Thyroid, Parathyroid, Adrenal Glands Module 6B: Diseases and Hormonal Regulation
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
What disease causes hyperthyroidism due to an enlarged thyroid gland?
Graves' disease
What are common symptoms of Graves' disease?
Weight loss, excess sweating, arrhythmia, protruding eyes, nervousness, and an enlarged thyroid gland.
What condition is characterized by low thyroid hormone levels?
Thyroiditis
What are the symptoms of thyroiditis?
Weight gain, fatigue, and intolerance to cold.
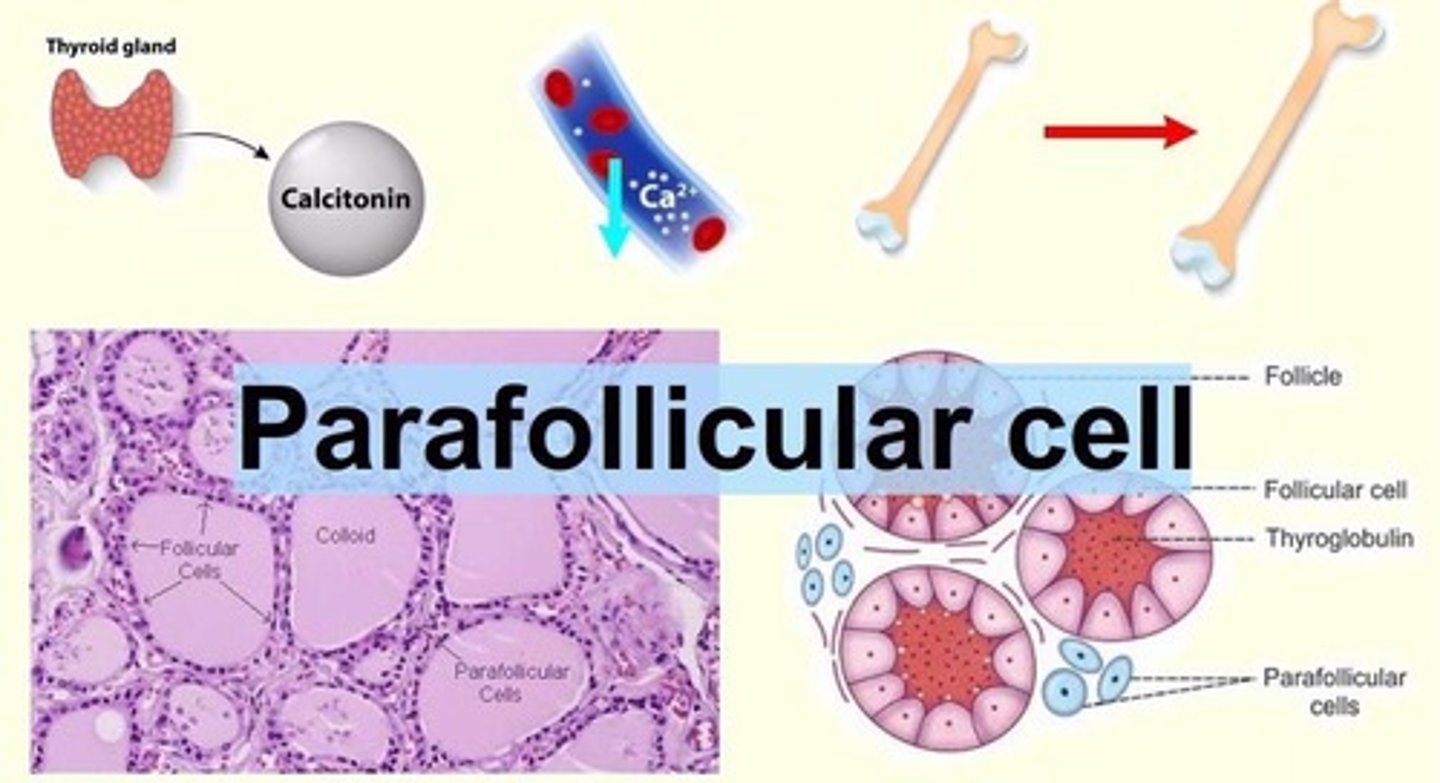
What type of cells in the thyroid gland secrete calcitonin?
