Parasites and Parasites tutorial
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
What are parasites?
Parasites are organisms (largely eukaryotes) that live in or on another organism, called the host, and benefit by deriving nutrients at the host's expense
What biological associations occur between species? link to parasitism ?
-SYMBIOSIS (living together).
-Relationship between 2 or more organisms. Usually long term.
Parasitism is a close and persistent long-term biological interaction between the parasite and its hos
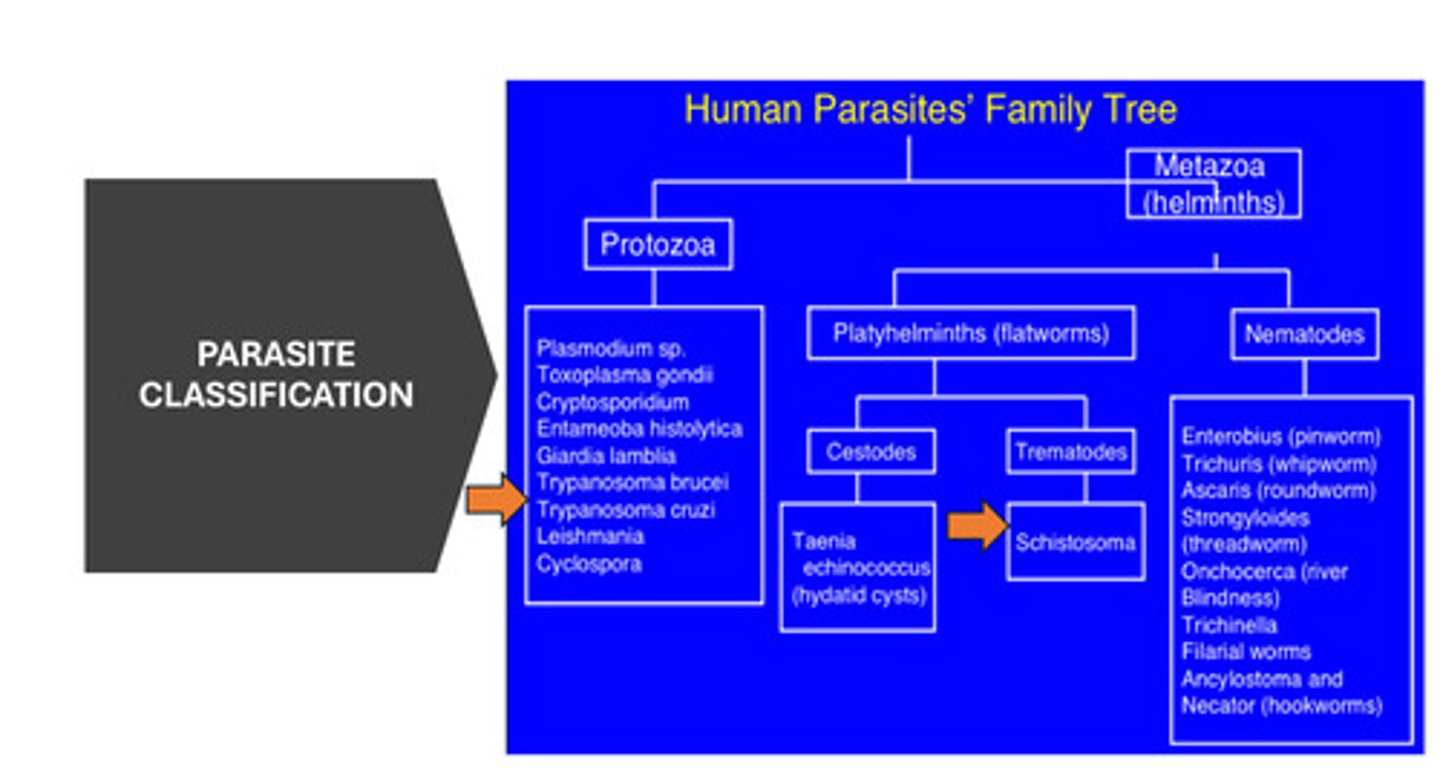
Parasite Classifications
What are:
-Ectoparasites
-Endoparasites
-Permanent (obligate) parasites
- Facultative parasite
- Pathogenic parasites
-Non-Pathogenic parasite
-Opportunistic parasites
• • Ectoparasites: Lives on surface of host E.g. lice, tick.
• Endoparasites: Lives within the body of the host. Plasmodium species, Ascaris species.
• Permanent (obligate) parasites: Can not live without its host. E.g. Trypanosoma species, Plasmodium species, Trichmonas vaginalis.
• Facultative parasite: Able to survive without the host if alternative food source becomes available. E.g. Candida albicans, Naegleria fowleri, etc.
