9 Neurodegenerative Diseases
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
Key Characteristics of a neurodegenerative disease
Insidious onset, gradual progressive degeneration of structure and function of nervous system
Incurable
Sarts in one or two locations and spreads based on disease
Accumulation of misfolded proteins
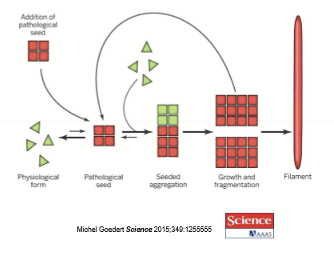
What is the prion hypothesis?
Pathological seeds cause misfolding of physiological proteins. The misfolded proteins aggregate and form into filaments
What is alzheimer’s caused by?
Pathogenic misfolded proteins that cause plaques and tangles
What proteins are misfolded in Alzheimer Disease?
Amyloid beta and Tau
What proteins are misfolded in Parkinson Disease?
alpha Synuclein
What proteins are misfolded in Huntington Disease?
Huntingtrin
What proteins are misfolded in Creutzfeldt-Jakob Disease?
Prion Protein (PrP)
What proteins are misfolded in Chronic Traumatic Encephalopathy (CTE)?
Tau (different location and spreading compared to Alzheimer)
What proteins are misfolded in Amyotrophic Lateral Sclerosis (ALS) ?
Superoxide Dismutase 1
Tests for neurodegenerative diseases often involve what?
Vision and perception
What is the difference between Dementia and Alzheimer’s?
Dementia is a clinical presentation, not a disease. It is an acquired memory loss that causes significant impairment.
Alzheimer’s Disease is a specific disease that can present with dementia. It is the most common cause of dementia.
What are some dementia-causing disease?
Alzheimer disease
Vascular dementia
Parkingson Disease
Huntington disease
Creutzfeldt-Jakob disease
Chronic traumatic encephalopathy
Frontotemporal dementia
What is the most common neurodegenerative disease?
Alzheimer disease, has an average onset at 65 with 50% having it at 80.
What are some characteristics of Alzheimer disease?
No effective diagnostic tool
No single effective medication to halt or significantly slow neurodegenerative disease in most people
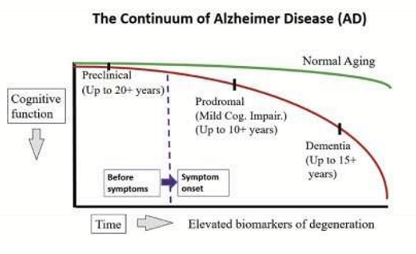
Stages of Alzheimer disease
Stage 1= Preclinical/Presymptomatic
May have difficulty with word-finding
Misplacing objects
Stage 2 = Mild Cognitive Impairment (MCI)
Difficulty with normal daily tasks
Getting lost d/t visual issues
Difficulty reading books/watching shows
Anxiety/ depression common/ anger
Stage 3 = Dementia due to AD
may have residual saying and become increasingly less communicative
Does not remember others or self
What are some vision related clinical presentations of AD?
Sleep disturbances
Contrast Sensitivity
Tasks difficult with inadequate light
Driving after dusk and before dawn
Losing self and others
Environmental agnosia: lost in familiar surroundings
Difficulty with figure-ground discrimination: foreground/background confusion
Prosopagnosia: inability to recognize faces
RNFL thinning: glaucoma/glaucoma-likeConvergence insufficiencyHemispatial neglect
How is AD diagnosed?
Brain atrophy via MRI and cognitive tests.
MRI shows enlarged ventricles, deeper sulci, and hippocampal atrophy
Congitive tests: Mini-mental state examination (MMSE) used to diagnose MCI and dementia
What cognitive impairments must be present for a diagnosis of MCI or Dementia, as assessed by the MMSE?
Memory and learning
Complex thinking and executive function
Language
Visuospatial abilities
With impairments in 2 of the areas of cognitive function
What is the pathogenesis of AD?
etiological factors
damage to Gut-Brain axis starts in gut
Damage to brain: microglia, BBB, Metabolism, inflammation, etc
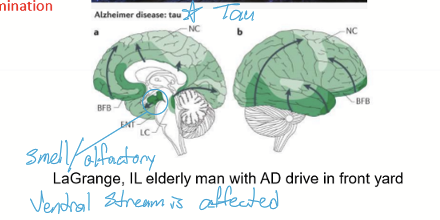
Misfolding of amyloid, spreading of misfolded amyloid, and induces a misfolding of Tau. Tauopathy spreads
What is the etiology of AD?
