Module 2 tuts p2.2 krebs, gluconeogenesis , ppp
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
45 Terms
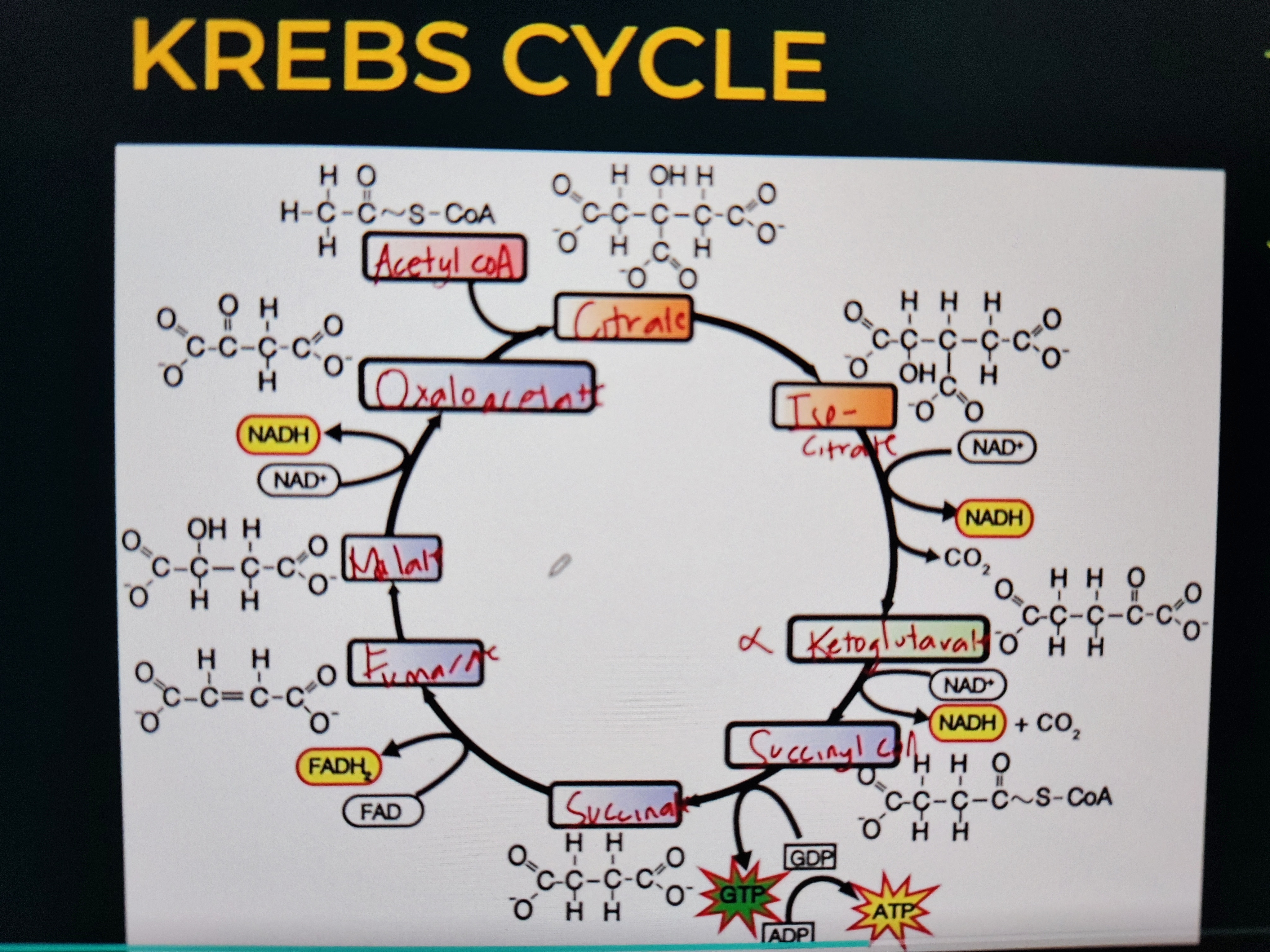
KREBS CYCLE
Aka Citric Acid cycle, TCA - Tricarboxylic Acid cycle
Elucidated by Hans Krebs
Site: Mitochondrial matrix
KREBS CYCLE
1. Acetyl CoA + Oxaloacetate → Citrate
Citrate synthase
Condensation reaction
2. Citrate → Isocitrate
Aconitase
Isomerization
3. Isocitrate → Alpha-ketoglutarate
Isocitrate Dehydrogenase
Oxidative Decarboxylation
4. Alpha-ketoglutarate → Succinyl CoA
α-Ketoglutarate Dehydrogenase
Oxidative Decarboxylation
5. Succinyl CoA → Succinate
Succinate thiokinase; Succinyl-CoA Synthetase
Hydrolysis & Substrate Level Phosphorylation
6. Succinate → Fumarate
Succinate Dehydrogenase
Oxidation Reaction
7. Fumarate → Malate
Fumarase
Hydration Reaction
8. Malate → Oxaloacetate
Malate Dehydrogenase
Oxidation Reaction
KREBS CYCLE: STEP 1
Step 1
Acetyl CoA + Oxaloacetate → Citrate/Citric Acid
Enzyme: Citrate synthase (ligase)
Reaction: Condensation reaction
Explanation: Combines a 2-carbon Acetyl CoA with a 4-carbon Oxaloacetate to form 6-carbon Citrate.
KREBS CYCLE: STEP 2
Step 2
Citrate → Isocitrate
Enzyme: Aconitase (Isomerase)
Reaction: Isomerization
Explanation: Rearranges Citrate into its isomer, Isocitrate, to prepare for oxidation.
KREBS CYCLE: STEP 3
Step 3
Isocitrate → Alpha-ketoglutarate
Enzyme: Isocitrate Dehydrogenase (Oxidoreductases)