Parafollicular cells (C cells)
What is the function of calcitonin?
Inhibits bone resorption by osteoclasts, stimulates bone formation by osteoblasts, decreases calcium absorption, and increases calcium loss at the kidneys.
What hormone is secreted by the parathyroid glands?
Parathyroid hormone (PTH)
What is the primary role of parathyroid hormone (PTH)?
Regulates blood calcium levels by activating osteoclasts and increasing renal calcium reabsorption.
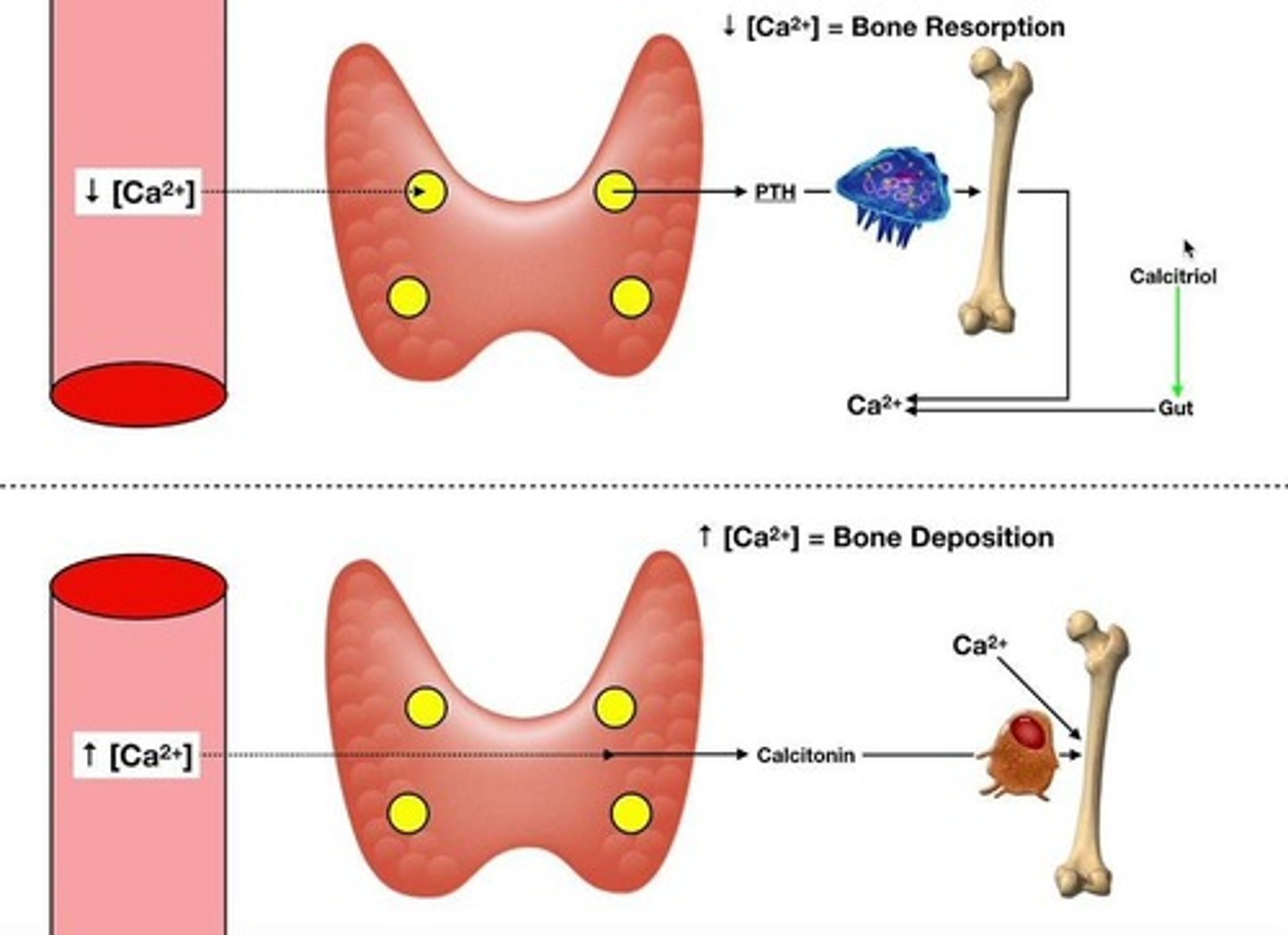
What is calcitriol and its role in calcium regulation?
