Pain & Psychosocial Adaptation: Chronic Illness and Disability
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
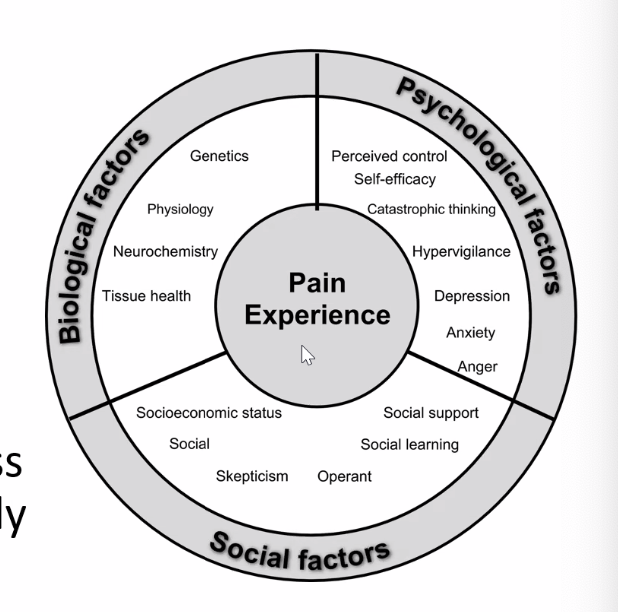
Biopsychosocial Model of Pain
Multidimensional, dynamic interaction among physiological, psychological, and social factors that reciprocally influence each other, resulting in chronic and complex pain syndromes
Sensory and affective experience
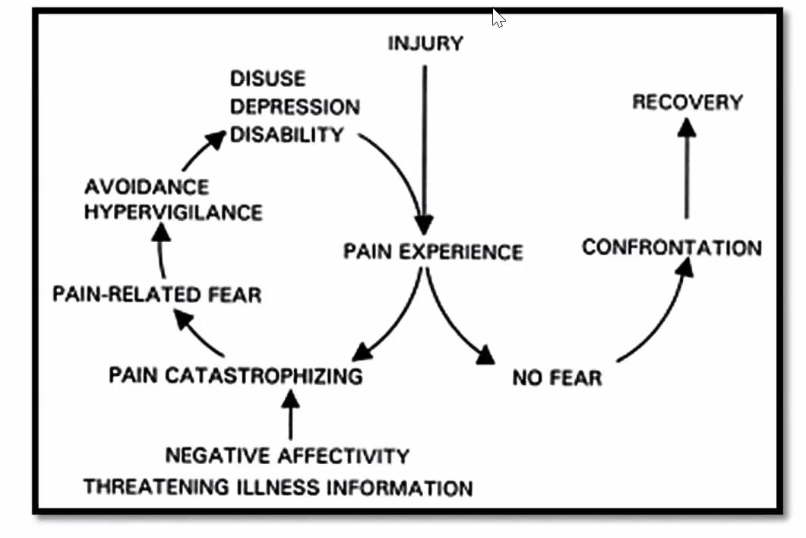
Fear Avoidance Model of Pain
Effect of Psychosocial Constructs and Processes on Pain-Related Outcomes
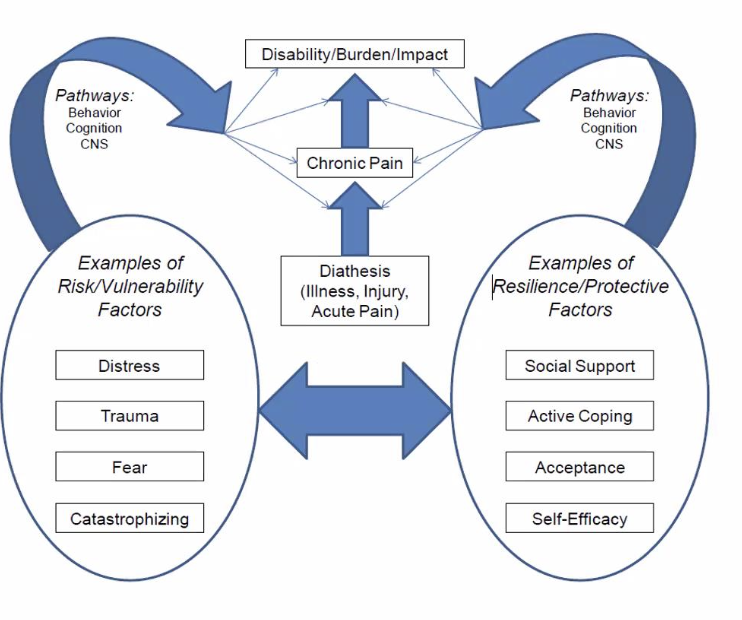
Psychosocial Factors Influencing Pain-Related Outcomes - Contribute to painintensity, long term outcomes such as physical disability, health care cost, mortality and suicide
Depression, anxiety, negative affect
Premorbid psychological dysfunction represents a risk for?