• Pathogenic parasites:- It causes disease in the host. E.g., E. histolytica
• Non-Pathogenic parasite:- Mostly harmless, obtains food and protection from the host without causing harm. E.g. Entamoeba coli
• Opportunistic parasites:-Parasites which cause mild disease in immunologically healthy individuals, but they cause severe disease in immuno-deficient hosts. E.g. Candida albicans, Toxoplasma gondii.
HOST CLASSIFICATION
What are:
• Definitive host:
• Intermediate host
• Animal reservoir host
• Accidental (Incidental) host:
• Paratenic host
• Definitive host:- The host for the adult stage of a parasite/most highly developed form/ sexually mature stages of a parasite/fertilization e.g Mosquito is the definitive host for malaria.
• Intermediate host:- The host for sexually immature/larval stage of a parasite/no fertilization takes place. e.g. Pig is an intermediate host for Taenia solium.
• Animal reservoir host:- Acts as sources of infection to the definitive host e.g Monkeys in South-east Asia as reservoir host in malaria transmission. Trichinellosis/Trichinosis (swine).
• Accidental (Incidental) host:- Life cycles can not be completed. Not the target host. The eggs of a fish parasite accidentally swallowed by a human.
• Paratenic host – No development of the parasite until it reaches the definitive host. Fish hosts harbours Diphyllobothrium latum, until eventually eaten by humans or other final host
Terminologies
What is:
Vectors
Zoonosis
Endemic
Epidemic
Pandemic
-Vectors:- Usually arthropods or other living carriers which transmit a disease (vector-borne disease).
-Zoonosis:- Diseases from vertebrate animals to humans.
-Endemic – A disease regularly found/always present among particular people or in a certain area.
-Epidemic – Rapid spreading of a disease, may result in deaths.
