NS502 2
1/445
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
446 Terms
What are the two types of cholinergic receptors?
Muscarinic and Nicotinic receptors.
Name four adrenergic receptors.
Alpha-1, Alpha-2, Beta-1, and Beta-2 receptors.
What is the primary function of the sympathetic division of the autonomic nervous system (ANS)?
Response to emergencies and the need for energy expenditure, promoting 'fight or flight' and inhibiting non-essential activities.
What is the primary function of the parasympathetic division of the ANS?
Restoration and conservation of body energy, promoting 'rest and digest' functions.
What does it mean for organs to have dual innervation?
It means that the organs receive impulses from both sympathetic and parasympathetic fibers.
What type of medication stimulates adrenergic receptors?
Adrenergic agonists, such as adrenaline.
What type of medication inhibits beta adrenergic receptors?
Beta-blockers.
What is an anticholinergic medication?
A cholinergic antagonist that inhibits cholinergic receptors.
How does the sympathetic division affect body systems compared to the parasympathetic division?
The sympathetic division affects more body systems than the parasympathetic division.
What is the role of chemical synapses in the ANS?
Chemical synapses facilitate the transmission of impulses between neurons, which is essential for understanding how medications work at the synapse.
What is the 'fight or flight' response associated with?
It is associated with the sympathetic division of the autonomic nervous system.
What is the 'rest and digest' response associated with?
It is associated with the parasympathetic division of the autonomic nervous system.
What is the significance of the stages of transmission at the synapse?
Understanding these stages is crucial for comprehending how medications affect synaptic transmission.
What is the effect of stimulating adrenergic receptors?
It typically results in increased heart rate, blood pressure, and energy expenditure.
What is the effect of inhibiting cholinergic receptors?
It generally leads to reduced parasympathetic activity, affecting functions like digestion and salivation.
What causes increased sympathetic discharge?
Increased sympathetic discharge is caused by physical or emotional stress, often referred to as 'E' situations: emergency, embarrassment, excitement, and exercise.
What is the fight or flight response?
The fight or flight response includes increased heart rate and blood pressure, increased blood flow to cardiac muscle, skeletal muscle, liver, and adipose tissue, decreased blood flow to kidneys and GI tract, dilation of airways, decreased mucus production, pupil dilation, decreased GI motility, release of adrenaline, and increased blood glucose levels.
What are adrenergic receptors activated by?
Adrenergic receptors are activated by noradrenaline and adrenaline.
What types of receptors do noradrenaline and adrenaline bind with?
Noradrenaline and adrenaline bind with both alpha receptors and beta receptors.
What effects do adrenergic drugs produce?
Adrenergic drugs produce effects similar to those produced by the sympathetic nervous system.
What determines the effect produced by adrenergic drugs?
The effect produced by adrenergic drugs depends on the type of receptor activated and the number of affected receptors in the tissue.
What is an agonist in pharmacology?
An agonist is a substance that binds to and activates a receptor, mimicking the effect of a natural neurotransmitter or hormone.
What is an antagonist in pharmacology?
An antagonist is a substance that binds to and blocks a receptor, thereby preventing a natural neurotransmitter or hormone from having an effect.
What are sympathomimetic drugs?
Sympathomimetic drugs, also known as sympathetic agonist drugs, mimic the effects of stimulation by the sympathetic nervous system, examples include adrenaline and noradrenaline.
What are sympatholytic drugs also known as?
Sympathetic antagonist drugs.
What is the primary action of adrenoreceptor agonists?
They mimic the effect of sympathetic stimulation.
What are the effects of adrenaline on the body?
Increased cardiac contractility, increased heart rate, increased blood pressure, and bronchodilation.
What is the effect of noradrenaline on blood pressure?
It increases blood pressure.
What does Salbutamol stimulate and what is its effect?
It stimulates β2 receptors to cause bronchodilation.
What are the main effects of beta antagonists (beta blockers)?
Decrease heart rate, decrease myocardial contractility, decrease blood pressure, and decrease speed of impulse through the AV node.
What is the purpose of alpha antagonists in treatment?
They are used for the treatment of hypertension and urinary obstruction.
