MELS500 End of semester
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
61 Terms
Histology
The study of microscopic anatomy of tissue (cells) - morphology and its function
Histopathology
The study of structural and functional abnormalities that are expressed as diseases of organs and systems.
What is single piece workflow?
Working with one specimen at a time
Describe histological workflow
What is the technological workflow?
Accessioning, gross cutup verification, tissue processing, embedding, microtomy, primary and advanced staining, case assembly, pathologist review, archive
Name seven details you can find in a lab request form
Patient name, NHI, Date of birth and age, Specimen details, Theatre or clinic, Time/date taken, Name of requesting clinician, contact details of requesting clinician
Describe the four classifications of laboratory hazards
Chemical, Physical, Biological, Psychosocial
What happens when an anomaly is found during specimen reception?
Requesting clinician is contacted and they either visit/fax the ab to correct this error (including the request form) and the specimen is registered with its’ relevant anomaly code
What are the aims of fixation and how is this achieved?
To preserve cells and tissue to mimic the state of it as if it were in the body, stop enzyme breakdown (autolysis) and microbial activity (putrefaction).
Precipitation
Coagulation
Autolysis
The shutdown of oxygen supply and the breakup of living tissue
Putrefaction
The breakdown of tissue by bacteria
What are the 5 properties of a good fixative?
Safe to handle, readily available, cheap, stable, penetrates tissue well without causing damage
What affects fixation?
Temperature, concentration of fixative, duration, mode of fixation, use of buffer, use of vacuum and agitation, penetration rate
How can we speed up fixation?
Concentration, type of fixative, temperature, size and thickness of tissue, type of tissue (fatty or bloody)
What are some of the limitations of fixatives?
Slow procedure, limited use on hard tissue, section thickness, loss of tissue constituents (lipids and enzymes)
Artefacts
Pigments which are created when exposed to a certain fixative
List 3 different kinds of artefacts
Formalin, mercury, dichromate
How to artefacts effect tissues?
Osmotic effects (volume changes in tissue), diffusion of labile substances (glycogen), leaching of substances, chemical changes
What are the three classifications of fixatives?
Microanatomical, histochemical, cytological
Name three examples of simple (neat) fixatives
Picric acid, chromic acid, potassium dichromate
Name three examples of compound (combination) fixatives
Formaldehyde, Bouins, Mercury
What are the two buffer salts used for 10% NBF
Sodium hydrogen phosphate and sodium dihydrogen phosphate
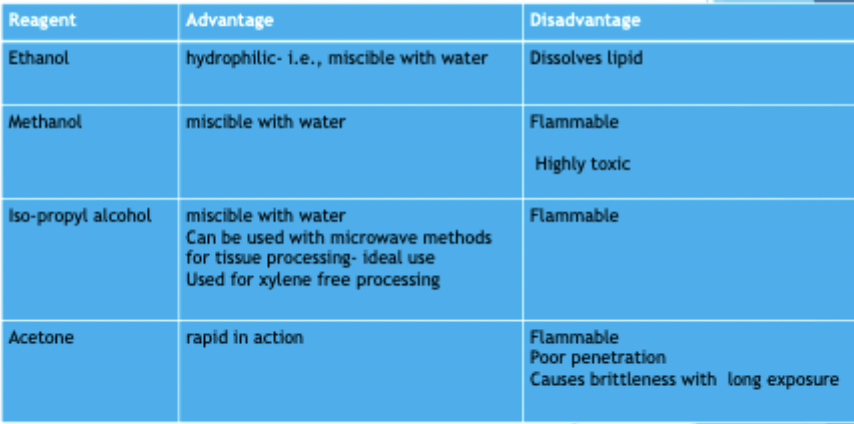
Name the advantages and disadvantages of ethanol, methanol, and acetone as fixatives
ADVANTAGES
Recommended for preservation of glycogen
At low temp may preserve enzymes
DISADVANTAGES
Acts by disrupting protein’s tertiary structure leading to protein coagulation
Harden tissue
Causes shrinkage
Doesn’t fix lipids
How would you demonstrate fat in a tissue?
