PSYC334 - October 7th FIRST EXAM
1/218
Earn XP
Description and Tags
Fall 2025
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
219 Terms
Defining a Psychological Disorder
Psychological disorder has three primary components:
Psychological dysfunction
Someone’s reaction to something. Is the reaction normal, or how normal is it? Spectrum of behaviors. Not adaptive.
Distress of impairment
Is it bothering them, and they can’t do what we expect them to do
Atypical response
Typical response may be atypical to someone else. Look at behaviors in context.
Case Example:
Young girl
Scenario 1:
Describes herself (and is described by others) as shy
Unlikely to raise her hand in class unless prompted
Worries regularly about being called on
Comes from a very loud family
Distressed
Atypical (her family is loud)
Normal range of behavior, no psychological problems
Scenario 2:
Describes herself and is described by others as shy
Refuses to go to school
Throws up when she thinks about speaking in public
Comes from a very quiet family
Atypical and not adaptive (bc she throws up)
Distressed because she refuses to go to school
Definition in the DSM-5:
“Behavioral, psychological, or biological dysfunctions that are unexpected in their cultural context and associated with present distress and/or impairment in functioning, or increased risk of suffering, death, pain, or impairment”
Mania (euphoria, increased energy)
The DSM:
Describes “typical” presentations of different psychological disorders (generalized anxiety disorder, binge eating disorder)
The typical profile is called a prototype → diagnostic criteria in DSM are prototypes
Psychopathology: scientific study of psychological dysfunction
Professionals:
Clinical or counseling psychologist (PhD or PsyD)
Psychiatrist (MD)
Psychiatric nurse (RN)
Licensed clinical social worker (MSW)
Mental health professional:
Consumer of science
Enhancing the practice
Evaluator of science
Determining the effectiveness of the practice
Creator of science
Conducting research that leads to new procedures useful in practice
Studying psychological disorders:
Focus:
Clinical description
Causation (etiology)
Treatment and outcome
Three major categories make up the study and discussion of psychological disorders
Key terms:
Presenting problem
Clinical description
Etiology
Course
Onset
Prognosis
Prevalence
Incidence
Presenting problem:
the reason someone came into a treatment setting
Clinical Description:
the thoughts, feelings, and behaviors that describe a client’s presentation
ex: “Aaron presents with a low mood. Over the last few months, he has reported feeling sad and thinking negatively about himself. His appetite and sleep have gotten worse, and he is spending less time with friends.”
Etiology:
why a disorder begins
Course:
the pattern of the disorder (chronic, episodic)
Onset:
how a disorder starts (acute, insidious)
Insidious: noticing signs for a really long time, getting close to the criteria for a psychological disorder
Prognosis:
anticipated progression of the disorder
Prevalence:
how many people in the population have a disorder
Incidence:
how many new cases occur during a period
ex: “Aaron’s depressive symptoms are episodic with an acute onset after he lost his job. With treatment, his prognosis is good.”
Supernatural
Deviant behavior seen as a battle of “good” vs “evil”
Believed to be caused by demonic possession, witchcraft, sorcery (or, by Paracelsus, the moon and the stars)
Treatments included exorcism, torture, and religious rituals
Biological
Hippocrates (460-377BC) - the “Father of modern Western medicine”
Mental disorders are understood as physical diseases
Linked abnormality with brain chemical balances
Foreshadowed modern views
Galen (129-198 AD) extended Hippocrates’ work
Humoral Theory of Disorders:
Functioning is related to having too much or too little of four key bodily fluids
Blood
Phlegm
Black bite
Yellow bite
Gut health can cause psychological problems
General paresis (late-stage syphilis, a sexually transmitted infection) and the biological link with “madness”
Includes psychological and behavioral symptoms caused by a bacterium
Bolstered the view that mental illness = physical illness