future development of chronic pain conditions
___________ were associated with more post-surgical pain and impairment
Higher presurgical emotional distress
Emotional distress and psychosocial stress have been shown to increase the likelihood of transitioning from ____ to ______
acute to chronic musculoskeletal pain
__________ improves pain intensity through reducing pain catastrophizing
Dispositional optimism
Childhood physical, sexual and psychological abuse are reported to be risk factors for adult development of pain syndromes such as
FM, irritable bowel syndrome, chronic pelvic pain, TMJ disorders
Presence of past trauma was associated with 2-3 fold increase in __________
subsequent development of chronic widespread pain
Reports of child abuse conferred 97% increase in risk for having _______
painful somatic syndrome
______ has been identified as a risk factor for chronic pain, transition from acute to chronic pain and elevated severity of pain and disability in abuse victims
PTSD
In patients with acquired amputation, ________ were less likely to develop persistent phantom limb pain
positive general social support
________ is strongly related to the development of children's persistent pain after a major surgery and is significantly related to the child's disability
Parental catastrophizing
_________________ may provide specific pathways by which parental catastrophizing amplifies a child's pain experience and behavior
Parental attention to pain and solicitousness behavior that encourage children to avoid regular activities
2 Crucial Interpersonal Factors for Psychotherapy Process
Stimulating the patient's expectations that treatment will help
Establishing a sound therapeutic relationship
Active vs Passive Coping
VActive coping - strategies that control pain or function despite pain • Passive coping - relinquishing control of pain to others
comprised of negative cognitive emotional processes such as helplessness, pessimism, rumination about pain and magnification of pain reports
Catastrophizing
refers to an individual's belief that his or her own ability to perform a certain behavior to achieve a desired outcome
Self-Efficacy
