Urology Lecture #2
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
What is the most common bacterial infection?
Cystitis
What is cystitis?
Infection of the urinary bladder
Why older men at an increased risk for cystitis?
BPH - Men have difficulty urinating and bacteria builds up in the bladder.
Who is cystitis more common in ?
Women
A 32-year-old woman presents to urgent care with a 2-day history of dysuria, urinary frequency, and suprapubic discomfort. She denies fever, chills, flank pain, or vaginal discharge. She reports one similar episode in the past year that resolved with antibiotics. She is sexually active and uses a diaphragm for contraception. Vitals are normal.
Urinalysis shows:
Positive leukocyte esterase
Positive nitrites
Moderate bacteriuria
No WBC casts
What is the most appropriate next step in management?
A) Prescribe nitrofurantoin for 5 days
B) Order a renal ultrasound
C) Begin ciprofloxacin and refer to urology
D) Reassure and observe without antibiotics
What is the diagnosis?
A) Prescribe nitrofurantoin for 5 days
1.) Cystitis
You suspect your patient has cystitis, what labs should you order?
Urine dipstick (+ nitrates, + leukocytes, Increased WBC)
Your patient has recurrent UTIs what should you order?
Renal CT or ultrasound
What are the first line antibiotics for cystitis?
1.) TMP-SMX
2.) Nitrofurantoin
3.) Fosfomycin
important to make adjustments based on culture
A 24-year-old man presents with gradual onset of left testicular pain over the past 2 days. He describes a dull ache that radiates to the left flank. He also reports dysuria and urinary frequency, but no nausea or fever. He is sexually active with multiple partners and does not consistently use condoms.
The left hemiscrotum is swollen, tender, warm, and erythematous
The epididymis is markedly enlarged and tender
Elevation of the testis relieves the pain (positive Prehn's sign)
Cremasteric reflex is intact
Urinalysis is positive for leukocyte esterase and WBCs
What is the diagnosis?
What diagnostic tests should you order?
1.) Epididymitis
2.) Urinalysis and urine culture
STI testing for C. trachomatis and N. gonorrhea
Scrotal ultrasound will find increased blood flow.
A 42-year-old man presents with 3 days of right testicular pain that has gradually worsened. He denies dysuria or urinary frequency. He is not sexually active and has no history of STIs. He does not recall any trauma. Physical exam reveals a tender, swollen epididymis, and the scrotum is warm and erythematous. Prehn's sign is positive. Urinalysis shows pyuria and bacteriuria.
What is the most appropriate empiric treatment for this patient?
A) Doxycycline 100 mg BID for 10 days + Ceftriaxone 500 mg IM once
B) Azithromycin 1 g PO once + Ceftriaxone 500 mg IM once
C) Levofloxacin 500 mg PO daily for 10 days
D) TMP-SMX DS BID for 7 days
What is the diagnosis?
1.) C) Levofloxacin 500 mg PO daily for 10 days
2.) Epididymitis
3.)
A 24-year-old man presents with gradual onset of left testicular pain over the past 2 days. He describes a dull ache that radiates to the left flank. He also reports dysuria and urinary frequency, but no nausea or fever. He is sexually active with multiple partners and does not consistently use condoms.
The left hemiscrotum is swollen, tender, warm, and erythematous
The epididymis is markedly enlarged and tender
Elevation of the testis relieves the pain (positive Prehn's sign)
Cremasteric reflex is intact
Urinalysis is positive for leukocyte esterase and WBCs
What is the most appropriate empiric treatment for this patient?
A) Ciprofloxacin and ibuprofen
B) Doxycycline and ceftriaxone
C) TMP-SMX and scrotal elevation
D) Levofloxacin and doxycycline
What is the diagnosis?
1.) B) Doxycycline and ceftriaxone
2.) Epididymitis
A 31-year-old man presents to clinic with right-sided scrotal pain that began 2 days ago and has progressively worsened. He describes the pain as a dull ache radiating to the right flank. He reports some dysuria but denies fever or urethral discharge. He is sexually active with men and engages in insertive anal intercourse.