Non-modifiable factors:
Genes like APOE4
Aging
Modifiable lifestyle factors:
Diet: ultra processed foods
High Carb diet (diabetes)
Low short chain fatty acids
High Trimethylamine N-oxide (TMAO)
Low Vitamins
Curcumin
Omega-3
Alcohol
Low Physical Activity
Poor sleep
Poor stress management and trauma
How do neurodegenerative diseases start?
Disruptions in the gut microbiome and/or tight junctions in the gut cause inflammation.
Leaky gut leads to a breakdown of the blood-brain barrier (BBB), allowing toxins, bacteria, and harmful molecules to enter the brain's extracellular fluid (ECF), which induces protein misfolding.
Amyloid-β42 plaques form due to improper cleavage of amyloid precursor protein (APP) by secretases. (A hallmark of neurodegenerative disease, but not necessarily the direct cause).
Tauopathy occurs when misfolded tau proteins form neurofibrillary tangles (NFTs). This is highly pathogenic and is exacerbated by misfolded Aβ42.
Is Alzheimer disease transmittable?
Yes, EyeBank does not allow corneal transplants from patients with AD.
What are the treatments for AD?
No Rx that stops the disease. Only Rx for symptomatic relief and delay of cell death.
Acethycholinesterase inhibitors (Aricept) compensates for loss of cholinergic neurons.
Memantine (Namenda) are NMDA blockers
What does Parkinson Disease affect?
It affects the initiation of intentional behavior = hypokinetic = difficult to move w/ tremors
What is Huntington Disease affect?
It affects the suppression of unwanted behaviors = hyperkinetic
What is the second most common neurodegenerative disease?
Parkinson Disease, with an average age of onset at 60 yrs old. There is no cure.
What is Parkinson Disease defined as?
A GROUP of movement diseases
What are the typical presentations associated with Parkinson Disease?
Bradykinesia
Rigidity
Resting tremor
Gait and Balance
Loss of smell
Sleep disorder
Constipation
Low blink rate
What are some visual and visuospatial presentations of Parkinson’s Disease?
Motility Issues
Visuospatial problems
Hallucinations: late in disease
What are some motility issues patients with PD present?
Ocular Surface irritation: 2/3 have KCS or Dry eye disease
Convergence insufficiency (80% of patients with early PD)
Freezing Gait; can be alleviated with external cues
What are some visuospatial issues patients with PD present?
Environmental agnosia
Prosopagnosia: inability to recognize the faces of familiar people
Recognition of movement in periphery decreases
What are the hallucinations patients with PD present?
Occurs in 9-44%. Can have passage or complex hallucinations.
What are passage hallucinations?
A type of visual hallucination where a person sees a fleeting figure or object moving in their peripheral vision. It is often brief and non-detailed.
What are complex hallucinations?
Detailed and vivid hallucinations that often involve people, animals, or objects in full form. It can be stationary or moving and may include multiple sensory modalities. Typically much more detailed and scary compared to passage hallucinations.
What does a primary motor problem in Parkinson’s disease (PD) suggest?
In early stage PD, predominant motor symptoms are less likely to have a significant memory impairment
What does a primary sensory problem in Parkinson’s disease (PD) suggest?
In early-stage PD, predominant sensory symptoms (e.g., pain, tingling, or loss of smell) may indicate a non-motor presentation of the disease. Non-motor dominant PD may be associated with a higher risk of cognitive decline over time.