Calcitriol is the active form of vitamin D, enhancing calcium absorption in the intestines.
What triggers the secretion of parathyroid hormone (PTH)?
Low blood calcium levels.
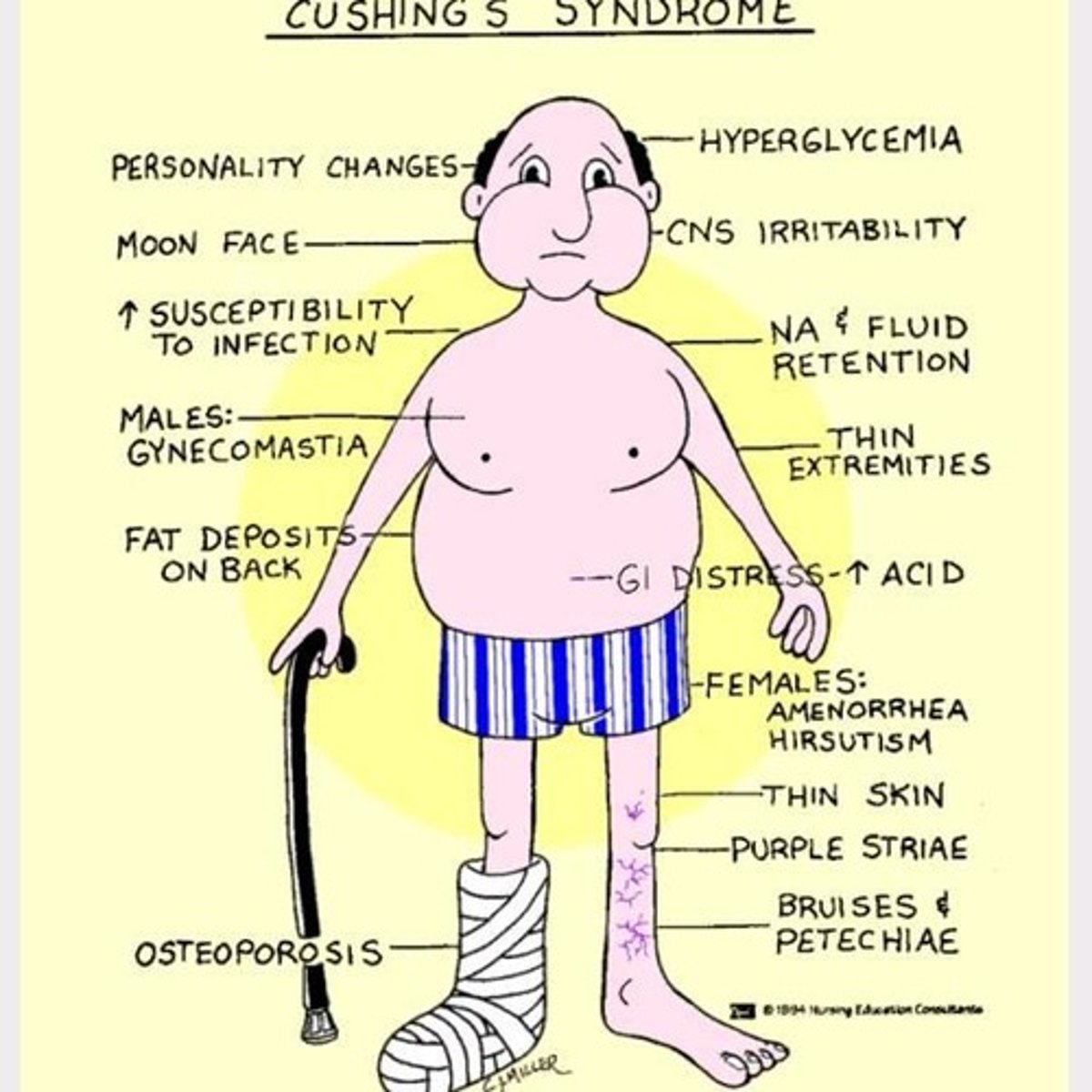
What is the main role of cortisol in the body?
