Myelodysplastic syndrome + Lymphomas
1/108
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
109 Terms
What is the most common peripheral blood finding in dyserythropoiesis in MDS?
The presence of oval macrocytes, especially when vitamin B12 and folate levels are normal
What should be suspected when oval macrocytes are seen with normal B12 and folate levels?
Myelodysplastic syndrome (MDS)
What RBC morphologies can appear in MDS despite adequate iron stores?
Hypochromic microcytes
What additional RBC abnormalities may be present in dyserythropoiesis in MDS?
Poikilocytosis
Basophilic stippling
Howell-Jolly bodies
Siderocytes
What are nuclear abnormalities seen in bone marrow RBC precursors in Dyserythropoiesis MDS?
Multinucleation
Abnormal nuclear shapes (e.g., lobes, buds)
Nuclear fragments in cytoplasm
Internuclear bridging
What are abnormal cytoplasmic features in Dyserythropoiesis erythroid precursors?
Basophilic stippling
Uneven cytoplasmic staining
What specific type of erythroid precursor is a hallmark of MDS?
Ring sideroblasts, which are erythroid precursors with iron-loaded mitochondria encircling the nucleus.
What is a key cytoplasmic clue of dysmyelopoiesis MDS in mature white blood cells?
Persistent basophilia in the cytoplasm of otherwise mature WBCs, indicating nuclear-cytoplasmic asynchrony.
What are common granulation abnormalities in neutrophils in MDS?
Larger-than-normal granules
Hypogranulation or agranulation (absence of granules)
What nuclear abnormalities may be seen in neutrophils on a peripheral smear in MDS
Hyposegmentation
Hypersegmentation
Ring-shaped nuclei
How does dysmyelopoiesis affect bone marrow cellularity?
Granulocytic hypoplasia or hyperplasia
Monocytic hyperplasia (common)
What are common platelet abnormalities seen in dysmegakaryopoiesis MDS
Giant platelets
Abnormal granulation, including hypogranulation or agranulation
Platelets with large fused granules
Circulating micromegakaryocytes (very small megakaryocyte-like cells in the blood)
What is dysmegakaryopoiesis?
The abnormal development of megakaryocytes, the cells that produce platelets.
What are the key bone marrow features of dysmegakaryopoiesis?
Large mononuclear megakaryocytes (one large nucleus instead of lobulated)
Bilobed nuclei (two connected nuclear lobes)
Multiple small, separate nuclei (instead of a single multilobed nucleus)
What is dysmyelopoiesis?
the abnormal development of granulocytic cells (e.g., neutrophils, eosinophils, basophils).
What is dyserythropoiesis?
the abnormal development of red blood cell precursors in the bone marrow.
According to the FAB system, what percentage of blasts is required for a diagnosis of acute leukemia?
At least 30% blasts in the bone marrow.
What is Refractory Anemia (RA)?
an MDS subtype characterized by anemia that does not respond to treatment, with <5% blasts in the bone marrow.
What are the key features of RA?
Anemia with little to no response to treatment
<5% blasts in bone marrow
<1% blasts in peripheral blood
May show dyserythropoiesis
What distinguishes RARS from RA?
RARS has the same criteria as RA but with ≥15% ring sideroblasts in the bone marrow (iron-laden erythroid precursors).
What defines Refractory Anemia with Ring Sideroblasts (RARS)
Anemia
Erythroid dysplasia only
≥15% ring sideroblasts
No blasts in blood
<5% blasts in marrow
What defines Refractory Anemia with Excess Blasts-1 (RAEB-1)
<5% blasts in peripheral blood
5%–9% blasts in bone marrow
No Auer rods
<1 × 10⁹/L monocytes
May show dysplasia in multiple cell lines
What is RAEB-T, and why is it significant?
is an advanced MDS subtype with 20–30% blasts in the bone marrow, often considered a pre-leukemic phase (transforms to AML).
What are the diagnostic blast levels for RAEB-T?
20–30% blasts in bone marrow
≥5% blasts in peripheral blood
Considered a transitional stage between MDS and acute myeloid leukemia (AML) in the FAB system
Now reclassified as AML under the WHO classification
What are the diagnostic features of CMML?
Persistent monocytosis: ≥1 × 10⁹/L
<20% blasts in bone marrow
<5% blasts of both myelocytic and monocytic lineages
±15% ringed sideroblasts
Shows persistent monocytosis
Dysplasia in one or more cell lines
May have organomegaly (e.g., splenomegaly)
What differentiates RAEB-2 from RAEB-1?
5%–19% blasts in peripheral blood
10%–19% blasts in bone marrow
± Auer rods present
<1 × 10⁹/L monocytes
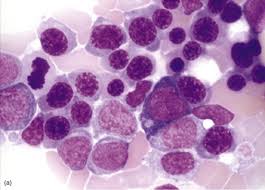
MDS Dyserythropoiesis

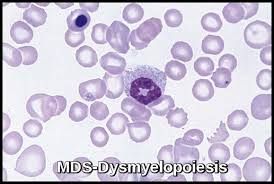
MDS Dysmyelopoiesis

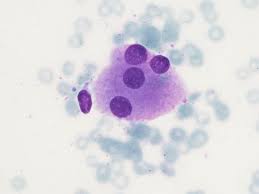
MDS Dysmegakaryopoiesis
What is the underlying cause of Myelodysplastic Syndromes (MDS)?
failure to produce enough healthy blood cells, due to genetic changes in a hematopoietic stem cell.
