Clinical Diagnosis Quiz 1: Neuro, HEENT, Optho (4/28/21)
1/214
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
215 Terms
System 2
System ___ thinking is slow, deliberate, and analytical and requires the significant effort.
System 1
System ___ thinking relies heavily on pattern recognition, intuition, and previous experience.
System 1
System ___ thinking is used when someone makes a direct association between new information (ie patient presenting with chest pain) and a similar example in memory (ie a previous patient with chest pain who had a MI).
script
An illness ____ refers to the way in which clinicians catalogue their own comprehensive pictures of disease states based on their previous experience.
System 1
What type of thinking (system 1 vs system 2) is very susceptible to cognitive biases?
System 2
What type of thinking (system 1 vs system 2) can lead to errors when applied to simple, routine problems?
Pre-test probability
The ____ is the probability of a patient having the disease before the test result is known.
(Ie what is the chance that a patient with chest pain is having a MI)
Post-test probability
The ____ is the probability of a patient having the disease after the test result is known.
(Ie what is the chance that a patient with chest pain is having a MI after his troponin returned elevated).
Rare diagnoses
When is system 2 thinking best used: common diagnoses or rare diagnoses?
Unusual presentations
When is system 2 thinking best used: textbook presentations of illnesses or unusual presentations of illnesses?
Sensitivity
The ____ of a test refers to its ability to correctly identify those with the disease.
Specificity
The ____ of a test refers to its ability to correctly identify those without the disease.
Sensitive tests (SnOut)
What types of tests are good for ruling diagnoses out: sensitive or specific tests?
Specific tests (SpIn)
What types of tests are good for ruling diagnoses in: sensitive or specific tests:
In (SpIn)
Specific tests are good for ruling diagnoses ____ (in or out).
Out (SnOut)
Sensitive tests are good for ruling diagnoses ____ (in or out)
Likelihood ratio
The _____ is used to convert your pre-test probability into a post-test probability.
Sensitivity/(1-specificity)
(How likely does someone with the disease test positive)/(How likely does someone without the disease test positive)
How do you calculate a positive likelihood ratio?
Treatment threshold
The _____ refers to how confident a clinician needs to be in a diagnosis before they decide that it is appropriate to initiate treatment.
High treatment threshold.
(You want to be sure someone has cancer before you start chemotherapy)
You think that your patient might have lung cancer. Should you have a high or low treatment threshold before starting chemotherapy?
Low treatment threshold.
(The amoxicillin probably won't do much harm even if they didn't really need it).
You think that your patient might have an ear infection caused by a bacteria. Should you have a high or low treatment threshold before prescribing amoxicillin?
Primary headaches
_____ headaches are headaches that are caused by an intrinsic dysfunction of the nervous system and not by other medical conditions such as hypertension, tumors, or trauma.
Secondary headaches
____ headaches are headaches that are caused by underlying organic conditions such as hypertension, trauma, tumors, or metabolic disorders.
No. Primary headaches (tension, migraines, cluster headaches) tend to begin earlier in life. New onset headaches in patients over 50 are concerning for secondary causes such as tumors, systemic disease, metabolic disorders, etc.
Are new-onset primary headaches common in patients over the age of 50?
Consider further testing. A change in the qualify of a chronic headache is raises concerns that there may be other underlying pathology.
A patient with chronic migraines tells you that the quality and timing of her headaches have been different over the past 2 weeks. Do you reassure her that these are just her normal migraines or do you consider further testing?
Males (5:1 ratio)
Are cluster headaches more common in males or females?
Females
Are migraine headaches more common in males or females?
Consider imaging. Headaches that are worse with exertion or valsalva are concerning for secondary headache.
A patient complains of a headache that gets worse when holding their breath and squeezing their abdominal muscles (Valsalva maneuver). Should you consider imaging or just send them home with some ibuprofen?
Yes.
A patient reports that they are having headaches that wake them up in the middle of the night. Should you consider imaging?
P - Pulsatile
O- Ongoing (lasts 4-72 hrs)
U - Unilateral
N- Nausea
D - Disabling
Describe the characteristics of a migraine headache using the POUND mnemonic.
Migraine
A patient describes having throbbing, right-sided headaches that last for 1-2 days with associated nausea and light sensitivity. What type of headache does she likely have?
subarachnoid hemorrhage
A headache that is described as a "thunderclap" or "worst headache of my life" is concerning for a ____.
CT Head (non-contrast)
- You can also do a lumbar puncture if the CT is negative, but you still think there is a high likelihood that the patient has a SAH. A CT still needs to be done first.
You are concerned that a patient may have a subarachnoid hemorrhage after coming to the ED with "the worst headache of [their] life." What test should you order first?
Xanthochromia
- This "yellowing" of the CSF supernatant is caused by the breakdown of blood (RBCs), which produces yellow bilirubin.
What finding on a lumbar puncture suggests a subarachnoid hemorrhage?
Lumbar puncture (the CSF can be used to culture bacteria/fungi)
(MRI can show inflammation of the meninges, but it won't tell you want organism is causing it)
You are concerned that a patient may have meningitis. What is the main test that you would order to confirm this diagnosis?
Tension headache
A patient states that they feel like some is "squeezing a belt" around their head. What type of headache does this sound like?
Migraine
(Tension headaches are more common, but people don't usually go to the doctor for them because they're much less disabling)
What is the most common type of headache that is seen in patients presenting to clinic?
Scotoma
(I accidentally misspelled this previously as "scomata," which actually isn't a thing. Scotoma is the correct spelling)
A _____ is when part of the visual field appears altered or lost. This sometimes occurs in patients that experience auras with their migraines.
No.
Are tension headaches commonly accompanied with nausea and vomiting?
Unilateral
Are cluster headaches usually bilateral or unilateral?
Cluster headaches
What types of headaches frequently present with ipsilateral conjunctival injection, lacrimation, and nasal congestion, and facial sweating?
Cluster headaches
Hypoxia, vasodilators, and alcohol are common triggers for what type of headaches?
Cluster headache
A patient describes severe headaches that feel as though someone is "stabbing" his eye and occur for several minutes before resolving only to return a few hours later. What type of headache is this?
