Molecular pharmacology/ Drug receptors and pharmacodynamicmechanisms /drug metabolism / Autonomic pharmacology
1/212
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
213 Terms
Pharmacology
Study of the actions and effects of drugs on living systems and interaction of drugs with living systems
Pharmacokinetics
How does the drug concentration change as it moves through different compartments of the body "what the body does to the drug"
From the time the drug is administered to the time it is metabolized, distributed, or eliminated
Pharmacodynamics
How does the drug exert its effects on the body "what does the drug do to the body?"
-after the drug is transported to the site of action
Affinity definition
Binding to the molecular target
Efficacy definition
Response to the drug
What does pharmacodynamics study?
Drug actions at target (receptor) sites and the physiological/ chemical/ behavioral effects produced by these actions
"The drugs mechanism of action"
Pharmacodynamics provides the bases for
Rational therapeutic uses and the design of therapeutic agents
Most drugs act by interacting with.....
A specific target (protein)
3 groups of functional proteins
Enzymes
Ion channels
Transporters
Receptors
How do drugs affect enzymes ?
Drugs can either increase or decrease the rate of enzyme mediated reactions
5 major types of drug effects / actions
Stimulation
Depression/ inhibition
Irritation/inflammation
Replacement
Cytotoxic effect
An example of a stimulation effect
Adrenaline on the heart
examples of inhibition /depression
Quinidine on the heart
Barbiturates on CNS
Omeprazole on gastric acid secretions
Examples of irritation/ inflammation
Epithelial cells
Necrosis and morphological changes