What does increased parasympathetic discharge lead to?
Conservation and restoration of body energy during times of rest.
What does the 'rest-and-digest' response include?
SLUDD: salivation, lacrimation, urination, digestion, defecation, and decreases in heart rate, airway diameter, and pupil diameter.
What neurotransmitter do cholinergic neurons release?
Acetylcholine (ACH).
What types of receptors does acetylcholine bind to?
Nicotinic receptors and muscarinic receptors.
Where are muscarinic receptors located?
In effectors innervated by parasympathetic nerves, including smooth muscle, cardiac muscle, lungs, and glands.
Where are nicotinic receptors located?
In the cells of adrenal medullae and neuromuscular end plates of skeletal muscles.
What are muscarinic agonists also known as?
Parasympathomimetics or cholinergics.
What is the effect of muscarinic receptor antagonists?
They block the parasympathetic response.
What is the action of Ipratropium?
It causes bronchodilation by blocking the parasympathetic response in the bronchioles.
What are the general effects of the autonomic nervous system (ANS) on organs/tissues?
The ANS regulates involuntary bodily functions, including heart rate, digestion, and respiratory rate.
What is the significance of the term 'negative chronotrope' in relation to beta blockers?
It refers to the ability of beta blockers to decrease heart rate.
What is the significance of the term 'negative inotrope' in relation to beta blockers?
It refers to the ability of beta blockers to decrease myocardial contractility.
What is the role of cholinergic receptor antagonists in pharmacology?
They block the effects of the parasympathetic nervous system.
What is the clinical use of muscarinic agonists?
They are very few in clinical use, with Pilocarpine being an example.
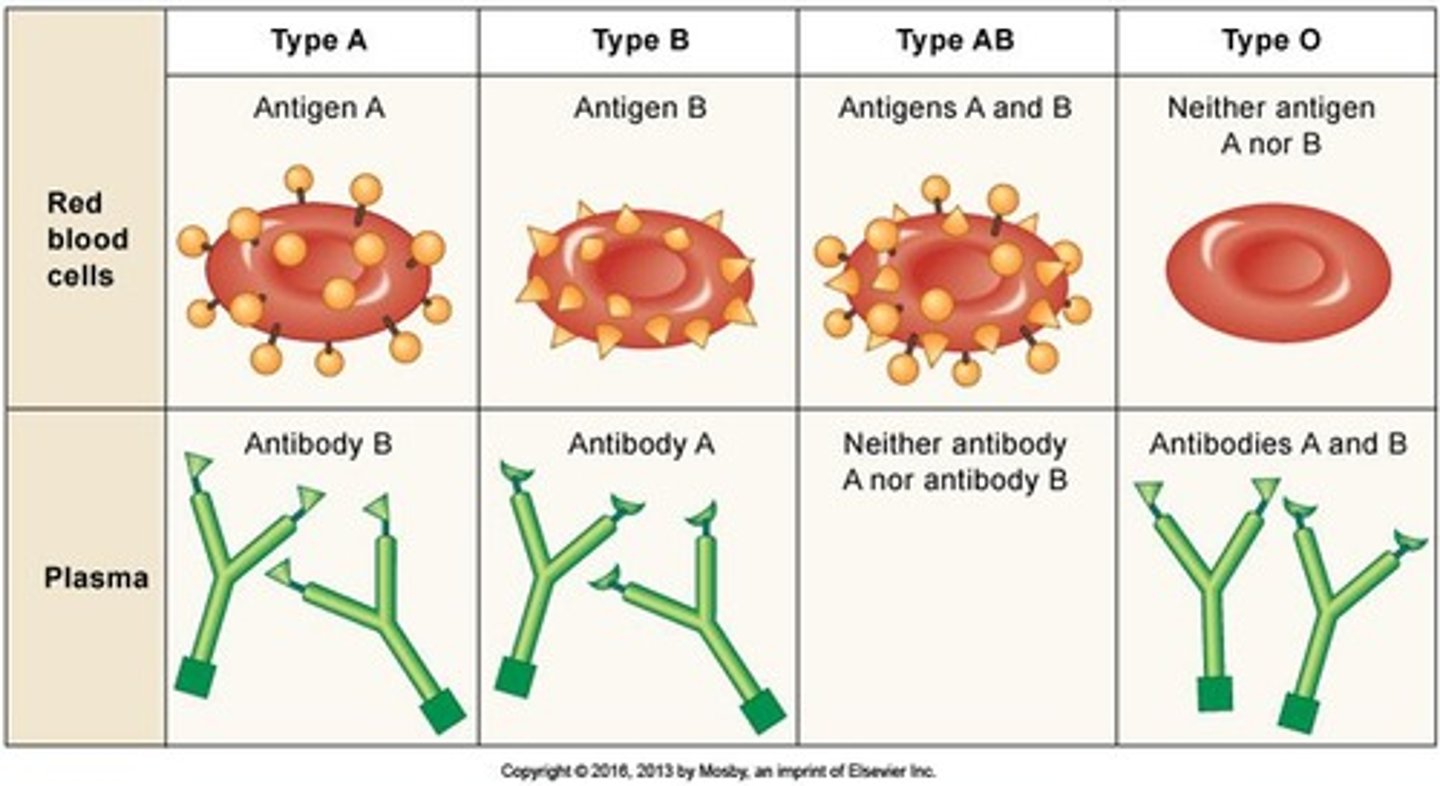
Why are ABO blood groups important during blood transfusions?
ABO blood groups determine the presence or absence of A and B antigens on red blood cells, which is crucial to avoid immune reactions during transfusions.
What are the three main processes involved in the homeostatic response to blood loss?
Vasoconstriction, platelet plug formation, and coagulation (blood clotting).
How long does bleeding normally stop in adults and children?
Bleeding normally stops within 1-9 minutes in adults and 1-13 minutes in children.
What is prothrombin time and why is it important?
Prothrombin time measures the time it takes for blood plasma to clot, important for assessing patients on anticoagulant therapy.