Decalcification
The removal for calcium salts (insoluble calcium salts are converted into soluble calcium salts by the action of the decalcifying agent so that the tissue becomes soft)
What is the process of decalcification?
Careful preliminary assesment, Proper fixation, Preperation of slices at a reasonable thickness for fixation and processing, choosing a suitable decalcifier (adequate volume, regular changing of this liquid), Determining an endpoint, processing using a suitable schedule
List the 3 criteria for decalcifying agents
Complete removal of calcium salts
Causes no damage to tissue
No adverse effect on the subsequent process
Minimal time
How is decalcification acheived?
Name one example of a strong and weak acid used
What does a chelating agent do?
Binds to calcium ion present in bone to carry out decalcification
What are the characteristics of ion exchange resins?
Faster decalcifying rate
Preserves cellular details
No need to changed solution
Resin can be re-used
What are the advantages and disadvantages of electrophoretic decalcification?
ADVANTAGES
Shortened time for complete decalcification
Better preservation of soft tissue
DISADVANTAGES
Limited number of specimens processed at a time
Not very practical
What four factors effect decalcification?
Concentration, temperature, agitation, fluid access
How do we know when decalcification is finished? What is the most ideal?
poking, prodding, bending (physical)
chemical tests (ammonium oxalate solution)
x-ray - most ideal (no damage)
Tissue processing
A procedure taking place between tissue fixation and embedding
What is the end goal of tissue processing?
Support the tissue before they can be sectioned for microscopy via infiltration and embedding
What is the most widely used infiltrating media used in histology?
What are the pre-requisites for tissue-processing?
Well-fixed, suitable size, proper placement in cassette (not squeezed in and wrapped in foam if fragile or minute)
What factors effect tissue processing?
Type of tissue (bone or fatty)
Reagent type
Agitation/fluid access
Temperature
Vacuum
What is the use of a vacuum in tissue processing?
Removes air bubbles, decreases boiling point of wax (viscosity), lowers boiling point of clearing agents (flammable)
What are the stages for tissue processing?
Fixation, dehydration, clearing, wax infiltration/impregnation
What agents are used for dehydration and what are their advantages and disadvantages?
What clearing agents can be used for tissue processing and what are their advantages and disadvantages?
Clearing agent - removes dehydrating agent
What considerations are there regarding clearing agents?
Must be miscible with dehydrating reagent and with infiltrating and embedding medium
What is the purpose of wax infiltration?
What should be considered for wax selection?
Stable at room temp, causes no tissue damage, safe to handle, readily available, used for all tissues
What will effect infiltration?
Size and type of tissue, clearing agent used, use of vacuum
Coagulant and Anticoagulant (fixatives)
Tolerant and anti-tolerant (fixatives)
Embedding
The technique of placing cells or tissue in a supporting medium so that thin sections can be cut using a microtome
What is the melting point of paraffin wax?
55º to 65º
What is the function of each embedding station?
Wax resovoir - holds wax
Forceps warmer
Cassette-holding tank
Mold bin
Wax dispenser
Cold plate - cool specimens
What is the procedure for embedding?
Open cassette
Check the tissue and lid
Select appropriately sized mould
Fill the mould a third-ways with paraffin
Place the tissue centrally in the mould ensuring the orientation is correct
Tamp the tissue down
Place the cassette onto the mould
Fill the cassette with wax to the top
Cold plate
Microtomy
The method of preparing thin sections using a microtome for microscopic study
What is the purpose of microtomy?
To enable the transparency of stained tissues and cells when viewing microscopically
How do you master microtomy?
Have a thorough knowledge of the equipment used and the type of investigation required and well -fixed good quality tissue
What is specimen tracking and why do we do it?
Identifies the patient information and any previous test carried out on the sample (esp. when additional tests are required)
Allows labs to know where samples are in the testing process
Why do we record anomalies and what are the repercussions of no recording them?
To establish a diagnosis and to allow the proper treatment for the patient.
Why do we QC?