Examples of replacement drugs
Levodopa in Parkinson's
Insulin in diabetes
Iron in anemia
Examples of cytotoxic effect
Anti-parasitic drugs
Antibiotic drugs
Anti-cancer drugs
Magnitude of drug response dependent on ....
Concentration achieved at the site of action/ receptor (dosage, extent of absorption, metabolism/ distribution to the site, rate/ extent of elimination)
Receptors are ...
Proteins inside or on the surface of cells that mediate drug activity
Receptors respond to....
Specific ligands (neurotransmitters, hormones, antigens, chemicals, or substances)
A ligand bind to a specific site (blank) and triggers a response (blank) in the cells
Receptor and signal
Ligands generally function as
Either an agonist or an antagonist
Agonist
Mimics the endogenous /physiologic ligand to produce similar response
Morphine for opioid receptors
Antagonist
Blocks the usual ligand and inhibits the physiological response
Naloxone for opioid receptors
Receptors have a
High specificity and selective affinity for the ligand (drug molecule)
Specificity
The measure of a receptors ability to respond to single ligand
Low specificity results in
Physiological responses not targeted or intended by the drug (side effects)
Affinity
The strength of attraction between the drug and its receptor
High affinity is associated with
A lower dose requirement
Occupancy theory
The effect of a drug results the occupancy of its receptor (sometimes)
1. One drug molecule combines reversible with one receptor
2. All receptors are identical and equally accessible to drug
3. Magnitude of response is proportional to the # of receptors occupied
4. The effective drug concentration does not change during the reaction
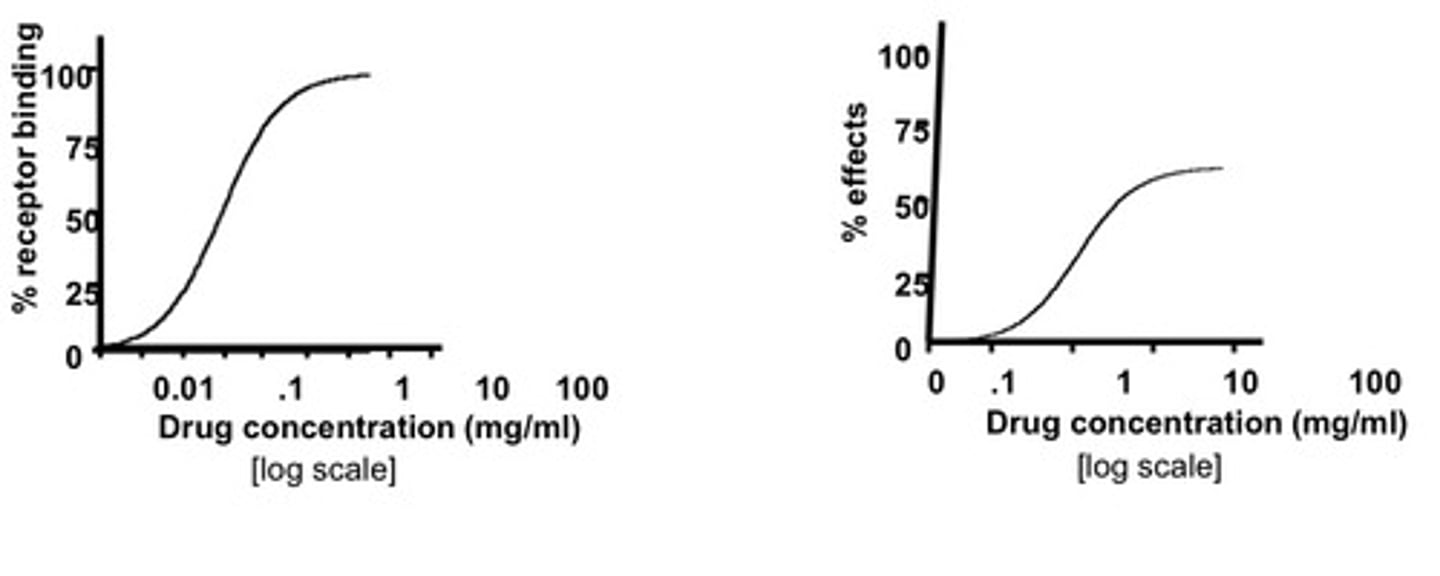