What are the effects of the sympathetic nervous system during blood loss?
It increases heart rate, strength of contraction, cardiac output, constriction of veins, venous return, and peripheral resistance.
What is the purpose of whole blood transfusions?
Whole blood transfusions are indicated for rapid and substantial blood loss.
What is re-suspended red cells and when is it used?
Re-suspended red cells consist of blood with plasma removed and replaced by an additive solution, used to restore oxygen-carrying capacity from severe blood loss or severe anemia.
What is autologous blood transfusion?
An autologous blood transfusion is when a patient receives a transfusion of their own blood.
What factors are considered before a blood transfusion?
Volume of blood lost, ongoing blood loss, risk of anemia, patient's hemoglobin level, symptoms of hypoxia, and risks associated with transfusion.
What are antigens in the context of blood?
Antigens are specific glycoproteins on the surface of body cells that identify individuals and can trigger an immune response.
What happens if a person with A antigens receives blood from a donor with B antigens?
The immune system will respond by destroying the donated red blood cells.
How are ABO blood groups categorized?
ABO blood groups are based on the presence or absence of A antigens and/or B antigens on red blood cells.
What blood group is assigned to a person with A antigens on their RBC?
Group A.
What blood group is assigned to a person with B antigens on their RBC?
Group B.
What is the role of vasoconstriction in the homeostatic response to blood loss?
Vasoconstriction reduces blood flow to minimize blood loss.
What is the significance of platelet plug formation?
Platelet plug formation is crucial for sealing small breaks in blood vessels to prevent excessive bleeding.
What is coagulation in the context of blood loss?
Coagulation is the process of blood clotting that helps to stop bleeding.
What is the main goal of a blood transfusion?
To deliver adequate amounts of oxygen to tissues.
What is the importance of assessing a patient's hemoglobin level before a transfusion?
It helps determine the risk of anemia and the need for a transfusion.
What is the role of adrenaline in response to blood loss?
Adrenaline increases heart rate and cardiac output, aiding in the body's response to blood loss.
What is the typical time frame for bleeding to stop in adults?
1-9 minutes.
What is the typical time frame for bleeding to stop in children?
1-13 minutes.
What blood group is categorized for a person with both A and B antigens?
