Introduction to Oncology - Lecture 19
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
LOs:
1) identify cancer risk factors
2) discuss screening recommendations for specific cancers
3) define terminology used in oncology and chemo
4) define the components and severity for TNM cancer staging
5) explain MOA, indication, and AEs for the meds and therapy categories
6) explain processes that occur during each phase of the cell cycle
7) state equation for body surface area
what is cancer
uncontrolled cell growth, leading to local tissue invasion and eventual metastases to distant locations
risk factors for cancer
-diet
-smoking
-acohol
-weight
-environmental expsure
-age
-biological sex
-genetics
-family hx
what types of cancer can tobacco increase the incidence of?
All cancers. Most notably:
-lung
-renal
-pancreatic
-head and neck
-testicular
How does tobacco increase cancer risk?
-DNA damage
-chronic, low grade inflammation
-accumulation of toxins
-immunosuppression
what types of cancer does alcohol increase the risk of?
Most cancers. Notably:
-breast
-colorectal
-liver
-head and neck
-stomach
how does alcohol increase the risk for cancer?
-acetaldehyde is a carcinogen
-oxidative stress
-increased estrogen levels
name some environmental exposures that can increase cancer risk
-radon
-herbicides
-pesticides
-asbestos
-mustard gas
________ is the single largest source of radiation for almost everyone in WA state
radon
what viruses may cause cancer?
-HPV
-EBV
what types of cancers can HPV cause?
-cervical
-vaginal
-anal
-penile
-oropharyngeal
7 common warning signs of cancer
-change in bowel or bladder habits
-sore throat that does not heal
-unusual bleeding or discharge
-thickening or lump in breast or elsewhere
-indigestion or trouble swallowing
-changes in wart or mole
-nagging cough or hoarseness
best way to reduce cancer incidence or to catch it in early stages
routine screening
explain the recommended cancer screenings, stratified by age
25-39
-cervical cancer screening (25 - 50+)
40-49
-breast
-cervical
-colorectal
-prostate (at 45 yo for AAs)
50+
-breast
-cervical
-colorectal
-prostate
-lung (if smoking hx)
what test is done for breast cancer screening?
What age is it performed at?
How often is it performed?
-mammogram
-40 - 55+ years old
-annually is optional from 40-44
-annually for 45-54
-q2 years for 55+ as long as life expectancy is > 10 years
what is the discrepancy in breast cancer screening?
ACA suggest mammograms start at age 45, but NCCN recommends to start at 40 years old
Don't need to know the above, just know that screening CAN begin at 40, but ABSOLUTELY should begin at 45
what tests are done for colon and rectal cancer?
At what age are they typically performed?
How often are they performed?
age for all is the same:
-40-85 years old
procedures:
-fecal occult blood test (FOBT) yearly
OR
-flexible sigmoidoscopy q 5 years
OR
-colonoscopy q 10 years
what tests are done for prostate cancer?
At what age is this test typically performed?
How often?
Age
≥ 50 years old (optional)
procedure:
Prostate Specific Antigen
frequency:
q1-2 years
-patients may decide to not be screened initially or for follow up, and should be decided with a physician
what test is done for cervical cancer?
At what age does it typically occur?
How often?
test:
Pap
age and frequency:
-21-29 q3 years
-30-65 q 5 years (w/ HPV screening)
-> 65 not tested unless high risk
what test is done for lung cancer?
What age does it typically occur?
How often?
test:
CT
age:
55-74
frequency:
-yearly if meet ALL of:
a) in good health
b) 30 year pack hx
c) still smoke or quit in last 1.5 years
how does cancer metastasize?
-Cancer cells invade blood and lymph, and angiogenesis occurs
-cancer cells attach to vascular endothelium and proliferate at secondary site
what are the letters used in the TNM naming system of cancers, and what do each letter mean?
-T = Tumor
N = Lumph node
M = metastasis
What are the different subclasses of T, N, and M, and what do they mean?
T = Tumor:
T0 - T4
-higher number = larger tumor
N = Lymph node
N0 - N3
-Higher number = more node involvement
M = Metasteses
-M0 = not metastasized
-M1 = Metastasized
Limitation of TNM system
only works for solid tumors. Hematological cancers do not fit this system
what are the different stages of cancer in numerical staging, and what does each one mean?
Stage 0
-carcinoma in situ ("pre cancer")
stage 1
-localized tumor; evidence of growth. Definitely cancer
stage 2
-local spread but still confided to original site
stage 3
-regional spread to nearby organs and/or lymph nodes
stage 4
-distant metastasis
what is neoadjuvant tx
Treatment given before primary tx (surgery) to help shrink tumor:
-chemo or radiation
-AKA induction therapy
what is adjuvant treatment?