Graded dose-response curve (A)
Plot of response versus the drug concentration or dose
Efficacy (Emax) and potency (EC50 or ED50)
Sigmoid curve (B)
Graded dose-response curve on a logarithmic concentration axis
Efficacy (Emax) and potency (EC50 or ED50)
EC50
Dose or concentration at which effect is half the maximal effect
Emax
Maximal effect
The smaller the EC50/ED50
The greater the potency (smaller dose is needed to reach 1/2 max)
Kd
dissociation constant, concentration at which 50% of receptors are bound, measure of affinity of the drug to it binding site
The smaller the Kd
The greater the affinity of the drug for its receptor
Bmax
maximal number of receptors bound
Binding curve
Percent of receptors bound by drug (Y)
Drug concentration unite (X)
Dose response curve
Effect (Y)
Drug concentration units (X)
Efficacy
The greatest effect (Emax) an agonist can produce if the dose is taken to the highest tolerated level
Potency
The amount of drug needed to produce a specified effect
Measured based on EC50
Determined by the affinity of receptors for the drug and the number of receptors available
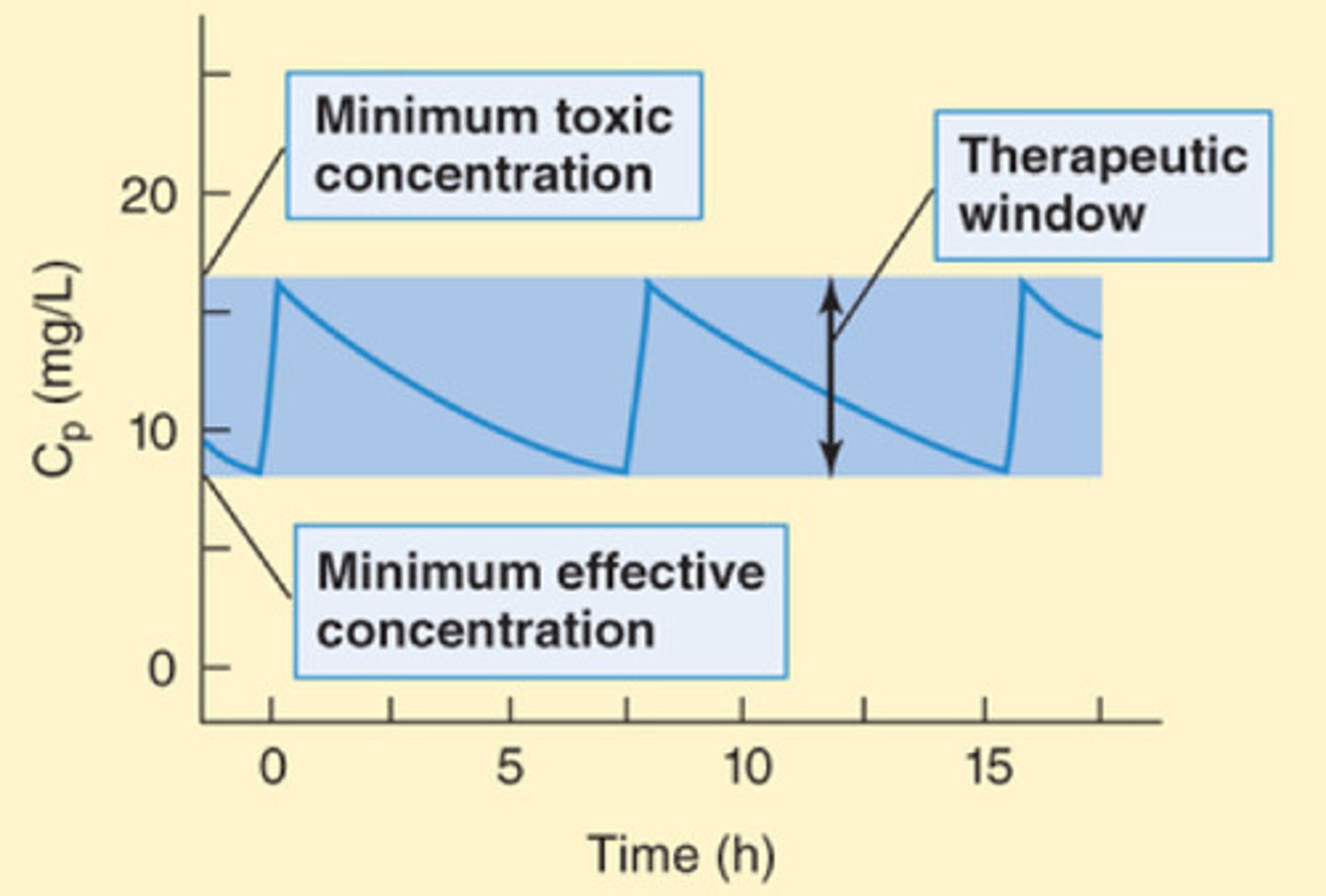
Therapeutic window
Safe range between the minimum therapeutic contraction and the minimum toxic concentration of the drug

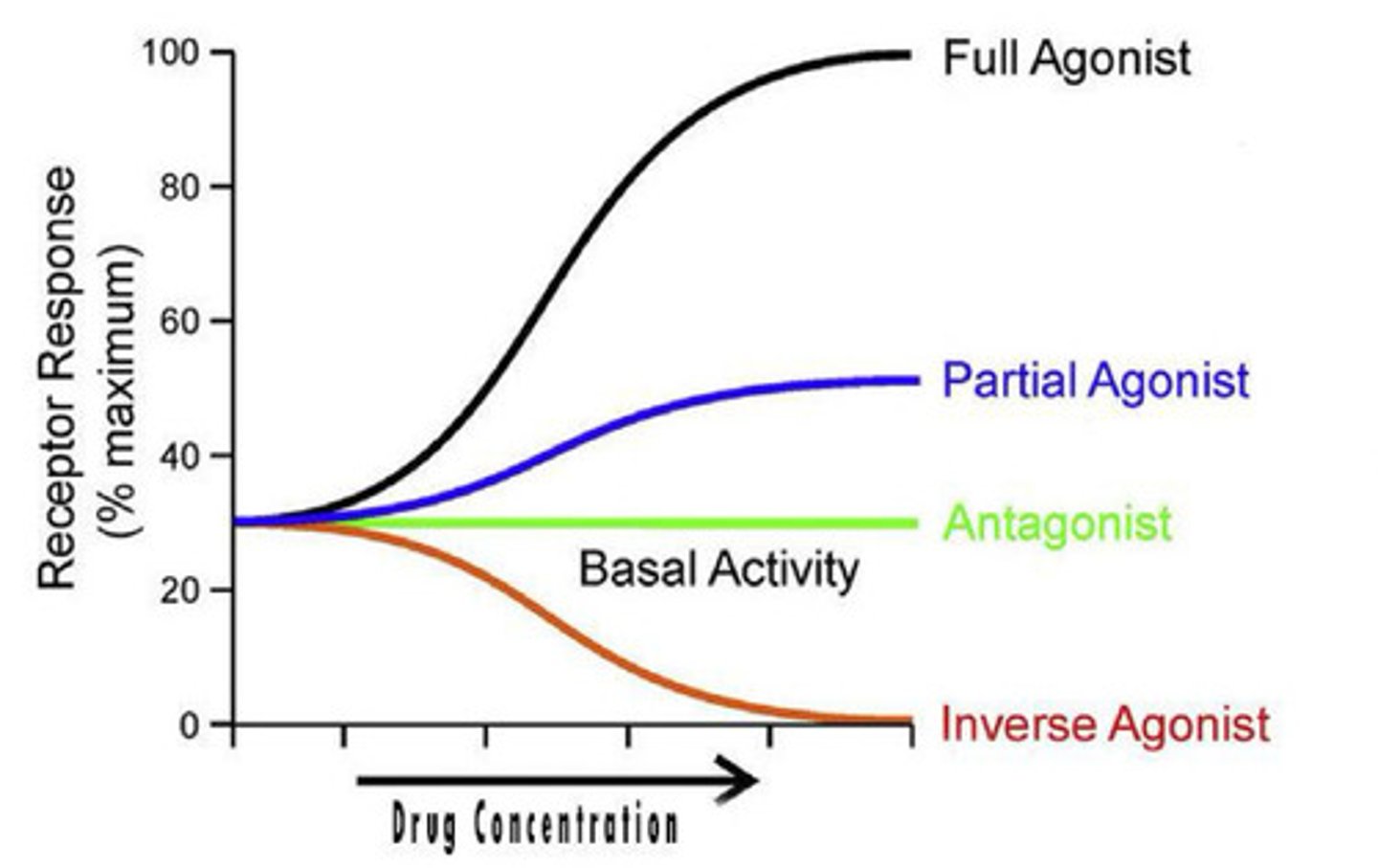
Full agonist
Drug capable of fully activating the effector system when it binds to the receptors
Has high affinity for the activated receptor conformation and sufficiently high concentration result in all the receptors achieving the activated states
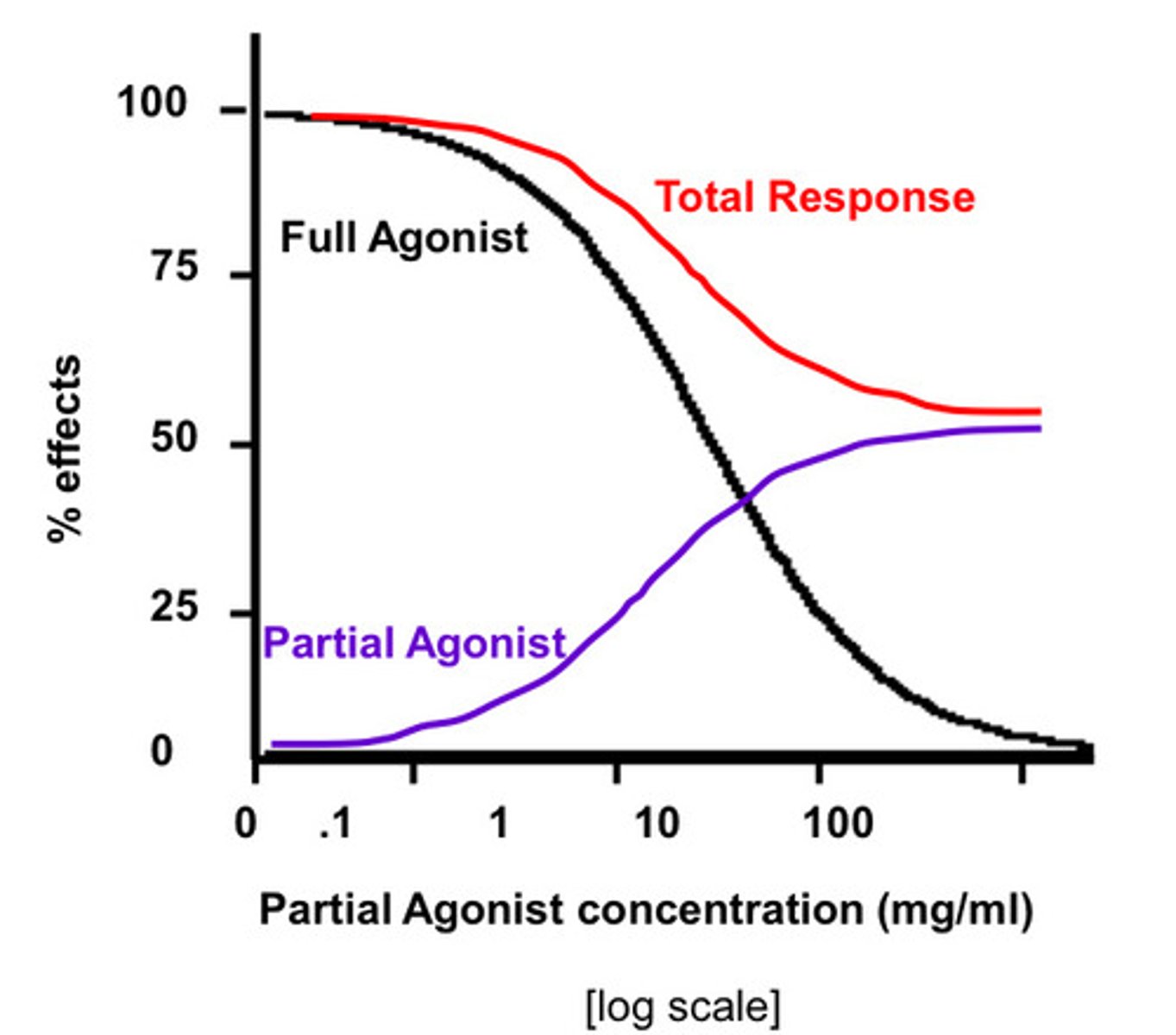
Partial agonist
Produces less than the full effect when it has saturated the receptors
Inverse agonist