On exam:
The right hemiscrotum is warm, tender, and swollen
Positive Prehn's sign
No testicular torsion on ultrasound
UA shows WBCs and bacteria
What is the most appropriate empiric antibiotic regimen for this patient?
What is the diagnosis?
1.) Levofloxacin 500 mg PO daily for 10 days + Ceftriaxone 500 mg IM once
2.) Epididymitis
Necrotizing fasciitis of the perineum and male genitalia
Fournier's Gangrene
Which bacteria cause Fournier's Gangrene?
•Gram negative rods such as E. coli, Klebsiella, enterococci
•Bacteroides, Fusobacterium, Clostridium, anaerobic or microaerophilic streptococci
When does mumps orchitis occur?
4-7 days after parotid symptoms with testicular pain and swelling
What is orchitis a complication of?
Epididymitis
A 19-year-old male presents with left testicular pain and swelling that began 2 days ago. He also reports fever, malaise, and myalgias. He denies dysuria, urethral discharge, or recent sexual activity. He has not been vaccinated since childhood and had a recent episode of parotitis a week ago.
The left testicle is swollen and tender, sparing the epididymis
Scrotal skin is erythematous and edematous
The epididymis is not enlarged
No inguinal lymphadenopathy
What is the most likely diagnosis?
A) Epididymitis
B) Testicular torsion
C) Mumps orchitis
D) Testicular cancer
How do you treat it?
C) Mumps orchitis
1.) Treat orchitis the same way as epididymitis. Since cause is viral mumps, treat with NSAIDs and supportive care like ice pack
A 22-year-old man presents to the clinic with painful urination and a yellow urethral discharge that started 3 days ago. He denies fever, testicular pain, or flank discomfort. He reports recent unprotected sex with a new partner 1 week ago.
Physical exam reveals a mucoid urethral discharge, no scrotal tenderness, and no inguinal lymphadenopathy. UA shows positive leukocyte esterase and pyuria, but urine culture is pending.
What is the most appropriate next step in management?
A) Ciprofloxacin and phenazopyridine
B) TMP-SMX and doxycycline
C) Ceftriaxone IM + doxycycline for 7 days
D) Azithromycin 2 g PO x1
What is the diagnosis?
C) Ceftriaxone IM + doxycycline for 7 days
Urethritis
What is the most common cause of balanitis?
Inadequate hygiene in uncircumcised man
A 46-year-old uncircumcised man presents with 3 days of penile irritation, pruritus, and mild pain at the glans. He notes increasing redness and some white, curd-like discharge under the foreskin. He denies dysuria, fever, or urethral discharge. He has a history of type 2 diabetes mellitus, poorly controlled. No recent antibiotic use.
On physical exam:
The glans penis is erythematous and edematous
There is a thick white exudate beneath the foreskin
No urethral discharge or inguinal lymphadenopathy
What is the most appropriate initial treatment?
A) Oral fluconazole
B) Topical miconazole or clotrimazole
C) Oral ceftriaxone and doxycycline
D) Topical corticosteroids alone
What is the diagnosis?
B) Topical miconazole or clotrimazole
1.) Balanitis
What is bladder incontinence?
Involuntary loss of urine
leakage of urine upon coughing, sneezing, or standing
Stress incontinence
Urgency and inability to delay urination. Decreased bladder compliance and detrusor overactivity.
Urge incontinence
Involuntary loss of urine from chronic urinary retention
Overflow incontinence
Why is overflow incontinence more common in older men then younger men?
Bladder outlet obstruction (BPH)
What causes bladder incontinence?
DIAPPERS
D - Delirium
I - Infection
P - Pharmaceuticals
P - Psychological factors
E - Excessive urinary output
R - Restricted mobility
S - Stool impaction
How do you test for bladder inconinence?
Stress incontinence - Have patient with full bladder relaz perineum and cough vigorously while standing, if leakage then they have stress incontinence.