John P. Grey
Believed causes of “insanity” were always physical
Led to reform of hospitals to give psychiatric patients better care (though they became too large)
Treatments:
Electric shock therapy
Crude surgery
Medication
Neuroleptics (major tranquilizers) → antipsychotics
Minor tranquilizers → anxiety and related disorders
Mental illness is understood to have biological roots, which has increased the role of science in psychopathology
Moral Therapy
Treated institutionalized patients as normally as possible in a setting that encouraged and reinforced normal social interaction
Declined in use due to the size and composition of the institutionalized population
Immigration
The mental hygiene movement (Dorothea Dix) and an increase in the number of hospitalized patients
Biological tradition
If we can’t treat the body, and you still have a disorder, there is no trying for biological treatment
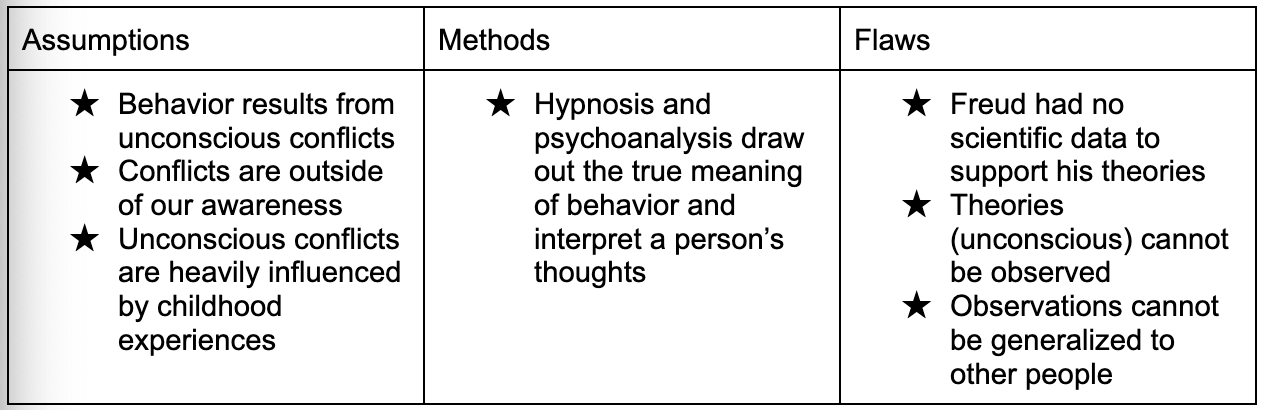
Psychoanalytic Theory (Freud)
The unconscious mind, intrapsychic conflicts
Id = maximizing pleasure. Illogical; emotional; irriational. Driven by pleasure principle
Superego = moral principles, conscience. driven by moral principles
Ego = mediates conflict between the id and superego. Logical;rational. Driven by reality principle
Defense mechanisms = unconscious protective processes that keep conflicts in check between the id and superego
Psychosexual stages of development = conflict arises at each stage and must be resolved
Id
maximizing pleasure. Illogical; emotional; irriational. Driven by pleasure principle
Superego
moral principles, conscience. driven by moral principles
Ego
mediates conflict between the id and superego. Logical;rational. Driven by reality principle
Defense Mechanisms
unconscious protective processes that keep conflicts in check between the id and superego
psychosexual stages of development =
conflict arises at each stage and must be resolved
Mechanism: Denial
refuse to acknowledge an aspect of objective reality
Mechanism: Displacement
transfers feelings about or a response to something that causes discomfort to another object or person
Mechanism: Projection
falsely attributes unacceptable feelings to another individual
Mechanism: Rationalization
conceals the true motivations for actions through elaborate reassuring or self-serving but incorrect explanation
Mechanism: Repression
blocks disturbing wishes, thoughts, or experience from conscious awareness
Historical Traditions: Psychological
Psychoanalytic Theory:
Ego psychology (Anna Freud)
Self-psychology (Heinz Kohut)
Collective unconscious (Carl Jung)
Inferiority/Superiority (Alfred Adler)
Psychoanalytic Psychotherapy:
Designed to reveal the nature of unconscious mental processes and conflicts through catharsis and insight
Techniques include free association (how you’re connecting ideas), dream analysis, and analysis of transference (how you interpret what your therapy is doing, in which you attribute things to the therapist and vice versa)
Psychodynamic Psychotherapy
Focus on expression of emotions
Exploration of attempts to avoid topics or engage in activities that hinder the progress of therapy
Identification of patterns in actions, thoughts, feelings, experiences, and relationships
Emphasis on past experiences and focus on interpersonal experiences
Emphasis on the therapeutic relationship
Humanistic Therapy:
Hierarchy of needs (Abraham Maslow)
Self-actualization: desire to become the most that one can be (top)
Esteem: respect, self-esteem, status, recognition, strength, freedom
Love and belonging: friendship, intimacy, family, sense of connection
Safety needs: personal security, employment, resources, health, property
Physiological needs: air, water, food, shelter, sleep, clothing, reproduction (bottom)
Emphasis on unconditional positive reg empathy, and innate tendency toward growth (Carl Rogers)
Hopeful for those dealing with life stressors
Cognitive-Behavioral
Classical Conditioning (Pavlov)
A learning process where an involuntary response to a natural stimulus becomes associated with a previously neutral stimulus. Examines how behaviors emerge through associations between stimuli.