Have a higher affinity for the inactive state than for the active state (decrease or abolish any constitutive activity, activity in the absence of ligand)
Antagonists bind to receptors but
Produce no effects! Bind to receptors, prevent agonists binding and block their actions
Neutral antagonist bind with
equal affinity to the Ri (inactivated) and Ra (activated) states, prevent binding by an agonist and prevent any deviation from the level of constitutive activity

When effect and occupancy aren't the same graph
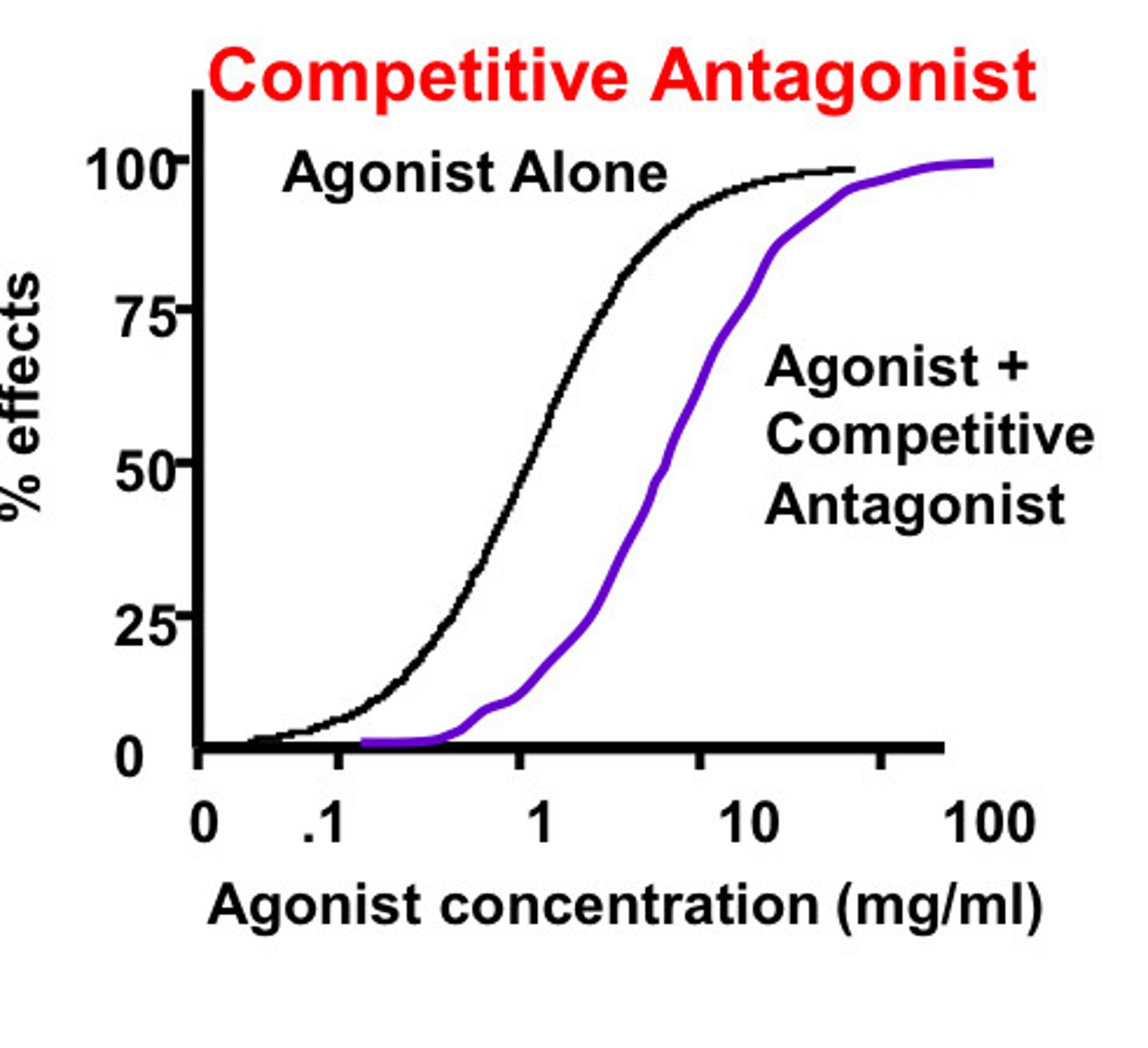
Competitive antagonist
Drugs that bind to or very close to the agonist receptor site in a reversible way without activating the effector system for that receptor
Noncompetitive antagonist
Acts at an allosteric site on the receptor may bind reversibility or irreversibly
Neutral antagonist
Bind the receptor without shifting the ratio of activated receptors to inactivated receptors
Combining competitive antagonist with an agonists
The agonist and the antagonist have to compete for the same binding site
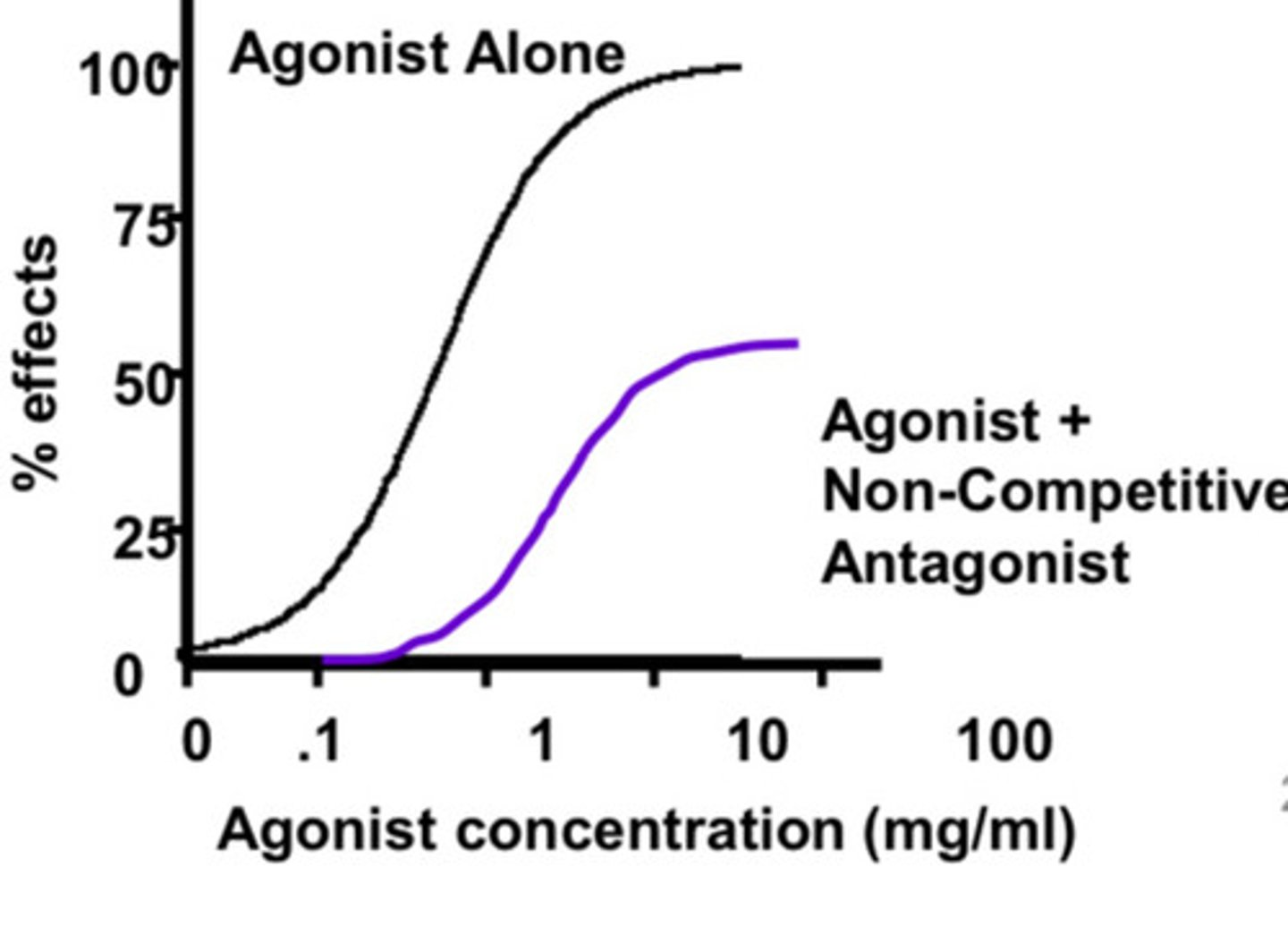
Combining a non-competitive antagonist with an agonist
Since the noncompetitive binds at a different spot from the agonist it is more effective at stoping activity, it doesn't have to compete
What do we not normally combine
Full agonist with partial agonist
Full agonist (single large dose) + partial agonist (increasing dose) graph
Spare receptors
Exist when maximal drug response (Emax) is reached at less than 100% occupation of receptors (Bmax), EC50<Kd
What does it mean for EC50 < Kd ?
To achieve 50% of maximal effect, less than 50% of the receptors need to activated
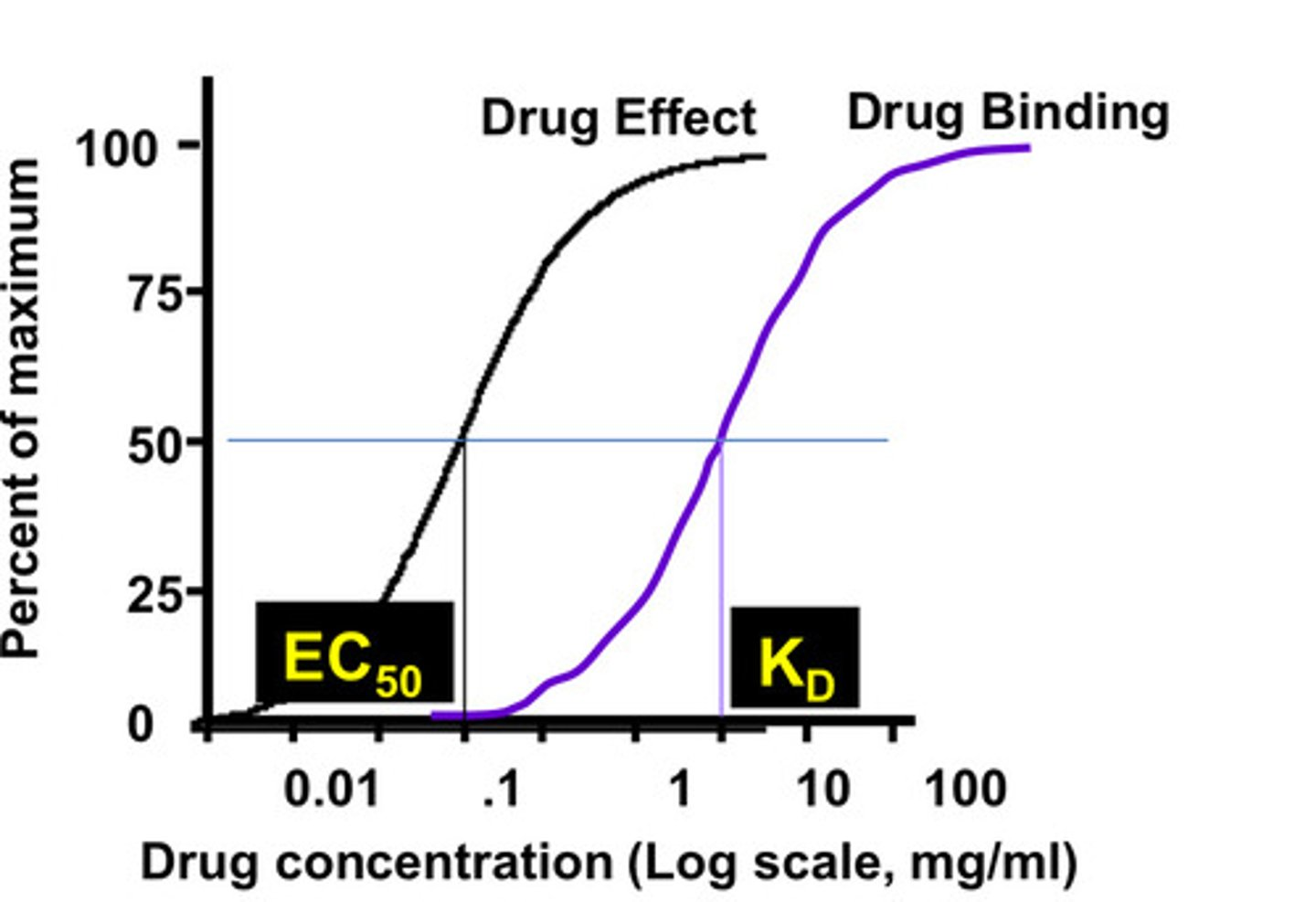
What is the significance of spare receptors ?