Bending forward
What is a classic aggravating factor of sinus headaches?
Sinus headache
A patient has a headache that worsens when he bends forward. This sounds like a ____ headache.
50%
What is the mortality rate of brain aneurysm rupture?
Ruptured brain aneurysm
What is the most common cause of subarachnoid hemorrhage?
Subarachnoid hemorrhage
A thunderclap headache is considered to be a ____ until proven otherwise.
Subarachnoid hemorrhage (also aneurysms and AV malformations)
A diagnosis of benign cough headache, benign exertional headache, or headache associated with sexual activity can only be made after excluding _____.
Temporal arteritis
A patent presents with a throbbing headache on the sides of her head. The temporal region is tender to palpation. What do you think is causing her headache?
Throbbing
Headaches from temporal arteritis are often described as ____.
Temporal arteritis
Headaches that occur with jaw claudication and scalp tenderness are concerning for ____.
Ophthalmic artery vasculitis
A patient with known temporal arteritis presents with new blindness. What do you think is causing her blindness?
Temporal artery biopsy
What is the "gold standard" for a diagnosis of temporal arteritis?
ESR (erythrocyte sedimentation rate)
What lab would you expect to be elevated in a patient with temporal arteritis?
Yes. A headache with any focal neurological deficits (numbness, tingling, lack of coordination, CN abnormalities) warrants a head CT.
A patient presents with a headache and a lack of coordination. Do you perform imaging?
Rinne test
In the ____ test, a vibrating tuning fork is placed at on the patient's mastoid process to test bone conduction. It is then moved to be parallel with the ear to test air conduction.

Rinne test
The ____ test is used to compare air conduction of sound to bone conduction of sound.
Air conduction
In a patient with a normal Rinne test, which should be louder: air conduction or bone conduction?
Conductive deafness.