Fear Conditioning (Watson)
Desensitizing your fears
Behavior Therapy
Systematic desensitization (phobias)
Exposure therapy is what helps us decrease our symptoms
Operant conditioning (Skinner)
Type of learning where behaviors are learned through consequences, either by increasing or decreasing their frequency
Schedules of Reinforcement Type: Fixed ratio
Explanation: reinforcement after a specific number of times
Schedules of Reinforcement Type: Fixed Interval
Explanation: reinforcement after a specific length of time
Schedules of Reinforcement Type: Variable Ratio
Explanation: reinforcement after a variable number of times
Schedules of Reinforcement Type: Variable interval
reinforcement after a variable length of time
Psychology Today:
Use more rigorous scientific methods
Know not one influence occurs in isolation
Biological, psychological, sociocultural
Thoughts, feelings, and behaviors
One-Dimensional Models:
Biological model
Explain behavior in terms of a single type of cause
Ignoring other pieces of information
Linear
Multidimensional Models:
Explain behavior from multiple influences
Systemic
Example influences on behavior include:
Biological
Behavioral
Emotional
Social + cultural
Environmental
Developmental
Genetic Contributions
Genes are molecules of DNA at various locations on chromosomes, within the cell nucleus
Genes are passed down
Key concepts:
dominant vs recessive genes
phenotype vs genotype
heritability
diathesis-stress
Genes typically account for <50% of variations in psychopathology
Adverse life events can overpower the influence of genes
Genetic contributions should not be considered without also considering the environment
Dominant vs recessive genes
Dominant: strongly influences a trait. Need only one of them to show up in order for us to have that trait
Recessive: must be paired with another recessive for it to show up
Phenotype vs. genotype
Phenotype: observable physical and biochemical characteristics such as appearance, development, and behavior
Genotype: complete set of genes, its genetic makeup
Heritability
How much variation in a given trait can be attributed to genetic variation
Ex: schizophrenia has high heritability. More likely to be related to genes.
Diathesis-stress vs epigenetics
Diathesis-stress:
Vulnerability to a disorder
Epigenetics:
Change in gene expression
Development and behavior are almost always polygenetic
Polygenetic: understanding of psychological traits and conditions, such as intelligence, personality, and mental health disorders, as being influenced by multiple genes rather than a single gene
Diathesis-Stress Model
Disorders are the result of underlying risk factors combining with life stressors that cause a disorder to emerge
Reciprocal Gene-Environment Model
Genes may increase the probability that an individual will experience stressful life events
Epigenetics
Environmental influences affect the expression of certain genes both for the individual and for their descendants
Cause chemical changes in our DNA
Neuroscience
Refers to the role of the nervous system in disease and behavior
Key Systems and Structures:
Central and peripheral nervous system
Neurons
The brain and its structures
Endocrine system
Nervous System —> Central nervous system (CNS)
brain, spinal cord
Nervous system —> Peripheral nervous system (PNS)
autonomic nervous system (ANS)
sympathetic division
parasympathetic division
somatic nervous system
Central Nervous System