AB
What blood group is categorized for a person with no A or B antigens?
O
What do ABO antibodies in plasma do?
They develop early in childhood to attach to foreign antigens and do not target our own antigens.
What is the difference between typing and cross-matching in blood transfusions?
Typing identifies the blood group, while cross-matching mixes donor and recipient blood to check for compatibility.
What can result from incompatible blood transfusions?
Serious harm or death, with severe reactions likely occurring within 15 minutes of starting the transfusion.
What is a universal donor blood type?
O negative blood, as it has no A, B, or D antigens.
Why are people with AB+ blood considered universal recipients?
They have A, B, and D antigens and do not produce A, B, or D antibodies.
What is the risk associated with using O negative blood in emergencies?
While it minimizes acute hemolytic reactions, a mild reaction is possible due to other antigens and antibodies.
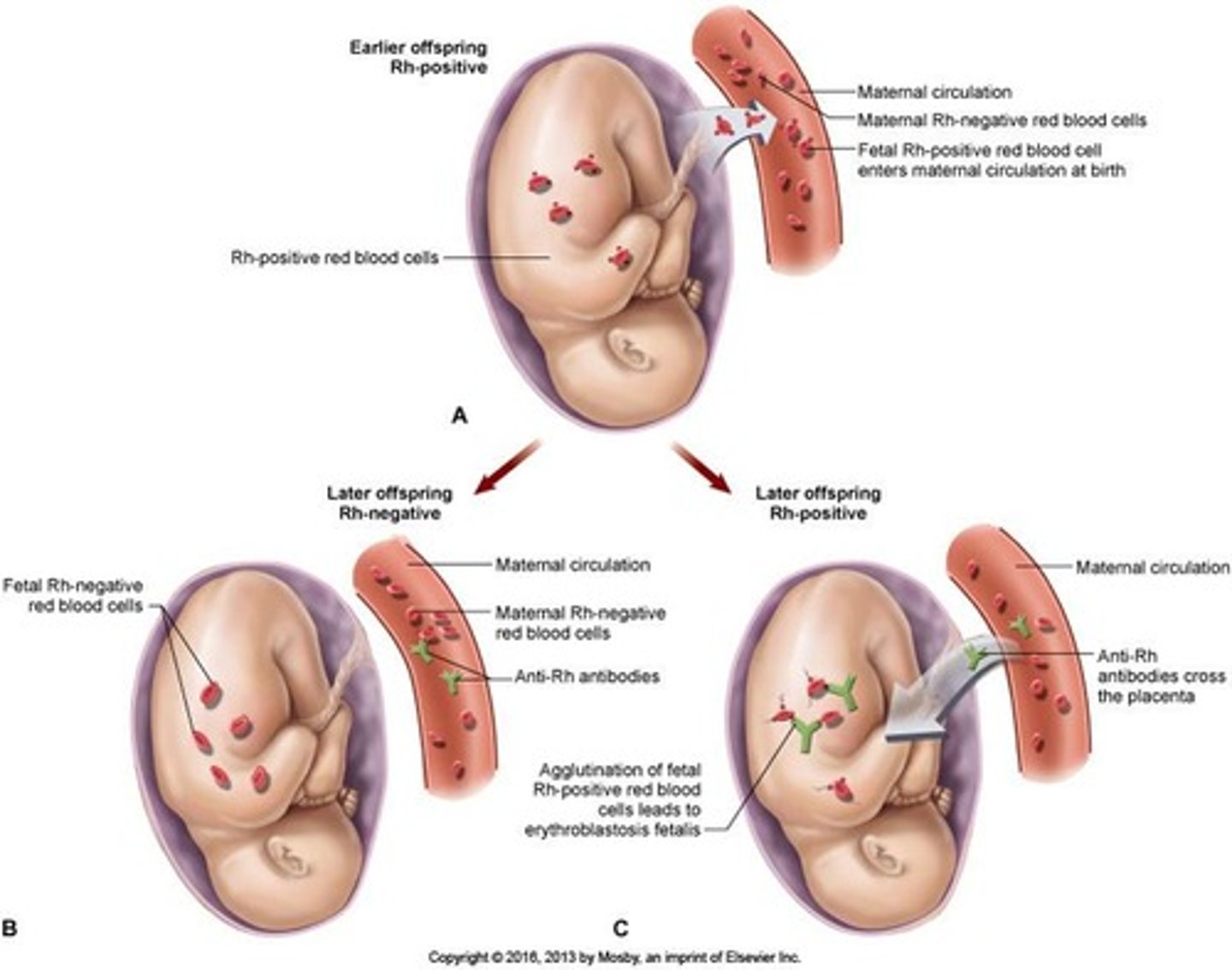
What antigen is associated with Rh positive and negative blood groups?