(The air conduction is diminished because there is a problem transferring the sound waves somewhere along the pathway from the outer ear to the tympanic membrane and middle ear. Bone conduction bypasses these structures by transferring the vibrations directly from the mastoid process to the receptors in the inner ear. Being able to perceive sound by bone conduction shows that the cochlear nerve and auditory pathway in the brain are intact.. Diminished air conduction with normal bone conduction isolates the lesion to the structures of the outer ear, middle ear, and tympanic membrane).
During the Rinne test, if a patient reports that the sound is louder through bone conduction than through air conduction, what type of hearing loss does the patient have?
Weber test
In the ____ test, a vibrating tuning fork is placed at the vertex of the patient's head and the patient is asked if the sound is the same in both ears.

Conductive deafness.
(When a patient has conductive hearing loss, sounds such as environmental noises are not able to reach the inner ear, which makes the receptors in that ear more sensitive to bone conduction. During the Weber test, if the sound is louder on the same side as the affected ear, the patient has conductive hearing loss)
A patient complains of hearing loss in his right ear. During the Weber test (tuning fork on top of head), he says that he can hear the sound better in his right ear. What type of hearing loss does this patient have?
Sensorineural deafness.
(If there is an issue with the cochlear nerve, neither air nor bone conduction will be able to be perceived in the affected ear. If the sound is louder on the opposite side of the affected ear, the patient has sensorineural deafness).
A patient complains of hearing loss in his right ear. During the Weber test (turning fork on top of the head), he says that he can hear the sound better in his left ear. What type of hearing loss does this patient have?
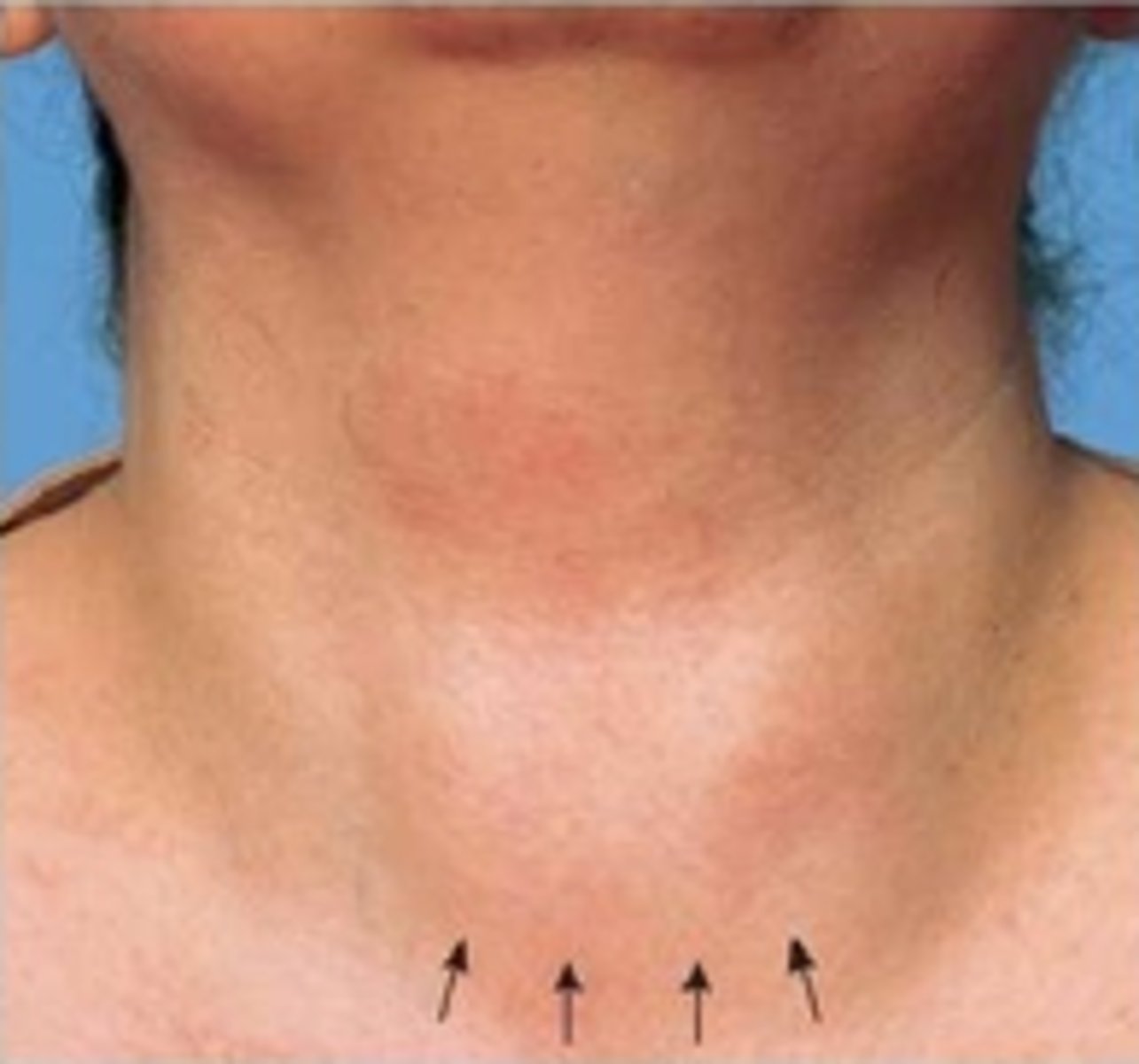
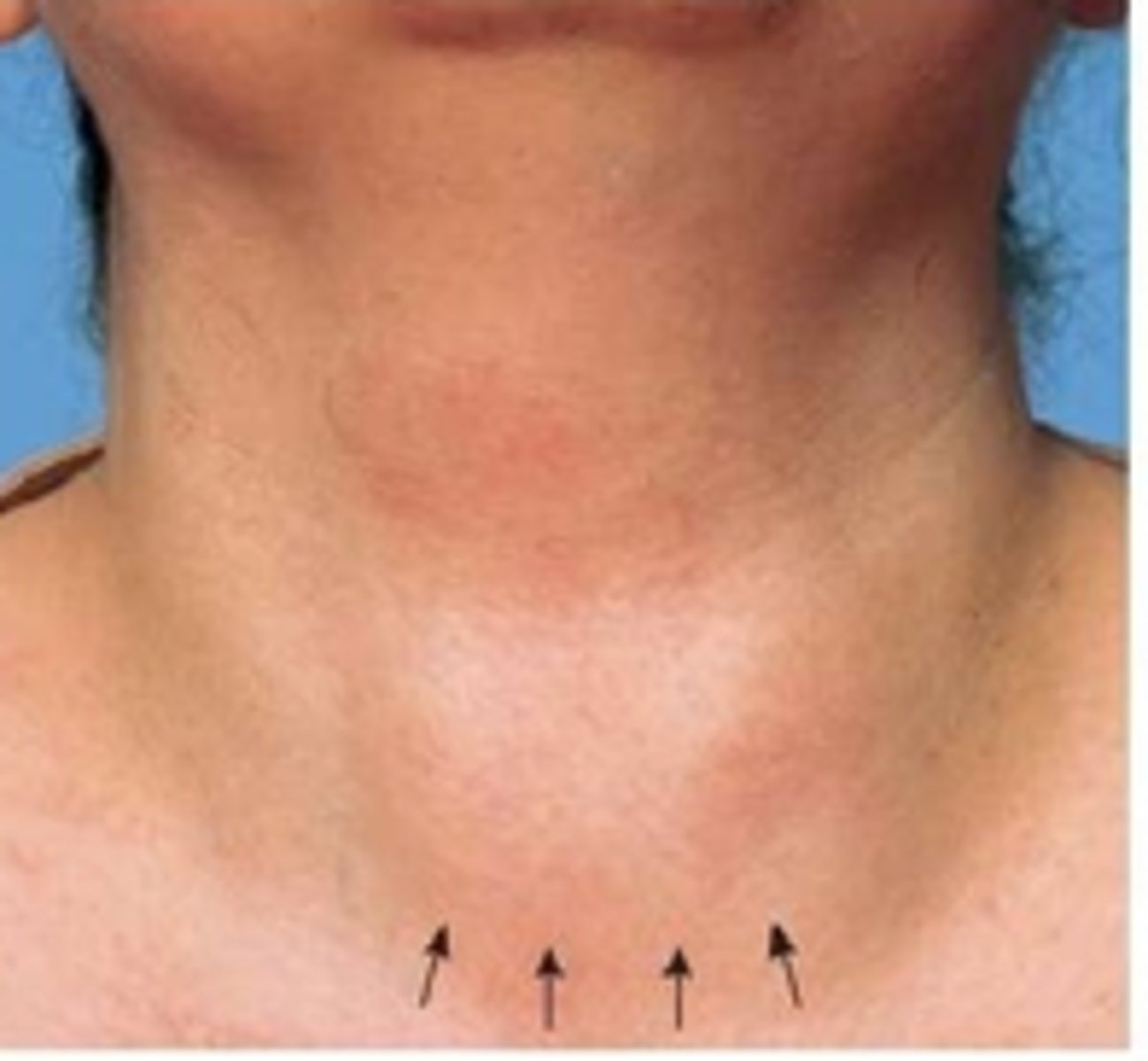
Goiter
What is this?