How do these genetic changes affect the bone marrow in MDS
They disrupt normal cell growth and differentiation, leading to:
Accumulation of abnormal, immature cells
Impaired production of functional blood cells
Which blood cell lines can be affected in MDS?
Erythroid lineage (RBCs)
Myeloid lineage (granulocytes/monocytes)
Megakaryocytic lineage (platelets)
Who is most commonly affected by MDS?
Older adults, typically over 50 years of age.
What are the common bone marrow and blood findings in MDS?
Hypercellular bone marrow
Peripheral pancytopenia (deficiency of all three blood cell types)
What are common signs of anemia in MDS?
Macrocytosis (large red cells)
Anisocytosis (variation in RBC size)
Increased MCV (mean corpuscular volume)
Increased RDW (red cell distribution width)
Is thrombocytopenia common in MDS?
Yes, low platelet count (thrombocytopenia) is usually present.
What are the features of platelets on a peripheral smear in MDS?
Variable in size
Some platelets appear hypogranular
How are WBC counts affected in MDS?
WBCs may be increased, decreased, or normal.
What types of WBC abnormalities are seen in MDS?
Abnormal granulation in neutrophils and eosinophils
Presence of Pseudo-Pelger-Huet cells (bilobed neutrophils)
What are lymphomas?
malignancies that originate from uncontrolled growth of cells in the lymphatic system.
What is the hallmark physical sign of lymphoma?
Abnormal enlargement of lymph nodes.
Is peripheral blood typically involved in lymphoma?
No, peripheral blood involvement is not common in most lymphomas.
How are lymphomas classified?
Hodgkin’s Disease (HD)
Non-Hodgkin’s Lymphoma (NHL)
What is a characteristic histologic feature of HD?
Presence of Reed-Sternberg cells — giant, multinucleated neoplastic cells.
What percentage of cells in lymph nodes are neoplastic in HD?
Only a few cells are neoplastic; most appear normal.
What type of cells are involved in Non-Hodgkin’s Lymphoma
B-lymphocytes (95%)
T-lymphocytes (5%)
How do the neoplastic cells in NHL appear?
They are uniformly abnormal, and many cells are neoplastic.
What is required for a lymphoma diagnosis?
Histological examination of lymph node tissue.
How does Hodgkin’s Disease typically start?
Unifocal — it usually begins in one lymph node.
How does Non-Hodgkin’s Lymphoma usually present?
Multifocal — involves multiple lymph nodes at onset.
How does HD spread compared to NHL?
HD: Spreads in a predictable, orderly pattern to adjacent nodes.
NHL: Spreads in a less predictable manner.
Does HD or NHL more commonly involve non-lymphatic tissues?
HD: Unlikely to involve non-lymphatic tissue.
NHL: May involve non-lymphatic tissues such as GI tract, bone marrow, or skin.
What age groups are most commonly affected by HD?
Bimodal distribution: ages 10–20 years and older than 45.
Which sex is more commonly affected by HD?
More common in men.
What is a classic early sign of HD?
Painless enlargement of a lymph node, especially in the neck (cervical) region.
Can the enlarged lymph node become painful in HD
Yes, rapid enlargement can cause a painful mass.
What are the “B symptoms” in Hodgkin’s Disease?
Fever
Night sweats
Weight loss
What are the “A symptoms” in Hodgkin’s Disease?
No symptoms
How does Hodgkin’s Disease spread through the lymphatic system?
It spreads to adjacent lymph nodes in a stepwise fashion.
What are potential causes of death in HD patients?
Patients may die from recurrent infections or organ failure.
What is the definitive test for diagnosing Hodgkin’s Disease?
Lymph node biopsy.
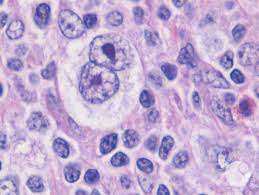
What confirms the diagnosis of Hodgkin’s Disease?
The presence of Reed-Sternberg (R-S) cells in the lymph node biopsy.
What are the features of a Reed-Sternberg cell?
Large size (4–8× a normal lymphocyte)
Usually bi-nucleated or multinucleated
Prominent eosinophilic nucleoli with a halo, giving an "Owl Eye" appearance
What changes may be seen in the peripheral blood of HD patients?
↑ Monocytes and eosinophils (absolute increase)
Normal platelets, no anemia early
Possible lymphocytosis initially
Large abnormal lymphocytes on smear
What blood changes occur as HD progresses?
