ANSC*3080: Labs
1/205
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
206 Terms
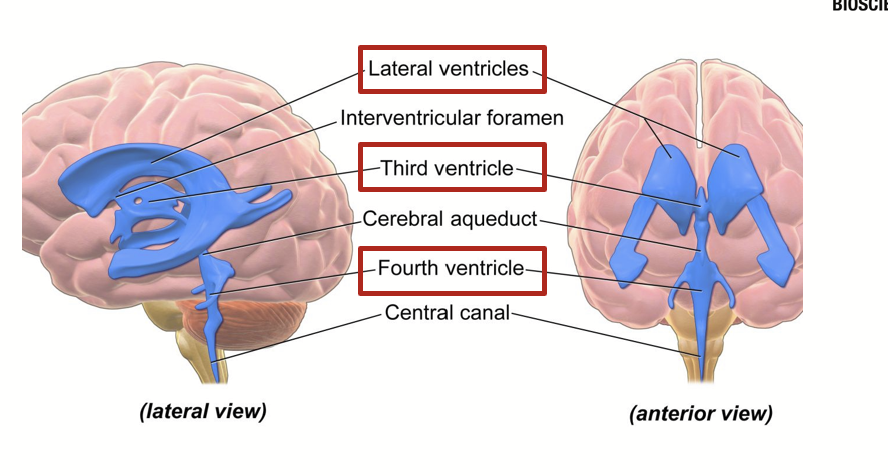
ventricles
Cavities in between brain structures that are connected to form a network of canals filled up with cerebrospinal fluid.
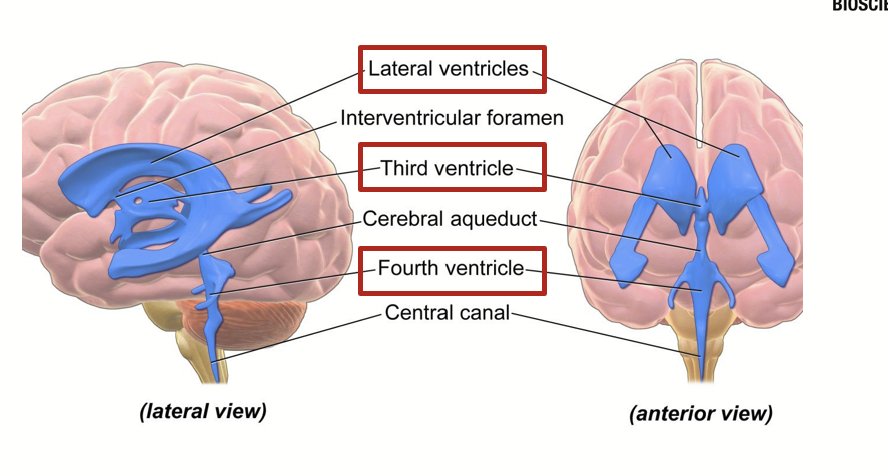
lateral ventricles
Ventricles found in or under the cerebrum or top of the brain.
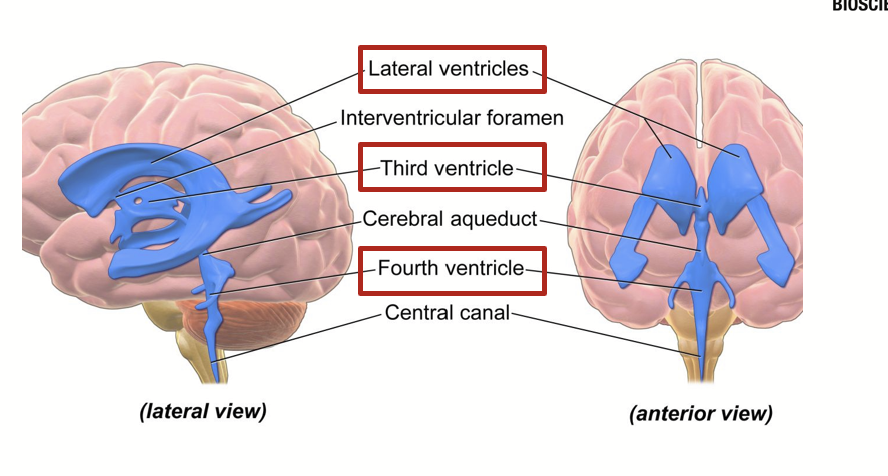
third ventricle
Ventricle in the center of the brain.