Tx given after primary tx (surgery):
-chemo
-sometimes radiation
Main tx options for cancer
-surgery
-radiation
-systemic therapy (chemo, targeted therapy, immunotherapy, alternative medicine)
goal of surgery for cancer
removal of tumor and adjacent lymph nodes
how does radiation therapy treat cancer
damages the tumor (and surrounding tissues)
AEs of radiation therapy
damage to healthy tissue and can cause cancer toxicities in the future
which cancer tx modality tends to be "safest" to the healthy tissues?
systemic therapy treatments (eg/ chemo)
factors that determine effectiveness of a chemotherapy
-heterogeneity
-drug resistance
-pharmacogenomics
-mutations
AEs of chemotherapy
-neutropenia
-anemia
-alopecia
-mucositis
-N/V
-many more
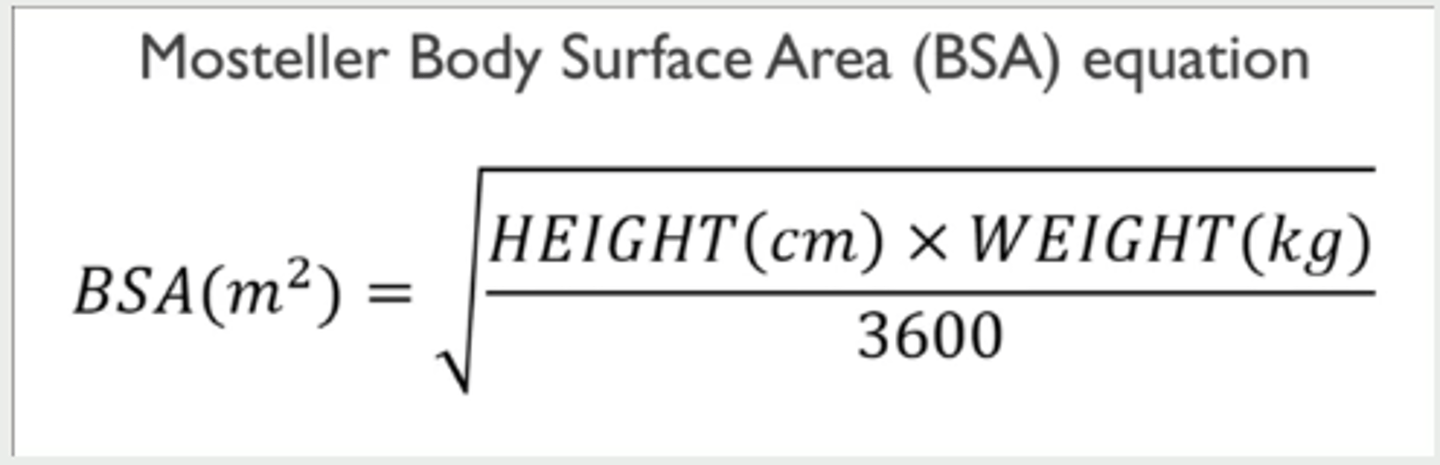
what are the dosing methods used in oncology
-flat dosing
-body surface area
Body surface area equation
How selective are chemotherapy agents
not selective, and treat a wide variety of cancers
significant AE of chemotherapy agents to know
extravascation
what is extravascation
leaking of medication from the vessel, causing blistering, sloughing, and/or necrosis
what to do if extravascation occurs
-stop infusion
-leave needle in for IV access for flushes and antidotes
cisplatin class
alkylating agent
How to treat extravascation from cisplatin
-cold compress 15-20 min q8h x 3d
-sodium thiosulfate
vinblastine class
vinca alkaloid
how to treat extravascation from vinblasine
-Hot compress 15-20 minutes QID x 1-2 d
-hyaluronidase
vinorelbine class
vinca alkaloid
how to treat extravascation from vinorelbine
-Hot compress 15-20 min QID x 1-2 days
-hyaluronidase
Summarize the class and tx of extravascation for:
-cisplatin
-vinblastine
-vinorelbine
cisplatin:
-alkylating agent
-Cold compress 15-20 min q8h x 3 days or sodium thiosulfate
vinblastine:
-vinca alkaloid
-Hot compress 15-20 min QID x 1-2d or hyaluronidase
vinorelbine:
-alkylating agent
-Hot compress 15-20 min QID x 1-2 days or hyaluronidase
what types of medications fall into the class of "targeted therapies" for cancer tx?
-mAbs
-endocrine/hormone therapy
-small molecules
Tamoxifen drug class and MOA
SERM
-blocks estrogen receptor
indications for tamoxifen
-breast cancer
-endometrial cancer
letrozole (Femara) drug class
aromatase inhibitor
-inhibits conversion of androgens to estrogens
in whom do aromatase inhibitors work best?
