Lower Digestive System
1/40
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
41 Terms
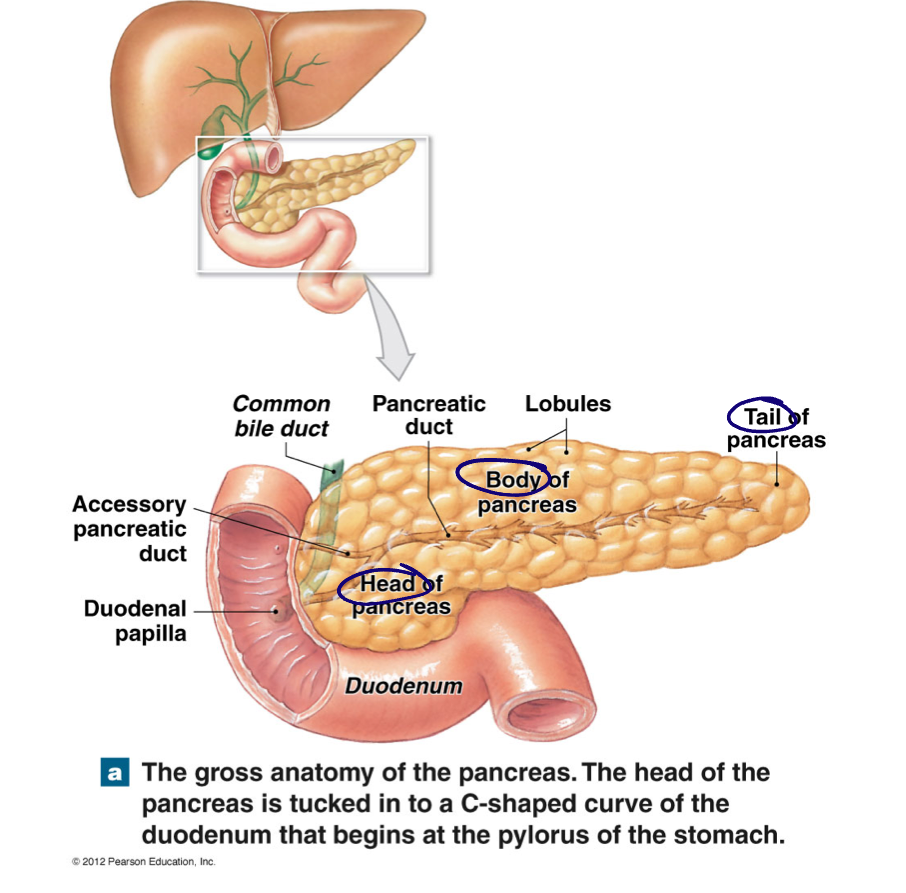
Pancreas → anatomy and function
Retroperitoneal
Head, body, and tail
Endocrine and exocrine function
Endocrine: release of insulin, glucagon, and somatostatin into blood stream
Exocrine: release of pancreatic juice (alkaline mixture - digestive enzymes, waters, buffers, ions) into duodenum via pancreatic duct
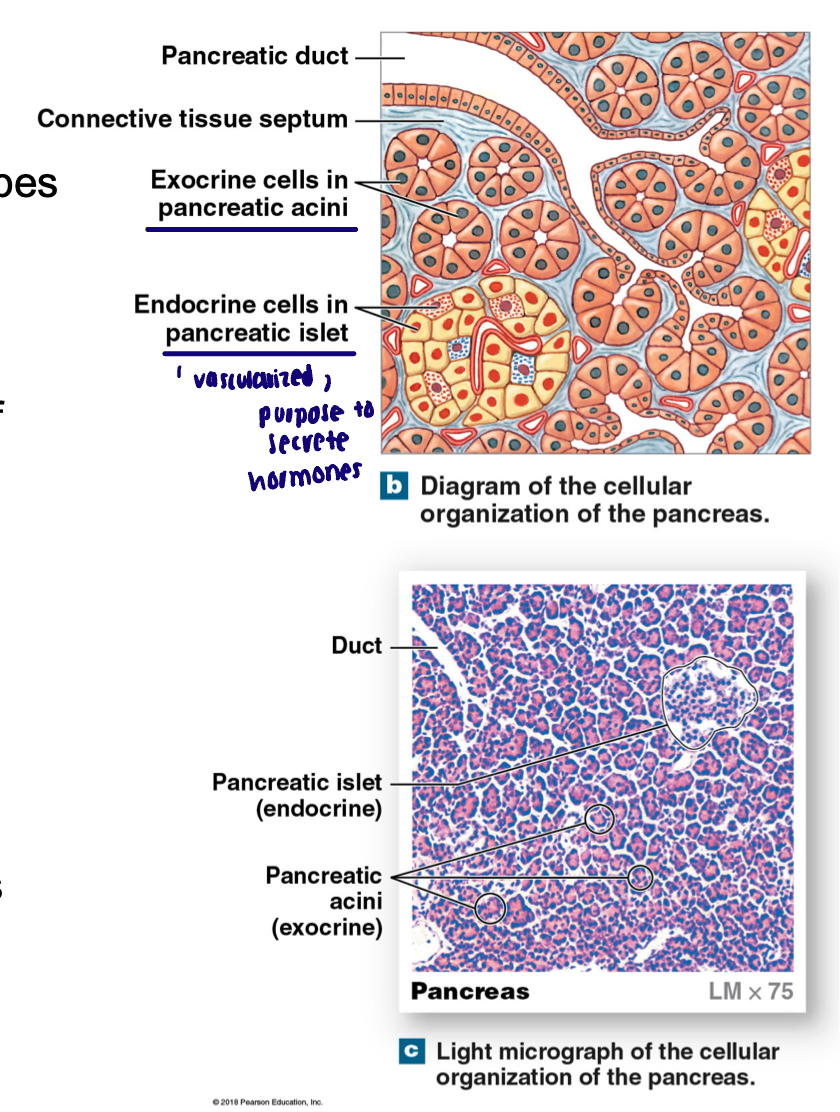
Histology of the pancreas → for endocrine and exocrine
Endocrine: Islets of Langerhans (pancreatic islet): subtypes of endocrine cells
Alpha: glucagon, 18-20% of cells
Beta: insulin, 73-75% cells
Delta: somatostatin (GHIH), 4-6% of cells
D cells also make somatostatin
Inhibit release of glucagon and insulin and slows rate of digestion
Exocrine:
Pancreatic acini: pockets of simple cuboidal cells that produce pancreatic juice
Empty into series of epithelial lined ducts leading to pancreatic duct
Insulin and glucagon maintain…
Glucose homeostasis and have antagonistic effects
Beta cells respond to…
INCREASED blood glucose (hyperglycemia) to release insulin
Other influences: SNS decreases release, PNS increases release
What is insulin
Circulates in what form
Half life
Degraded by
Peptide hormone (cannot go through plasma membrane)
Circulates in free form; half life 3-8 minutes, degraded by liver and kidney
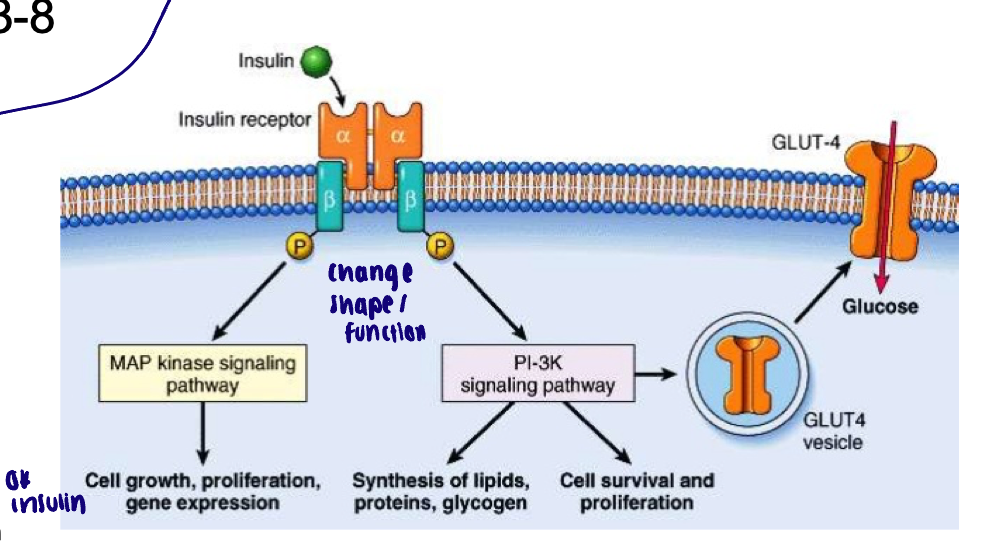