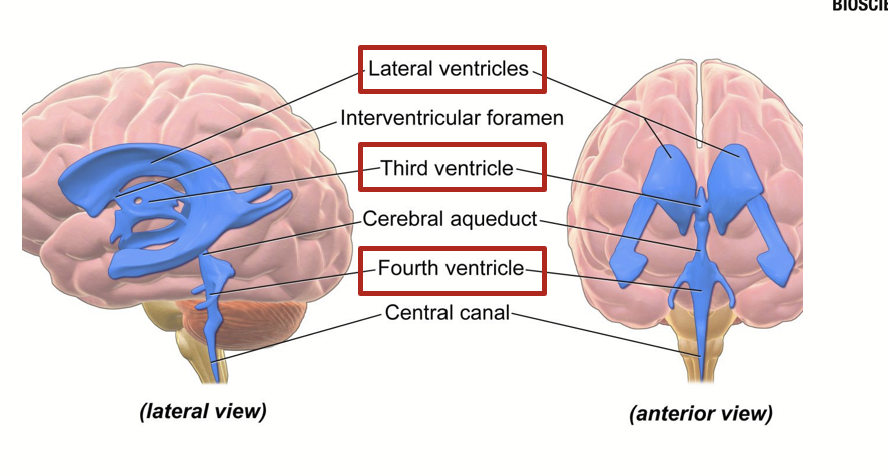
fourth ventricle
The ventricle found towards the bottom of the brain near the brain stem.
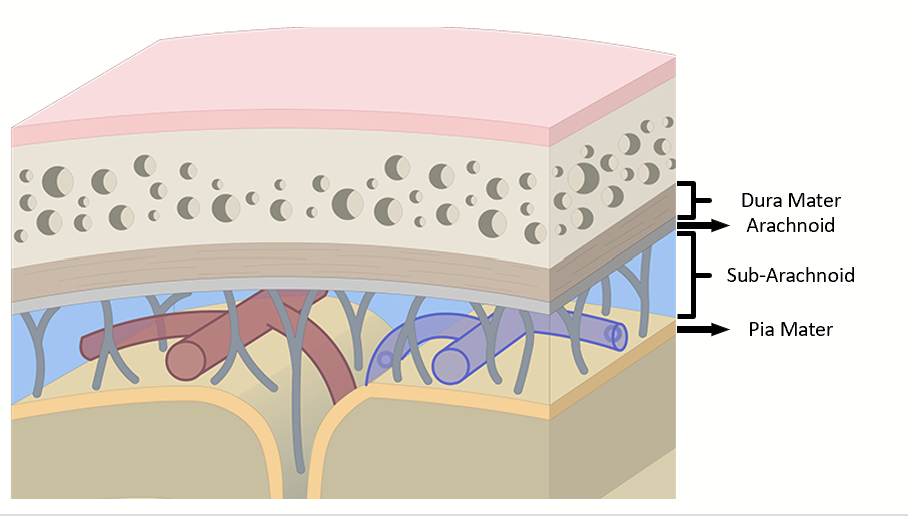
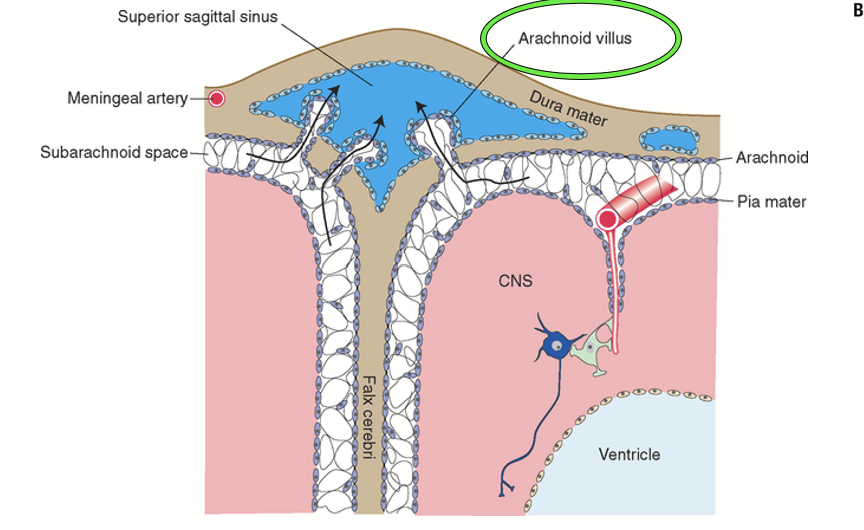
meninges
Help maintain the structural integrity of the brain, provide additional protection and are responsible for the formation of cerebrospinal fluid. Correspond to three layers tightly wrapping the outside of the brain and the spinal cord. Act as a barrier between blood and nervous tissue.