Key to the CNS are neurons, which transmit information throughout the nervous system
Neurotransmitters:
Excitatory: increase the likelihood that the connecting neuron will fire
Inhibitory: decreases the likelihood that the connecting neuron will fire
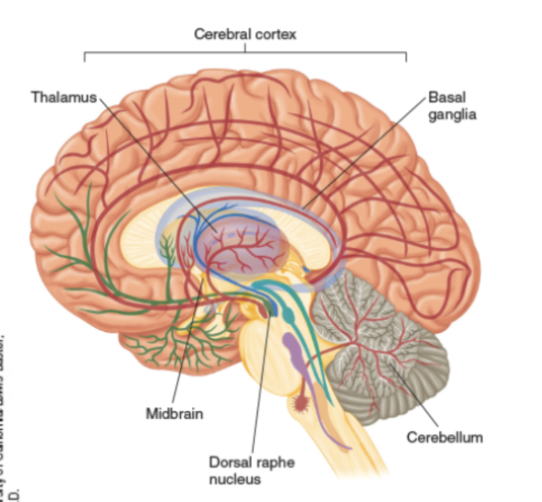
Brainstem (medulla, pons, cerebellum):
Handling automatic functions (breathing, sleeping, coordinated movement)
Thalamus and hypothalamus:
Regulating behavior and emotion
Limbic System:
regulating emotional experiences/expressions, our ability to learn to control our impulses, and our basic drives of sex, aggression, hunger, and thirst
Hippocampus
Memory
Amygdala:
Fear, aggression
Cingulate gyrus
Septum
Basil ganglia and caudate nucleus
Associated with Parkinson’s and Huntington's Disease
Controlling motor activity
Cerebral cortex:
Performing higher level functioning (thinking, language, memory, sensory)
Hemispheres:
Left: in control of the right side
Verbal, cognitive processes
Right: in control of the left side
Perception, creating images
Lobes:
Temporal
Recognizing sights and sounds, long-term memory storage
Parietal
Recognizing various sensations of touch, monitoring body positioning
Occipital
Visual inputs
Frontal
Higher cognitive functioning
The PNS (Peripheral Nervous System) coordinates with the brainstem to make sure the body is working properly
Somatic nervous system:
controls voluntary muscle movements
Autonomic nervous system:
controls our automatic or involuntary bodily functions
Regulate the cardiovascular system, endocrine system, digestion, and body temperature
Things we don’t think about that we do in everyday life are what the autonomic system controls
Somatic nervous system:
controls voluntary muscle movements
Autonomic nervous system:
controls our automatic or involuntary bodily functions
Regulate the cardiovascular system, endocrine system, digestion, and body temperature
Things we don’t think about that we do in everyday life are what the autonomic system controls
Sympathetic nervous system
Parasympathetic nervous system
Sympathetic nervous system:
Flight, fight, freeze
Mobilizes our body during times of stress or dangerous situations (by increasing heart rate, diverting blood to muscles, and releasing adrenaline, allowing more oxygen to the brain and limbs)
“Sympathizing” with the stress
Parasympathetic nervous system:
Balances the sympathetic nervous system
Energy conserving
Back to baseline, calms the body down, and has bodily functions operating as normal
“Rest and digest”, calms the body, slows heart rate, aids digestion, and promotes rest, recovery, and healing by using the neurotransmitter acetylcholine
Endocrine glands produce hormones (chemical messengers) and release them into the bloodstream
Adrenal glands: hormone —> epinephrine, cortisol —> function: energy in response to stress
Thyroid: hormone —> thyroxine —> function: energy metabolism and growth
Gonadal Glands: hormone —> estrogen, testosterone —> function: sexual functioning
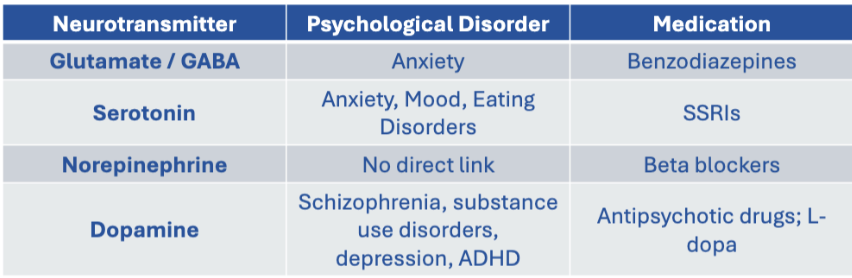
Neurotransmitters
chemical messengers that transmit messages between neurons
Main neurotransmitters include:
Glutamate
Gamma aminobutyric acid (GABA)
Serotonin
Norepinephrine
Dopamine
Impact functioning by introducing:
agonists: increase the activity of a neurotransmitter by mimicking its effects
Antagonists: decrease or block a neurotransmitter