Receptor activity of insulin
Where are there insulin receptors and what are the exceptions
Structure
Steps involved
Most cells of the body contain insulin receptors (exceptions: portions of brain, kidney, RBC, lining of GI)
Tetramer with kinase activity on Beta subunits
Beta subunits phosphorylate each other
Increase absorption of glucose into cells
Promote energy storage
In glycogen - liver and skeletal muscle
Essentially, putting glucose transporters on cell membrane (GLUT4)
Receptor for insulin is tyrosine kinase
When insulin binds to alpha subunits → phosphorylates Beta subunits
Overall effect of insulin on target organs
ANABOLIC
Stimulates glucose uptake by target cells, and promote synthesis of carbohydrates, fats, and proteins
What is diabetes Mellitus
Impaired entry glucose into cells and elevation of glucose in blood
Type I and II
Type I DM
Around 5% of cases of DM
Beta cell destruction, due to autoimmune dysfunction
Type II DM
Around 95% of cases of DM (growing)
Associated with obesity
Loss of regulation of:
Insulin secretion: beta cells can still make insulin but dysfunctional response to glucose levels
Insulin resistance: decreased tissue responsiveness to insulin
Clinical features of DM
Hyperglycemia
Glycosuria
Thirst/urination
Muscle fatigue
Bruising
Nerve tingling/numbness
Confusion/dizziness
Cardiovascular disease
Kidney disease
Loss of vision
Diabetic ketoacidosis