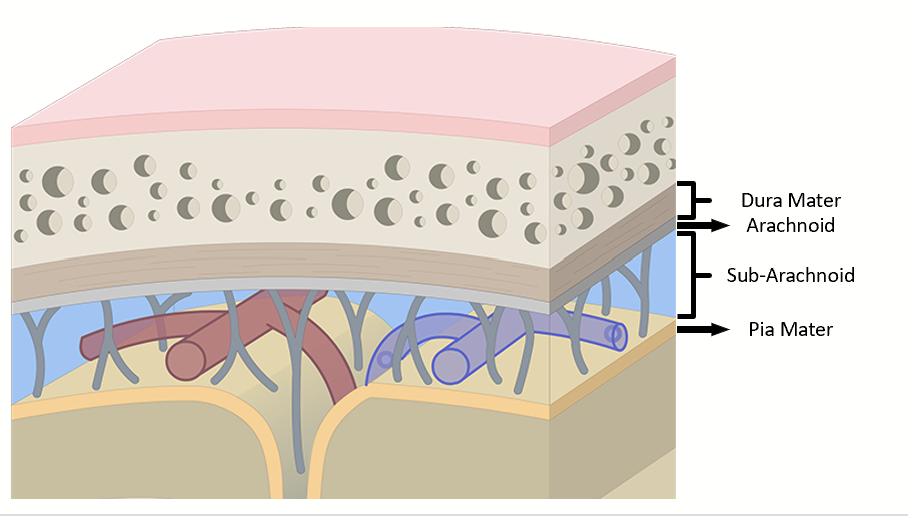
dura mater
The layer of the meninges stuck against the skull.
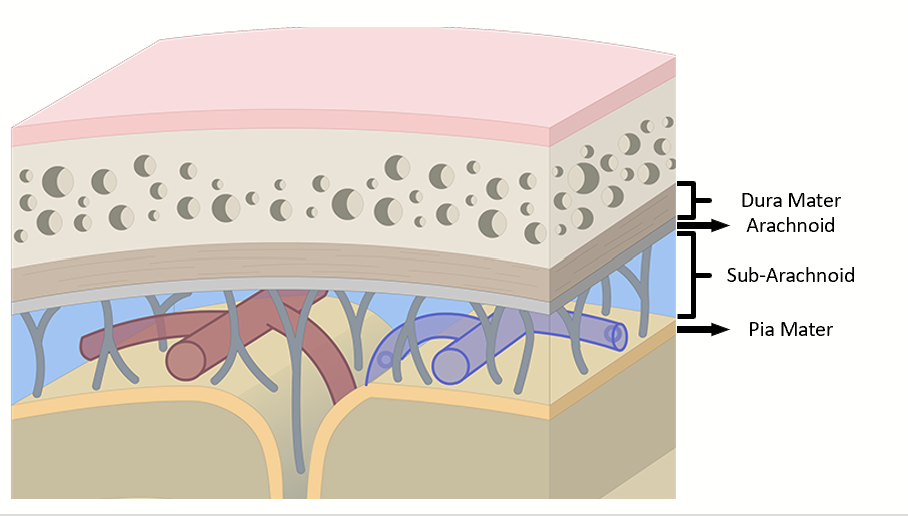
arachnoid
The layer of the meninges that is a looser mesh membrane against the dura mater.
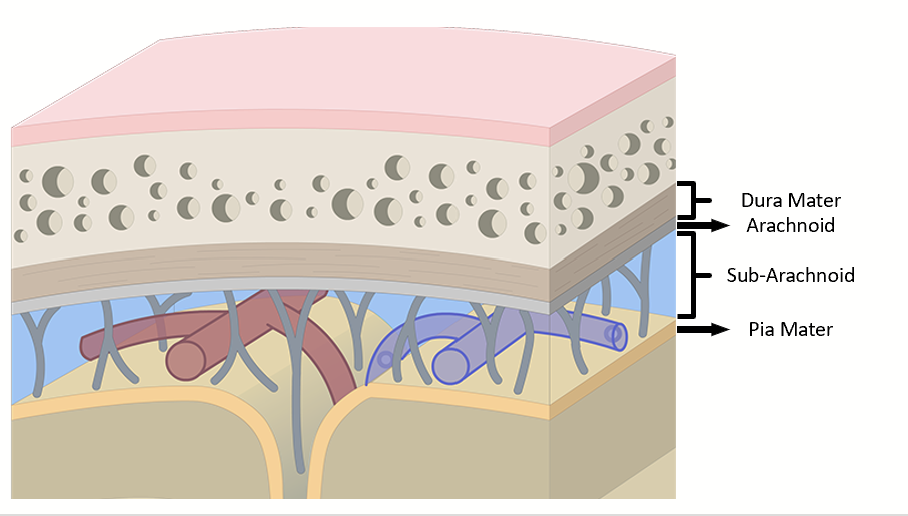
pia mater
The layer of the meninges that is a thin tight membrane directly against the nervous tissue.