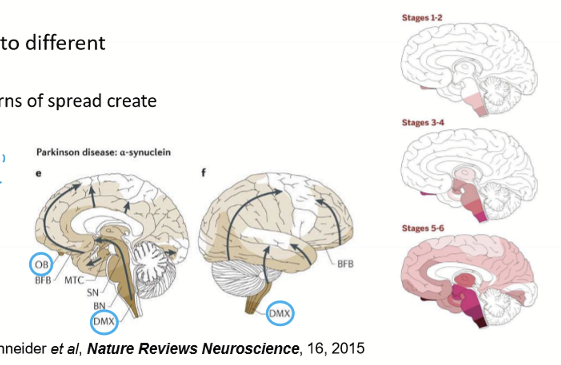
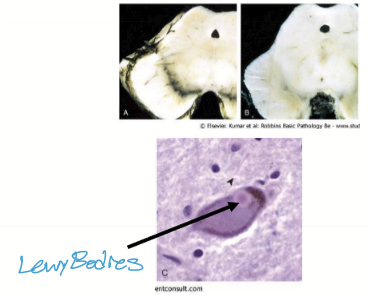
Pathogenesis of Parkinson Disease
Triggers
Begins in gut and/or olfactory bulb
Misfolding of alpha synuclein: loss of smell/constipation; can see misfolded proteins in retina
Travels to brain via Vagus or CN1
Damages Dopaminergic Substantia Nigra Pars Compacta
Causes a patterned spread
What are some Parkinson Disease triggers?
Genetic mutation in alpha synuclein gene
Chronic pesticide and herbicide exposure (~250x increased risk)
Pollution
Infection with certain gut bacteria
Low SCFA
How long does it take for the misfolded alpha synuclein to travel to the brain?
~10-15 years
How long does it take for the patient to show symptoms from the misfolded alpha synuclein entering the brain?
~10-15 years
How does PD spread once in the brain?
It spreads to the Dorsal Motor Nucleus (DMX) of Vagus, then to the midbrain. Eventually, it affects the substancia nigra pars compatca of the midbrain
When the substancia nigra pars compacta of the midbrain is affect, what happens?
Lewy Bodies form and are made of misfolded alpha synuclein. There is also a loss of dopaminergic neurons, causing hypokinetic presentaions. Treatement usually begins at this point.
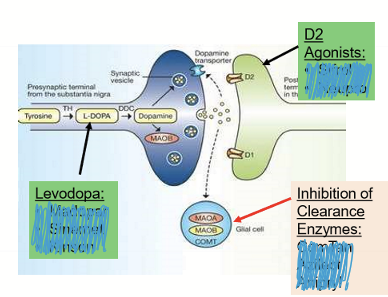
What are the treatments for PD?
Increase dopamine:
Levodopa with carbidopa
Inhibition of clearance nezymes
MAO B inhibitors
COMT inhibitors
D2 agonists
Other:
Memantine (namenda) to decrease excitotoxicity
Cholinergics (Aricept) to improve brain activity
Surgery: Deep brain stimulation (DBS); involve putting electrodes into the brain
What are the side effects of the oral medications for PD?
If there is too much Rx, there is an increase in unwanted movement = Dyskinesia (abnormal movements)
What are some key characteristics for Huntington Disease?
Hyperkinetic: involuntary movements from damaged basal ganglia (unable to suppress unwanted movements)
AD huntingtin protein
Incurable
Autosomal Dominant disease
What are the clinical presentation of Huntinton’s Disease?
Chorea: purposeless dance-like movements
Athetosis: snake-like movements of hands
Abnormal eye movements: Saccades
Severe Dementia
What is the pathology of Huntington’s Disease?
Misfolded proteins accumulates in the basal ganglia, affecting the caudate and putamen (responsible for inhibiting unwanted movements) and enlarge ventricles
What is Creutzfeldt-Jakob Disease?
A neurodegenerative disease caused by prions.
What is the clinical presentation of Creutzfeldt-jakob disease?
Rapid deterioration
Ataxia
Dementia
Impaired motor:
speech
swallowing (dysphagia)
Sudden jerky movement
Die within a year of diagnosis
How does the brain appear histologically from CJD?
spongy appearance

What is Chronic Traumatic Encephalopathy?
A progressive neurodegenerative disease caused by repeated head injuries/concussions.
What is the epidemiology of Chronic Traumatic Encephalopathy?
athletes
military
traumatic brain injury
What are the presentations of chronic traumatic encephalopathy?
Emotional dysregulation: judgement, anger, impulse control
Dementia
What is the pathogenesis of chronic traumatic encephalopathy?
Multiple concussions: coup and countercoup, rotation causes axonal shearing between cortex and white matter and within white matter
Tau misfolding induced by inflammation: amygdala