Excess production of ketone bodies → acid-base imbalance
Life threatening if untreated
Pancreatic juice → primary effects and how much
Neutralize acidic chyme (aqueous component → buffer acidic chyme)
Enzymatic digestion → vast majority of chemical digestion from enzymes from pancreas
Pancreatic secretions: approximately 1 liter/day
Aqueous component
H2O, HCO3- (bicarb), PO4- (phosphate buffering system)
Enzymatic components
Pancreatic alpha amylase → amylase also in saliva
Breaks down carbs
Pancreatic lipase
Breakdown of lipids
Nucleases
Breakdown of nucleic acids
Pancreatic proteases and peptidases
Breakdown of proteins
Released in an inactive form; activated when then come in contact with brush border enzymes
Hormonal regulation of pancreatic juice - aqueous component
Secretin → responsive to pH change
Stimulus for release of secretin: decrease pH of duodenal content because we need to buffer chyme
Hormonal regulation of pancreatic juice - enzymatic component
Cholecystokinin (CCK)
Stimulus for release of CCK: breakdown products of fats and proteins in duodenum
Additional functions: contraction of gall bladder and relaxation of sphincters
Both of these hormones (secretin and CCK) are released from…
Enteroendocrine cells in the duodenal mucosa
Function of the liver
More than 200 functions
Metabolic regulation
Hematological regulation
Production of bile
Metabolic regulation → Liver function