_________________ is related to increased feelings of control, use of more active coping strategies and better functional outcomes
Generalized positive outcome expectancy or dispositional optimism
True/False: Both patient and provider expectations for treatment success were strong predictors of respones
True
Medical Model of Disability
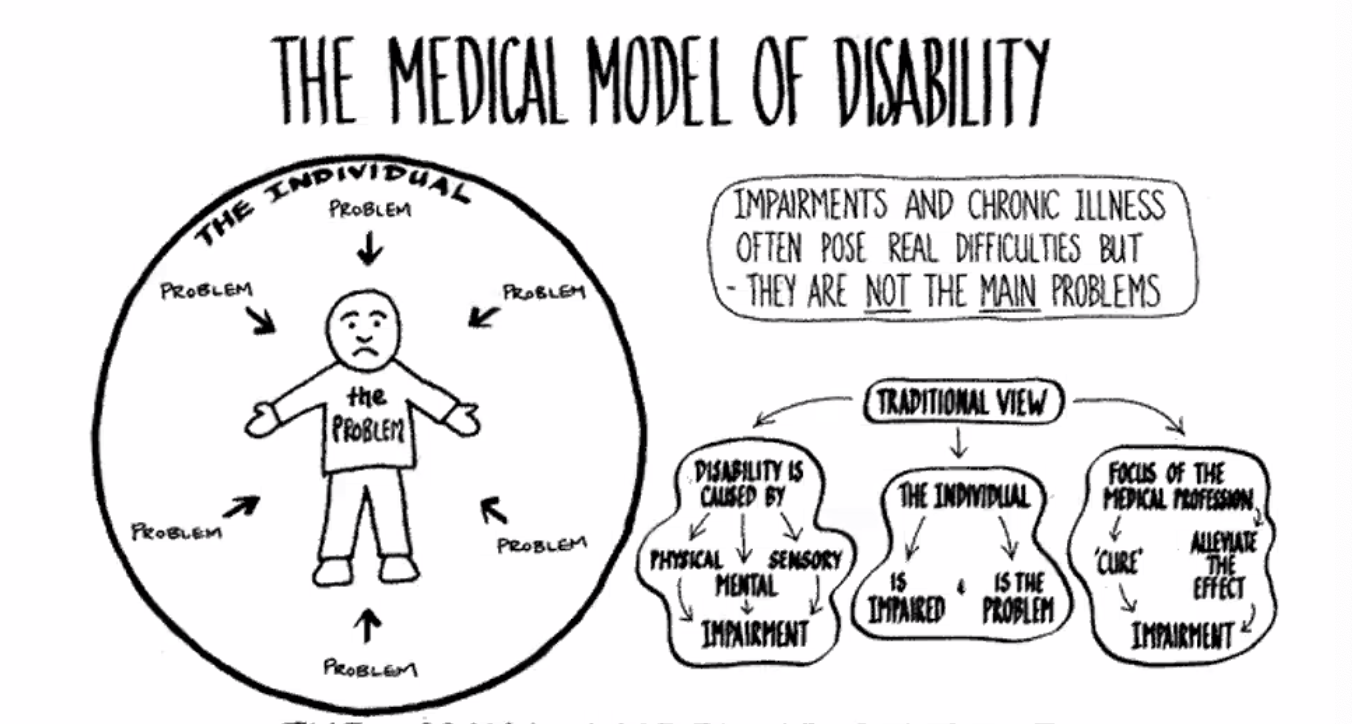
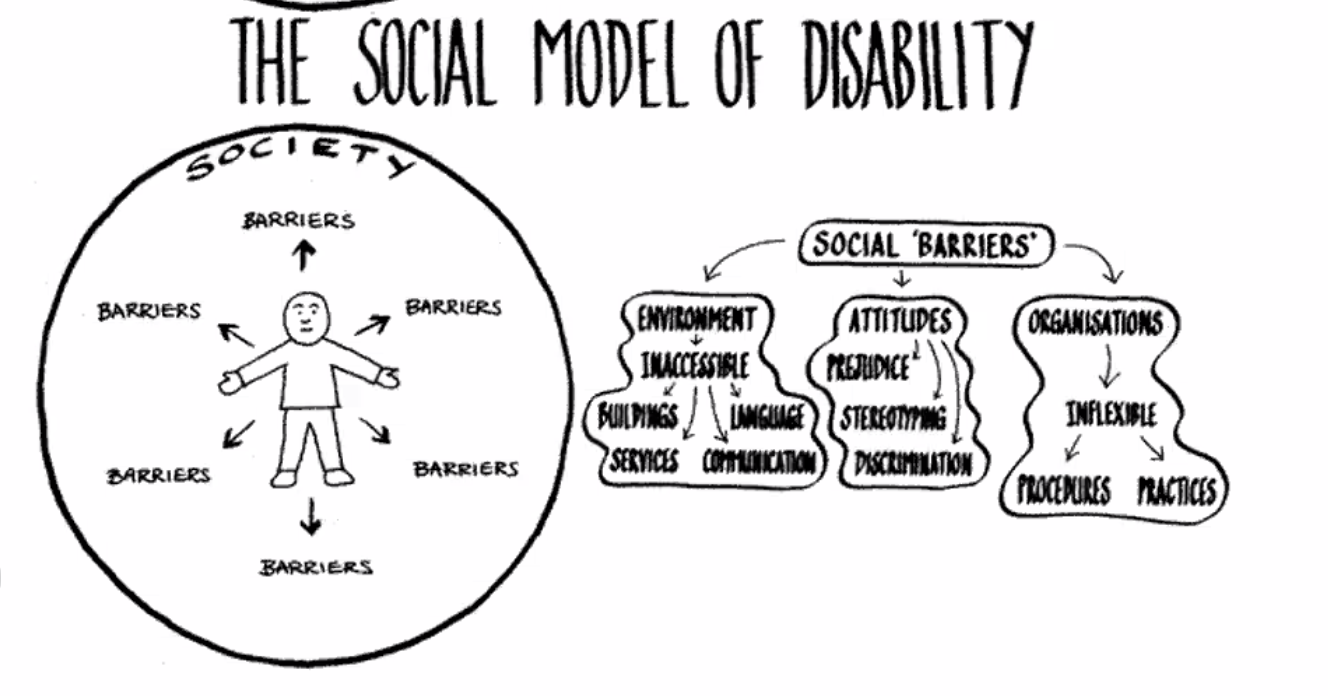
Social Model of Disability
Impairments
Concerned with abnormalities of body structure and appearance and with organ or system function
Any loss or abnormality of psychological, physiological or anatomic structure or function
Disturbance at organ level
Disability
Reflects the consequence of impairment in terms of functional performance and activity
Disturbance at the level of person
Inability to walk and perform ADL
Handicap
Disadvantage which prevents from performing a role
Reflect interaction with and adaptation to the individual's surroundings
Societal level
Immobility, dependence
Some persons with disability die up to ___ years earlier than those without disabilities
20
Persons with disabilities have twice the risk of developing conditions such as?
depression, asthma, diabetes, stroke, obesity or poor oral health
Statistics on Chronic Illness and Disability
• Approximately 54M Americans (1 in 5) have physical, sensory, psychiatric or cognitive disabilities that interfere with daily living
• > 9M Americans with disabilities are unable to work or attend school
• Costs of annual income support and medical care provided by US government is about $60B
• Disabilities are higher among older people, minorities and lower socioeconomic groups
• 8 of the 10 most common causes of death in US are associated with chronic illness
Factor that Create a Profound Effect on the Life of the Individuals with Chronic Illness and Disability
Degree of functional limitations
Interference with ability to perform daily activities and life roles
Uncertain prognosis
Prolonged course of medical treatment and rehabilitation
Psychosocial stress associated with the incurred trauma or disease process itself
Impact on family and friends
Sustained financial losses
Dynamics to the Psychosocial Adaptation to CID - Stress
Increased frequency and severity of stressful situations • Need to cope with daily threats
One's life and well being
Body integrity