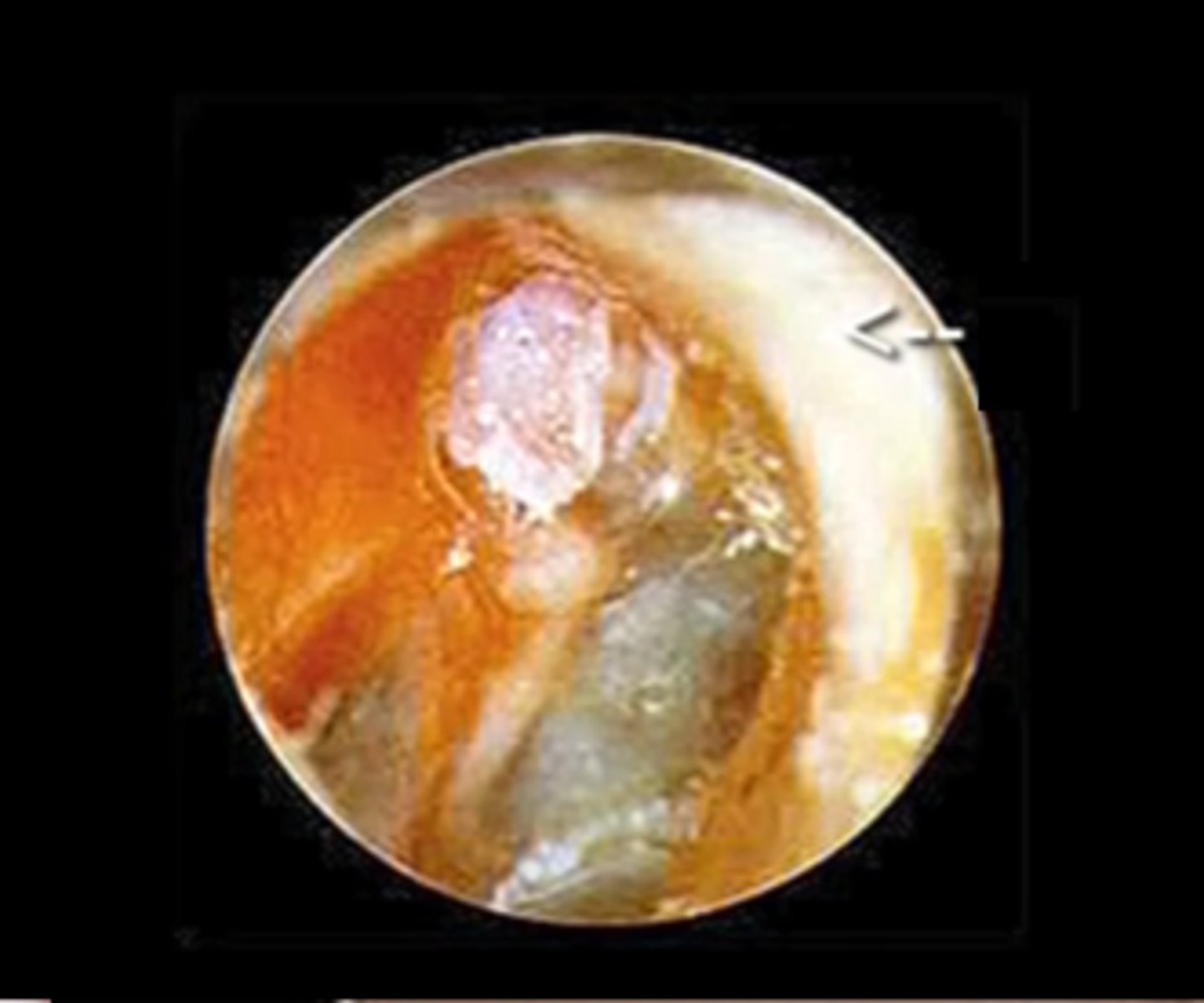
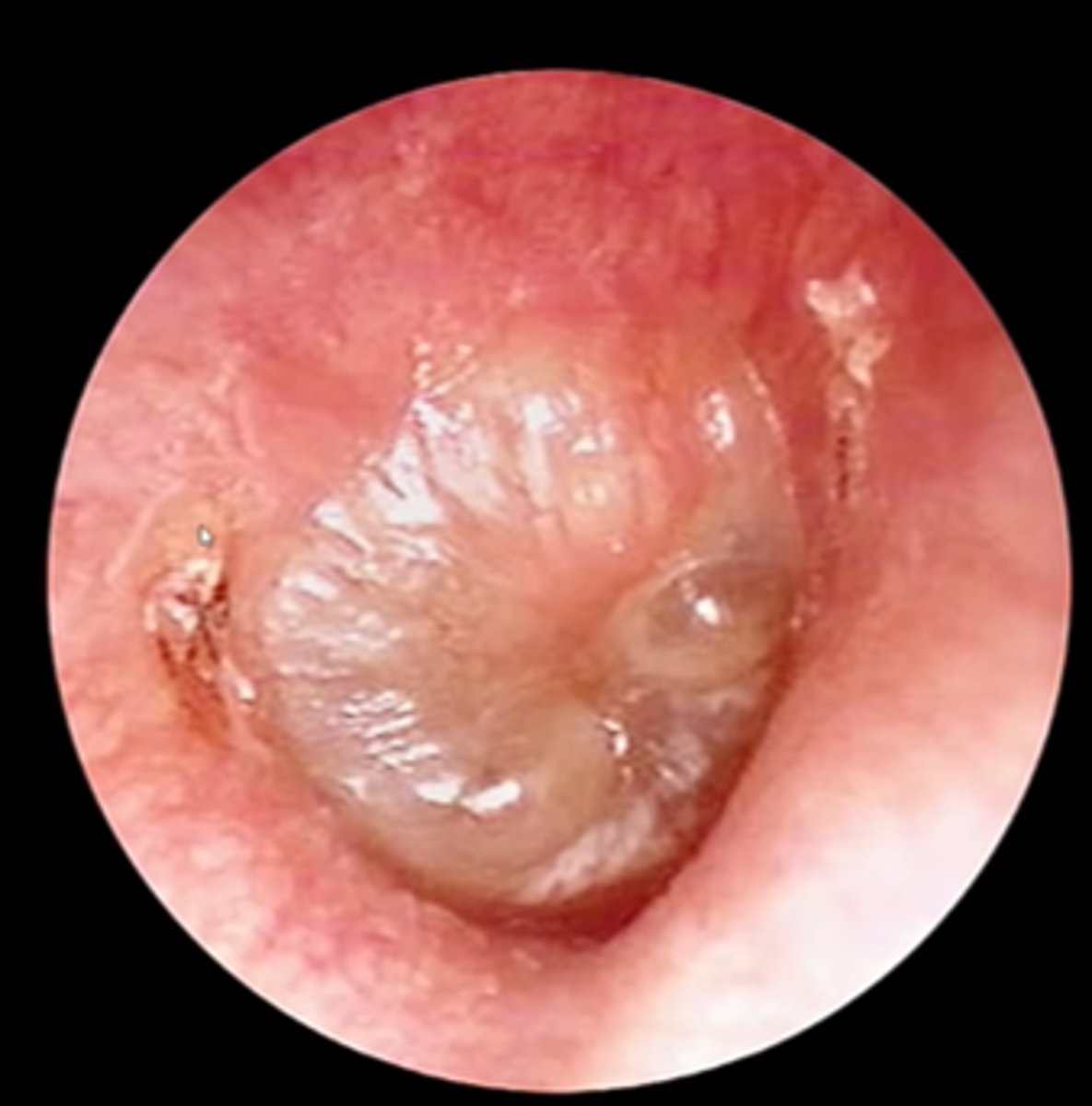
Attic cholesteatoma
(A cholesteotoma is a non-cancerous proliferation of keratinized squamous epithelial cells in the middle ear. These often produce enzymes that can erode the surrounding tissue, including the ossicles. Bacteria can accumulate in this area, leading to infection. This needs to be surgically removed). An attic cholesteatoma specifically occurs in the "attic" of the middle ear, which is the area of the middle ear that is superior to the ossicles.
