CH18 - Host defenses
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
What is adaptive immunity?
Adaptive immunity is your body's learned defense against specific germs.
First exposure: slow primary response
Later exposures: fast and strong secondary response
It has specificity (targets exact invader) and memory (remembers it for next time).
What are the two main branches of adaptive immunity?
Humoral immunity – B cells make antibodies to fight invaders in body fluids.
Cellular immunity – T cells attack infected or abnormal cells directly.
What makes each naïve B or T cell unique?
Each naïve B/T cell has a unique receptor created by VDJ recombination, a random DNA-cutting and splicing process during development in the bone marrow.
creates a huge variety of antigen receptors, so the immune system can recognize many different threats.
What happens when a naïve B or T cell is activated?
The cell undergoes clonal expansion, making many identical copies that have the same specific receptor to fight the detected threat.
What are memory B and T cells?
Some activated B/T cells become memory cells that stay in the body.
If the same pathogen returns, they quickly clonally expand again, making a faster and stronger secondary immune response.
Do all the daughter cells from a stimulated B/T cell have the same receptor?
Yes. All cells made from a specific B or T cell have the same receptor as the original one, created by VDJ recombination.
steps of humoral immunity
macrophages engulfs the pathogen
presents the pathogen’s antigen MHC
T helper activation
B cell activation
B cells turn into plasma cells and B memory cells
plasma cells secrete antibodies
What are antigens, epitopes, and how are they related to antibody structure?
Antigens (immunogens): Trigger adaptive immune responses
Epitopes: Small regions on an antigen that are recognized by antibodies or T-cell receptors
Antibody (e.g., IgG):
Made of 4 chains (2 heavy, 2 light)
Has Y-shape
Variable regions bind to specific epitopes
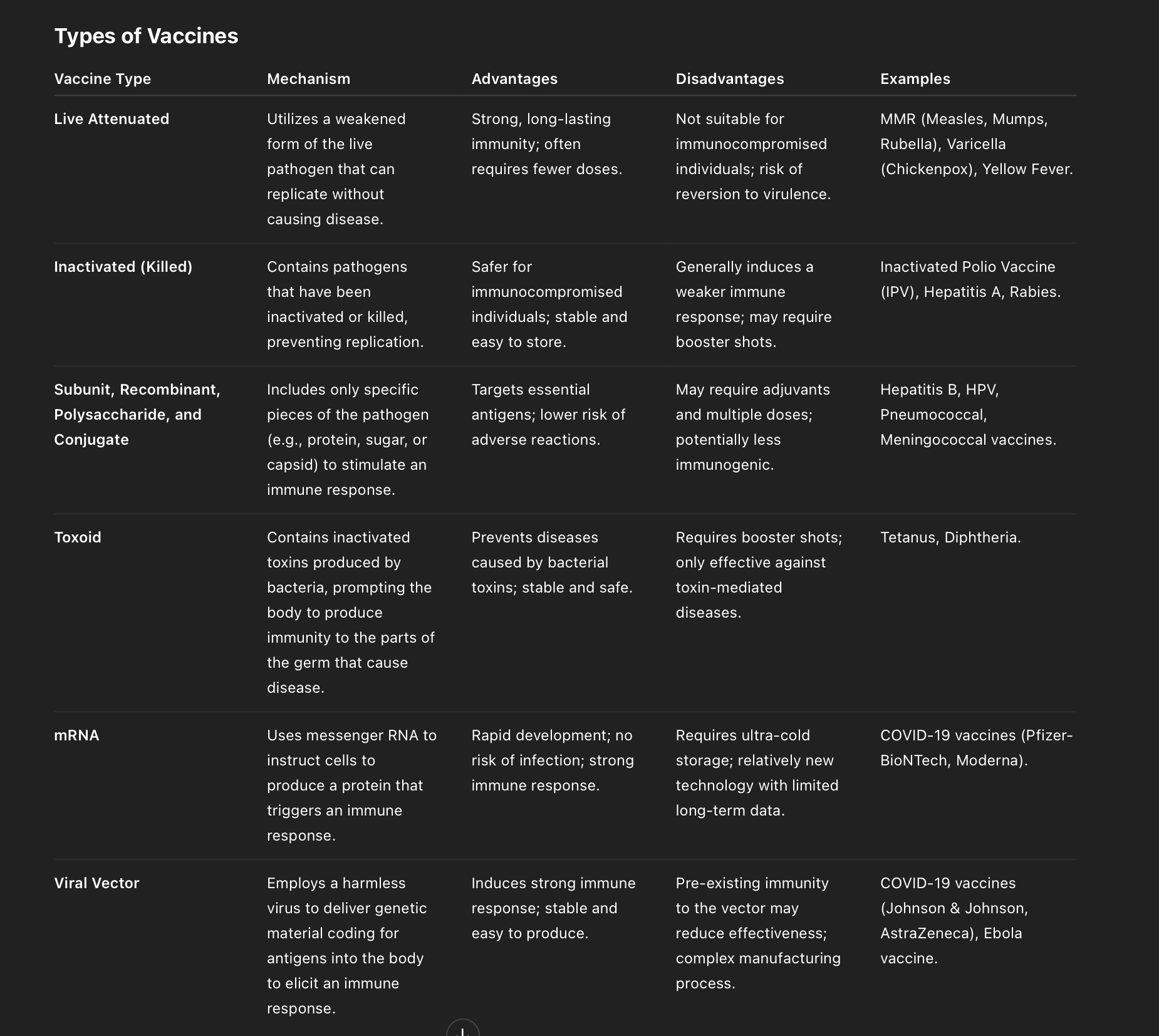
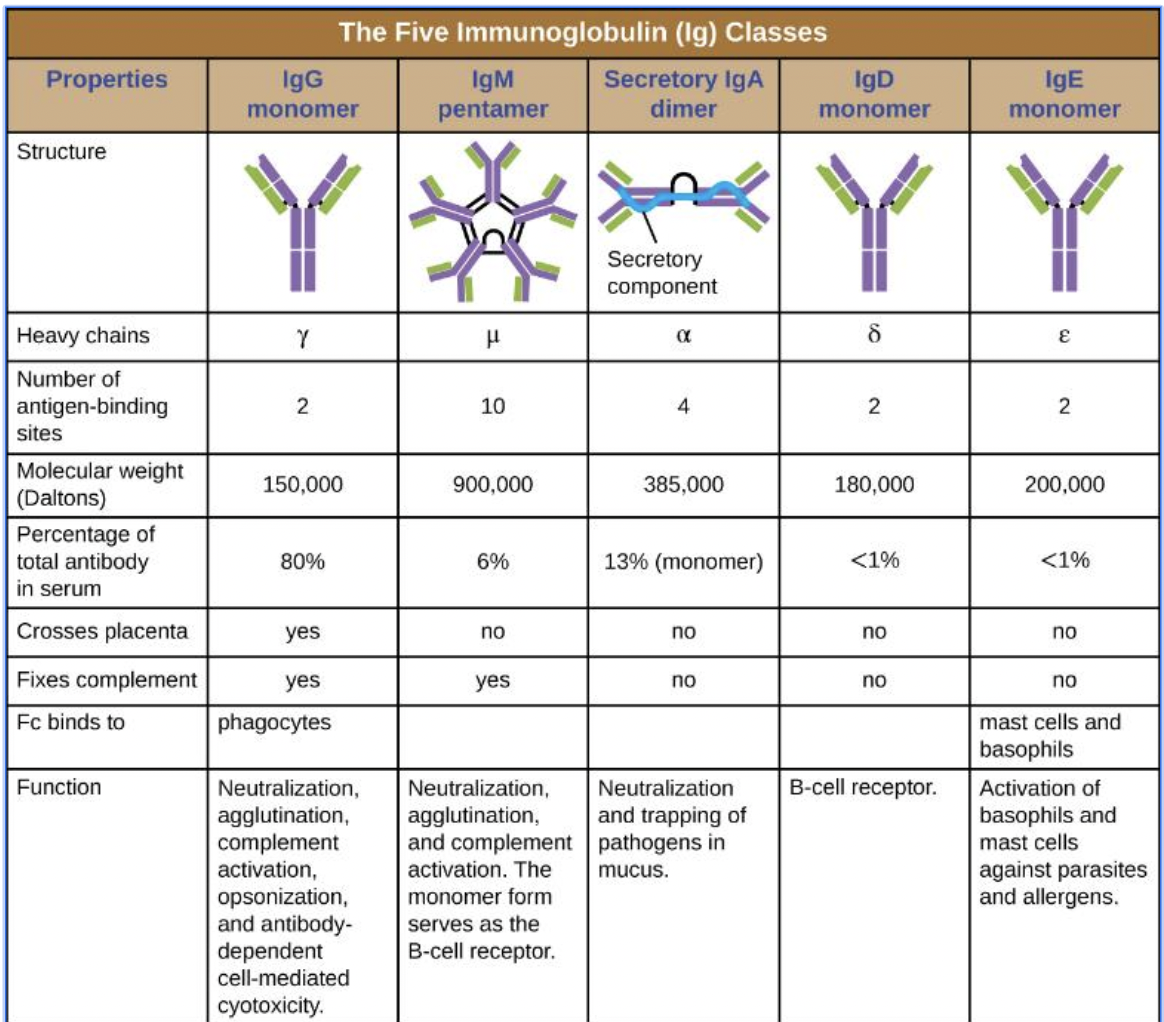
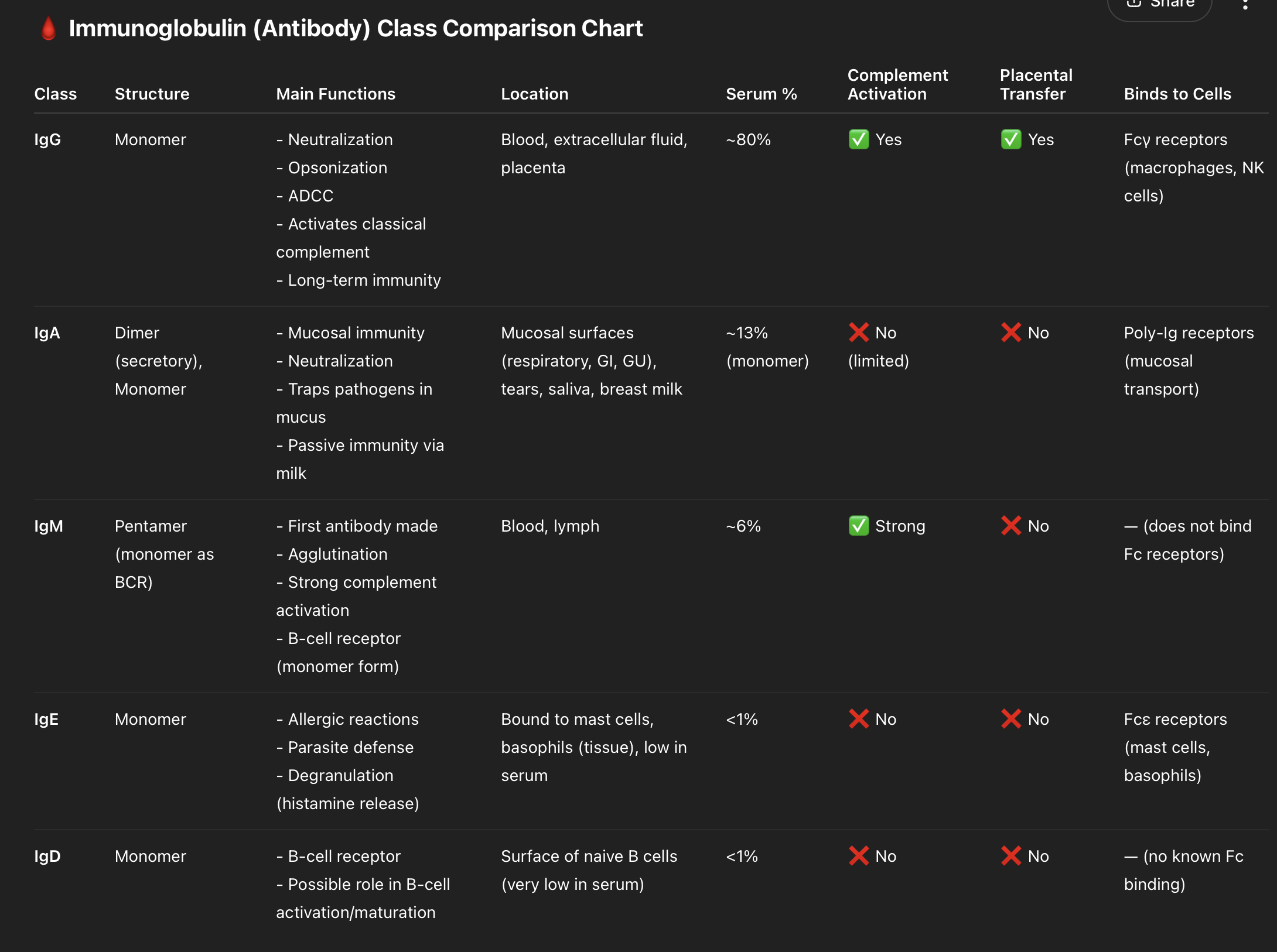
"GAMED" – The 5 antibody types
G – IgG, A – IgA, M – IgM, E – IgE, D – IgD
🧠 IgG – "Greatest amount"
Mnemonic: "G = General-purpose"