Reaction: Oxidative Decarboxylation
Explanation: Isocitrate is oxidized, releasing CO₂ and forming NADH and Alpha-ketoglutarate; from 6C to 5C
KREBS CYCLE: STEP 4
Step 4
α-Ketoglutarate → Succinyl CoA
Enzyme: α-Ketoglutarate Dehydrogenase (Oxidoreductases)
Reaction: Oxidative Decarboxylation
Explanation: Another CO₂ is released, and NADH is generated while forming Succinyl CoA; 5C to 4C
KREBS CYCLE: STEP 5
Step 5
Succinyl CoA → Succinate
Enzyme:
Succinate thiokinase (hydrolase)
Succinate synthase (ligase)
Reaction: Hydrolysis & Substrate Level Phosphorylation
Hydrolysis
Water is added, breaking the high-energy thioester bond between succinyl group and CoA.
This releases Succinate and Coenzyme A (CoA-SH) as two separate molecules.
Substrate Level Phosphorylation
The energy released from breaking the Succinyl-CoA bond is used to directly form GTP from GDP + Pi (inorganic phosphate).
GTP (guanosine triphosphate) is then quickly converted to ATP
KREBS CYCLE: STEP 6
Step 6
Succinate → Fumarate
Enzyme: Succinate Dehydrogenase (Oxidoreductases)
Reaction: Oxidation Reaction
Explanation: Succinate is oxidized to Fumarate while FAD is reduced to FADH₂.
KREBS CYCLE: STEP 7
Step 7
Fumarate → Malate
Enzyme: Fumarase (Lyase)
Reaction: Hydration
Explanation: Water is added across the double bond of fumarate. This breaks the double bond, converting it into a single bond, forming Malate.