Inverse agonists: produce effects opposite to the neurotransmitter
Psychiatric Medication
Examples of how psychiatric medication works to affect neurotransmitters include:
Increasing the flow of a specific neurotransmitter
Decreasing the flow of a specific neurotransmitter
Directly inhibiting or blocking the production of a neurotransmitter
Increasing the production of competing biochemical substances that may deactivate the neurotransmitter
Preventing the chemical from reaching the next neuron by closing down or occupying receptors in that neuron
Blocking the reuptake process
Glutamate + GABA
Glutamate = excitatory
GABA = inhibitory
The balance of glutamate and GABA determines whether a cell will fire or not
GABA has been studied extensively in relation to anxiety
Benzodiazepines (minor tranquilizers) make it easier for GABA molecules to attach themselves to the receptors of specialized neurons
Changing the way neurons talk to each other to decrease the symptoms of psychopathology
The calmer the person is
GABA reduces OVERALL arousal (not just anxiety)
Serotonin
influences many of our behaviors, including regulation of mood, behavior, and thought processes
Low levels of serotonin are associated with impulsivity
Aggression, suicide, overeating, and obsessive sexual behaviors
Selective serotonin reuptake inhibitors (SSRIs) affect the serotonin system
SSRIs are used to treat anxiety, mood, and eating disorders
Norepinephrine
stimulates alpha-adrenergic and beta-adrenergic receptors
May be associated with panic, but likely not directly involved in specific psychological disorders
Beta blockers block beta receptors so that their response to a surge of norepinephrine is reduced
Response to a surge of norepinephrine is reduced. Keeps blood pressure low, heart rate lower
Dopamine
has been connected to several mental health disorders, including schizophrenia, substance use disorders, depression, and ADHD
Dopamine turns on various brain circuits, possibly associated with certain types of behaviors; once the switch is turned on, other neurotransmitters may then inhibit or facilitate emotions/behavior
Associated with exploratory, outgoing, pleasure-seeking behaviors
Balances out serotonin
L-dopa (drug for Parkinson’s disease) impacts dopamine circuits (switching on the locomotor circuit)
Neurotransmitters and their relevance to psychopathology
Implications for Psychopathology
Understanding the brain is critical to understanding psychopathology, but it does not explain the sole cause of any disorder
Damage to an area of the brain
Increased/decreased activity in an area of the brain
Too much/too little of a neurotransmitter
Other Influences on Brain Structure + Function
Neurological activity may be influenced by:
Psychotherapy
Placebos
Stress and early development
Gut health
Paradigm
A framework or model that shapes how individuals view and understand a field
It guides research and treatment
They make sense of complex phenomena
Paradigms have different assumptions, methods, and communities of scholars
Biological Paradigm
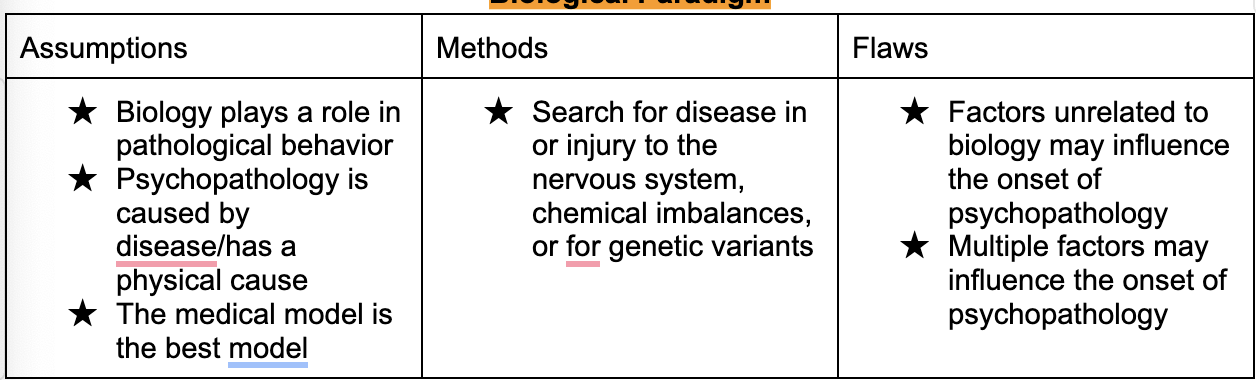
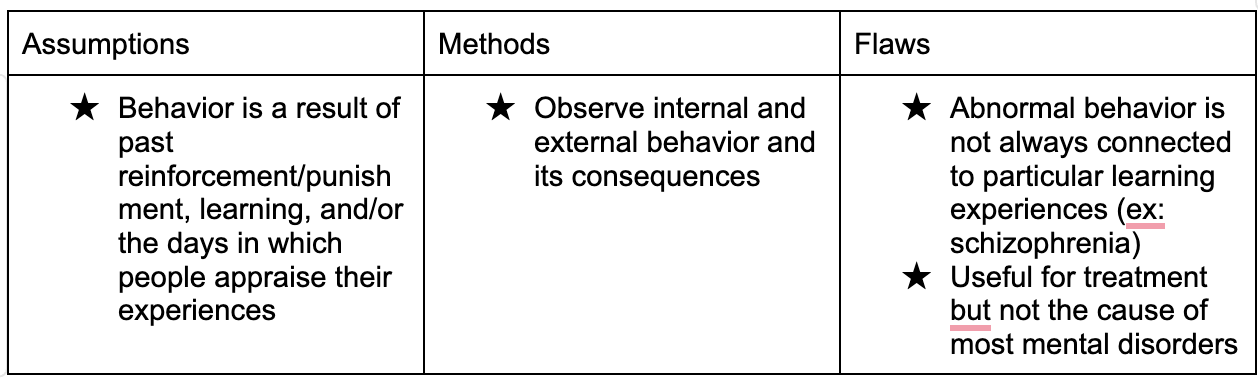
Behavioral and Cognitive Science
Cognitive science refers to how we acquire and process information, and how we store and retrieve information
Social learning
Prepared learning (evolution)
Ex: food poisoning. Not likely to want to eat that food again. Your body inherently learns not to eat something that made you sick.