The D antigen.
How can Rh negative individuals develop anti-D antibodies?
Through exposure to the D antigen during transfusions of Rh positive blood or pregnancies with an Rh positive fetus.
What happens upon second exposure to the D antigen in Rh negative individuals?
A transfusion reaction occurs, resulting in hemolysis of the RBCs in the donated blood.
What type of transfusion reaction occurs with incompatible blood transfusion?
Acute hemolytic reaction.
What is the consequence of transfusing Rh positive blood into an Rh negative person?
It can lead to the development of anti-D antibodies and subsequent transfusion reactions.
What is the significance of the D antigen's discovery?
It was discovered in the blood of Rhesus monkeys and is critical for determining Rh blood type.
What is the best practice when transfusing blood?
Fully cross-match and use donor blood of the same group as the recipient.
What are the possible reactions to O negative blood transfusion?
No acute hemolytic reaction, but a mild reaction is possible due to other antigens.
What is the role of antibodies in blood plasma?
They help identify and attack foreign antigens.
What is the importance of knowing a recipient's blood group before a transfusion?
To prevent serious transfusion reactions and ensure compatibility.
What is the risk of acute hemolytic reactions?
They can cause severe complications and are most likely to occur shortly after the transfusion begins.
What is the relationship between the D antigen and pregnancy?
Rh incompatibility can occur if an Rh negative mother carries an Rh positive fetus, leading to potential complications.
What is the consequence of not matching blood types correctly during transfusions?
It can lead to severe transfusion reactions, including hemolysis.
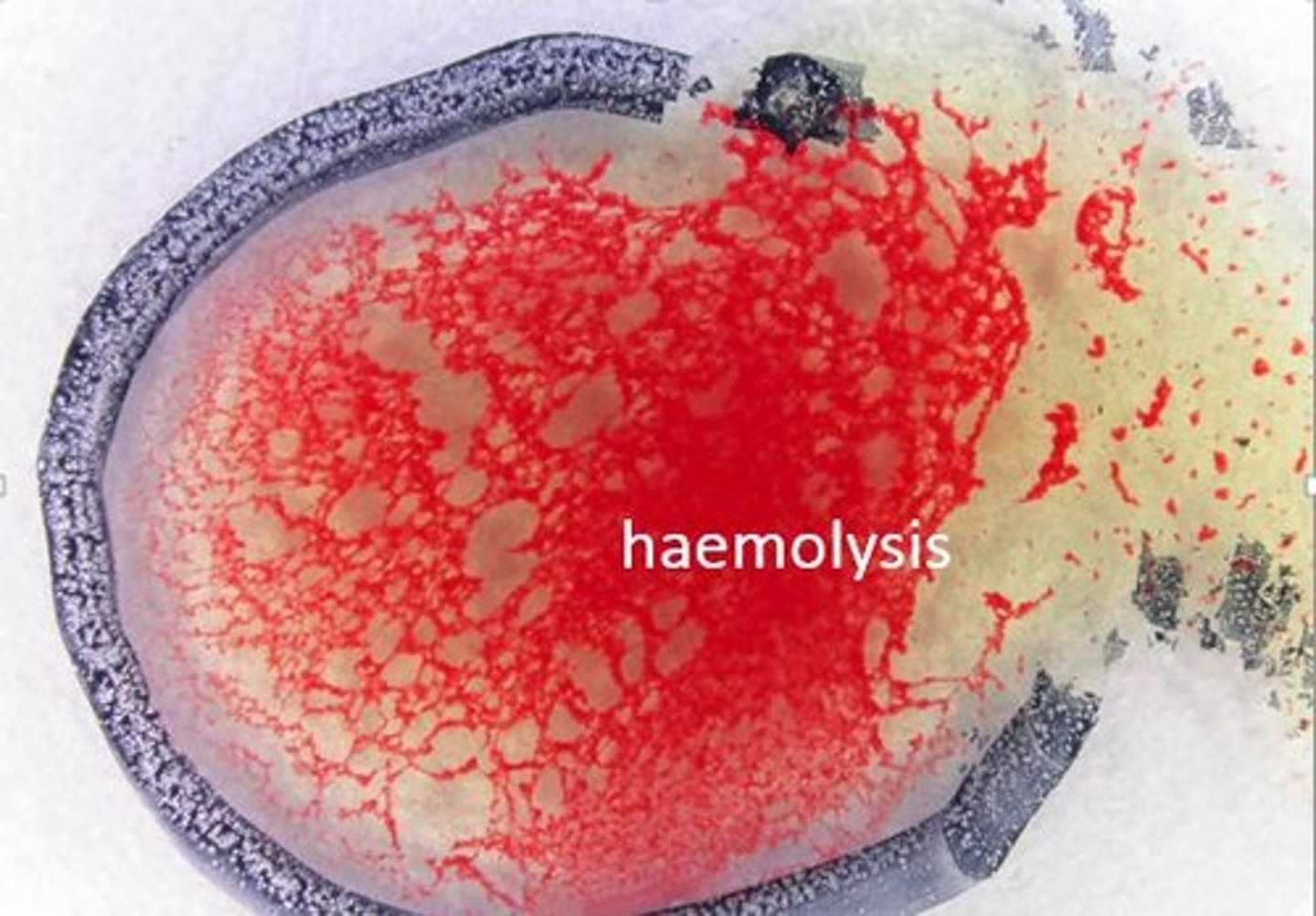
What is agglutination in the context of blood transfusions?
Agglutination is the clumping of red blood cells (RBCs) that occurs when antibodies attach to RBCs carrying the corresponding antigen, preventing them from flowing freely through blood vessels.
What can result from the obstruction of blood capillaries during a transfusion reaction?