A 67-year-old woman presents with complaints of sudden episodes of urinary leakage over the past several months. She says she often feels a strong, uncontrollable urge to urinate and cannot make it to the bathroom in time. These episodes occur during the day and sometimes at night. She denies stress-related leakage (e.g., when coughing or sneezing). She voids frequently and reports a long-standing history of overactive bladder.
Physical exam is unremarkable, and a post-void residual volume is within normal limits. UA is negative for infection.
Which of the following is the most appropriate first-line pharmacologic treatment?
A) Mirabegron
B) Oxybutynin
C) Pseudoephedrine
D) Bethanechol
B) Oxybutynin
78-year-old man presents to the clinic with constant dribbling of urine and a sensation of incomplete bladder emptying. He reports straining to urinate, a weak urinary stream, and getting up multiple times at night to void. He denies dysuria or urgency. He has a history of benign prostatic hyperplasia (BPH) and is not currently on any medications for it.
His bladder is palpable and distended
Post-void residual volume is over 300 mL
DRE reveals an enlarged, smooth prostate
What is the next best step in management?
A) Begin tamsulosin and monitor for symptom improvement
B) Refer for prostate biopsy
C) Urgent catheterization and urologic referral
D) Prescribe oxybutynin
C) Urgent catheterization and urologic referral
What are some treatment options for urinary incontinence?
- Topical estrogen
- Anticholinergic meds
- Beta 3 adrenergic agonists
-
What should you do in your workup of overactive bladder?
Rule out UTI
Check for post void residual urine
A 72-year-old woman presents with complaints of frequent urination and a sudden urge to void that she cannot always control. She reports waking up 2-3 times a night to urinate and occasional leakage of urine before reaching the toilet. She denies dysuria, fever, or hematuria.
Physical examination is unremarkable. Urinalysis is negative for infection. Post-void residual volume is 30 mL.
What is the most appropriate initial treatment?
A) Tamsulosin
B) Topical estrogen
C) Bladder training and timed voiding
D) Urethral bulking agent injection
C) Bladder training and timed voiding
What is the first line treatment for overactive bladder?
Bladder training and pelvic floor strengthening
What is the 2nd line treatment for overactive bladder?
Anticholinergic meds, beta 3 adrenoreceptor agonists
What is the 3rd line treatment of overactive bladder?
Sacral neuromodulation
Peripheral tibial nerve stimulations
Intravesical botox
What is vesicoureteral reflux?
A pediatric urologic condition where urine flows backward from the bladder into the ureters and sometimes up to the kidneys
This condition although a pediatric is not usually diagnosed until adolescence when patients present with hypertension and substantial proteinuria
Vesicoureteral reflux
A 3-year-old girl is brought to the pediatric clinic by her mother due to fever, vomiting, and dysuria for the past 2 days. She has had multiple febrile UTIs over the past year. On examination, she is febrile to 101.8°F (38.8°C) and appears ill. Abdominal palpation elicits mild suprapubic tenderness.
Labs:
UA: + leukocyte esterase, + nitrites, + WBCs
Urine culture: E. coli >100,000 CFU/mL
A renal and bladder ultrasound shows hydronephrosis and cortical scarring on the left kidney.
What is the most appropriate next step to confirm the diagnosis?
VCUG - Voiding cystourethrogram
What can renal ultrasound or IVP show you in someone with vesicourethral reflux?
Renal scarring or hydronephrosis
Who is IVP contraindicated in?
Patients with kidney dysfunction who are at a higher risk for contrast nephropathy
A 5-year-old boy presents for follow-up after a recent hospitalization for febrile pyelonephritis. This was his second documented episode of a febrile UTI in the past year. He has been doing well since discharge, and the mother denies current symptoms. Physical exam is unremarkable.
The primary care provider wants to evaluate for possible structural abnormalities, renal damage, or hydronephrosis related to recurrent infections.
What is the most appropriate initial imaging test to evaluate renal anatomy and potential scarring?
A) Voiding cystourethrogram (VCUG)
B) MRI of the kidneys
C) CT urography
D) Renal ultrasound or IVP
What is this condition?
