Respiratory Exam (2nd year abbreviated)
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
What is the acronym describing what you should do when beginning a respiratory exam?
WINDEC
WINDEC
Wash hands
Introduce yourself (name and role)
Name of patient
Date of birth of patient
Explain the examination you will be performing
Consent from patient
What is the first step in performing a respiratory exam (after WINDEC)?
General inspection upon approach - looking at and around the patient for any signs of acute illness
What should you look for when first generally inspecting the patient?
Age
Also look at their surroundings - any objects that can provide some information about them - eg. cigarettes/vapes, O2 delivery devices, sputum pots, other medical equipment, mobility aids, charts, and prescriptions.
Signs of acute illness:
Look at their position
Observe their breathing (rate and pattern)
Listen to their breathing - cough, stridor, or wheeze present?
Cyanosis
Pallor
Oedema
Drowsiness and confusion
Are they in pain?
Cachexia
What parts of the body are assessed in a respiratory exam?
Hands
Neck
Face
Anterior and posterior thorax
When observing the hands, what are you looking for?
Cyanosis
Tar staining
Tremors - flapping or fine
Skin temperature
Thenar muscle wasting
Skin changes - eg. bruising and thinning of skin (indication of steroid use)
Joint swelling or deformity (indication of RA, which can affect respiratory system)
Signs of systemic illness
Check for finger clubbing
Measure pulse (15 seconds for OSCE - and count resp rate too)
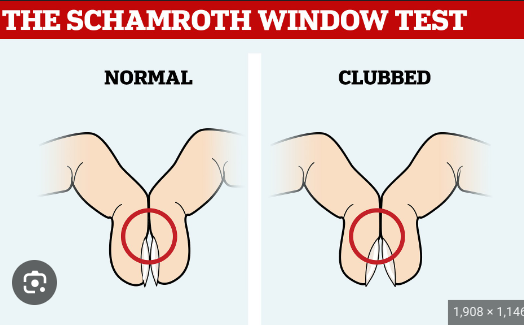
How do you check for finger clubbing?
Press index fingers together and check for the diamond.
What is finger clubbing a sign of?
It may be idiopathic, but it can be a sign of an underlying health condition - usually one that causes chronic low oxygen levels. Some of the more common underlying health conditions are:
Lung malignancy (most common pulmonary cause)
Other types of thoracic malignancy
Interstitial lung disease
Cardiovascular disease
Infectious disease
GI disease
Some infectious diseases
How does chronically low oxygen cause finger clubbing?
The body produces more vascular growth factors when oxygen levels are low.
These factors stimulate the growth of new blood vessels, which change the shape of the finger.
When examining the face, what should you be looking out for?
Central cyanosis (blue lips)
Anaemia (pale)
Plethoric complexion (congested red faced, associated with polycythaemia and CO2 retention)
Horner’s syndrome (ptosis, miosis, enophthalmos)
Other signs of systemic illness
After inspecting the patient’s face, what should you ask them to do?
Open their mouth and stick out their tongue so you can examine them as well.
After examining the patient’s face and tongue, what should you do next?
Examine the neck.
What are the steps for examining a patient’s neck?
Check tracheal position
Check cricosternal distance
Check for tracheal tug
After examining the patient’s neck what comes next?
Inspecting the patient’s anterior and posterior thorax. Remember to ask them to take a deep breath at this point.
What are you looking for when inspecting the patient’s anterior and posterior thorax?
Hyperinflation
Asymmetry
Scars
After inspecting the patient’s anterior and posterior thorax, what should you do?
Palpation.
After palpation, what comes next?
Chest percussion
After chest percussion, what comes next?
Auscultation.
After auscultation, what should you do?
Finish the examination.
Cyanosis
Bluish colour in the skin, lips and nail beds caused by a shortage of oxygen in the blood.


What is this?
Tar staining on fingers.
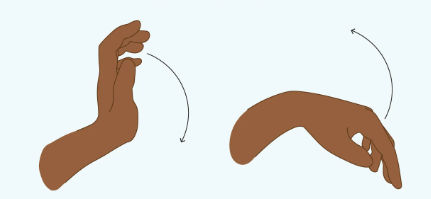
What is this involuntary hand movement called?
Flapping tremor - it can be a sign of pulmonary disease.