Full effect can be reached with <100% occupancy
Duration of effector activation > duration of drug-receptor interaction
# of receptors > # of effector molecules
Endogenous receptor mechanisms visual
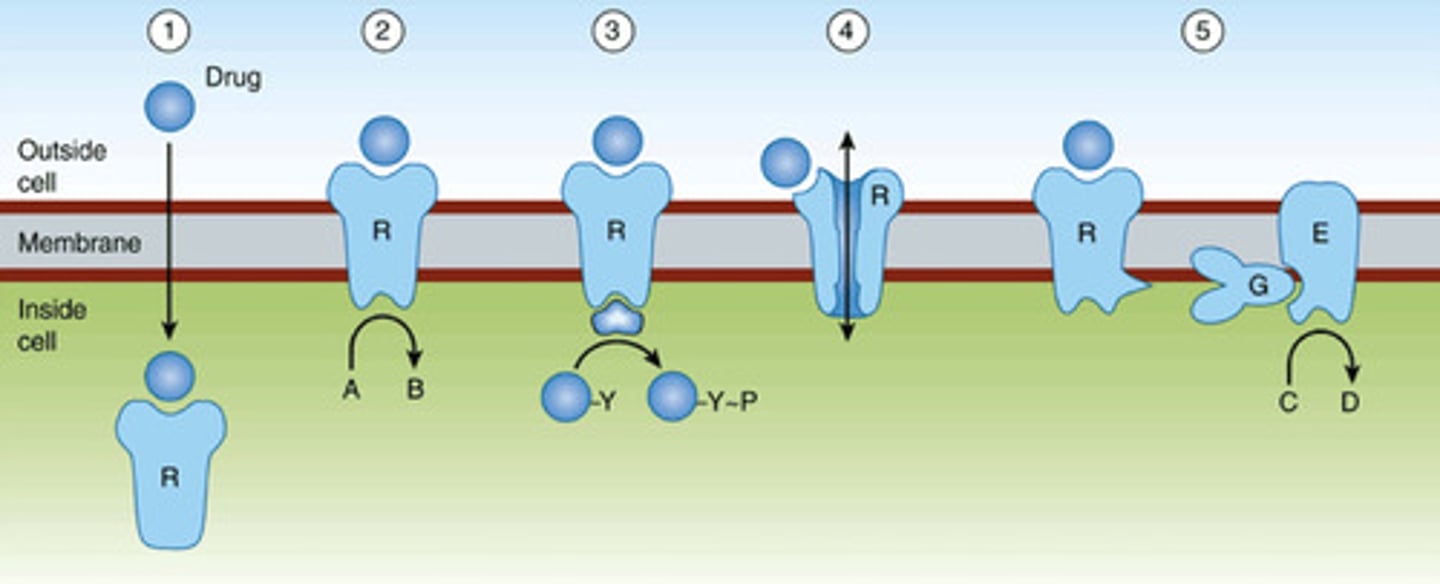
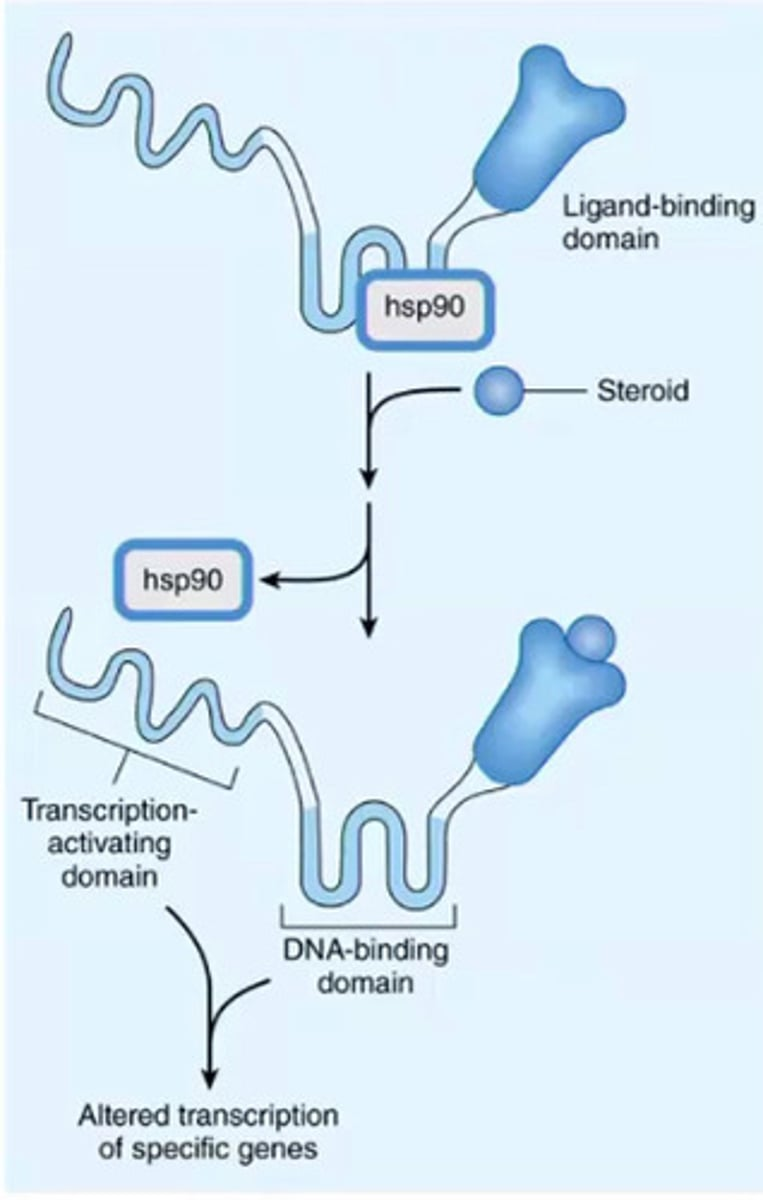
Intracellular nuclear hormone receptor
Drug must be small/ lipophilic to get inside and reach receptor, the receptor has a ligand binding domain where the hormone will bind and it has a DNA binding domain (bind to promoter on DNA) and transcription-activating domain will include TF/TA and the binding will initiate gene expression
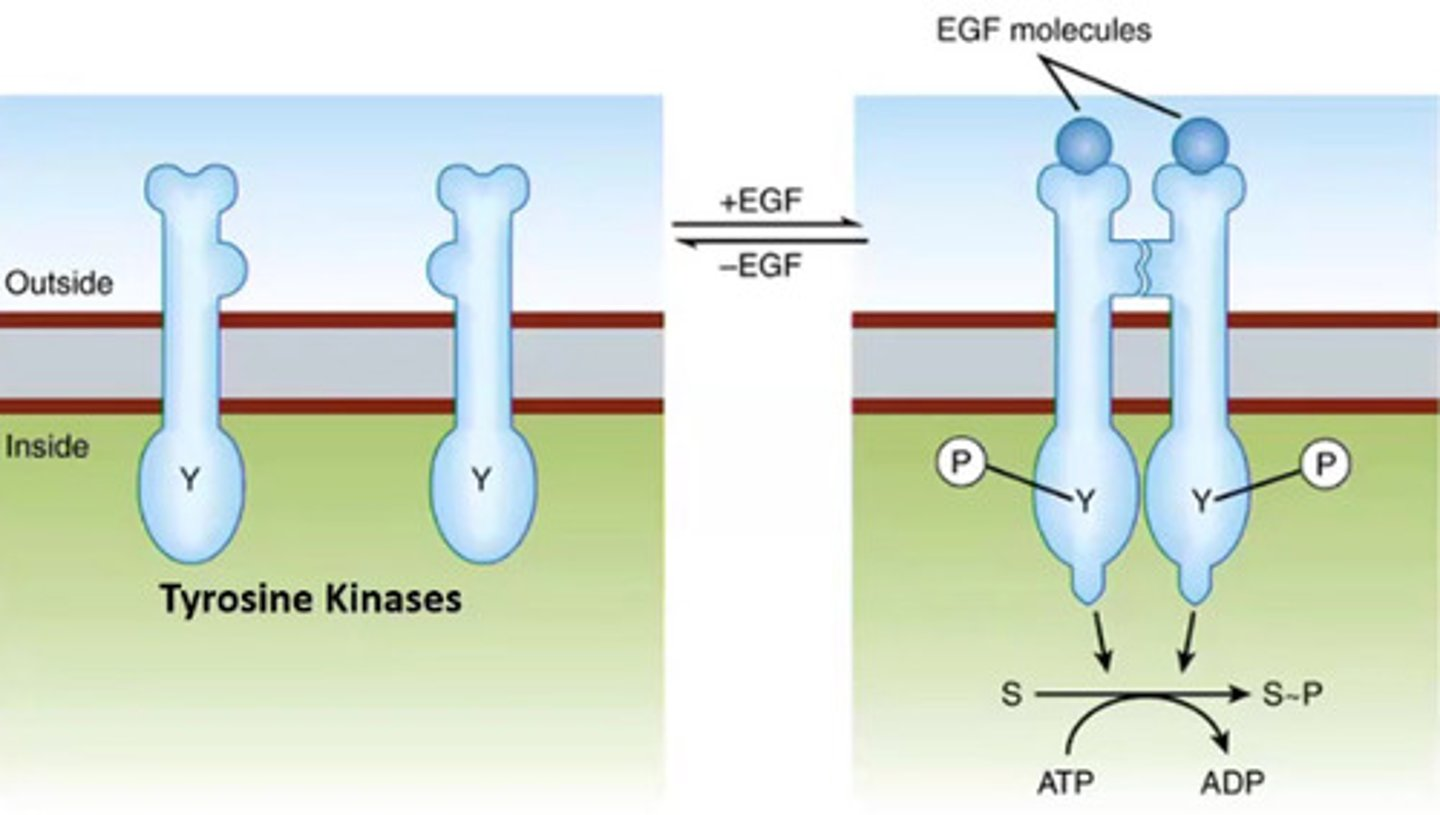
Ligand-regulated kinase receptors
They are kinases that are regulated by the binding of a ligand, on the cell membrane, when the ligand binds it activated dimerization of the receptor and the receptor will start activating each-other by phosphorylation, the activated kinase will now phosphorylate things down stream