Extract nutrients from GI system blood before it returns to systemic circulation. Stores nutrients and corrects deficiencies
Maintains homeostasis of blood carbohydrate, lipid, and amino acid levels [glycogen storage]
Removal of wastes, ie. drugs/toxins to be degraded and conversion of ammonia into urea
Storage of vitamins and minerals
Hematological regulation → Liver function
Immune: macrophages destroy old RBCs cells and antigen presentation
Synthesis of clotting factors
Synthesis of plasma proteins
Synthesis of angiontensinogen
Removal of hormones
Liver anatomy
Approximately 3.3 lbs, Reddish brown, located mostly in right upper abdominal cavity
4 lobes of liver: Right lobe, left lobe, caudate lobe, quadrate lobe
Porta hepatis: blood delivered to liver via hepatic portal vein (venous blood from stomach and intestines) and from hepatic artery
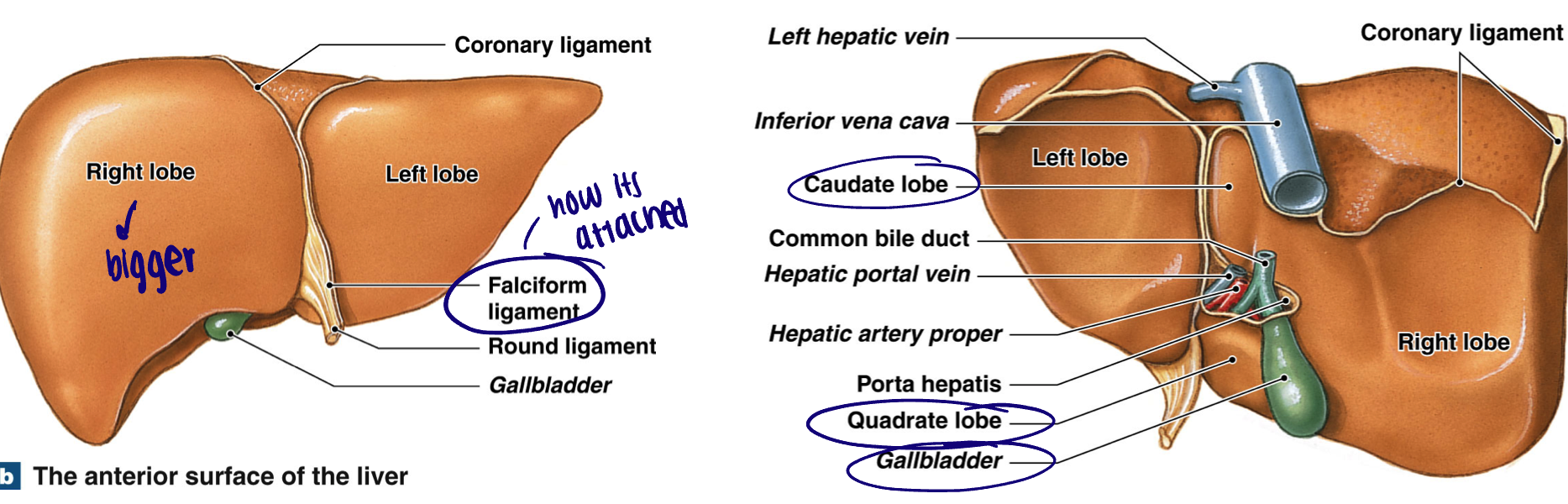
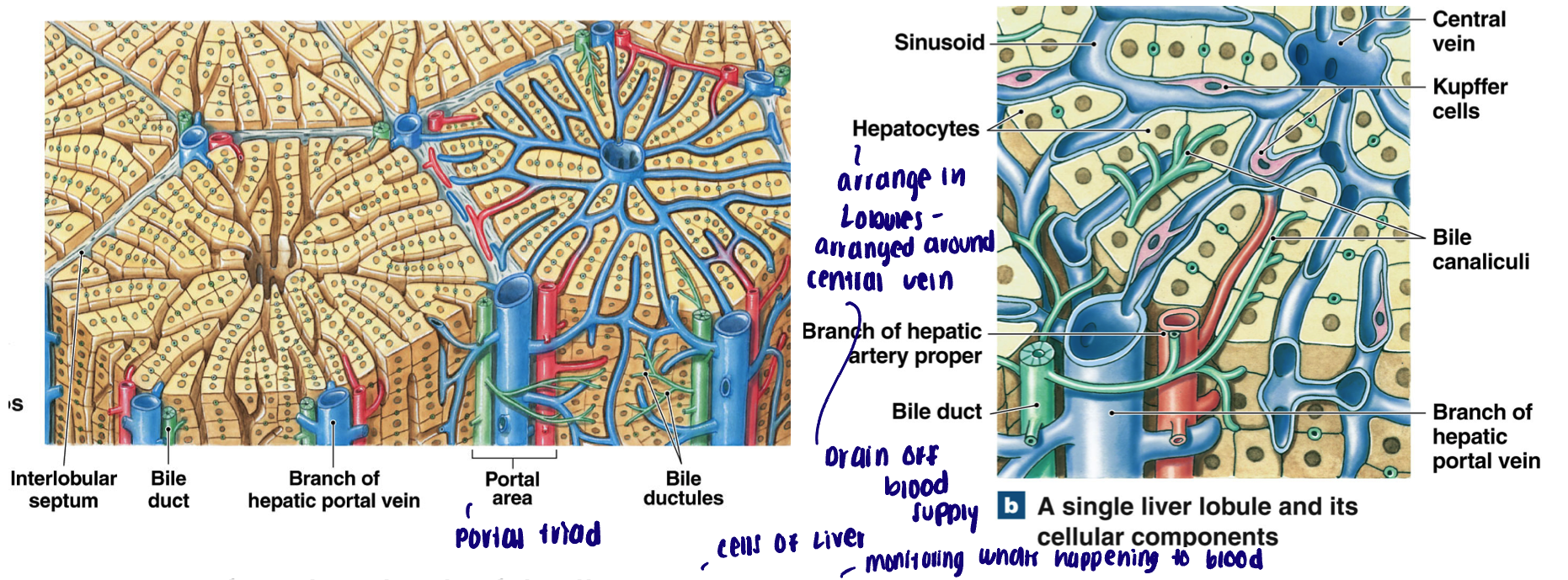
Liver histology
Lobule: functional unit of the liver, hepatocytes arranged in plates around a central vein. Sinusoids allow hepatocytes to ‘filter’ fluid as it moves towards central vein
Portal triads: found at each corner; branch of hepatic artery, portal vein, bile duct
Blood from portal vein and hepatic artery (bringing oxygenated blood to liver) enter hepatic sinusoids which ultimately empty into central hepatic veins (drains into inferior vena cava)