What can be observed on the hand on the right?
Thenar muscle atrophy.
Why is checking for wasting of the hand muscles relevant in a respiratory exam?
The localised muscle wasting could be due to a tumour in the apex of the lung compressing a nerve.
What are some signs of systemic disease in the hands?
Raynaud’s phenomenon
Clubbed fingers
Buerger’s disease (blocked blood vessels in fingers - pale fingers, ulceration, gangrene)
RA
Gout
Diabetes (eg. trigger finger)
Dactylitis (swelling)
Cysts
Red spots
White fingernails (sign of liver or kidney disease)
Red streaks on nails
Abnormal nail shapes (eg. pincer nail)

What does this image show?
The patient has Horner’s syndrome (one droopy eyelid). Respiratory causes could be tumours in the lungs and surrounding tissues or infection, as can damage nerve pathways running through that area.
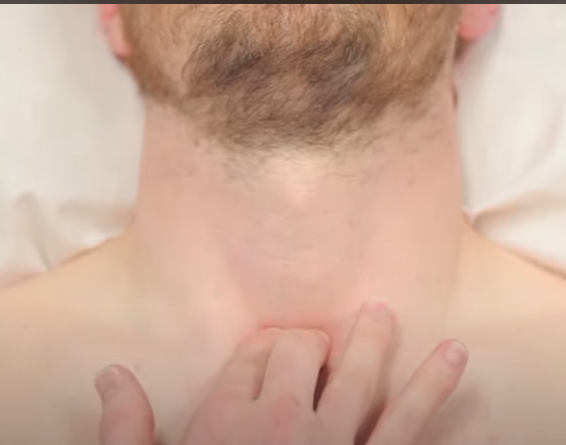
How can you check for tracheal deviation?
First explain to the patient what you are going to do and let them know it may be uncomfortable. Place index and ring finger on the two clavicular heads/on either side of the trachea??? and then place your middle finger in the suprasternal notch. The trachea should be in the midline.
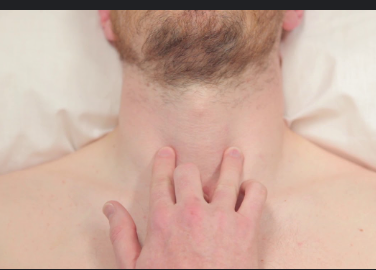
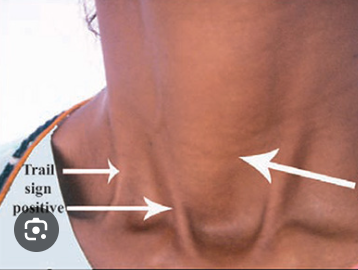
What does this photo show?
Tracheal deviation.
How can you check for cricosternal distance?
Place three fingers in a vertical line up from the suprasternal notch. You should be able to feel the lower border of the cricoid cartilage (may be 4 fingers instead). If the distance is shorter than 3 fingers then this may indicate the patient has a hyperinflated chest.

What respiratory problem can asterixis indicate a patient has?
Flapping tremor can indicate there is CO2 retention.
What can the presence of a fine tremor indicate in a respiratory exam?
The patient has potentially taken beta-2-agonists like salbutamol - commonly found in inhalers.
What can a prolonged expiratory phase indicate?
This is often the case with patients who have asthma exacerbations or COPD.
What should the normal respiratory rate be?
12-20 breaths a minute
Bradypnoea
RR is less than 12 breaths a minute
Tachypnoea
RR is more than 12 breaths a minute
When inspecting the mouth and tongue, what are you searching for?
Central cyanosis (blue lips or tongue)
Oral candidiasis (thrush)

What does this photo show?
Oral candidiasis
Oral candidiasis
Oral thrush - a fungal infection in the mouth commonly associated with steroid inhaler use (local immunosuppression).