Pandemic – World-wide spread of a disease (usually a new disease)
Parasite Classification diagram
What causes Malaria, how is it spread and who is most vulnerable to it?
• Pregnant women and children are most vulnerable.
• Malaria is caused by Plasmodium parasites. The parasites are spread to people through the bites of infected female Anopheles mosquitoes (malaria vectors) which bite mainly between dusk and dawn. -Temporary, facultative ectoparasites
What are the parasite species that cause malaria in humans:
• Plasmodium falciparum -Most common in Africa, the most dangerous form of malaria, with the highest rates of complications and mortality. Debilitating anaemia is caused by Chronic infections
• Plasmodium vivax - Most geographically widespread, produces less severe symptoms. Relapses, however, can occur for up to 3 years, and chronic disease is debilitating. Once common in temperate climates, P. vivax is now found mostly in the tropics, especially throughout Asia.
• Plasmodium malariae - typical malaria symptoms, can persist in the blood for very long periods, individuals can have it for decades without ever producing symptoms (Note: these asymptomatic individuals can infect others, eithre through blood donation or mosquito bites)
• Plasmodium ovale - rare, can result in relapses, and generally occurs in West Africa
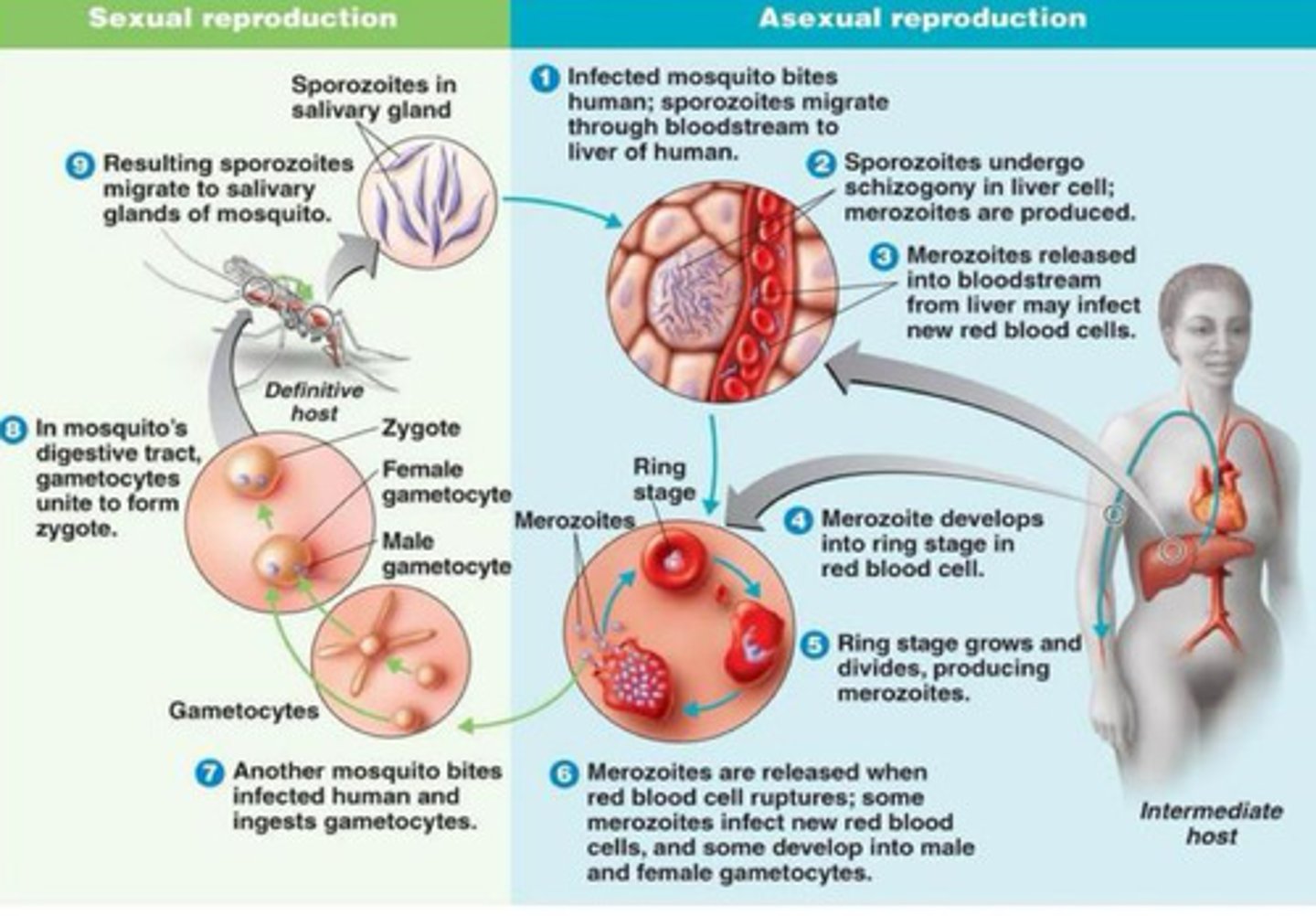
What are the 2 hosts of Plasmodium?
• Human – Intermediate host where asexual reproduction takes place. Sporozoites are the infective stage for human.
• Mosquito – definitive (final) host where sexual reproduction occurs. The infective stage for mosquito are the gametocytes
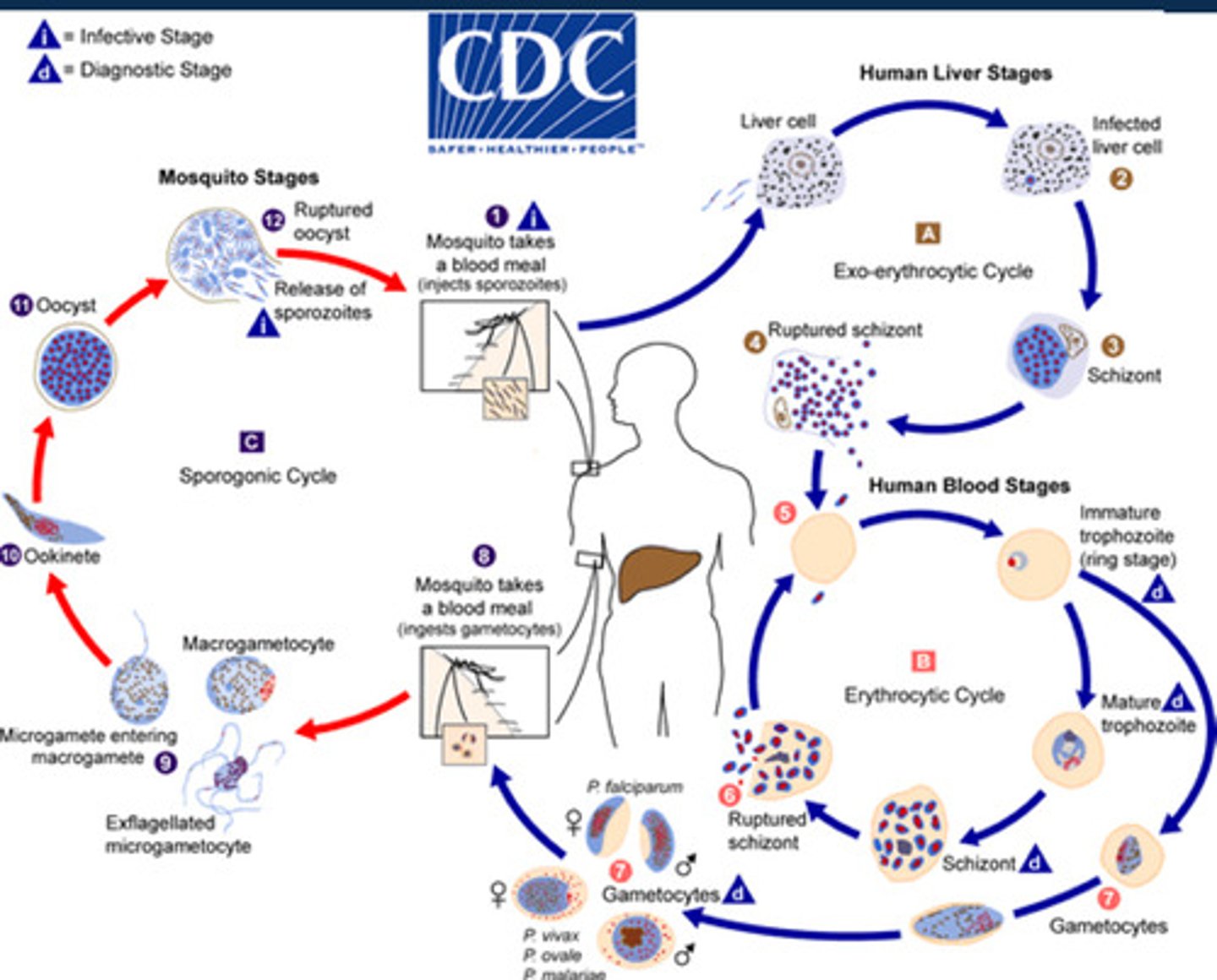
What are the 3 stages of the life cycle of the Plasmodium species that causes malaria?