Implicit memory
Type of unconscious, non-declarative long-term memory that influences behavior and performance without conscious recall of past experiences
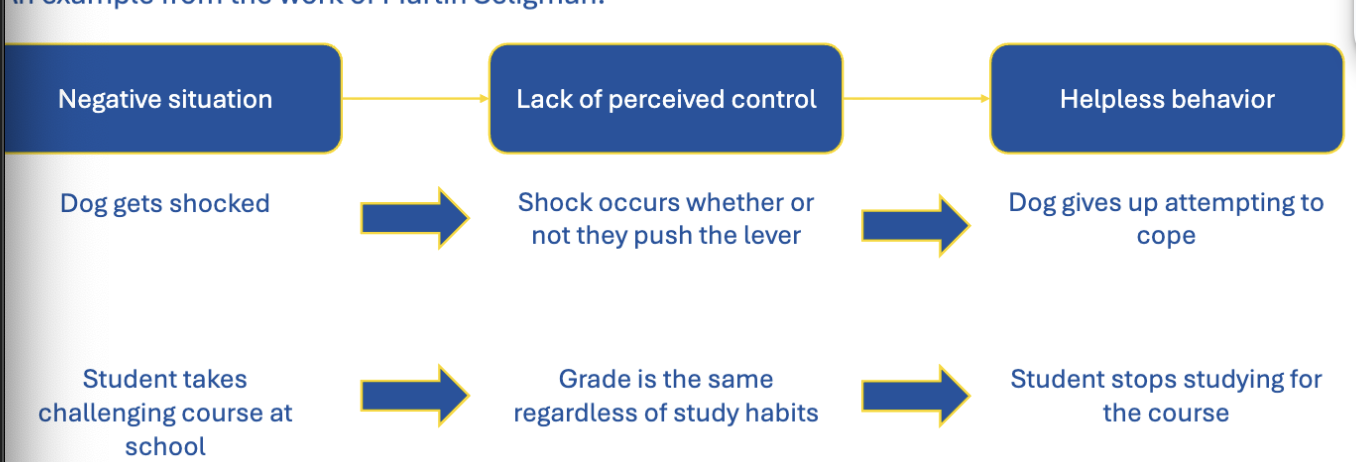
Example: Learned Helplessness
An example from the work of Martin Seligman
Emotions
Another contributor to the development of psychopathology, sometimes included in the cognitive behavioral perspective, is emotions
Emotion = a feeling state that is strong lived, and in response to an external event
Behavioral, cognitive, physiological
Behavioral and Cognitive Paradigm
Psychodynamic Paradigm
One-Dimensional vs. Multidimensional Models
One-Dimensional
Explain behavior in terms of a single type of cause
Linear
Multidimensional
Explain behavior from multiple influences
Systemic
We want more of this approach when looking at psychopathology
Biopsychosocial Model
Biological
Genetics and genetic vulnerability
Physical health
Brain chemistry
Disease or injury
Exposure to toxins
Psychological
beliefs/thoughts
Emotions
Behaviors
Coping skills
Prior history of mental health
Sociological:
Family relationships
Peer relationships
Cultural background
Cultural beliefs about mental health
Biopsychosocial Assessment
We can use the biopsychosocial model to better understand the etiology and symptoms of mental health disorders through clinical interviewing
Clinical interview:
A process meant to gather pertinent information for making a diagnosis and planning for treatment
Biological:
Family history
Physical health, injury
Medications
Substance use
Psychological
Current thoughts, feelings, behaviors
Early childhood adversity
Current life stressors
History of mental health symptoms or disorders
Social
Peer relationships
Family relationships
social/support/community
College environment
Cultural understanding of anxiety
Imagine that an 18-year-old female college student presents to your clinic with symptoms of anxiety. If you are adhering to the biopsychosocial model, what questions might you ask to better assess the etiology and presentation of the disorder?