Hepatocytes synthesize bile which is emptied into small ductules which converge into small bile ducts (carried opposite direction from central vein)
Where is bile produced and then stored/concentrated
It is produced in the liver; stored and concentrated in the gallbladder
Function of bile
Break apart large lipid droplets within chyme of the duodenum
Composition of bile
Bile salts: synthesized from cholesterol
Amphipathic: solubilize lipids in an aqueous environment
Bile pigments: bilirubin (yellow); byproduct of heme degradation
Ions: buffer the acidity of chyme
Water: bulk of bile; dilute chyme
How much bile formed and what happens to it
Around 1 Liter of bile formed/day
Most of the bile salts are “recycled”
Bile salts are absorbed in the ileum and returned to the liver via the hepatic portal vein
What does the bile duct system consist of
All bile produced by hepatocytes ultimately drains into the common hepatic duct
Bile enters/exits gallbladder via the cystic duct
Cystic duct and hepatic duct converge to form the common bile duct
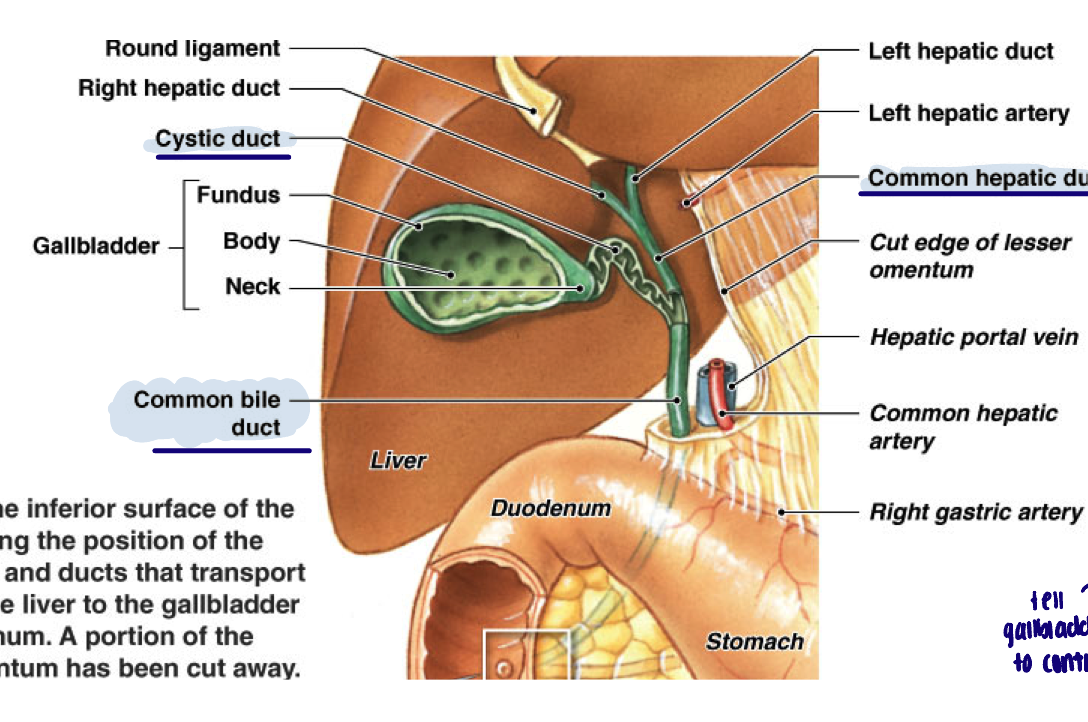
Gallbladder
Hollow pear shaped organ; storage of bile, concentrating of bile (via fluid reabsorption)
Parts of bile duct system
Hepatopancreatic ampulla: Site of convergence of bile duct and pancreatic duct
Hepatopancreatic (Oddi) Sphincter: allows bile and pancreatic juice into duodenum
CCK: hormone, contracts gall bladder, relaxes hepatopancreatic sphincter
Function of the small intestine