1. Exoerythrocytic stage (in the liver of humans): After an infected female Anopheles mosquito bites a human, sporozoites enter the bloodstream and travel to the liver, where they infect liver cells. Sporozoites undergo schizogony in the liver cell to produce merozoites (Parasite has now multiplied) . These are released into the blood stream from the liver to go on to infect new red blood cells (leads you on to the Erythrocytic stage)
2.Erythrocytic stage (in human red blood cells): The parasite leaves the liver and infects red blood cells (RBCs), where it continues to multiply. This stage is responsible for the clinical symptoms of malaria, such as fever, chills, and anemia.
3. Sporogonic stage (in the mosquito): When a mosquito bites an infected person, it ingests the gametocytes (sexual forms of the parasite) from the bloodstream. These gametocytes develop and reproduce in the mosquito’s gut, eventually forming sporozoites, which migrate to the mosquito's salivary glands, ready to infect another human host.
This life cycle allows Plasmodium to alternate between human and mosquito hosts, ensuring its survival and transmission.
Specifics in diagram
What are the clinical features of malaria (Plasmodium infection)
• Malaise and headache
• Fever, chills and sweats
• myalgia and abdominal pain
• vomiting
• mild watery diarrhoea
• anaemia
• mild jaundice
• splenomegaly
• pulmonary symptoms -cough (children)
• convulsions (children)
What are the increased complications in Severe falciparum malaria
• Increased risk of mortality from malaria infection
• Manifests with distinct syndromes: Severe anaemia, severe respiratory distress, coma
How do we diagnose Malaria?
• WHO recommends prompt malaria diagnosis either by microscopy or malaria rapid diagnostic test (RDT) before treatment.
• Diagnostic testing improves the disease management help to reduce the emergence and spread of drug resistance by reserving antimalarial medication for confirmed cases.
• Malaria rapid diagnostic tests (RDTs) have the potential to greatly improve the quality of management of malaria infections, especially in remote areas with limited access to good quality microscopy services
• Blood for the test is commonly obtained from a finger-prick and results are available within 15-30 minutes. Diagnosis continued • Detect specific antigens (proteins) produced by malaria parasites .
• Can detect a single or multiple species of and some further distinguish between P. falciparum and non-P. falciparum infection, or between specific species.
Explain the importance behind microscopy and Malaria?
-Centrepiece of malaria diagnosis in most large health clinics and hospital
• Method of choice for the investigation of malaria treatment failures.
• Identification of Plasmodium parasites species and various parasite stages (for example, trophozoites, gametocytes)
• The quantification of parasite density to monitor response to treatment.
• Giemsa is the classical stain used for malaria microscopy.
• Examination of both thin and thick films from the same patient
How do we prevent malaria?
• Personal protection and the environmental management of mosquitoes are important in preventing illness.
• Mosquito bed nets are in use in endemic areas to prevent mosquito bites
-Vaccines (Current vaccine has approximately 50% protective efficacy)
Treatments for malaria (chemotherapy)
1.Quinoline: Inhibits hemecrystallization 2. Artemisinin: Binds hemeiron/iron and generates oxygen radicals. Damages SERCA Ca++ P-ATPase
3. Antifolate: Inhibit DNA synthesis
4. Atovaquone: Collapses mitochondrial membrane potential 5. Antibacterial: ribosome inhibition-tetracycline, clindamycinand erythromycin, DNA gyraseinhibition-fluoroquinolones
What is TRYPANOSOMA?
is a genus of parasitic protozoa that causes serious diseases in humans and animals.