Independence and autonomy
Fulfillment of familial, social and vocational roles • Future goals and plans
Economic stability
Dynamics to the Psychosocial Adaptation to CID - Crisis
Sudden onset, life-threatening, loss of valued functions
Although crisis is time limited, during its presence life is affected by disturbed psychological, behavioral and social equilibrium
Its consequences are long lasting and may evolve into pathological disorders
Dynamics to the Psychosocial Adaptation to CID - Loss and grief
Triggers a mourning process for the lost body part or function
Constant reminder of the permanency of the condition
Daily triggering events act to remind of the permanent disparity between past and present or future situations
Dynamics to the Psychosocial Adaptation to CID - Mourning
Non-acceptance of the facts
Erupting Emotions
Parting with the former
Finding a new self as well as new perspectives for one’s future
Dynamics to the Psychosocial Adaptation to CID - Body image
Unconscious mental representation or schema of one's own body
Evolves gradually and reflects interactive forces exerted by sensory (visual, auditory, kinesthetic), interpersonal (attitudinal), environmental (physical conditions) and temporal factors
CID alters and distorts own's body image and self-concept
Successful psychosocial adaptation to CID is said to reflect the integration of
physical and sensory changes into a transformed body image and self- perception
Dynamics to the Psychosocial Adaptation to CID - Self - concept
Linked to body image and often seen as conscious, social derivatives of it
Self-identity (sense of self) is privately owned and outwardly presented
May be denied in social interactions with others who respond to the person as disabled first = lost sense of real self
Self-esteem gradually becomes eroded and negative self-perceptions follow
Dynamics to the Psychosocial Adaptation to CID - Stigma
Negative set of beliefs about people with specific characteristics
Increased life stress, reduced self-esteem and withdrawal from social encounters, including treatment and rehabilitation
Structural Stigma
Public Stigma
Self-Stigma
Stigma - Social avoidance
left out of social activities, circle may be more distant, people hesitant to make eye contact or start conversation