Leukocytosis
Granulocytosis resembling a leukemoid reaction
Toxic granulation in advanced disease
Lymphocytopenia (a poor prognostic sign)
Rare plasma cells and occasional Reed-Sternberg cells
Is the bone marrow typically involved in HD?
Rarely involved
BM biopsy may be positive, but BM aspirate is usually negative
How common is NHL compared to Hodgkin’s Disease?
3 times more common than Hodgkin’s Disease.
What is the most common symptom of NHL?
Painless enlargement of lymph nodes, especially cervical nodes.
What systemic symptoms may occur in NHL?
Fever
Weight loss
Night sweats
(Seen in about 30% of patients)
Are blood counts typically abnormal in NHL?
No, blood counts are often normal.
What serologic test may occasionally be positive in NHL?
Direct Antiglobulin Test (DAT) may be positive in some patients.
What characterizes low-grade NHL?
slow-growing and primarily involves lymph node enlargement.
What is a typical feature of intermediate-grade NHL?
extranodal disease (outside the lymph nodes) and more rapid lymph node enlargement.
What makes high-grade NHL more severe?
rapid disease progression and aggressive lymph node enlargement.
Which type of Hodgkin’s Disease has scarce Reed-Sternberg cells and many lymphocytes?
Lymphocyte Predominant type – characterized by scarce R-S cells.
What is the hallmark of Nodular Sclerosis Hodgkin’s Disease?
Occasional R-S cells are seen in Nodular Sclerosis type.
Which subtype of HD shows many Reed-Sternberg cells?
Mixed Cellularity type – it has many R-S cells along with a mixed population of background cells.
Which HD variant has abundant R-S cells and few lymphocytes?
Lymphocyte Depleted type – marked by abundant R-S cells and low lymphocyte count.
What background cellular elements are typically seen in nodular sclerosis Hodgkin lymphoma?
Small lymphocytes, eosinophils, and histiocytes.
What characterizes the cellular background in mixed cellularity classical Hodgkin lymphoma?
A diffuse background composed of small lymphocytes, histiocytes, eosinophils, neutrophils, and plasma cells.
What type of lymphocyte is commonly seen in low-grade lymphocytic lymphoma?
Small lymphocytes
What is a small cleaved cell?
a type of lymphocyte with notched or indented nuclei, often seen in certain lymphomas.
How big are large cells (cleaved or non-cleaved) compared to normal lymphocytes?
They are typically 2 to 3 times the size of a normal lymphocyte.
What defines an immunoblastic large cell?
4 to 5 times the size of a normal lymphocyte and has a prominent nucleolus.
What characterizes a lymphoblastic cell?
has a convoluted or large nucleus, often associated with aggressive lymphomas.
What is a small non-cleaved cell?
it has a round nucleus without indentations and is seen in certain high-grade lymphomas like Burkitt lymphoma.
What are the different lymphocyte types
–Small lymphocyte: low grade lymph. lymphoma
–Small cleaved cell
–Large cell (cleaved & non-cleaved): 2-3x lymph
–Immunoblastic large cell: 4-5x normal lymph
–Lymphoblastic cell: nucleus convoluted or large
–Small non-cleaved cell
What type of cell is involved in Mycosis Fungoides and Sezary Syndrome?
Mature T-helper cells are involved in both conditions.
What is an early symptom seen in Mycosis Fungoides?
Pruritis, or severe itching, is often an early sign.
What skin changes are observed in Mycosis Fungoides?
The skin may become thickened, wrinkled, and red, forming plaques or generalized erythroderma.
How is Mycosis Fungoides diagnosed?
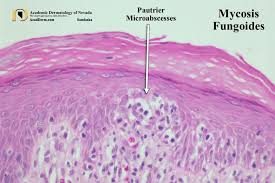
Through skin biopsy, showing dermis and epidermis involvement.
What organs are typically affected in Sezary Syndrome?
Lymph nodes, liver, spleen, and lungs may be involved.
What key lab feature is seen in both Mycosis Fungoides and Sezary Syndrome?
Lymphocytes with cerebriform nuclei are characteristic.

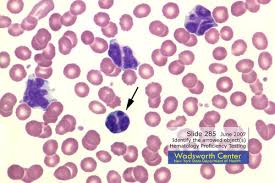
cerebriform nuclei Mycosis Fungoides and Sezary Syndrome
What is Mycosis Fungoides?
the most common cutaneous lymphoma, composed of small to medium-sized lymphoid cells with cerebriform (irregular) nuclei and a preference for the epidermis and dermis.
What is Sézary Syndrome?
a disseminated form of cutaneous T-cell lymphoma characterized by widespread skin involvement (erythroderma), lymphadenopathy, and circulating malignant T cells with cerebriform nuclei (Sézary cells).
What histologic feature is characteristic of Mycosis Fungoides in the epidermis?
Pautrier microabscesses — aggregates of neoplastic lymphocytes in the epidermis.
What type of malignancy is Burkitt lymphoma?
A highly aggressive B-cell malignancy.
Which geographic region is most commonly affected by the endemic form of Burkitt lymphoma?
Sub-Saharan Africa.