-Humans are the main host except for T. b.brucei
What is African Trypanosomiasis and what parasite causes it?
-Sleeping sickness
This is widely caused by protozoan parasites of the genus Trypanosoma.
-They are transmitted to humans by tsetse fly (Glossina genus).
• HAT – T. brucei rhodensienses and T. brucei gambienses.
• AAT – T. brucei brucei (Nagana)
- Diagnosis and treatment of the disease is complex and requires specifically skilled staff.
• Many cases go undiagnosed and unreported.
• Sleeping sickness is curable with medication, but is fatal if left untreated.
What are the 2 are two subspecies of Trypanosoma brucei that affect humans?
Trypanosoma brucei gambiense: Causes a chronic form of the disease, primarily found in West and Central Africa.
-Trypanosoma brucei rhodesiense: Causes an acute form of the disease, primarily found in East and Southern Africa.
Trypanosoma brucei gambiense : Disease profile - symptoms and how is it transmitted
• Infection is by a bite from an infected tsetse fly, which is only found in West Africa.
• 1 to 3 weeks infective bite develops into a red sore (chancre).
• Several weeks to months later, other symptoms include fever, rash, swelling of the face and hands, headaches, fatigue, aching muscles and joints, itching skin, and swollen lymph nodes. '
• T. b. gambiense trypanosomiasis results essentially from man-to-man transmission, and the animal reservoir plays a role in sustaining the disease only in low-incidence areas.
What is the effect of T. brucei gambiense infection on the CNS?
• Illness progression - Weight loss, Progressive confusion, personality changes, daytime sleepiness with night time sleep disturbances, and other neurologic problems.
• Patients fall into coma and death will eventually occur after several years of infection if untreated
What is the epidemiology of T. brucei gambiense infection ?
-Found in 36 sub-Saharan Africa countries in rural areas where tsetse fly are found and people depend on agriculture, fishing, animal husbandry or hunting.
-Many cases go undiagnosed and unreported.
How do we diagnose T. brucei gambiense infection?
• Diagnosis rests on microscopy used in finding the parasites in body fluid or tissue.
• T. b. rhodesiense parasites can easily be found in blood while T. b. gambiense infection is by microscopic examination of lymph node aspirate, usually from a posterior cervical node.
• Trypanosomes can also be found in lymph node fluid or in fluid or biopsy of a chancre (a painless ulcer).
• Serologic testing is used for screening purposes only and the definitive diagnosis rests on microscopic observation of the parasites.
• Trypanosomes can often be observed in cerebrospinal fluid in persons with second stage infection through lumbar puncture.
Treatment for T. b. gambiense and T. b. rhodesiense infection?
• Pentamidine: T. b. gambiense sleeping sickness. Despite non negligible undesirable effects, it is in general well tolerated by patients.
• Suramin: T. b. rhodesiense. It provokes certain undesirable effects, including urinary tract and allergic reactions.
• Melarsoprol: it is active in both gambiense and rhodesiense infections - Derived from arsenic and has many undesirable side effects, such as encephalopathy which can be fatal (3% to 10%).
• An increase in resistance to the drug has been observed in several foci particularly in central Africa.
• Eflornithine: less toxic than melarsoprol, registered in 1990. It is only effective against T.b. gambiense. The regimen is complex and difficult to apply. '
• A combination treatment of nifurtimox and eflornithine was introduced in 2009
What is the economic impact of these infections?
• Impact on the development of agriculture in Africa. • Those affecting cattle are undoubtedly the most important economically since they are a major cause for reduced meat and milk production and draught power for agricultural production.
What is Schistosomiasis and what causes it?
• Helminthes worms called Schistosomes are causative organisms for the disease.
• Also known as bilharzia or "snail fever", is a parasitic disease carried by freshwater snails.
• The freshwater snails (e.g., Oncomelania hupensis) act as the intermediate host.
Epidemiology of Schistosomiasis ?
Prevalent in tropical and sub tropical areas. Poor communities without access to safe drinking water and adequate sanitation are more affected
How does SHISTOSOMES occur?
-Defecation or urination into freshwater sources deposit parasite eggs which hatch in water.
-Infection occurs when larval forms of the parasite (cercaria) penetrate the skin during contact with infested water.
What is the life cylcle of SHISTOSOMES ?
• Larvae develop into adult schistosomes in the body and live in the blood vessels where the females release eggs.
• Eggs are passed out of the body in the faeces or urine to continue the parasite's life cycle.
• Others become trapped in body tissues, causing immune reactions and progressive damage to organs.
What are the symptoms of Schistosomiasis?
• No initial symptoms when first infected.
• A rash or itchy skin may develop within days after infected.
• About 1-2 months of infection, symptoms including fever, chills, cough, and muscle aches may develop.