Stigma - Stereotyping
presumed helpless, unable to care for self, unable to make decisions
Stigma - Discrimination
Jobs, housing, opportunities
Stigma - Condescension
coddles or over-protected due to perceptions of helplessness
Stigma - Blaming
Accused of using disability for unfair gains
Stigma - Internalization
Person himself feel ashamed or embarassed
How Disability Stigma Affect Your Relationship with Patients? - Concealment
Reluctant to use assistive device or disclose their diagnosis
How Disability Stigma Affect Your Relationship with Patients? - Disability Pride
Some express pride and positive identity to counteract stigma
Join groups with same disability
May opt against medical treatment because they have developed an identity around the disability
How Disability Stigma Affect Your Relationship with Patients? - Social Integration
Choose t o make a disability more evident to improve their options for social participation (using a wheelchair instead of walker to travel with family without fatigue)
How Disability Stigma Affect Your Relationship with Patients? - Need for Respect
Build a collaborative partnership with patient built on trust and respect communicates your support for the patient as a whole person
Dynamics to the Psychosocial Adaptation to CID - Uncertainty and Unpredictability
Stable or predictable - amputation, cerebral palsy
Unstable and unpredictable - epilepsy, cancer, DM, MS
Exacerbation and remissions
Unpredictable complications
Experiences of pain and loss of consciousness • Alternating pace of gradual deterioration
Dynamics to the Psychosocial Adaptation to CID - Perceived uncertainty in illness
uncertainty, or inability to structure personal meaning, results if the individual is unable to form a cognitive schema of illness-associated events
Dynamics to the Psychosocial Adaptation to CID - Quality of Life Domains
Intrapersonal (health, perceptions of life satisfaction, feelings of well being)
Interpersonal (family life, social activities)
Extrapersonal (work activities, housing, schooling or learning and recreational)
QOL is linked to a more positive ____________
positive self-concept and body image, increased sense of control over CID
QOL is negatively associated with?