Majority of chemical digestion:
Enzymes secreted from small intestinal epithelium (small fraction of digestion)
Pancreatic juice
Bile from the gallbladder
Absorption of breakdown products of carbohydrates, lipids, proteins
Also vitamins and minerals (90% of nutrient absorption)
Absorption of fluids:
Secretions from accessory glands and GI organs
Fluids from food
Recycling of bile salts
Anatomy of the small intestine
Duodenum:
10 inch section following stomach; mixing bowl - entry of pancreatic and bile duct - duodenal glands (mucus and bicarbonate); few plicae, small villi
Jejunum:
8 ft segment following duodenum; majority of chemical digestion and absorption; abundant plicae and large villi
Ileum:
11.5 ft final segment; remainder of absorption (vit. B12, bile salts); reduction in plicae and villi; abundant lymph tissue; ends at ileocecal valve
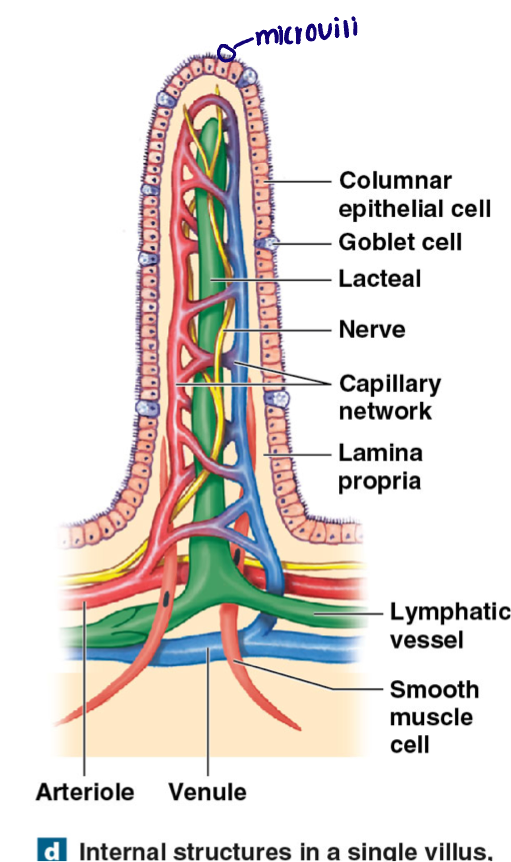
Histology of small intestine - what is used to maximize surface are
Plicae circulars: series of (permanent) transverse folds
Villi: finger like projections covering entire surface, each villi covered in simple columnar epithelium
Microvilli (brush border): hair like projections off each epithelial cell
Each villus absorbs productions of digestion into…(small intestine histology)
Lamina propria: connective tissue
Capillaries: carry absorbed material to hepatic portal
Central lacteal: lymphatic vessel (transport large materials)