• Urinary Schistosomiasis - Haematouria (blood in urine). Chronic infection can also lead to increased risk of bladder cancer.
• Intestinal Schistosomiasis - Gastrointestinal bleeding. Abdominal pain and enlarged liver in complications.
• Rarely, eggs are found in the brain or spinal cord and can cause seizures, paralysis, or spinal cord inflammation
Diagnosis of Schistosomiasis?
• Through detection of parasite eggs in stool or urine specimens by microscopy.
• Antibodies and/or antigens detected in blood or urine samples are also indications of infection.
• Filtration technique using nylon, paper or polycarbonate filters is the standard diagnostic technique for urogenital Schistosomiasis.
• Detection of microscopic blood in urine by chemical reagent strips.
• Eggs of intestinal Schistosomiasis can be detected in faecal specimens using the Kato-Katz technique; using methylene blue-stained cellophane soaked in glycerine or glass slides.
Tutorial : for parasites
• To be able to summarise the life cycles, clinical features & management of the following parasitic infections:
• Plasmodia (malaria)
• Leishmania
• Giardia
• Taenia
• To be able to briefly discuss individual characteristics of other parasitic infections
Life cycle of a parasite
example used Giardia duodenalis
• Infects both the duodenum & the small intestine
• Ingested cysts release trophozoites that adhere to intestinal mucosa by a ventral sucking disc
• Trophozoites divide by binary fission
• Causes local damage & heavy infection may lead to malabsorption
• Infection is by water or food or person-to-person (faecal-oral)
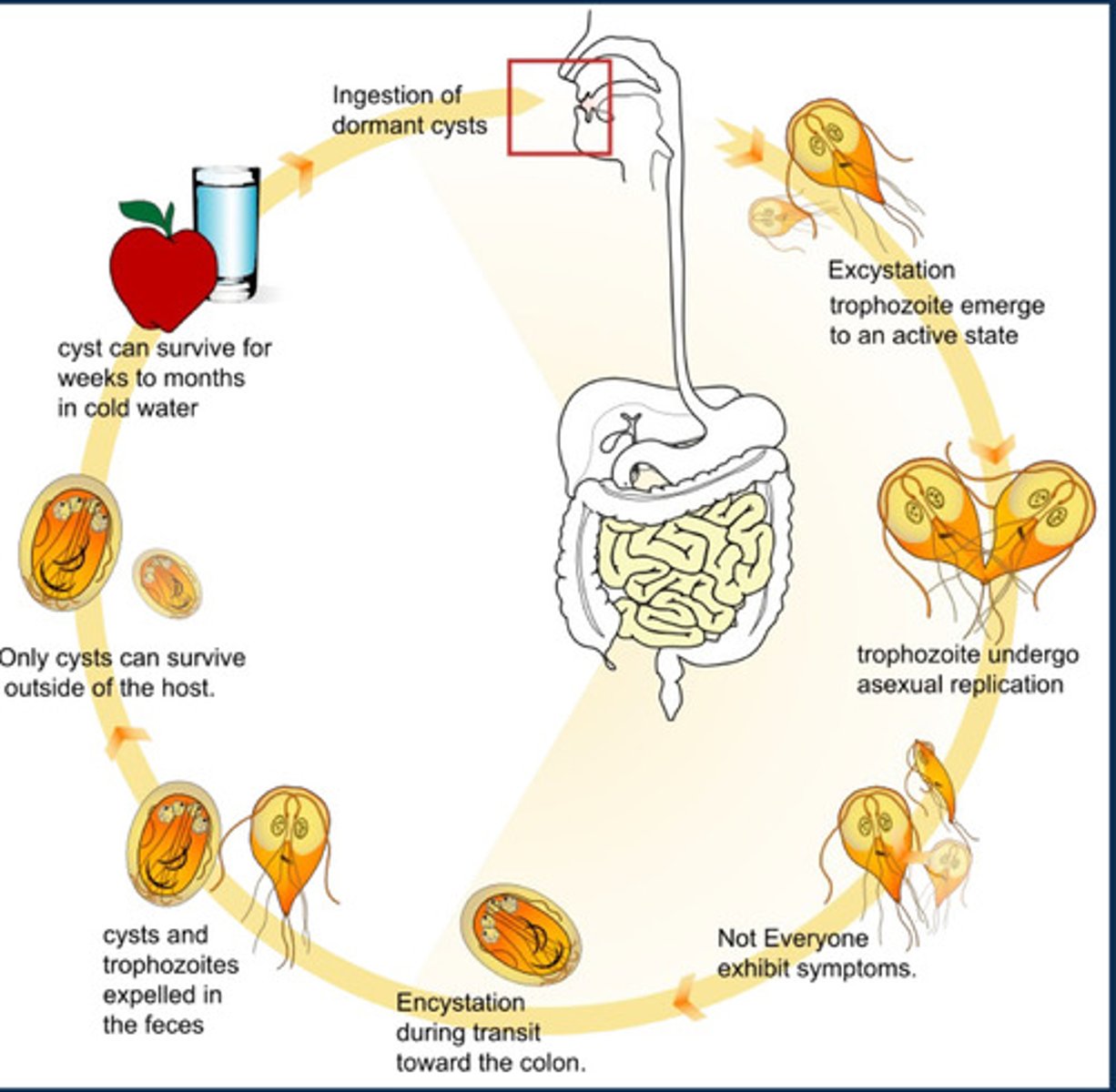
Clinically how can we identify parasitic infection e.g. in Giardia duodenalis and treat
-May be asymptomatic but can produce profuse watery diarrhoea
Diagnosis :
stool microscopy
Treatment: tinidazole (Alternatives include metronidazole)
-Control is essential to prevent re-infection – hand hygiene & good sanitation (Counselling)
What is Leishmania an outline its life cycle, also how is it transmitted?