What is this?
Surgical removal
What is the treatment for a cholesteatoma?
Cholesteatoma
A _____ is a non-cancerous proliferation of keratinized squamous epithelial cells in the middle ear that can produce enzymes that cause erosion of the ossicles. This growth can also collect bacteria, leading to infection.
This is pars flaccida.
(The top part of the tympanic membrane is extra flaccid (floppy/loose))
What is wrong with this tympanic membrane?
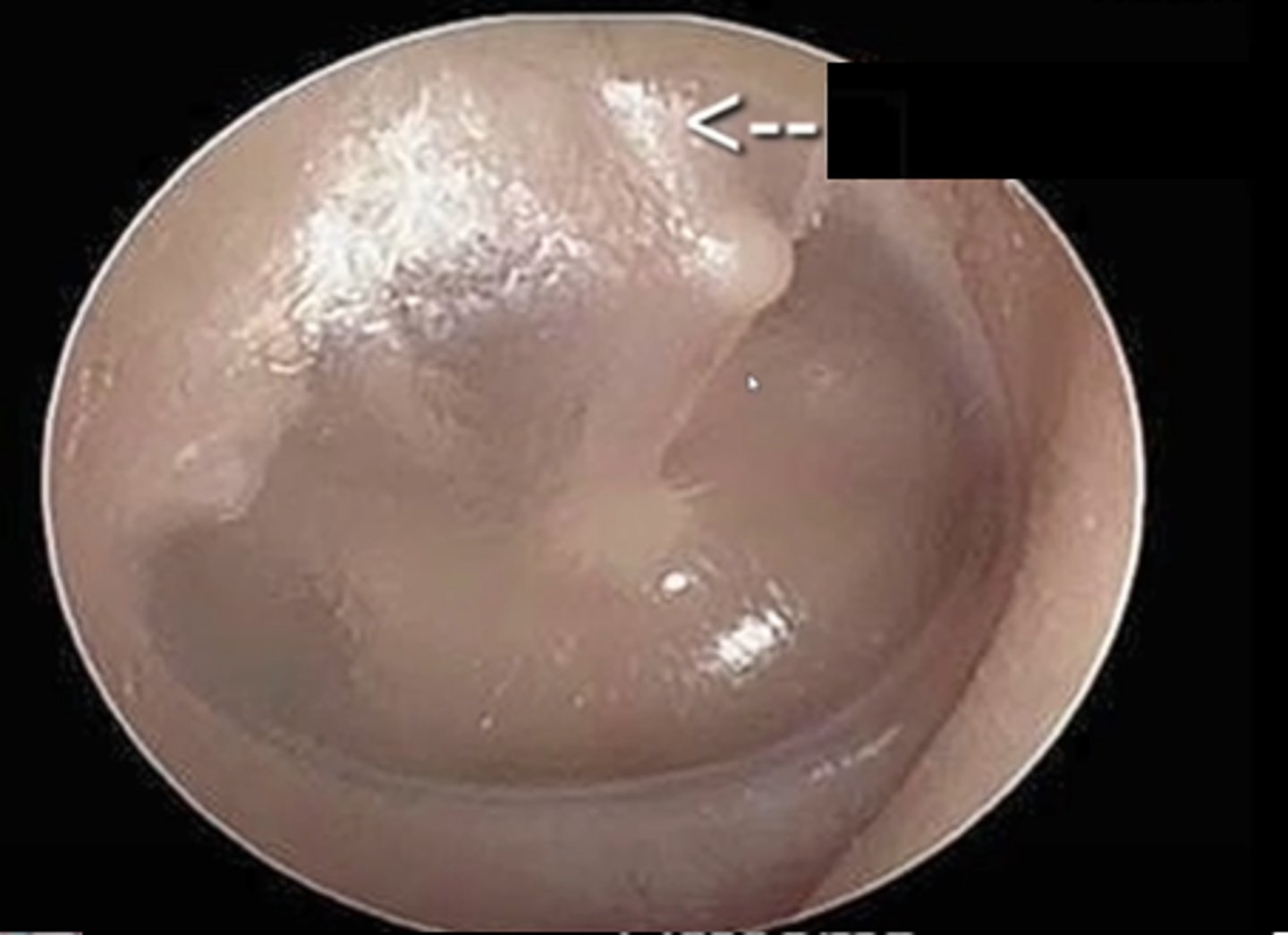
Pars flaccida
____ is when a portion of the tympanic membrane is loose/floopy.
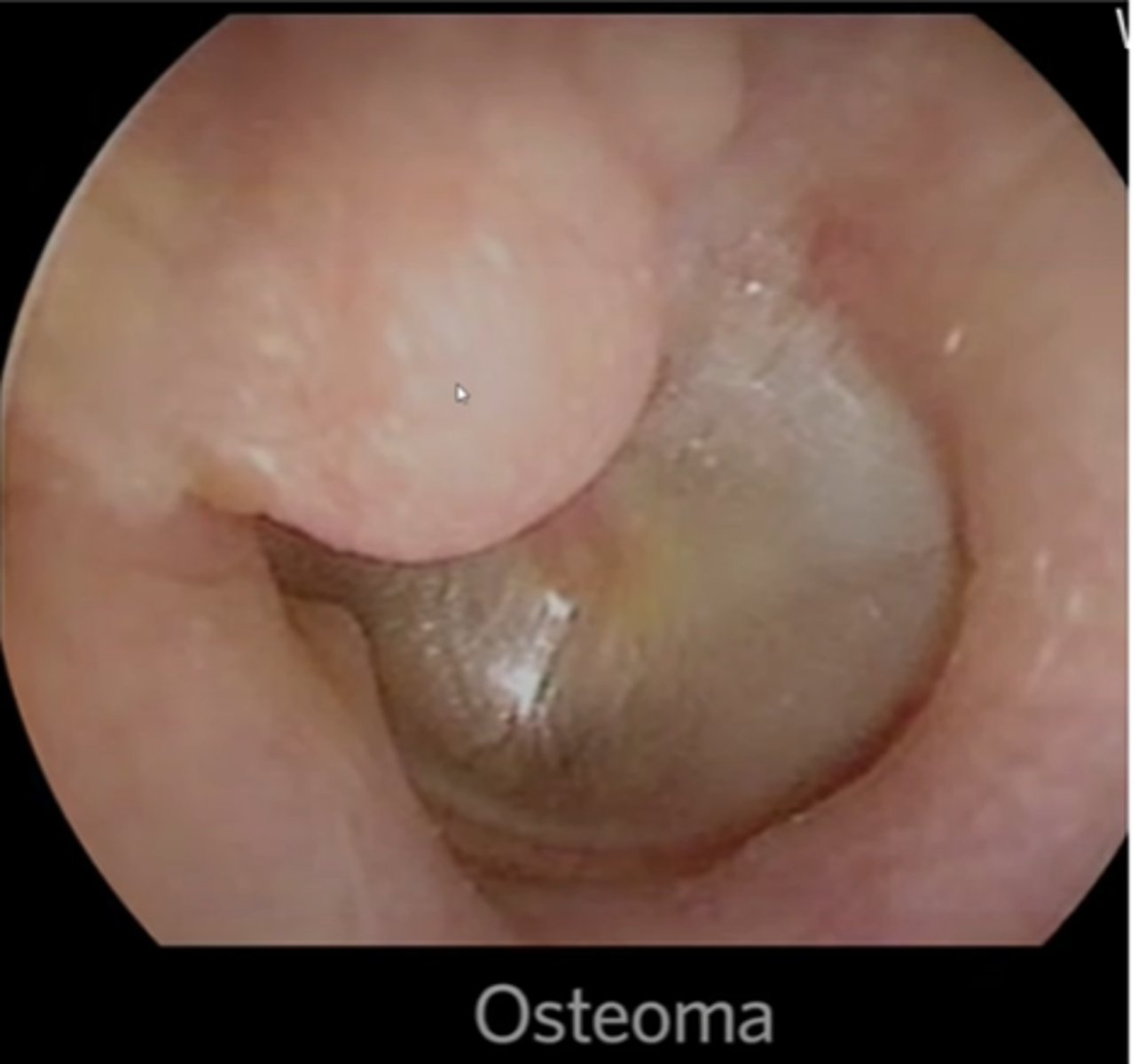
This is an osteoma in the external auditory canal.
(An osteoma is a benign, bony neoplasm in the ear canal. It often occurs when there is frequent irritation of the external auditory canal, such as with surfers who frequently get cold water in their ears)
What is this?
Perforation of the tympanic membrane
What is this?

Tympanosclerosis
(Tympanosclerosis is scarring of the tympanic membrane that usually occurs in patients that had recurrent otitis media or ear tubes).
What is this?

Tympanosclerosis
_____ is scarring of the tympanic membrane that frequently is seen in patients that had recurrent otitis media or ear tubes.
Acute otitis media
What is this?
Otitis media
____ is inflammation of the middle ear
Blue effusion (hemotympanum).
(This is a collection of blood in the tympanic cavity, usually caused by trauma)
What is this?
Tympanic membrane
What structure is seen here?

Impacted cerumen (ear wax)
What is this?

Otitis externa (inflammation of the external ear)
What is this?
-Btw this is an ear

Otitis externa
_____ is inflammation of the external ear
Staph and strep
What are two bacteria that frequently cause otitis externa?
Pseudomonas
A patient with diabetes presents to clinic with otitis externa. Even though this infection is most likely caused by staph or strep, what type of bacteria would you also like to cover when you select your antibiotic?
Ramsay Hunt Syndrome.
-This is essentially shingles involving the facial nerve. The dormant Varicella Zoster virus in the facial nerve becomes reactivated, causing inflammation of the facial nerve, leading to Bell's Palsy. You also get the painful, blistering rash within the dermatome innervated by the facial nerve, which is found in the external auditory canal.
(The sensory branch of the facial nerve that supplies the external auditory canal is called the nervus intermedius).
A patient presents to clinic with unilateral facial paralysis and painful blisters in the external ear canal. What does this patient have?