D) Renal ultrasound or IVP
1.) Vesicoureteral reflux
Which vesicoureteral reflux grade is this?
Reflux into a ureter without dilatation
Grade 1
Which vesicoureteral reflux grade is this?
Reflux into the renal pelvis and calyces without dilatation
Grade II
Which vesicoureteral reflux grade is this?
Mild to Moderate dilatation of the ureter, renal pelvis, and calyces with minimal blunting of the fornices
Grade III
Which vesicoureteral reflux grade is this?
Moderate ureteral tortuosity and dilatation of the renal pelvis and calyces
Grade IV
Which vesicoureteral reflux grade is this?
Gross dilatation of the ureter, pelvis, and calyces; loss of papillary impressions; ureteral tortuosity
Grade 5
How do you treat grade 1-2 vesicoureteral reflux?
Monitor - Low risk of pyelonephritis and can resolve spontaneously
How do you treat grades 3-5 vesicoureteral reflux?
Antibiotic prophylaxis and surgical correction may be needed
Persistent unpleasant sensations attributable to the bladder.
Interstitial cystitis
A 35-year-old woman presents to the clinic with a 6-month history of urinary urgency, frequency, and suprapubic pain. She reports that the pain worsens when her bladder is full and improves after urination. She denies dysuria or hematuria. She has no fever, and her urine culture is negative. She notes that certain foods and stress make her symptoms worse. Pelvic exam reveals tenderness in the bladder base and mild allodynia.
What is the most likely diagnosis?
A) Acute cystitis
B) Endometriosis
C) Interstitial cystitis
D) Urethritis
How do you treat it?
C) Interstitial cystitis
1.) Supportive care, can use pentosan polysulfate sodium
Bladder injuries are most commonly associated with ________.
pelvic fractures
How do you diagnose ureteral injury?
CT urograpm, IVP, or cystoscopy with retrograde pyelogram
A 65-year-old man undergoes transurethral resection of the prostate (TURP). Post-operatively, he develops lower abdominal pain and difficulty voiding. Foley catheterization yields 600 mL of blood-tinged urine. Imaging shows contrast extravasation confined to the area around the bladder but not into the peritoneal cavity.
Which of the following is the most appropriate initial management?
A) Immediate surgical repair
B) Cystoscopy
C) Foley catheter drainage with observation
D) Intravenous antibiotics only
What is the diagnosis?
C) Foley catheter drainage with observation
This is an extraperitoneal bladder injury. Often due to iatrogenic or pelvic trauma, are usually managed non-operatively with large-bore Foley catheter drainage unless complications arise.
A 29-year-old male is brought to the trauma bay after a motorcycle collision. He was wearing a helmet but sustained a blunt force injury to the lower abdomen from hitting the gas tank. He is awake and alert but complains of severe lower abdominal pain and inability to urinate. Foley catheter placement yields gross hematuria.
Focused Assessment with Sonography for Trauma (FAST) is negative for free fluid. A CT cystogram is performed and shows contrast extravasation into the peritoneal cavity, surrounding loops of bowel.
What is the most appropriate next step in management?
What is the diagnosis?
1.) Immediate surgical repair
2.) Intraperitoneal bladder injury
What are delayed intraperitoneal injuries associated with?
Azotemia, ascites, sepsis
What is the second most common urologic malignancy?
Bladder cancer
What is a risk factor for bladder cancer?
Tobacco use
You suspect your patient has bladder cancer, what labs do you order?
UA/microscopic UA
Urine cytology
Urovysion test
How do you definitely diagnose bladder cancer?
Cystoscopy with biopsy/transurethral resection of bladder tumor.
A 67-year-old male with a 40-pack-year smoking history presents to the clinic with complaints of intermittent episodes of painless gross hematuria over the past month. He denies flank pain, fever, dysuria, or recent trauma. He reports increased urinary urgency and frequency for several months but attributed it to age. He has no history of urinary tract infections. A urinalysis confirms >3 RBCs/HPF, and urine culture is negative. A CT urogram is ordered and shows a filling defect within the bladder wall.