-Intracellular parasite for humans, transmitted by sandfly bites
Life cycle: Two forms
• Amastigote (intracellular parasites, stage in the parasites, life cycle found in mammalian host) – round, replicates by binary fission, has nucleus, but no flagellum
• Promastigote (found in insect host, sandflies) – elongated, flagellated
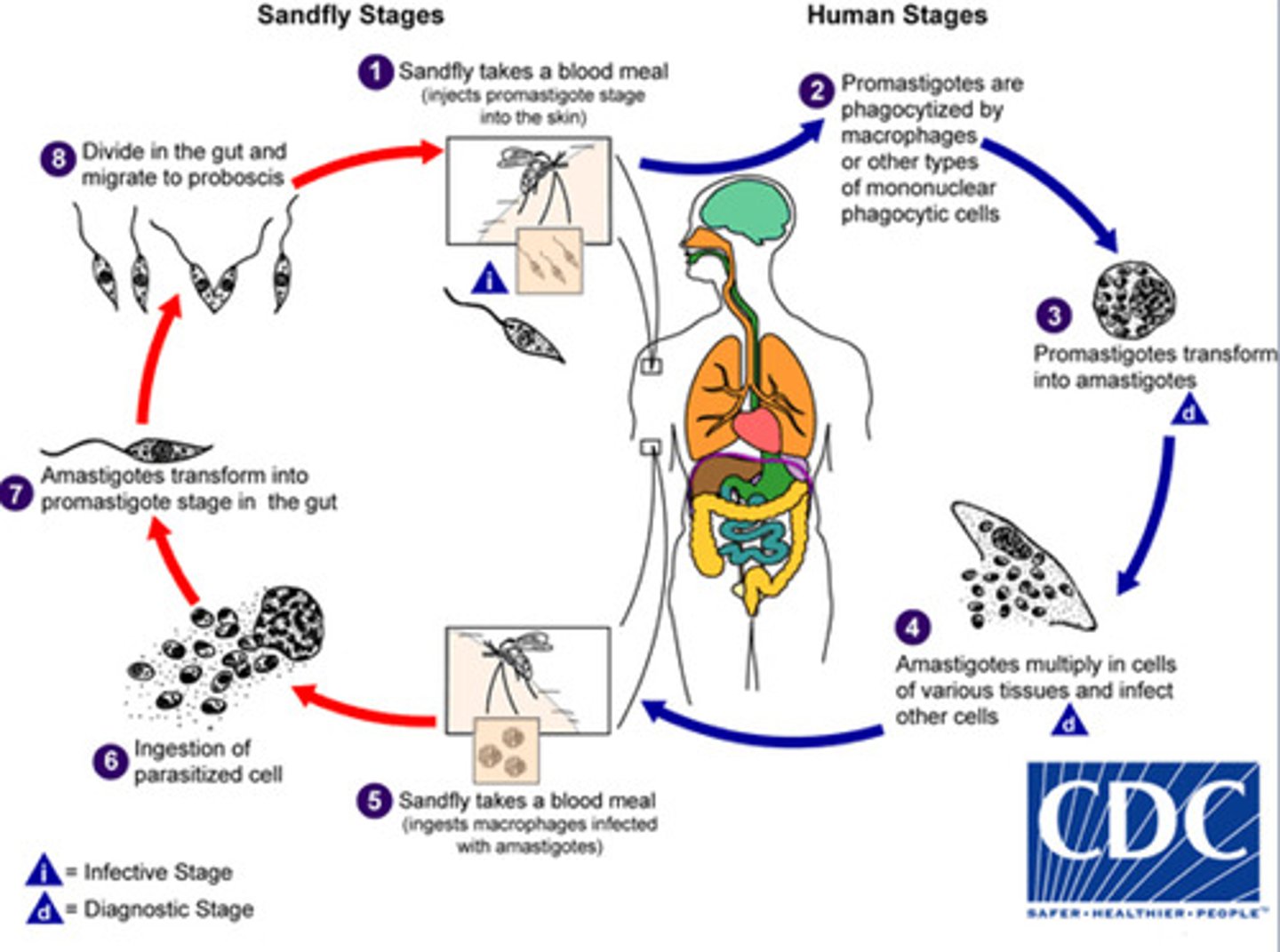
How can we identify and treat leishmania clinically
-Local destruction occurs with invasion of macrophages
-• Infection can be mucocutaneous or visceral:
• In visceral disease - infection disseminates to spleen, liver & lymphoid
• In mucocutaneous disease – infection invades mucosa
-Activation of T-cells & CMI are important in host response
Diagnosis: microscopy & staining of tissue samples
Note: symptoms
• Disseminated disease produces fever, anaemia & weight loss
• Mucocutaneous disease produce granulomas & sores
Treatment:
Mild - Antimony-based compounds - sodium stibogluconate or meglumine
Severe - Liposomal amphotericin Or, less commonly & if treatment failure – fluconazole or miltefosine
-For visceral disease - Liposomal amphotericin
why microscopy to diagnose parasitic infection over pcr
While PCR is generally more sensitive and specific for detecting parasitic infections, microscopy remains a widely used diagnostic method for several reasons:
Cost-effective & accessible: Microscopy is cheaper and widely available; PCR needs expensive equipment and trained personnel.