*EGF= epidermal growth factor
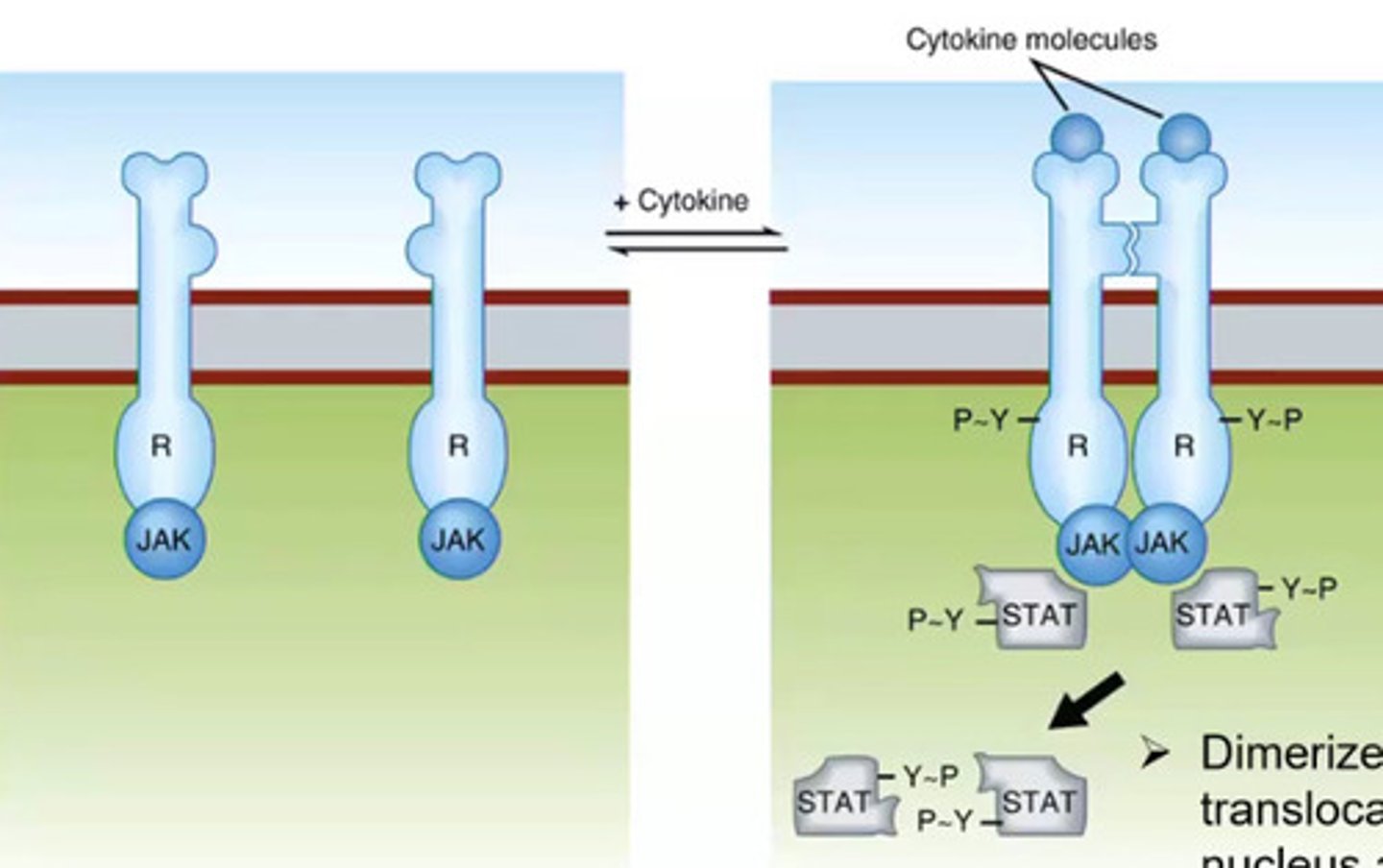
Cytokine receptors
Monomers on cell membrane when the ligand binds it forms a dimer, it will activate a protein kinase (JAK), JAK will then activate substrate (STAT), phosphorylation STAT will then translocate to the nucleus and activate gene expression
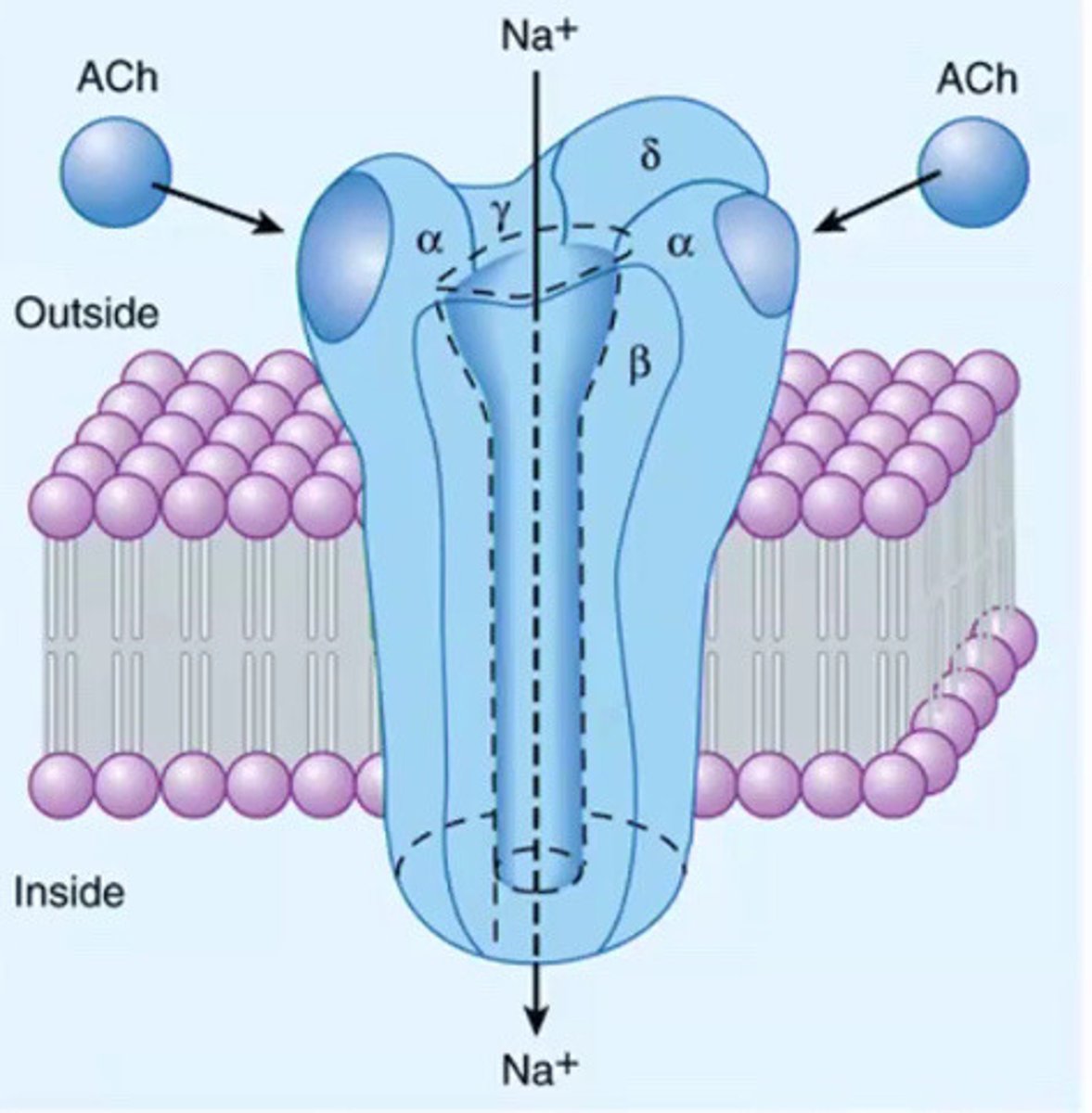
Ligand-gated ion channels
The channel will open and close to allow ions in/out of the cell that is regulated by the binding of the ligand, transmembrane proteins made of multiple subunits, binding of the ligand cause conformational change to receptor to open the gate that allow ions to move based on gradient
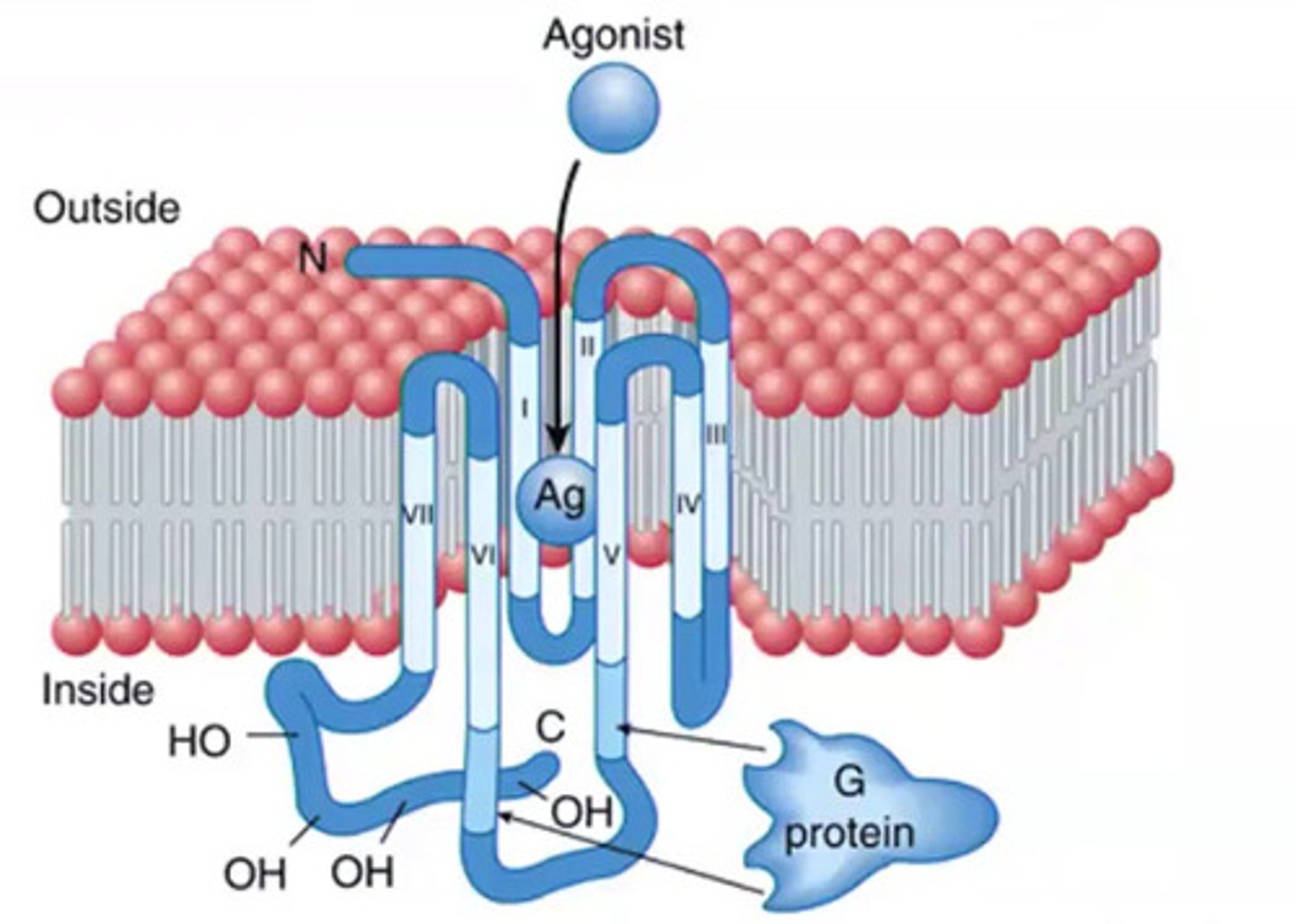
G-protein coupled receptors (GPCRs)