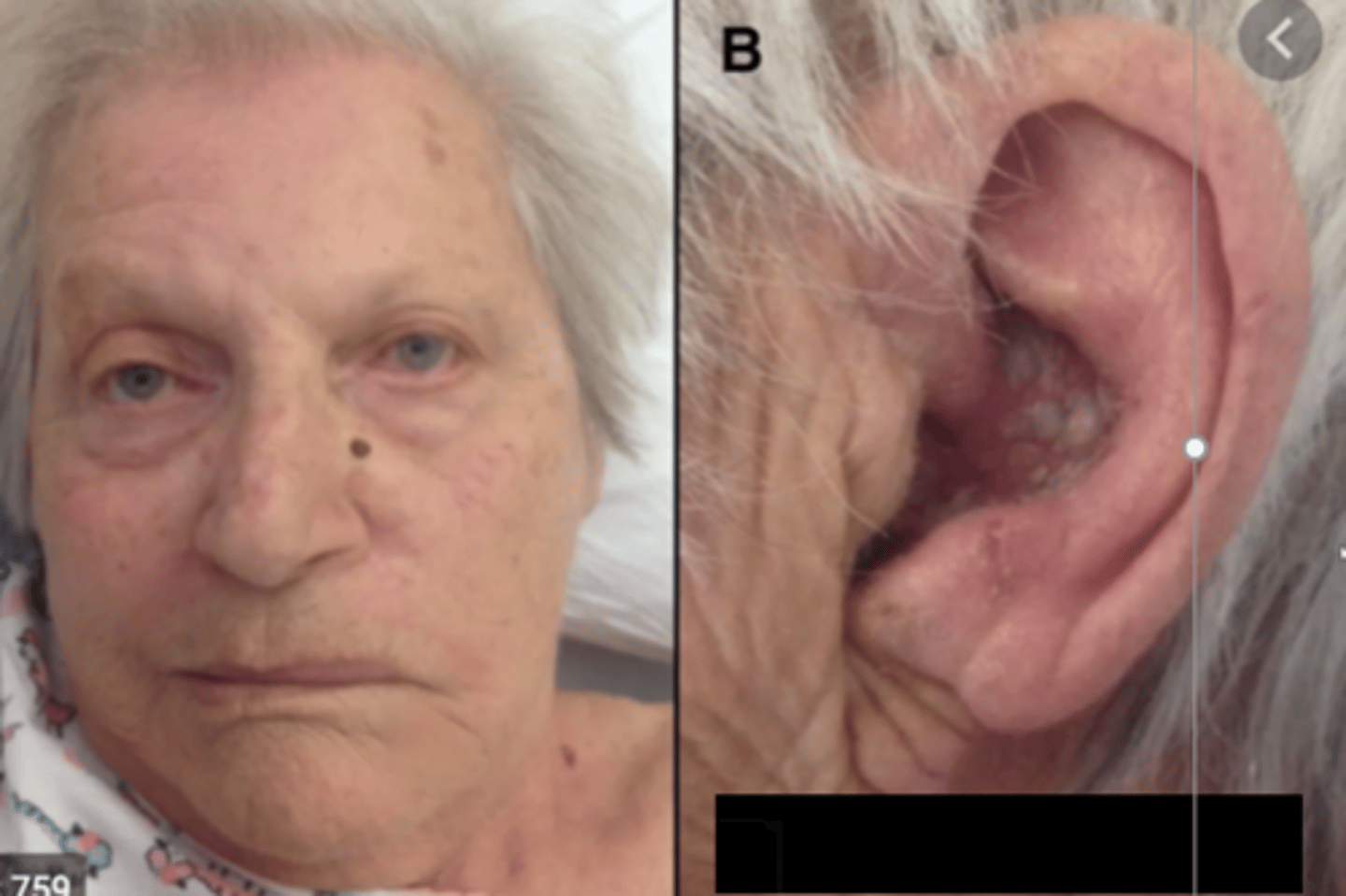
Ramsay Hunt Syndrome
____ occurs when a patient develops a Varicella Zoster infection (shingles) within the facial nerve, leading to facial paralysis (Bells Palsy) and a painful, blistering rash in the external auditory canal
Cauliflower ear
(This occurs when the ear cartilage dies and develops scarring. This frequently occurs after an auricular hematoma separates the perichondrium from the cartilage, cutting off the cartilage's vascular supply, causing the cartilage to die)
What is this?

Cauliflower ear
_____ is a condition in which a patient's ear cartilage dies and forms scars following an auricular hematoma.
Auricular hematoma
(collection of blood in the external ear)
What is this?

Auricular hematoma
A _____ is a collection of blood within the external ear.
Cauliflower ear
(The recurrent hematomas causes the perichondrium to separate from the auricular cartilage, which cuts off blood supply to cartilage, causing the cartilage to die and scar)
A patient that has recurrent auricular hematomas is at risk for developing _____.
Preauricular pit
What is this little indent in front of the ear called?

Auricular hillocks
The structures of the external ear are embryonically derived from the _____.
512 Hz
What frequency tuning fork should be used when performing the Rinne and Weber test?
60 cm
A patient with normal hearing should be able to hear a whisper from ____ cm away.
Goiter
What is this?
Parotid papilla (opening of the parotid duct next to the upper 2nd molar)
What is this?