Regulates the body's response to stress, metabolism, and increases blood glucose levels.
What are the three main effects of cortisol?
Promotes gluconeogenesis, breakdown of skeletal muscle, and enhances lipolysis.
What is Addison's disease characterized by?
Low cortisol and aldosterone levels.
What is Cushing's syndrome characterized by?
High cortisol levels.
What is the function of insulin?
Regulates blood glucose levels by increasing glucose uptake into cells.
How does insulin secretion occur in response to high blood glucose?
Glucose enters β-cells, is metabolized to produce ATP, which leads to depolarization and calcium influx, resulting in insulin release.
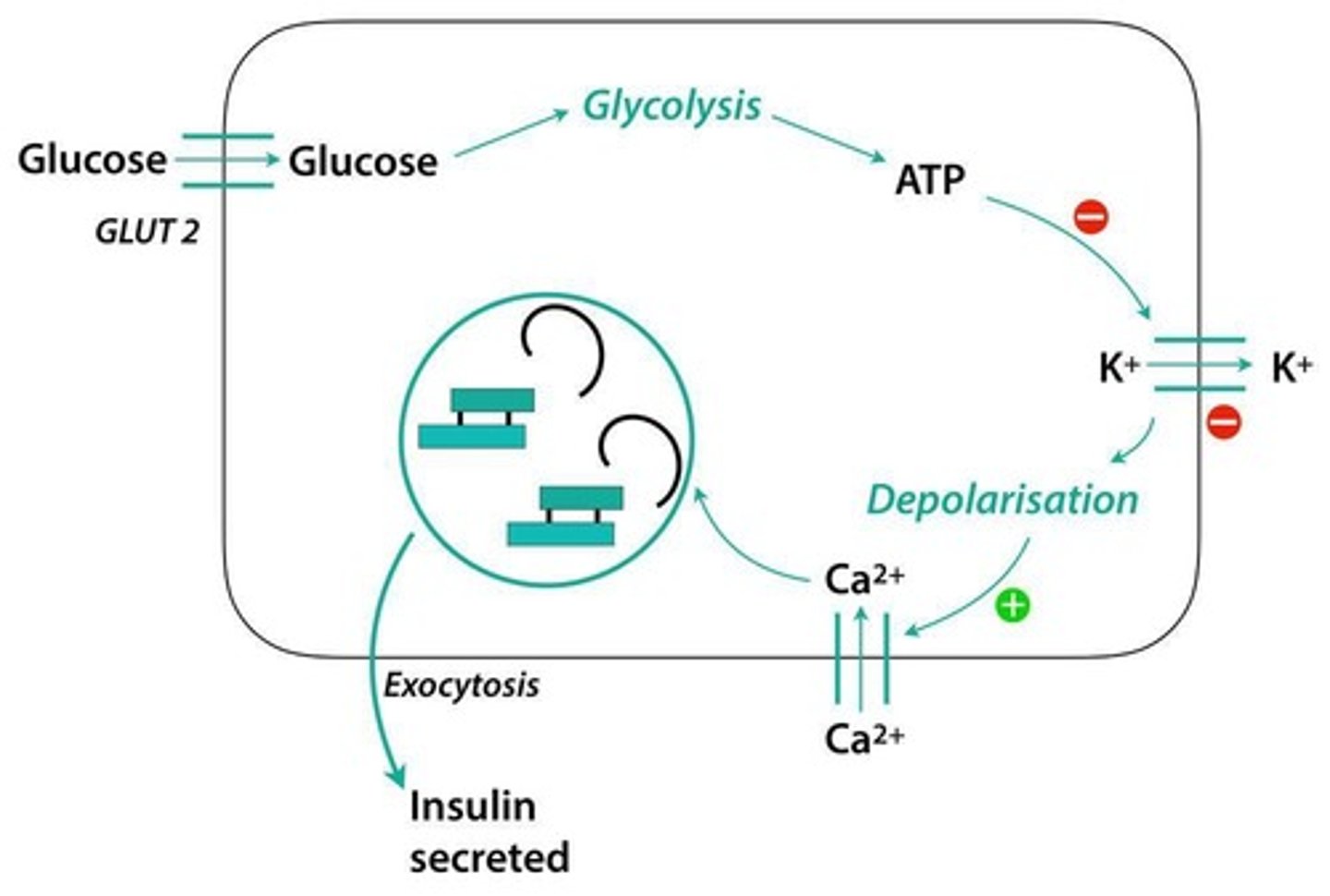
What is the role of GLUT4 transporters in insulin action?