Post menopausal women, because ovaries are not producing estrogen
indications for letrozole (femara)
breast cancer
Leuprolid (Pupron) drug class and MOA
Gonadotropin Releasing Hormone Agonist (GnRH agonist)
-inhibits gonadotropin secretion
indications for Leuprolide (Lupron)
-prostate cancer
-breast cancer
AEs of the endocrine/hormone cancer therapies (tamoxifen, letrazole, leuprolide)
-hot flashes
-muscle and joint pain
-hypercholesterolemia
which agents are mAbs for cancer?
-rituximab
-trastuzumab
-cetuximab
-bevacizumab
MOA of rituximab (rituxan)
Binds to B-lymphocyte CD20, causing B-cell death
-cytotoxic effects, cell structure effects, apoptosis, and makes cancer more susceptible to other therapies
MOA of Trastuzumab (herceptin)
-monoclonal Ab against HER-2
MOA of cetuximab (erbitux)
EGFR antagonist (Epidermal Growth Factor Receptor Antagonist)
-induces apoptosis and inhibits EGFR production
MOA of bevacizumab
VEGF (vascular endothelial growth factor) inhibitor
-prevents endothelial cells and blood vessels, allowing immune system to kill the cancer
common AEs of mAbs for cancer
infusion rxn:
-flushing
-itching
-SOB
can lead to hospitalization or death
how to attenuate infusion rxn from mAbs used in cancer
pretreat w/ APAP or diphenhydramine
what should be done if an infusion rxn occurs from a mAb?
-stop infusion
-treat reaction
-do not resume until pt is back at baseline
-resume at slower rate and titrate as tolerated
what is a tyrosine kinase
transmembrane receptor that requires extracellular ligand binding, as well as phosphorylation of intracellular binding sites for activation
How do tyrosine kinase inhibitors work for cancer treatment?
inhibit downstream signaling in cell to prevent proliferation or induce apoptosis
which agents are Tyrosine Kinase inhibitors for cancer
-imatinib (gleevec)
-crizotinib (xalkori)
-erlotinib (tarceva)
Imatinib target
BCR-ABL of philadelphia chromosome
target of crizotinib (xalkori)
ALK
target of erlotinib (tarceva)
EGFR
AEs of the TKIs used for cancer
-anemia
-neutropenia
-rash
-edema
-N/V/D
which agents are "immunotherapy" for cancer?
-pembrolizumab (keytruda)
-axicabtagene ciloleucel (Yescarta)
target for pebrolizumab (keytruda)
PD-1
-blocking PD-1 pathway allows activated tumor-specific T cells to kill tumor cells and secrete cytokines to restore anti-tumor immune responses
-essentially "wakes up" the immune system and lets it know a cancer is present
target for axicabtagene ciloleucel (Yescarta)
N/A
how does CAR-T cell therapy work?
T cells are taken from the body and engineered to produce chimeric antigen receptors (CAR)
Reinfused CAR T cells recognize and kill cancer cells
Which medication class is associated with high risk of Acnieform (papulopustular) rash?
EGFR inhibitors
-erlotinib
-cetuximab
A 40 year old male would like to discuss prostate screenings with his primary care provider (PCP). What is the correct age that this patient should start discussing the pros and cons of prostate screenings with his PCP?
50
What is a common side effect of pembrolizumab?
cold sensitivity
What is a common side effect of cisplatin?
a) cardiotoxic
b) N/V
c) hepatotoxic
d) neuropathy
N/V
A patient is diagnosed with cancer that has the following TNM staging: T3 N0 M0. Which of the following is the most accurate description of her tumor?
fairly large, no lymph node involvement, non-metastasized
Which of the following is true regarding adjuvant cancer therapy?
a) Given after primary therapy to prevent recurrence with intent to cure
b) Given before primary therapy to reduce tumor burden/size
c) Given to relieve symptoms but not to cure patient
A
Calculate an ANC for a patient with the following labs:
WBC 1.2 x 103/mL,
Segs 30%,
Bands 10%,
PLT 160,000/mm3,
Hgb 12 gm/dL
480 cells/mL
[WBC x (%Segs + %Bands)] / 100
[1200 x (40)] / 100 = 480
What is the MOA of alectinib?
ALK inhibitor
which agents act against:
-VEGF
-EGFR
-ALK
-BCR ABL
-PD1
VEGF
-bevacizumab
EGFR
-cetuximab
-erlotinib?
ALK
-crizotinib
-alectinib
BCR ABL
-imatinib (gleevec)
PD-1
-pebrolizumab
patient w/ colon cancer has histology testing that reveals malignancy that is EGFR positive. What medication would you recommend as treatment?
cetuximab or erlotinib
what is a common AE for TKIs?
a) polycythemia
b) edema
c) dyspepsia
d) HTN
B) edema