Cell types of small intestine
Simple columnar epithelium (brush border)
Goblet cell: produce mucus
Intestinal crypts (glands) found at the base of the villi
Brush boarder stem cells
Paneth cells: immune cells; release antibacterial chemicals
Endocrine cells: release CCK, secretin, and others
Motility of small intestine
Duodenum moves chyme toward jejunum
ENS: weak peristaltic contractions, regulated by pacesetter cells
Gastroenteric and gastroileal reflexes: generate majority of peristalsis in remaining intestine
Stimulated by stretch in stomach
Gastroenteric: increases movement and secretion across entire small intestine
Gastroileal: relaxation of the ileocecal valve
PNS
Increase speed and force of ENS
Intestinal hormones (CCK, motilin)
Can enhance or suppress reflexes
Function of the large intestine
Absorption of fluid and ions:
Around 1500 mL chyme/day enters (mostly water) only 200 mL/day exits
Efficient absorption of remaining bile salts
Bacterial synthesis of vitamins: Notably Vitamin K, Biotin (B7), and vitamin B5
Then absorbed by large intestine
Storage and elimination of feces
Composition of feces
75% water
4% bacteria
Indigestible materials
Dead epithelial cells
Pigments: urobilins and stercobilins (breakdown of heme)
Nitrogenous wastes: e.g. ammonia (bacterial break down of amino acids)
Other bacterial metabolites: e.g. hydrogen sulfide
Anatomy of the large intestine