How do you assess for tracheal tug?
Place two fingers on the trachea in the suprasternal notch.
Ask the patient to inhale and exhale deeply
If the trachea moves downwards when they exhale, tracheal tug is present.
Tracheal tug (Oliver’s sign)
Abnormal movement of the trachea on inspiration that indicates possible aortic arch aneurysm or dilation.
What chest wall deformities may be present upon inspection of the thorax?
Remember to get the patient to lift their arms to get a clearer view of the lateral chest wall.
Asymmetry
Pectus excavatum (caved in appearance of chest)
Pectus carinatum (protrusion of the sternum and ribs)
Hyperexpansion (barrel chest)
What are the causes of tracheal deviation?
Tension pneumothorax
Large pleural effusions
Lobar collapse
Pneumonectomy
How do you assess chest expansion?
Walk behind them
Ask the patient to take a deep breath in
Place hands on the side of the patient’s chest inferior to the nipples and wrap fingers around each side of the chest (hands are firm, pull skin back a little)
Ask patient to breathe in and out
Observe the movement of your thumbs - they should move symmetrically upwards and outwards upon inspiration and symmetrically downwards and inwards on expiration.
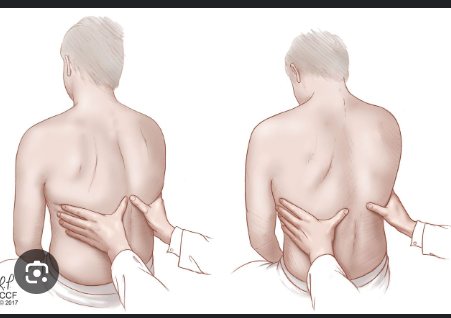
What can cause symmetrical reduced expansion of the chest?
Pulmonary fibrosis
What can cause asymmetrical reduced expansion of the chest?
Pneumothorax
Pneumonia
Pleural effusion
Percussion technique
Place non-dominant hand on patient’s chest
Position the middle finger over the area you want to percuss, firmly pressed against the chest wall and rigid
With your dominant hand’s middle finger, strike the middle phalanx of your non-dominant hand using a swinging movement of the wrist
Remove striking finger quickly otherwise you may muffle the resulting percussion note
Types of percussion note
Resonant
Dull
Stony dull
Hyper-resonance
Resonant note (percussion)
A normal finding
Dull note (percussion)
Suggests increased tissue density (eg. cardiac dullness, consolidation, tumour, lobar collapse)
Stony dull note (percussion)
Typically caused by an underlying pleural effusion.
Hyper-resonance (percussion)
Opposite of dull - suggests decreased tissue density (eg. pneumothorax)
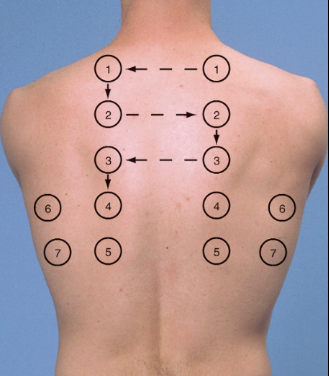
What are the locations of the posterior thorax you should percuss?
What are the locations of the anterior thorax you should percuss?
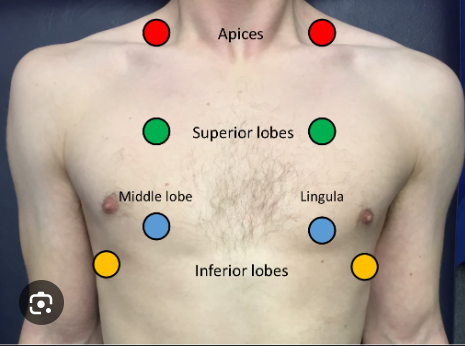
Auscultation technique
Ask patient to relax and breathe deeply in and out through their mouth.
Place the diaphragm of the stethoscope on the chest wall and listen to inspiration and expiration.
Auscultate each side of the chest at each location for direct symmetrical comparison.
Assess the quality and volume of breath sounds and note any added sounds.
What words are used to describe the quality of breath sounds?
Vesicular
Bronchial
Vesicular breathing
Normal quality of breath sounds in healthy individuals
Bronchial breathing
Harsh-sounding (similar to auscultating over the trachea), inspiration and expiration are equal and there is a pause between. It is associated with consolidation.
What do quiet breath sounds indicate?
Reduced air entry into that region of the lung (eg, pleural effusion, pneumothorax)
Name some added breath sounds you may hear upon auscultation
Wheeze
Stridor
Coarse crackles
Fine end-inspiratory crackles
Wheeze
A continuous, coarse, whistling sound produced in the respiratory airways during breathing.
What is a wheeze associated with?
COPD
Asthma
Bronchiectasis
Stridor
A high-pitched extra-thoracic breath sound resulting from turbulent airflow through narrowed upper airways. (causes include swelling of the face or neck, foreign objects etc.)
Coarse crackles
Discontinuous, brief popping lung sounds typically associated with pneumonia, bronchiectasis and pulmonary oedema.
Fine end-inspiratory crackles
Sounds like velcro. This is usually associated with pulmonary fibrosis.
How does the exam conclude?
Explain to the patient that the examination is complete
Thank the patient for their time
Wash your hands