Faster results: Microscopy provides diagnosis within hours; PCR takes longer, delaying treatment decisions.
Parasite load detection: Microscopy quantifies parasitemia; PCR may not provide immediate parasitemia levels.
Species identification: Experienced microscopists can identify parasites; PCR is more precise but requires advanced tools.
Widely used: Microscopy is the standard for stool screening; PCR is less common due to cost and resource needs.
Better for endemic areas: Microscopy detects multiple parasites in one sample; PCR is more specific but less practical in high-infection regions.
Limited by resources: PCR is slow and requires specialized equipment, making microscopy more practical in routine healthcare settings.
What is plasmodium what what are the four species that infect humans
They are Sporozoan protozoan parasites of humans & animals
-cause Malaria
• Four species infect humans:
• P. falciparum – causes malignant malaria • Most severe type
• P. vivax – benign malaria • Most widely seen form
• P. malariae – “quartan” malaria
• P. ovale – “tertian” malaria
What us plasmodiums life cycle?
-Transmitted by female Anopheles mosquito
-Sexual cycle in mosquito
-Two asexual phases in human:
- Initially liver (pre-erythrocytic) & then in blood (erythrocytic)
-Blood phase consists of different forms
-Fever occurs when merozoites are released from infected RBC
-Interval between fever depends on time for plasmodia asexual cycle
How do we diagnose and identify parasitic infection of plasmodia ?
Diagnosis: by looking at blood. Thick films or thin films & then stains (Films show parasites in various forms - each species has specific morphology)
-Acute malaria (caused by P. falciparum) is a medical emergency
Symptoms: Fever (patient shivers & cold, then hot & dry, then sweats), headache, prostration & serious complications, Headache & myalgia, Red cell destruction - anaemia & splenomegaly; red cell sludging & cytokine release (can lead to Cerebral malaria with convulsions & coma and/or Nephrotic syndrome due to haematuria & renal failure - Black Water fever)
Plasmodia - treatment & prophylaxis
Severe malaria:
• Impaired consciousness/coma, low Hb, AKI, shock or parasite count >5%
• IV artesunate (alternative is IV quinine)
• Treat with IV until parasite count is <1% & patient can take oral therapy
• Switch to artemether/lumefantrine
Non severe:
either artemether/lumefantrine or atovaquone/proguanil – both oral
For P. malariae, vivax or ovale:
-Chloroquine is first-line for all
-Note: (Ovale also needs primaquine - treats dormant forms in the liver)
briefly discuss individual characteristics : Trypanosoma
Morphology: Elongated unicellular protozoa with nucleus, kinetoplast, and single flagellum forming an undulating membrane.
Life cycle: Alternates between insect vectors and vertebrate hosts. Two transmission modes: salivarian (e.g., T. brucei) and stercorarian (e.g., T. cruzi).
Immune evasion: Uses antigenic variation of surface glycoproteins (VSGs) to evade host immune responses.
Pathogenicity: Causes diseases like African trypanosomiasis (sleeping sickness) and Chagas disease.
Adaptations: Flagellum aids in motility and host invasion. Morphological changes (trypomastigote, epimastigote, amastigote forms) allow survival in diverse host environments.

briefly discuss individual characteristics : Amoebozoa
briefly discuss individual characteristics :Entamoeba histolytica
briefly discuss individual characteristics :Apicomplexa
briefly discuss individual characteristics : Toxoplasma gondii