general health and history
family and genetic history
symptom exploration
cognitive patterns
college and academic life
relationships and social support
cultural and personal context questions
Takeaways from Module 2
There are multiple approaches to understanding the causes of psychopathology that impact how we think about, diagnose, and treat mental health disorders
One-dimensional versus multidimensional
Biological, cognitive/behavioral, psychoanalytic paradigms
Biopsychosocial model
Defining Psychopathology:
Recall the DSM definition:
“Behavioral, psychological, or biological dysfunctions that are unexpected in their cultural context and associated with present distress and/or impairment in functioning, or increased risk of suffering, death, pain, or impairment”
Why classify behaviors as mental disorders?
The goal of a classification system is to subdivide or organize a set of physical or mental conditions
DSM + ICD are based on symptom presentations, “prototypes”
These systems do not propose cause “etiology”
Access to knowledge base and research
Informs treatment decisions
Validates concerns (ex: PTSD)
Treatment access and development (ex: internet gaming disorder)
Insurance
Disability payments
Accommodations
Benefits
Creates a shared language (including for providers)
Aids treatment decision-making
Facilitates research on etiology and treatment
Necessary for insurance reimbursement
Drawbacks
Risks reducing people to “simple” labels
Can affect others’ beliefs or expectations about abilities
Unrelated problems can be misattributed to the disorder
Approaches to Classification
Categorical: assumes or suggests qualitative differences
objects/concepts differ in kind
Each represents a distinct type of something
Dimensional
Focuses on quantitative differences
obejcts/concepts differ in degree
All exist in one continuum
Where does the DSM fall?
Mostly categorical
Meets criteria
Also dimensional
Changes in the DSM-5
Introduces dimensional axes rating:
Severity
Intensity
Frequency
Duration
AND new understanding of some diagnoses as existing on a spectrum
Ex: autism spectrum disorder, schizophrenia spectrum disorder
A third approach
A prototypical approach:
Identifies essential characteristics
Allows nonessential variations
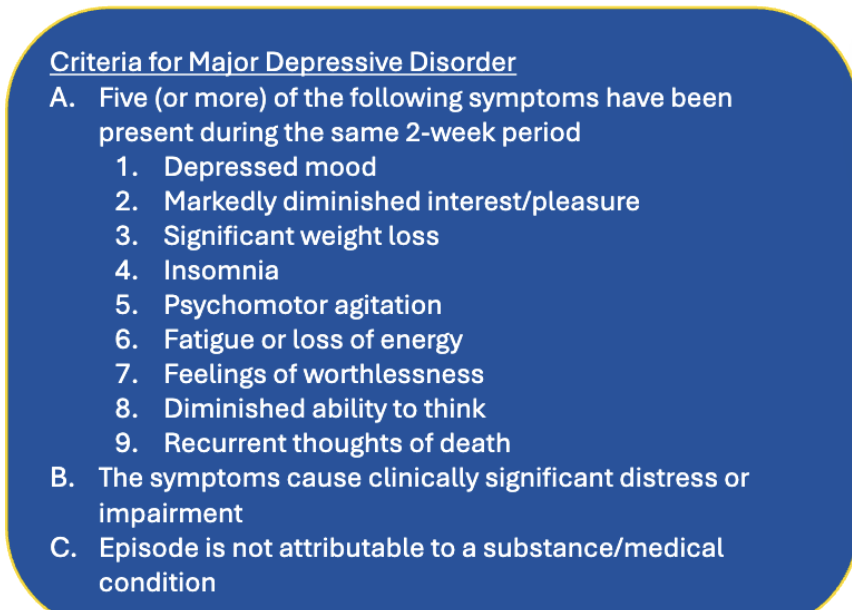
How is a diagnosis made?