Couple the presence of a ligand/agonist to activate ion os a specific G protein, and this will induce and initiate important cellular functions and responses, transmembrane that snake through the cellular membrane 7 times (N terminus outside and C inside), when the ligand binds it will trigger a conformational change that triggers the the G protein to be activated and activate downstream effectors
more than 70% of drugs on the market target ...
GPCRs
What the 2 states of G proteins ?
GDP bound and GTP bound
GDP
guanosine diphosphate
GTP
guanosine triphosphate
G protein subunits
alpha, beta, gamma
When the G protein is the activated state
The G alpha subunit is bound to GDP
Once a ligand binds to G protein receptor ...
G proteins are activated by exchanging GDP for GTP and the beta and gamma subunits dissociate then GaGTP and BY go on to activate targets (effectors)
G-protein activation cycle image
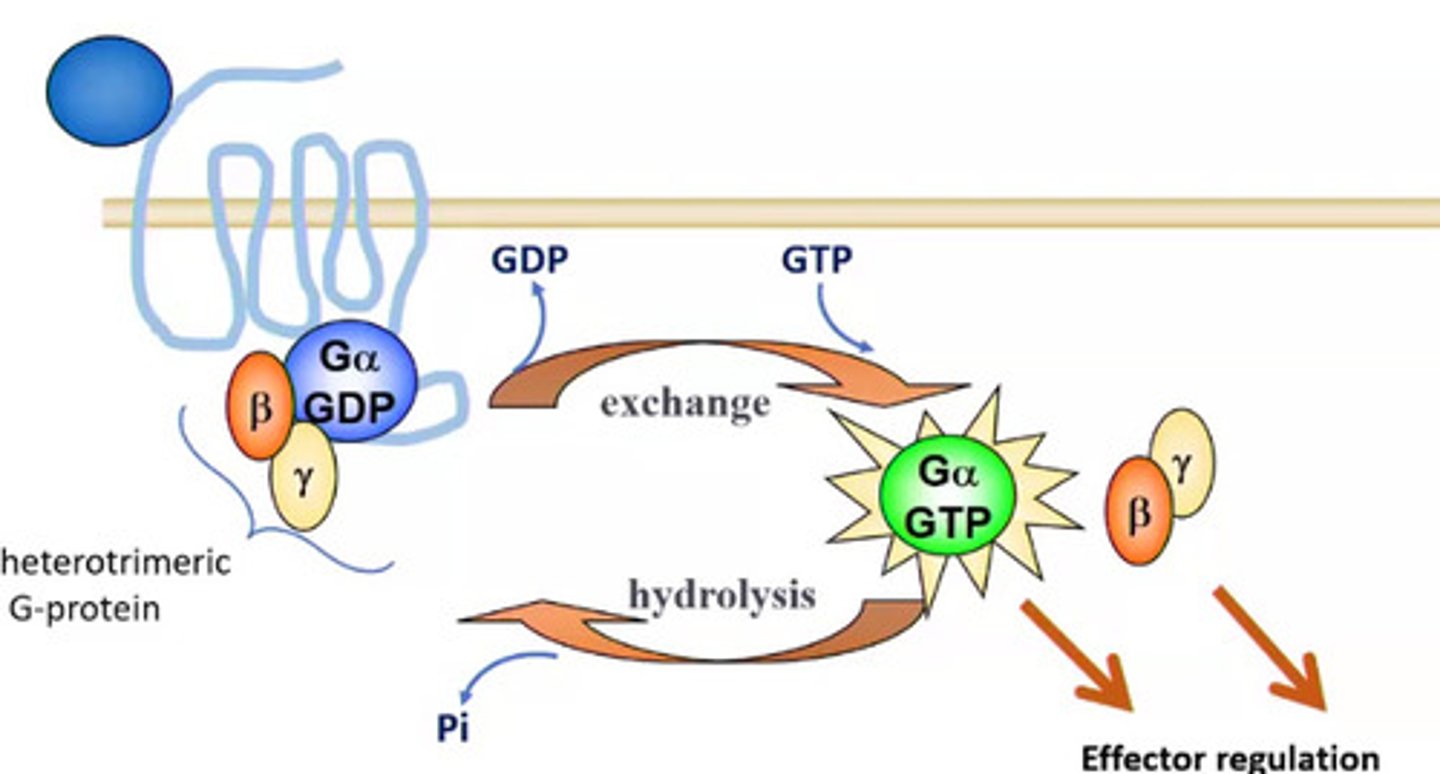
How is activation of GTP turned off?