GLUT4 transporters increase in the cell membrane, facilitating glucose uptake by insulin-sensitive cells.
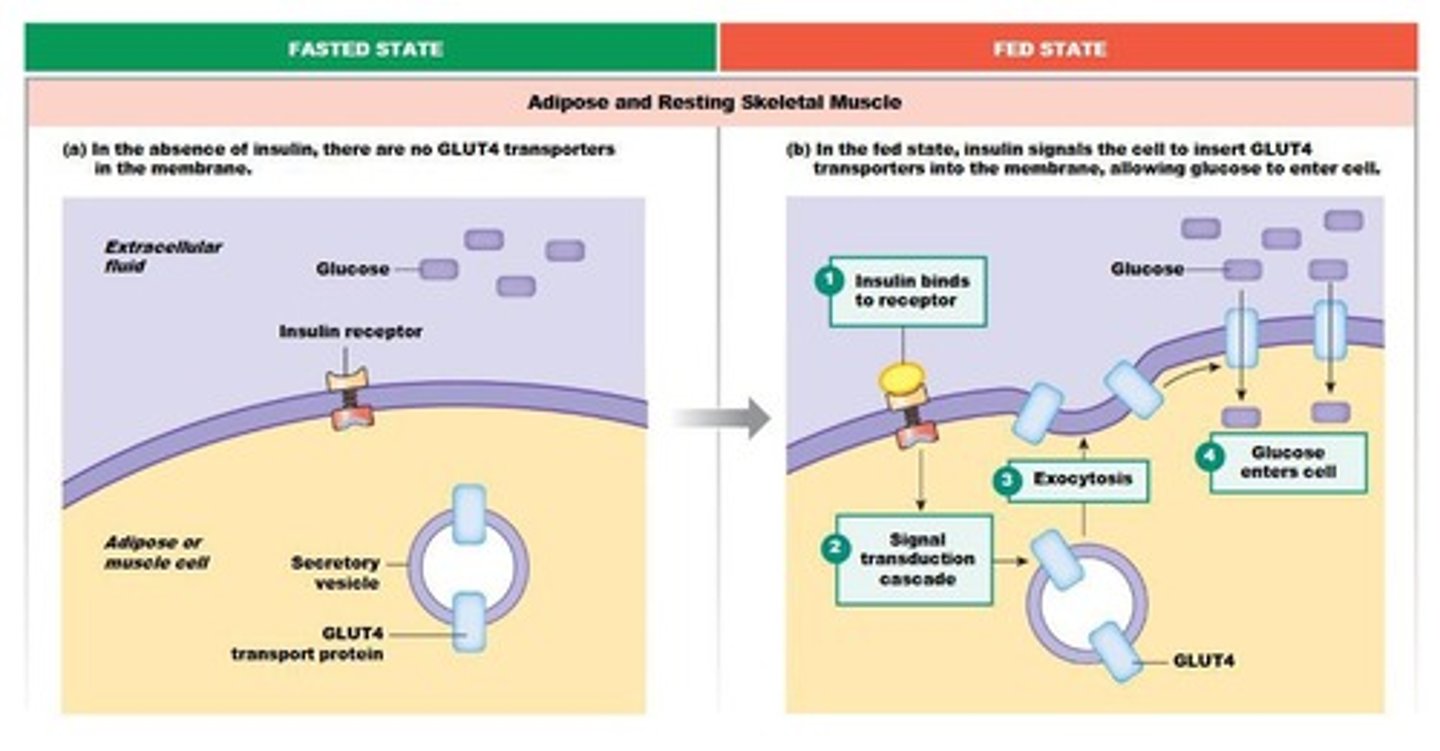
What happens to glucose once it enters muscle and liver cells?