Non hydrolytic bond cleavage
KREBS CYCLE: STEP 8
Step 8
Malate → Oxaloacetate
Enzyme: Malate Dehydrogenase (Oxidoreductases)
Reaction: Oxidation Reaction
Explanation: Malate is oxidized - loses 2 electrons (2e⁻) and 1 hydrogen ion (H⁺)
These are accepted by NAD⁺, reducing it to NADH
KREBS CYCLE: PRODUCTS
1 NADH = 2.5 ATP’s
1 FADH₂ = 1.5 ATP’s
1 Acetyl CoA = 3 NADH, 1 ATP, 1 FADH
2 Acetyl CoA’s:
6 NADH × 2.5 = 15
2 FADH₂ × 1.5 = 3
2 ATP’s via SLP = 2
TOTAL: 20 ATP’s
KREBS CYCLE: ENZYMES and REACTION SUMMARY
“Our City Is Kept Safe & Secure From Monsters”
Step 1
Reaction: Acetyl CoA + Oxaloacetate → Citrate
Enzyme: Citrate synthase (Ligase)
Reaction: Condensation reaction
Step 2
Reaction: Citrate → Isocitrate
Enzyme: Aconitase (Isomerase)
Reaction: Isomerization
Step 3
Reaction: Isocitrate → Alpha-ketoglutarate
Enzyme: Isocitrate Dehydrogenase (Oxidoreductases)
Reaction: Oxidative Decarboxylation
1 NADH
Step 4
Reaction: Alpha-ketoglutarate → Succinyl CoA
Enzyme: α-Ketoglutarate Dehydrogenase (Oxidoreductases)
Reaction: Oxidative Decarboxylation
1 NADH
Step 5
Reaction: Succinyl CoA → Succinate
Enzyme: Succinate thiokinase (hydrolase), Succinate synthase (ligase)
Reaction: Hydrolysis & Substrate Level Phosphorylation
1 ATP
Step 6
Reaction: Succinate → Fumarate
Enzyme: Succinate Dehydrogenase (Oxidoreductases)
Reaction: Oxidation Reaction
1 FADH2
Step 7
Reaction: Fumarate → Malate
Enzyme: Fumarase (Lyase)
Reaction: Hydration
Step 8
Reaction: Malate → Oxaloacetate
Enzyme: Malate Dehydrogenase (Oxidoreductases)
Reaction: Oxidation Reaction
1 NADH
KREBS CYCLE: STEP 9
Step 9: Additional in some references for krebs (gluconeogenesis step)
Pyruvate → Oxaloacetate
Enzyme: Pyruvate Carboxylase (Ligase)
Reaction: Carboxylation reaction
Explanation: In gluconeogenesis, pyruvate in the mitochondria is converted to oxaloacetate by adding CO₂.
From 3C pyruvate to 4C oxaloacetate
This step requires biotin as a cofactor and ATP as an energy source.
GLUCONEOGENESIS
Glucose + New + Formation
Formation of new glucose from non-carbohydrate precursors
Happens in starvation and prolonged fasting
GLUCONEOGENESIS
Precursors:
Glycerol from fats
Fats are esters of glycerol and 3 fatty acids
Glucogenic Amino Acids like alanine
Pyruvate or pyruvic acid
Lactate or lactic acid
Ketone bodies
When fats breakdown, ketone bodies are produced
Acetone
Acetoacetic acid
B-hydroxy butyric acid - most abundant
They are used by our brain cells and heart cells for energy (KETOSIS)
Glycogen
A branched glucose polymer (polysaccharide) that serves as the body's short-term energy reserve.
Catabolism
Breaks down complex molecules into simpler ones, releasing energy.
Glycogen to glucose units - glycogenolysis
Anabolism
Uses energy to build complex molecules from simpler ones.
Glucose to glycogen - Glycogenesis
GLYCOGEN METABOLISM
GLYCOGENESIS
GLYCOGENOLYSIS
GLYCOGENESIS
Generation or formation of glycogen from glucose units (anabolism)
Regulated by Insulin
GLYCOGENOLYSIS
Breakdown of glycogen to form glucose units (catabolism)
Formation of glucose from glycogen
Regulated by Glucagon and Epinephrine
HORMONES THAT REGULATE GLYCOGEN METABOLISM
Glucagon - glycogenolysis
Epinephrine - glycogenolysis
Insulin - glycogenesis
True
Insulin responds to excess glucose by signaling for its storage as glycogen in the liver and muscles, lowering blood sugar.