Which of the following is the most likely diagnosis?
A) Bladder cancer
B) Cystitis
C) Nephrolithiasis
D) Benign prostatic hyperplasia (BPH
A) Bladder cancer
What is the most common type of bladder cancer?
Urothelial carcinoma
What stage of bladder cancer is only the superficial layers affected?
Tis
Ta
Which bladder cancer stage is the following description?
Invasion into mucosal layer (Lamina Propria
Stage T1
Which bladder cancer stage is the following description?
Invasion into detrusor muscle
T2
Which bladder cancer stage is the following description?
Invasion into perivesical tissue
T3
Which bladder cancer stage is the following description?
Invasion into surrounding structures
T4
How do you treat bladder cancer?
Resect the tumor, surveillance with routine cystoscopies to evaluate for recurrence
How do you treat T2 bladder cancer?
Gold standard is radical cystectomy and urinary diversion
A 66-year-old man presents with painless gross hematuria. CT urogram reveals a bladder mass. Cystoscopy with biopsy confirms urothelial carcinoma invading the muscularis propria. There is no evidence of distant metastasis. He is otherwise healthy and desires definitive treatment.
Which of the following is the most appropriate next step in management?
A) Intravesical BCG therapy
B) Neoadjuvant chemotherapy followed by radical cystectomy
C) Transurethral resection (TURBT) alone
D) Surveillance cystoscopy every 3 months
B) Neoadjuvant chemotherapy followed by radical cystectomy
This is stage T2 bladder cancer since it has invaded detrusor muscle.
Who is urethral prolapse most common in?
Prepubertal females and postmenopausal women
A 72-year-old postmenopausal woman presents with complaints of vaginal bleeding and urinary urgency. She denies any recent trauma or infection. On physical exam, a doughnut-shaped, erythematous mass is observed protruding from the urethral meatus. She reports mild tenderness but no fever or systemic symptoms.
What is most likely the diagnosis?
How do you confirm this diagnosis?
How do you treat it?
- Urethral prolapse
- Confirmed with the identification of urethral meatus as the central opening in prolapsed tissues.