Most abundant (80%)
Crosses placenta
Does everything: Neutralization, opsonization, complement, etc.
🧠 IgA – "Airways and mucosa"
Mnemonic: "A = sAliva, teArs, mucosA"
Secretory dimer, traps pathogens in mucus
Found in mucosal surfaces (GI, respiratory)
🧠 IgM – "Massive first responder"
Mnemonic: "M = Mega pentamer, Main early antibody"
Largest (pentamer), 10 binding sites
First made in response
Strong in agglutination and complement
🧠 IgE – "Eosinophils & allergy"
Mnemonic: "E = Explode in allergies"
Binds to mast cells & basophils
Triggers allergic reactions & fights parasites
🧠 IgD – "Don't know much"
Mnemonic: "D = Dumb mystery receptor"
Low quantity, role unclear
Functions mainly as B-cell receptor
neutralization
involves binding specific antibodies to antigens found on bacteria, viruses, or toxins, blocking their harmful effects and preventing infection or damage.
How do antibodies function as opsonins in the immune response?
T – Tag the pathogen (with antibody igG)
A – Attach via Fc receptor (phagocytic ) x Fc region of IgG of pathogens
G – Grab and engulf (phagocytosis)
agglutination
clumping (agglutination) of pathogens
IgM antibodies have 10 antigen-binding sites (pentamer)
They bind to multiple bacteria simultaneously via epitopes
This leads to clumping (agglutination) of pathogens
Aggregates form when multiple antibodies cross-link different pathogens
What is (ADCC) and how do NK cells contribute?
Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC)
A – Antibodies attach to large pathogen
D – Direct NK cell via Fc receptor binding x Fc region of pathogen
C – Close contact between NK and target
C – Cytotoxins released to kill the invader
Antibodies comparison
cell mediated immune response ATCTR
A – Antigen presentation (dendritic cells capture antigen from infected cells and present to MHC I CD8 and MHC II CD4)
T – T cell activation
CD8 T cells: costimulation from APCs and IL-2 from CD4
CD4 T cells: become activated helper T cells
C – Clonal expansion
cytotoxic T cells: kill - CD8 cell mediate immune
helper T cells: secrete cytokines - CD4 humoral
memory T cells: long-term immunity - CD4 humoral
T – Target killing
R – Regulation & memory
dendritic cells process and present bacterial antigens to activate T cells?