perceived stress and feelings of loss and grief
CID Triggered Responses - early
Shock
Anxiety
Denial
CID Triggered Responses - Intermediate
Depression
Anger / hostility
CID Triggered Responses - late reactions
adjustments (reintegration, acceptance)
CID Triggered Responses - Shock
Short-lived reaction
Marks the initial experience following the onset of a traumatic or sudden injury or diagnosis of a life threatening or chronic and debilitating disease
"psychic numbness"
Psychic Numbness
Cognitive disorganization and dramatically decreased or disrupted mobility and speech
CID Triggered Responses - Anxiety
Characterized by panic-like feature on initial sensing of the nature and magnitude of the traumatic event
Confused thinking, cognitive flooding, multitude of physiological symptoms including rapid heart rates, hyperventilation, excess perspiration and irritable stomach
CID Triggered Responses - Denial
Defense mechanism mobilized to ward of anxiety and other threatening emotions
Involves minimization and even complete negation of the chronicity, extent and future implications associated with the condition
Involves selective attention to one's physical and psychological environments
Wishful thinking, unrealistic expectations of recovery, or blatant neglect of medical advice and recommendations
CID Triggered Responses - Depression
Reflect the realization of the permanency, magnitude and future implications associated with loss of body integrity, chronicity of condition, or impending death
Feelings of despair, helplessness, hopelessness, isolation and distress
CID Triggered Responses - Anger / Hostility
Aggressive acts, abusive accusations, antagonism, passive-aggressive modes of obstructing treatment
Internalized Anger
Self-attributions of responsibility for the condition onset of failure to achieve successful outcomes
Externalized Hostility
Blame others for CID onset or unsuccessful treatment efforts or aspects of the external environment
CID Triggered Responses - Adjustment
Reorganization, reintegration or reorientation
CID Triggered Responses - Adjustment Components
Earlier cognitive reconciliation of the condition, its impact, and its chronic or permanent nature
An affective acceptance, or internalization, of oneself as a person with CID, including a new or restored sense of self concept, renewed life values and a continued search for new meanings
An active pursuit of personal, social, and/or vocational goals
CID Associated Coping Strategies - Coping
Psychological strategy mobilized to decrease, modify or diffuse the impact of stress-generating life events
Disengagement coping strategies, Engagement coping strategies
CID Associated Coping Strategies - Disengagement coping strategies
Seek to deal with stressful events through passive, indirect, even avoidance- oriented activities
Denial, wish-fulfilling fantasy, self and other blame, resorting to substance abuse
Associated with higher levels of psychological distress difficulties in accepting one's condition and poor adaptation
CID Associated Coping Strategies - Engagement coping strategies
Efforts that defuse stressful situations through active, direct and goal-oriented activities such as information seeking, problem solving, planning and seeking social support
Linked to higher levels of well-being, acceptance of condition and successful adaptation
Psychosocial Reaction-Specific Interventions - Earlier Phases
Supportive, affective-insightful or psychodynamic in nature are more useful in earlier phases of adaptation
Encouraging to vent feelings associated with guilt, shame,, mourning for loss of function
Reinforcing social contacts and activities
Practicing self-assertiveness, self-determination and independent living skills
Psychosocial Reaction-Specific Interventions - Later Phases
Active-directive, goal-oriented or cognitive-behavioral in nature may be more beneficial during the later stages
Practicing anger expression in socially sanctioned forms
Behavior modification techniques to reduce physically and verbally aggressive acts
Global Clinical Interventions
Provide patient and family with emotional, cognitive and behavioral support
Equip the patient with adaptive coping skills that could be successfully adopted when facing stressful situations
Global Clinical Intervention - Examples
Assisting clients to explore the personal meaning of the CID
Vent feelings leading to acceptance of condition permanency, altered body image and realization of decreased functional capacity
Providing clients with relevant medical information
Providing clients with supportive family and group experiences
Teaching clients adaptive coping skills for successful community functioning
Assertiveness, interpersonal relations, decision making, problem solving, stigma management and time management skills
QOL - Rehabilitation
Attainment of person-environment congruence, where the person with CID is said to demonstrate better psychosocial adaptation
Establishing Respectful Communication
speak directly to your patient. Make eye contact
use ordinary language. "see you later" to a blind or "lets walk to the park" to nonambulatory
Ask patients with speech impairments how they prefer to communicate
bawal:
interrupt or rush a patient who communicates slowly
guess what a patient is trying to say
Respecting Patient Privacy and Autonomy
provide written materials
ensure your office and toilets are accessible and they can navigate the space independently
office practice is accessible (layout, procedures)
ask a patient the best way to provide physical assistance fi it is needed
bawal: touch, pull or grab patient's body without asking for consent, handle patient's mobility device without consent
Resect Disability Identity and Culture
respect a patient's choice to downplay or highlight their disability in particular settings
Introduce your patient to support groups
Bawal:
use negative words to describe disability (tragedy, suffering, confined to wheelchair)
"golden rule thinking" - imagining how you would personally feel with a disability as a way to infer how your patients feel