- Treatment
--> first rule out UTI
--> sitz baths and topical estrogen
donut shaped mass at anterior vaginal wall
Urethral prolapse
Your patient has urethral prolapse with urethral strangulation, what do you do?
Consult urology emergently
What is urethral stricture?
Fibrotic narrowing composed of dense collagen and fibroblasts
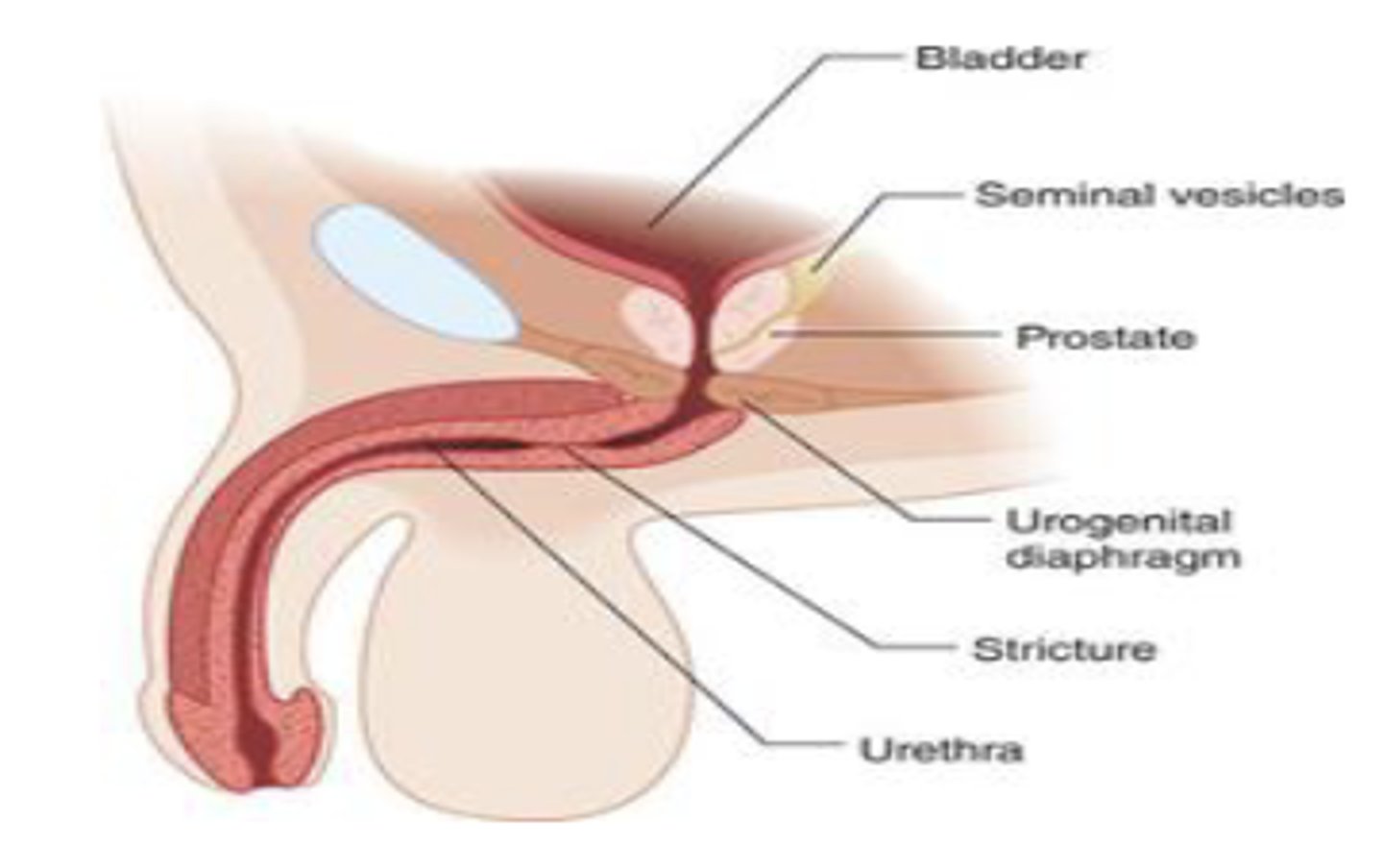
What is a common complication of urethral stricture?
Prostatitis
A 57-year-old man presents with a 6-month history of progressive difficulty urinating. He reports a slow urinary stream, straining to void, and post-void dribbling. He denies dysuria or fever. He also notes his urinary stream has become splayed, and he occasionally notices blood in his semen. His past history includes a sexually transmitted infection 10 years ago.
On physical examination, there are no palpable masses, and the bladder is non-distended. A post-void residual reveals 150 mL of retained urine.
Which of the following is the most likely diagnosis?
A) Benign prostatic hyperplasia
B) Urethral stricture
C) Bladder outlet obstruction due to stone
D) Prostatitis
How you diagnose this condition?
How do you treat this condition?
1.) B) Urethral stricture
2.) RUG, VCUG, local flexible cystoscopy, flow rate and post void residual
3.) Urethral dilation
Blood at the meatus
Urethral injury
A 26-year-old male is brought to the emergency department after a high-speed motorcycle crash. He is conscious but reports severe pelvic pain. Physical exam reveals ecchymosis over the perineum and lower abdomen, a high-riding prostate on digital rectal exam, and visible blood at the urethral meatus. A Foley catheter has not yet been placed.
Which of the following is the most appropriate next step in management?
A) Immediate Foley catheter placement
B) Abdominal CT with contrast
C) Retrograde urethrogram
D) Cystoscopy
E) Non-contrast CT of the pelvis
What is the diagnosis?
How do you treat it?
C) Retrograde urethrogram
1.) This patient has a urethral injury
2.) Suprapubic cystostomy - Standard management
Reconstructive surgery - Definitive treatment
What is definitive treatment for urethral injury?
Reconstructive surgery