It is phosphorylated by hexokinase to prevent it from exiting the cell and is either used for ATP production or stored as glycogen.
What is the role of glucagon in blood sugar regulation?
It increases blood sugar levels during fasting.
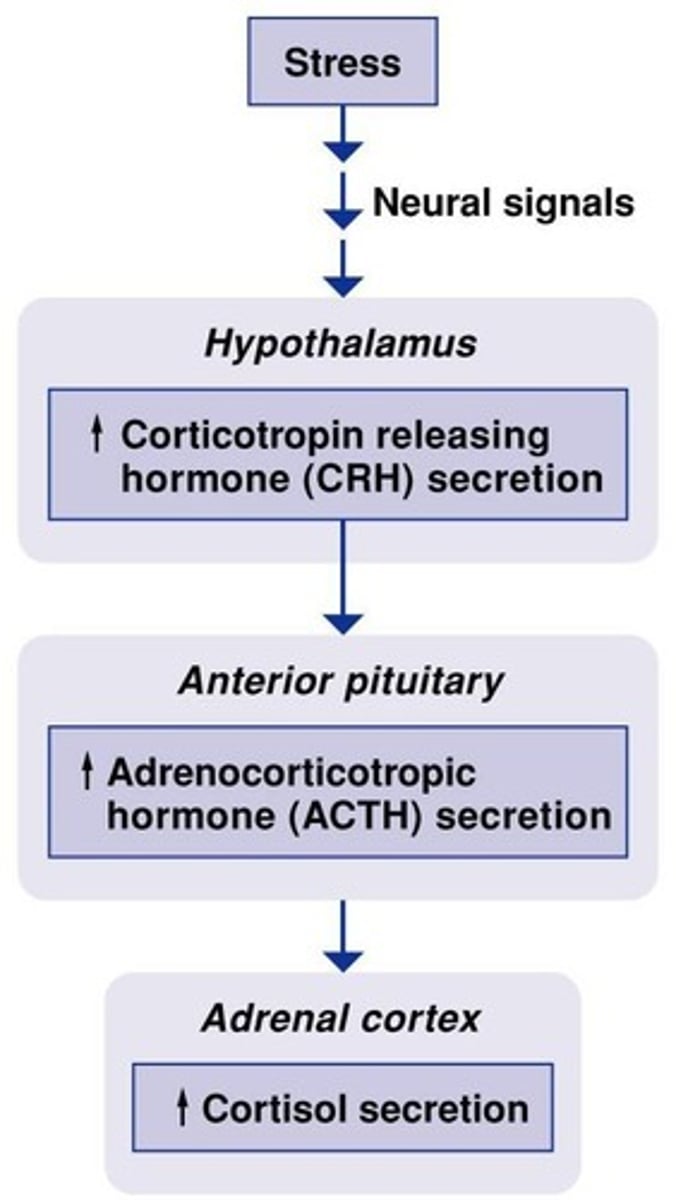
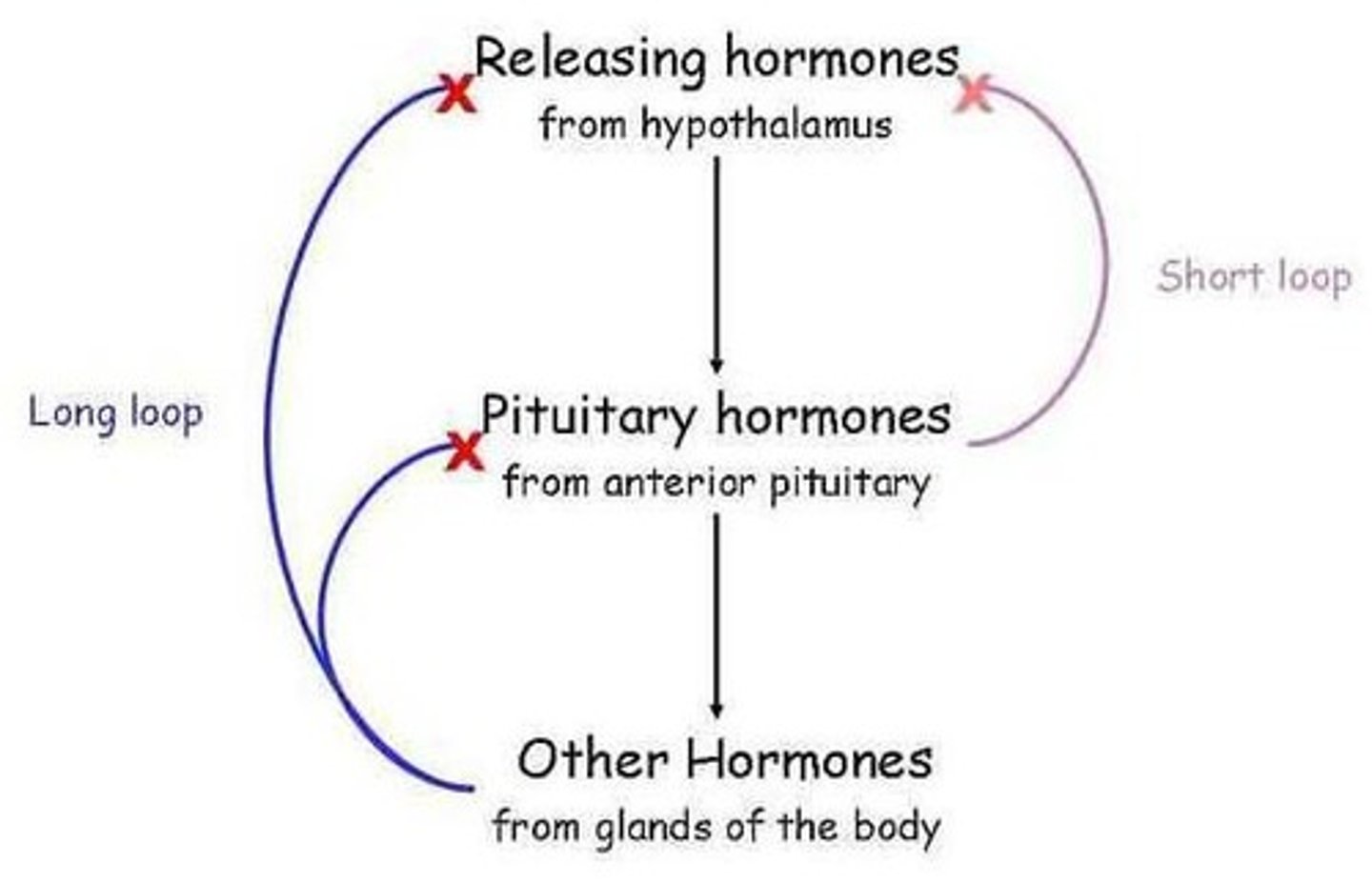
What is the HPA axis and its role in cortisol regulation?
The HPA axis involves the hypothalamus, pituitary gland, and adrenal cortex, regulating cortisol secretion through negative feedback.
What is the feedback mechanism for high blood calcium levels?
High blood calcium activates calcitonin, which inhibits osteoclasts and promotes bone synthesis.
What are the three types of hormones secreted by the adrenal cortex?
Mineralocorticoids (aldosterone), glucocorticoids (cortisol), and sex hormones (androgens).
What is the primary function of aldosterone?
Regulates plasma sodium and potassium levels and extracellular fluid volume.
What triggers the release of adrenocorticotropic hormone (ACTH)?
Corticotropin releasing hormone (CRH) from the hypothalamus.
What is the significance of the negative feedback in the HPA axis?
It ensures that hormone levels remain balanced by inhibiting further hormone release when levels are adequate.
What is the effect of cortisol on skeletal muscle?
It promotes the breakdown of skeletal muscle, primarily type FG fibers.
What is the role of osteoblasts in calcium regulation?
Osteoblasts are activated by calcitonin to promote bone synthesis and deposition of calcium.