Divided into three parts (around 5 ft long):
Cecum: small pouch, begins compaction
Appendix: lymphatic organ
Colon: haustra, series of pouches
Ascending, transverse, descending, sigmoid segments
Rectum: terminal portion
Leads to anal canal and anus (opening)
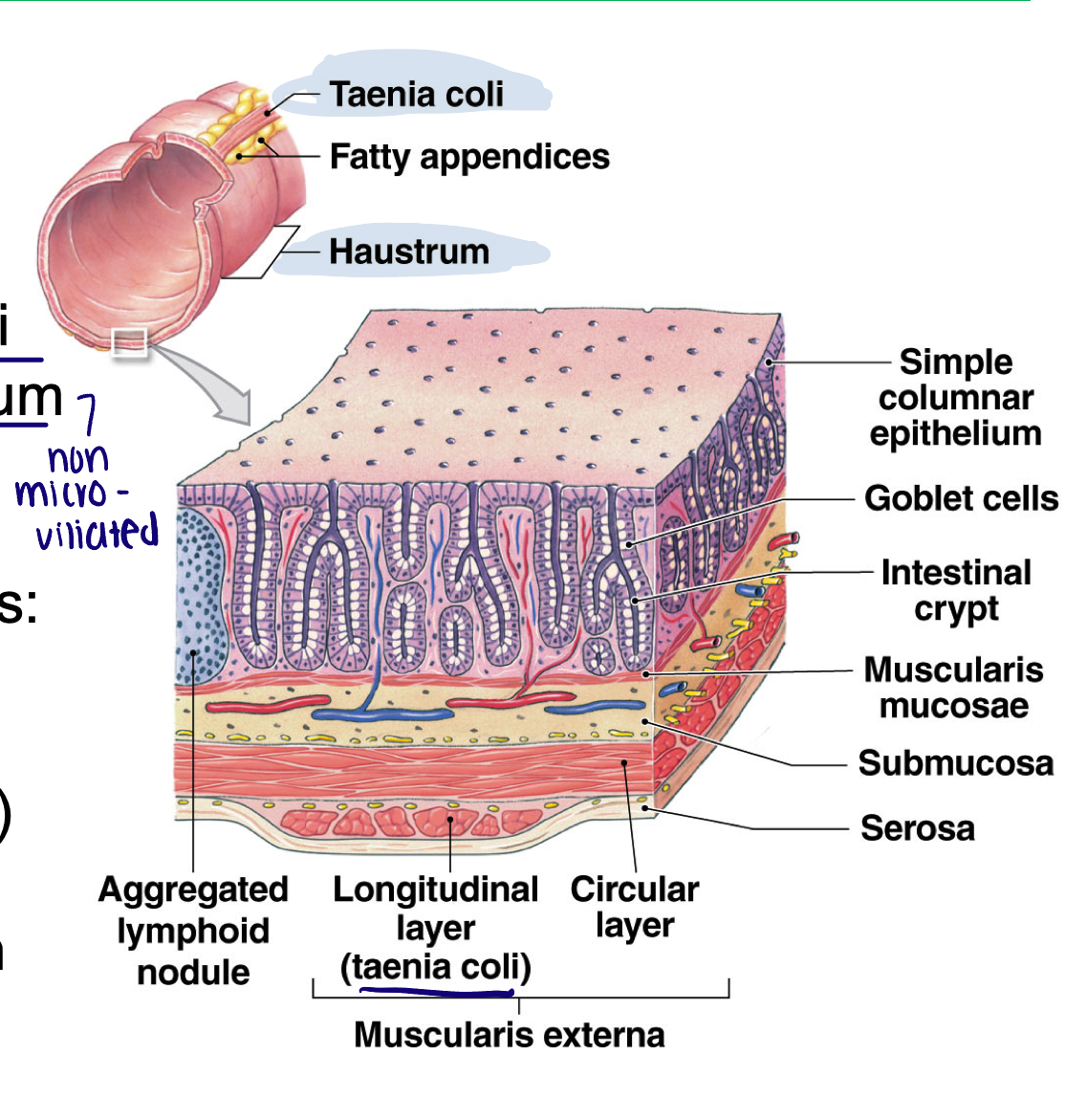
Histology of the large intestine
Surface of the colon:
Smooth: no plicae, no villi
Simple columnar epithelium (non micro villiated)
Deep intestinal glands (crypts)
Numerous goblet cells: mucus
Arranged into haustra (sacs)
Muscle layer reduced to think bands called taenia coli
Motility of the large intestine
Gastroileal reflex: opening of ileocecal valve in response to gastric stretch, moves chyme into cecum
Movement from cecum to transverse colon:
Very slow, hours to allow for water reabsorption
ENS
Peristaltic waves
Segmentation contractions: haustral churning
Mass movements:
Powerful peristaltic contractions
Move material from transverse colon through rest of large intestine
Stimulated by dissension of stomach and duodenum
Occur around 1-3 times a day
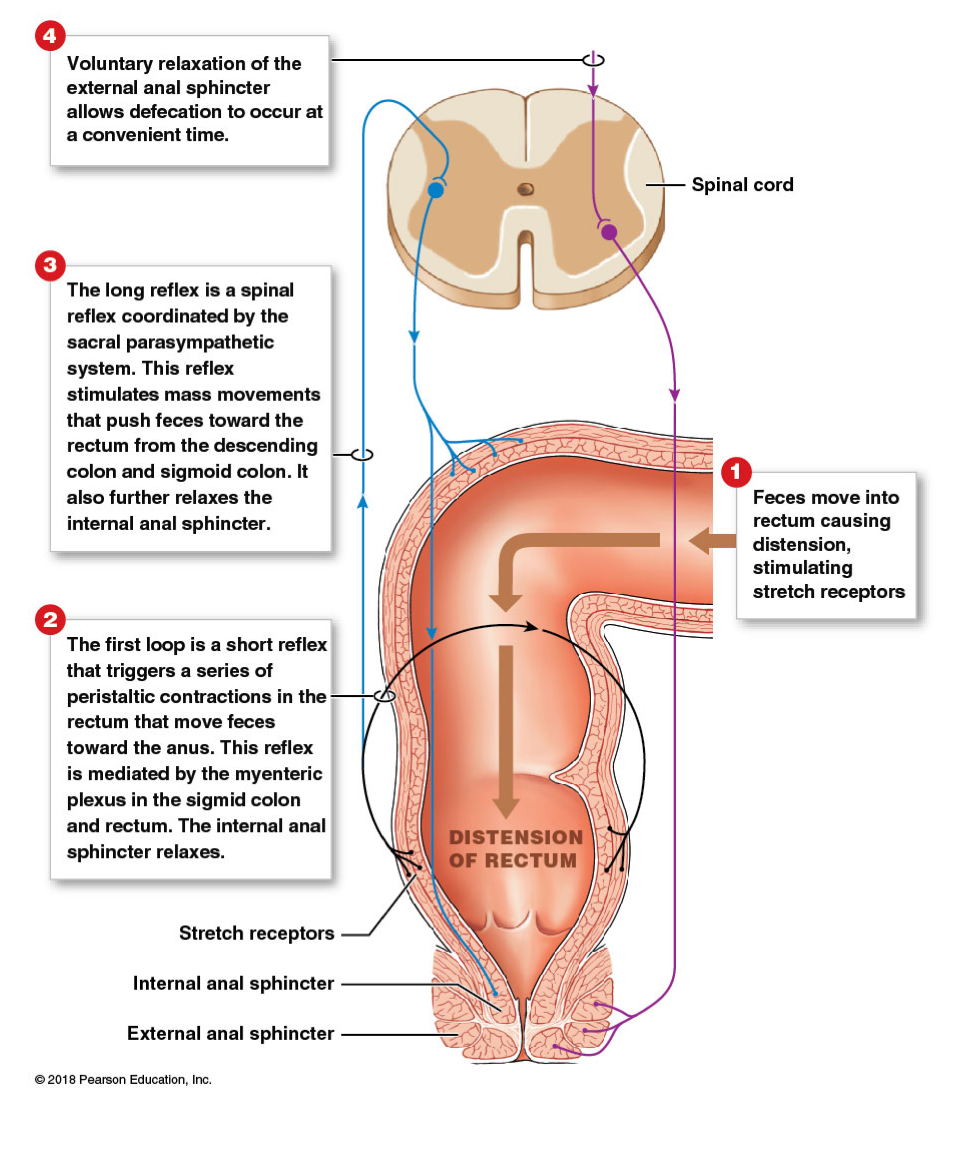
Defecation reflex
Mass movement: push feces into rectum → stimulate stretch receptors
Activates ENS defection response:
Increased peristalsis in sigmoid colon and rectum
Activates PNS defecation response:
Increased mass movement in descending and sigmoidal colon
Relaxation of internal anal sphincter
Relaxation of external sphincter: voluntary