Glucagon and epinephrine counter this by promoting glycogenolysis (glycogen breakdown to glucose) to raise blood glucose levels, with epinephrine also initiating fatty acid release to provide alternative fuel.
PENTOSE PHOSPHATE PATHWAY
AKA Hexose Monophosphate Shunt (HMP)
PENTOSE PHOSPHATE PATHWAY
PRODUCTS:
Hexoses → Pentoses
Glucose is converted to ribose, ribulose, xylulose
For synthesis of nucleic acid - RNA, and DNA
NADPH → reduced form of Nicotinamide Adenine Dinucleotide PHOSPHATE
Keeps glutathione reduced
Important in fatty acid synthesis (CO-ENZYME)
PENTOSES → ribose
Glutathione
Must remain in its reduced form (GSH) to neutralize harmful reactive oxygen species (ROS) and prevent cellular damage.
NADPH from PPP is required to keep glutathione reduced.
Role of G6PD (Glucose-6-Phosphate Dehydrogenase)
Catalyzes the first committed step: Glucose-6-phosphate → 6-Phosphogluconolactone.
Produces NADPH from NADP⁺ during this reaction.
Importance of NADPH
Maintains reduced glutathione for protection against oxidative damage.
Provides reducing power for biosynthetic reactions (e.g., fatty acid synthesis).
G6PD Deficiency
Low NADPH production leads to oxidative damage in red blood cells (RBCs).
Damaged RBCs break down prematurely
Hemolytic anemia, surviving less than 120 days.
G6PD Deficiency
CI to these drugs: THESE ARE OXIDANTS so these might worsen the case of people who have G6PD deficiency
Sulfonamides like Co-Trimoxazole (SULFAMETHOXAZOLE+ TRIMETHOPRIM)
Anti-malarials like Primaquine, Chloroquine
Nitrofurans like Nitrofurantoin
Quinolones like Nalidixic acid
High dose of ASA
Naphthalene or moth balls
Transketolase
Catalyzes transketolation
Co enzyme: TPP - Thiamine Pyrophosphate (Vit B1) ⭐
Thiamine deficiency
No TPP produced → decrease in transketolase activity
True
Remember:
NAD - Vit B3 (Niacin)
FAD - Vit B2 (Riboflavin)
Transketolation - Vit B1 (Thiamine)
CARBOHYDRATE METABOLISM DISORDERS
Ketosis
Diabetes Mellitus Type I
Ketosis
Develops when the body is starved with glucose during prolonged fasting or starvation
Normal, controlled response to low glucose
Blood pH
7.35 to 7.45
Acidosis - Decrease in pH blood
Alkalosis - Increase in pH blood
Diabetic ketoacidosis (DKA)
Common in DM type I
The body overproduces ketone bodies for energy.
Excess ketones lower blood pH, leading to metabolic acidosis.
Fruity-smelling breath (acetone).
Leads to CNS depression if not treated
Diabetes Mellitus Type I
Insulin Dependent Diabetes Mellitus / Juvenile-Onset DM
Beta cells of the pancreas are gone. No insulin is produced.
This condition is controlled by daily injections of insulin
Autoimmune
Insulin
Source: Animal (can cause allergic rxn)
Porcine Insulin - pig
Bovine Insulin - cattle
Humulin
Eli Lilly manufactures _____, the first commercially available biosynthetic human insulin, which was created using recombinant DNA technology in E. coli bacteria ⭐
No allergic rxn
Diabetes Mellitus Type 2
Non-Insulin Diabetes Mellitus / Adult-Onset DM
A normal amount of insulin is produced, either it is not released fast enough when blood sugar rises or the target tissues have a reduced responsiveness
Diabetes Mellitus Type 2
Oral Hypoglycemic Agents
Commonly used in Type 2 DM
Targets insulin resistance
Insulin injection
Only if there's still high blood sugar level after taking OHAs
Diabetes Insipidus
A pituitary disorder that directly affects kidney function; no unusual level of glucose in the urine is observed
Absence of antidiuretic hormone or vasopressin
Can excrete up to 20L/day
Desmopressin
Drug used to manage Diabetes Insipidus