Diagnoses are made by skilled clinicians based on:
Number of symptoms
arbitrary
How long the symptoms have lasted
arbitrary
Whether the symptoms cause distress or functional impairment
Subjective
Clinical Assessment
The systematic evaluation and measurement of psychological, biological, and social factors in an individual presenting with a possible psychological disorder
Clinical interview
Behavioral assessment
Psychological testing
Neuropsychological testing
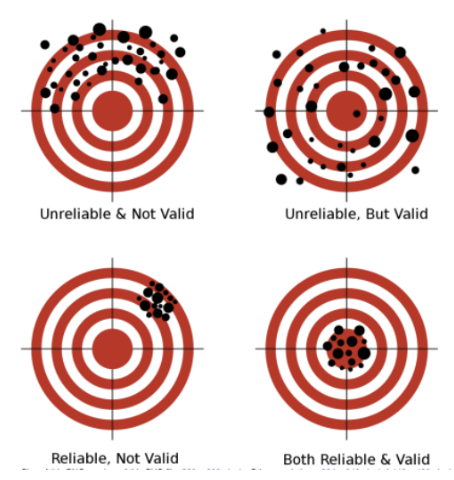
Reliability
The degree to which a measurement is consistent
Interrater reliability:
Consistency across multiple rates
Test-retest reliability:
Consistency across multiple times taking a test
Validity:
The degree to which a measurement measures what it is supposed to measure
Concurrent validity: how well a new measure aligns with the “gold standard”
Predictive validity: how well a score predicts future outcomes
Standardization
The process by which a certain set of standards or norms is determined so that the test-taker is compared to similar test-takers
Clinical Interview
Process is meant to gather pertinent information for making a diagnosis and planning for treatment
Presenting problem
Detailed history (development, social history, etc)
Attitudes and emotions
Current and past behavior
Clinical Interview: Unstructured
Clinical Interview: Semi-Structured
Carefully phrased and tested questions that elicit useful information in a consistent manner
Advantages
Clinician can feel confident that a semi-structured interview will accomplish its purpose
Disadvantages
Loss of spontaneity
May inhibit the patient from volunteering useful information that is not directly relevant to the questions being asked
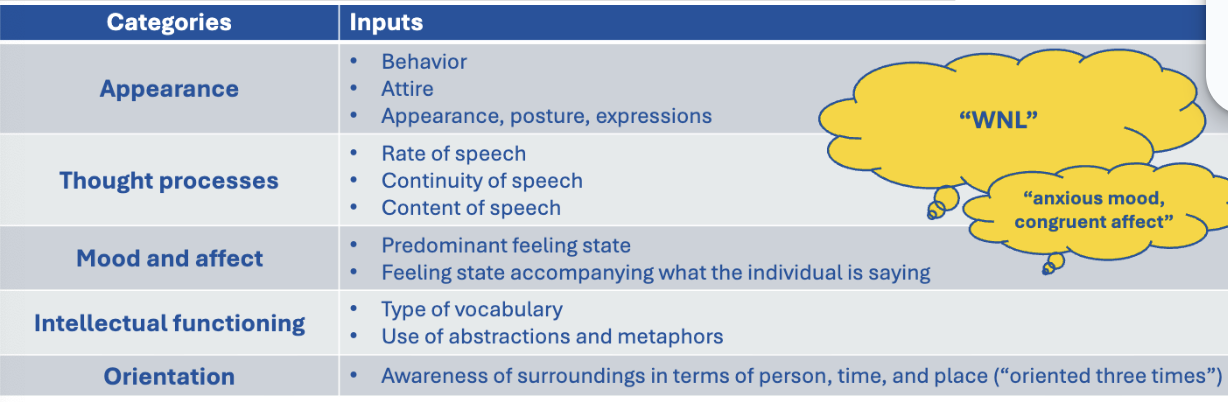
Clinical Interview: The Mental Status Exam
During most client encounters, clinicians perform the mental status exam
Behavioral Assessment
Allows us to use direct observation to formally assess an individual’s thoughts, feelings, and behaviors in a specific situation or context
Antecedents: what happened before the behavior?
Behavior: What was the behavior?
Consequences: what happened after the behavior?
Behavioral Assessment: Rating Scale
We can also observe behavior through checklists and behavior ratin scales
Self rating scale
Parent rating scale
Teacher rating scale
Pscyhological Testing:
Tools to determine cognitive, emotional, or behavioral responses that might be associated with a specific disorder
More general tools that assess long-standing personality features
Psychological Testing: Projective Tests
Theory: people project their own personality and unconscious fears onto other people and things (ex: ambiguous stimuli)
Rorschach inkblot test
Thematic apperception test
Sentence completion test