Obstruction of blood capillaries can hinder blood flow to tissues, potentially leading to serious complications.
What is haemolysis and how does it relate to blood transfusion reactions?
Haemolysis is the rupturing of red blood cells, which can occur after agglutination, leading to the release of hemoglobin into plasma and potential kidney obstruction.
What are the symptoms of acute haemolytic reactions?
Symptoms include heat along the vein, flushing of the face, urticaria, headache, lumbar pain, chills, fever, chest/abdominal pain, nausea, vomiting, tachycardia, hypotension, and dyspnoea.
What is the main cause of acute haemolytic reactions?
Acute haemolytic reactions are primarily caused by incompatible transfusions, often due to pre-transfusion sampling errors or mistakes during the checking process.
What preventive measures can be taken to avoid acute haemolytic reactions?
Preventive measures include meticulously verifying and documenting patient identification from sample collection to component infusion.
What are febrile reactions in blood transfusions?
Febrile reactions, also known as non-haemolytic reactions, are caused by sensitization to donor leucocytes, platelets, or plasma proteins.
What are common symptoms of febrile reactions?
Symptoms include chills, a temperature rise of more than 1°C, low blood pressure, tachycardia, nausea, vomiting, headache, flushing, and muscle pain.
How are febrile reactions typically managed during a transfusion?
In the absence of renal shutdown, febrile reactions are rarely fatal, and it is common to continue the infusion while monitoring the patient's temperature.
What is the role of potassium (K+) in acute haemolytic reactions?
The release of potassium into plasma during haemolysis can lead to heart arrhythmias.
What is circulatory overload in the context of blood transfusions?
Circulatory overload occurs when fluid is administered faster than the circulation can accommodate, resulting in symptoms like cough, dyspnoea, pulmonary congestion, headache, hypertension, tachycardia, and distended neck veins.
What is sepsis in relation to blood transfusions?
Sepsis can occur from the transfusion of bacterially contaminated blood components.