Synovial fluid
viscous and mucinous and lines most joints
Arthrocentesis
the puncture of a joint to obtain synovial fluid
Viscosity
comes from the polymerization of the hyaluronic acid is essential for the proper lubrication of joints
Describe normal synovial fluid. List abnormal colors and clarity and what they may indicate.
Normal
colorless and clear
Abnormal
Yellow/clear: non-inflammatory effusions
osteoarthritis
Yellow/cloudy: inflammatory process
RA or SLE
white/cloudy: inflammatory, may contain crystals
gout or pseudogout
green/cloudy: septic
infection
Red/brown/xanthochromic: hemorrhage
trauma, tumors, hemophilia
List proteins synovial fluid does not contain. List causes for increased protein
contains all except
Fibrinogen
beta-2-macroglobulin
Alpha-2-macroglobulin
Increased protein levels
Ankylosing spondylitis
arthritis
arthropathies that accompany Crohn disease, gout, psoriasis
Describe levels of synovial glucose and the correlation with serum glucose and what it indicates.
synovial glucose levels should be interpreted using serum glucose levels
synovial glucose levels should be <10 mg/dL lower than serum levels
infectious joint disorders can cause synovial glucose to be 20 to 100 mg/dL lower than serum levels
other joint disorders can cause a decrease of 20 mg/dL less than serum gllucose
List the normal percentages of cells in synovial fluid and list abnormal cells that can be seen and what they indicate.
Normal synovial fluid may contain small amounts of lymphocytes and a few neutrophils
monocytes 48%
Lymphocytes 24%
Macrophages 10%
Neutrophils 7%
Synovial Lining Cells 4%
Abnormal
Eosinophils >2% may indicate arthritis, hemorrhagic joint effusions, lyme disease, parasitic arthritis, rheumatoid diseases and tubercular arthritis
septic arthritis exhibits high levels of neutrophils
LE cells can be seen in about 10% of patients with SLE and in some RA patients
plasma cells
Describe MSU, CCPD, and cholesterol crystals and what disease states they indicate.
MSU
thin, needle like
negative bifringence
yellow when parallel
Gout
CCPD
Smaller, rod-like or rhomboid
positive bifringence
blue when parallel
Pseudogout
Cholesterol crystals
Large, flat, transparent plates with notched corners
exhibit a variety of colors under polarized light
may be present in chronic effusions with patients with osteoarthritis or RA
Identify crystals seen in synovial fluid.
Define bronchoalveolar Lavage (BAL).
Not a natural occurring fluid, produced during procedure when warm saline is added to the lungs and then withdraw it
laboratory receives the withdrawn specimen
used to determine types of organisms and cells present in areas of the lung that are inaccessible
cell count must be performed within 1 hour
Describe possible colors and clarity and what they indicate. (BAL)
bloody/pink/brown
could indicate an an alveolar hemorrhage
Milky/white/brownish
could indicate pulmonary alveolar proteinosis
List normal cells seen in BAL fluid, and disease states that cause increased amounts of lymphocytes and eosinophils.
Normal
ciliated columnar epis
squamous epis
alveolar macrophages
neutrophils (low numbers
lymphocytes and eosinophils can be present in low numbers
Describe collection requirements and indications for a seamen analysis.
Indications
infertility
vasectomy effectiveness
forensic studies
sperm donor evaluation
paternity cases
Must be collected through masturbation and the patient should be abstinent for at least 48-72 hours
when transporting the specimen temp changes should be avoided
Describe how to check for viscosity (liquefaction) and list the normal time for liquefaction.
normal semen is slightly viscous and will dispense drop by drop from a pipette
increased viscosity will show a string of fluid when dispensed from a pipette
normal liquefaction time is 30 to 60 min
Describe normal seminal fluid. List abnormal seminal fluid color, what it may indicate and the cause. List normal volume for seminal fluid.
semen is opaque and can have a variety of normal colors
gray
white
light yellow
deep yellow color is associated with certain drugs brown or red colored may contain blood
a turbid specimen usually contains leukocytes and may indicate a reproductive tract infection or inflammation
normal volume is 2-5 mL
List normal sperm concentrations, the time frame to test for motility, and describe the grading for motility.
normal
between 20-250 million/mL
Time frame
within 1 hr of collection
grading
progressive (straight line)
non-progressive (circled, vibrating)
non-motile
at least 80% should demonstrate forward progress in a normal sample
motility can be affected by temps and abys
Define viability. Describe how to read a viability slide. Explain why sperm is observed for agglutination.
Viability
determines if the non-motile sperm are viable or non-viable
Slide reading
eosin stain will make live sperm white and dead sperm pink
agglutination may be normal
if they are clumped head to head or tail to tail then it might indicate anti-sperm antibodies
Describe normal sperm morphology and list what areas of the sperm abnormalities could be seen.
Normal morphology
flattened oval head and elongated tailpiece
contains nucleus that takes up 65% of the head
tailpiece varies in thickness
Headpiece abnormalities
acrosomal abnormalities
constricted heads
enlarged or pinheads
nuclear abnormalities
Tailpiece abnormalities
coiled tailpiece
cytoplasmic extrusion mass
multiple tails
tail length
List other cells that can be found in seminal fluid and what each indicates