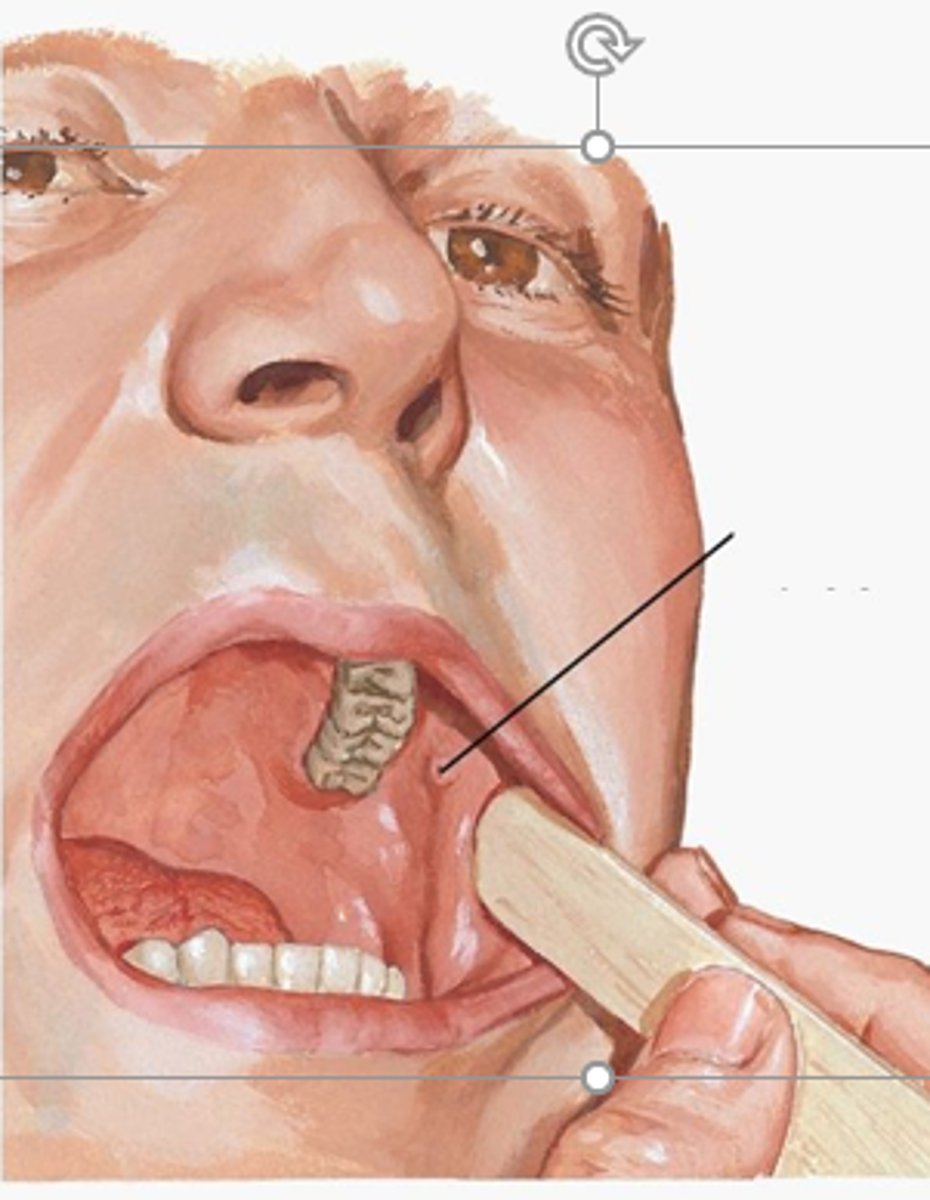
Upper 2nd molar
The parotid papilla (opening of the parotid duct) is found next to the _____.
Parotid papilla
What structure is the arrow pointing to?

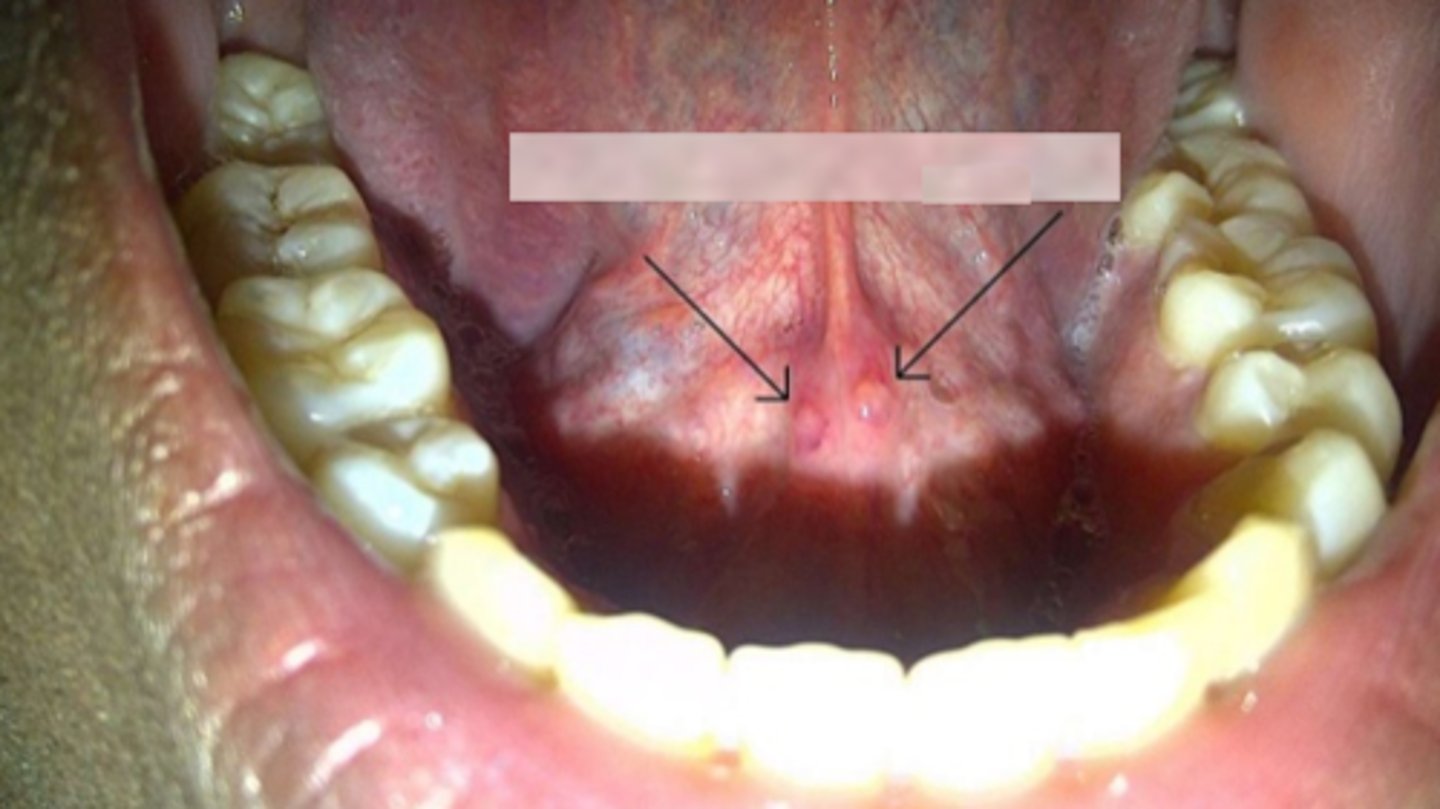
Sublingual caruncles
-These are the papilla that contain the openings of the submandibular duct (aka Wharton's duct)
What are these little bumps?
Kiesselbach plexus/Little's area
The most common cause of a nosebleed in children is injury to the vessels in the ____.
Skull base/temporal bone
Necrotizing otitis externa is an infection of the _____.