GTP can be turned off through hydrolysis of GTP to form GDP
What activates effectors in the G-protein activation cycle ?
GalphaGTP and B/Y
Inactive G protein
bound to GDP
Active G protein
bound to GTP
4 major classes of G-alpha proteins that can be activated by GPCRs
Gs, Gi, Gq, and G12 (cancer)
B/y dissociates from which G-alpha protein?
Gi
Gs effector
adenylyl cyclase (+) in the cell membrane
Gi effector
adenylyl cyclase (-) in the cell membrane
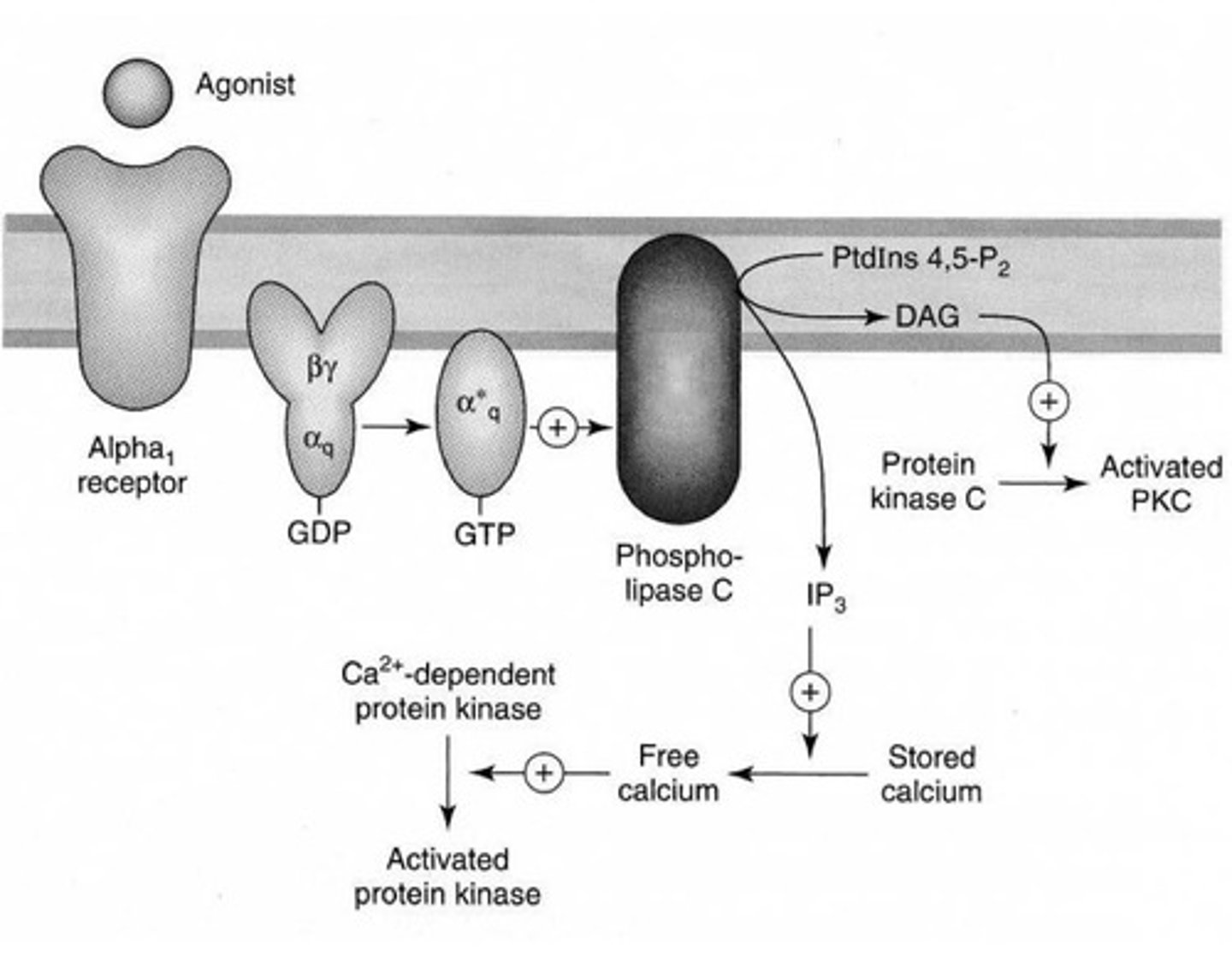
Gq effector
Stimulates phospholipases (enzymes on cell membrane)
B/Y subunits effects
Stimulatory effect on ion channels (calcium) and phospholipase C and adenosine cyclase (only when they leave the Gi)
Effectors
Targets of G proteins
Enzymes or ion channels
Enzymes generate
Second-messengers, hydrophilic soluble products that can diffuse in the cytoplasm and bind to their targets
What 2 enzymes can be activated or inhibited by G proteins ?
AC and PLC
What second messenger can adenylyl cyclase produce?
cAMP (cyclic adenosine monophosphate)
What second messenger can phospholipases produce?
IP3 (inositol 1,4,5-triphosphate)
DAG (diacylglycerol)
G-protein effect on ion channels
Modulate gating by the G proteins (inhibited or stimulated)
Adenylyl cyclase
Produces cAMP
Stimulated by Gs
Inhibited by Gi
cAMP activates
cAMP-dependent protein kinase (PKA) holoenzyme
PKA substrates
Transcription factors (cAMP response element CRE)
Ion channels (AChR, GluR, GABAA, ionotropic receptors,a den calcium channels)
What deactivates adeneylyl cyclase ?
Phosphodiesterases (PDE), cleave a phosphate from cAMP
adneylyl cyclase regulation image
C=catalytic
R=regulatory

Phospholipase C
Membrane bound protein
Multiple isoforms = different regulatory domains (activated by Gq and GBY from Gi)
Produces DAG and IP3
Hydrolyzes PIP2
DAG in membrane which activates PKC
soluble IP3 releases Ca++ which further activates PKC
What activates PKC?
DAG and Ca++
PKC substrates
Transcription factors (MAP kinases)
Ion channels (AchR, GluR, GABAAR)
Ca++ effects (IP3)
Calcium-dependent kinases: smooth muscle contraction
What terminates the signals triggered by phospholipase C?
DAG is phosphorylated / deacylated
IP3 is dephosphorylated
Calcium is sequestration
Phospholipase C regulation image
Voltage gated ion channels
Q-type calcium channels (voltage-activated)
Couple action potential to NT release