“Please Let Dendrites Present My Target”
P – Phagocytosis: Dendritic cell phagocytoses a bacterial cell into a phagosome
L – Lysosome fusion: form phagolysosome
D – Degradation: Antimicrobial enzymes degrade the bacterium
P – Processing (by proteases): Proteases process antigens → select epitopes
M – MHC II loading: Epitopes are loaded onto MHC II molecules
T – T cell activation: Presented on the surface to CD4⁺ helper T cells, which are activated
MHC I found where
all nucleated body cells
antigen binding cleft of MHC I is formed by domain alpha 1 and alpha 2
endogenous produced proteins to CD8 T cells
cell mediated immunity
MHC II found where
found on macrophages, dendritic cells, and B cells
antigen binding cleft MHC II formed by domains alpha 1 and beta 1
Exogenous/Phagocytized antigens to CD4 T cells
humoral immunity
red bone marrow where and function
found on head of femur (thighbone), and flat bones )ilium, scapula_
production and differentiation of many blood elements (RBCs, leukocytes, platelets)
yellow bone marrow
adipose cellsi
immature T lymphocytes
produced in red bone marrow
travel to thymus for maturation
structure of thymus
Thymus is a bi-lobed, H-shaped gland above the heart
Surrounded by a fibrous capsule (connective tissue)
Each lobe has lobules with:
Dark cortex (dense with immature T cells)
Light medulla (fewer, mature T cells)
Key site for T cell maturation
Prominent in newborns; shrinks with age (involution)
steps of thymic selection Pass, Fail, Fly"
Pass – Positive selection: keep MHC-recognizers
Fail – Negative selection: kill self-reactors
Fly – Mature T cells exit thymus
Thymic selection ensures only functional, non-self-reactive T cells mature:
✅ Step 1: Positive Selection
Purpose: Keep T cells that can recognize self-MHC
Kill T cells that do not bind MHC at all
Occurs in thymic cortex
❌ Step 2: Negative Selection
Purpose: Eliminate T cells that bind too strongly to self-antigen/MHC
Kill T cells that could cause autoimmunity
Occurs in thymic medulla
🩸 Step 3: Maturation/Export
Surviving T cells become naive, mature CD4⁺ or CD8⁺ T cells
Exit thymus to enter peripheral circulation
cytotoxic T cell function
activated by MHC I on infected body cell
release perforin and granzymes that invade infected ells => apoptosis/death
Superantigen Activation
Superantigen bypasses normal recognition
Bridges MHC II and TCR directly, even without antigen specificity
Causes massive, non-specific T cell activation
Leads to cytokine storm and excessive inflammation
What happens during T cell-dependent activation of B cells?
Antigen Recognition: B cell binds to specific antigen via BCR.
Antigen Processing: B cell internalizes and presents antigen on MHC II.
T Cell Interaction: Helper T cell recognizes the same antigen via TCR + MHC II.
Cytokine Release: Activated T cell secretes cytokines.
B Cell Activation: Cytokines stimulate B cell.
Outcome: B cell proliferates and differentiates into memory B cells and plasma cells (antibody producers).
How do T-independent antigens activate B cells?
Antigen Structure: Repeating epitopes on T-independent antigens cross-link BCRs.
No T Cell Help Needed: Activation occurs without T cell interaction.
Second Signal: Often requires innate signal (e.g., TLRs binding PAMPs).
B Cell Response: Activation leads to proliferation and differentiation into plasma cells.
Outcome: Rapid antibody production, mainly IgM; no memory cell formation.
4 types of immunity
passive nature: acquired from antibodies pass in breast milk and placenta
passive artificial: gained from another person/animal
active natural: gained through illness and recovery
active artificial: vaccine
edward jenner
cowpoxvaccination technique to prevent smallpox
types of vaccine