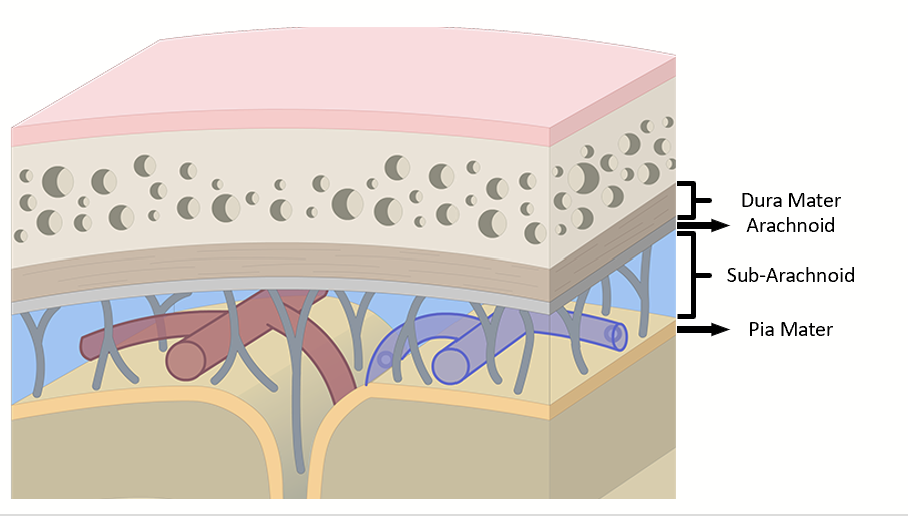
sub-arachnoid space
Space between the arachnoid and the pia matter. Filled with cerebrospinal fluid.
cerebrospinal fluid
Produced by the choroid plexus (specialized areas of the pia mater) in the third and fourth ventricles. Flows through the ventricles to the central canal of the spinal cord and enters the sub-arachnoid space in the fourth ventricle.
Forms a cushion inside the meninges, allows it to act as a shock absorber and provide nutrition to the brain. Also acts in detoxification.
Continuously produced and thus if it is not drained, it will accumulate and create pressure, compressing nervous tissue, resulting in permanent damage and death.
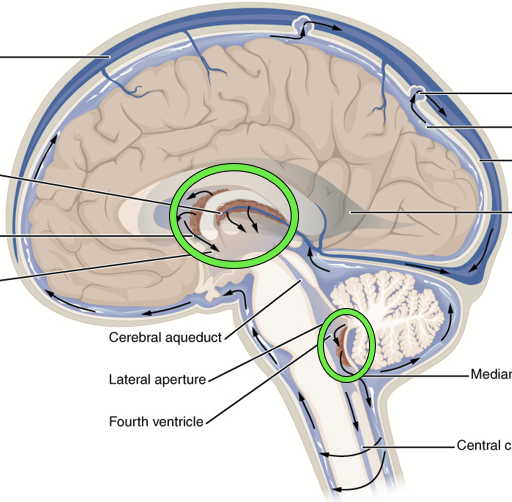
choroid plexus
Specialized areas of the pia mater where blood is “filtered” to produce cerebrospinal fluid with the optimum composition for survival and function of nerve cells.
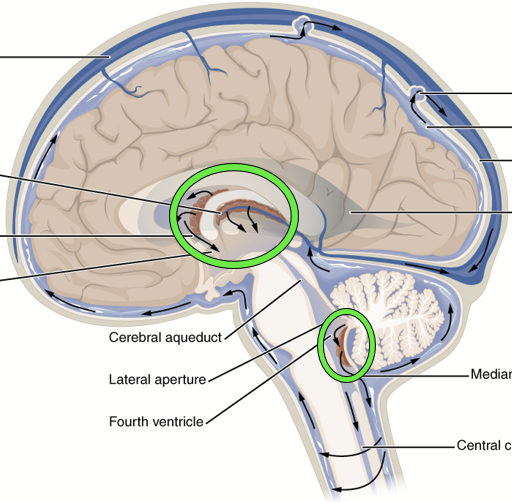
arachnoid villus
Drainage system of the brain. “Pressure valves” that release extra fluid from the sub-arachnoid space into a collection pouch within the dura mater at the top of the brain called the venous sinus.
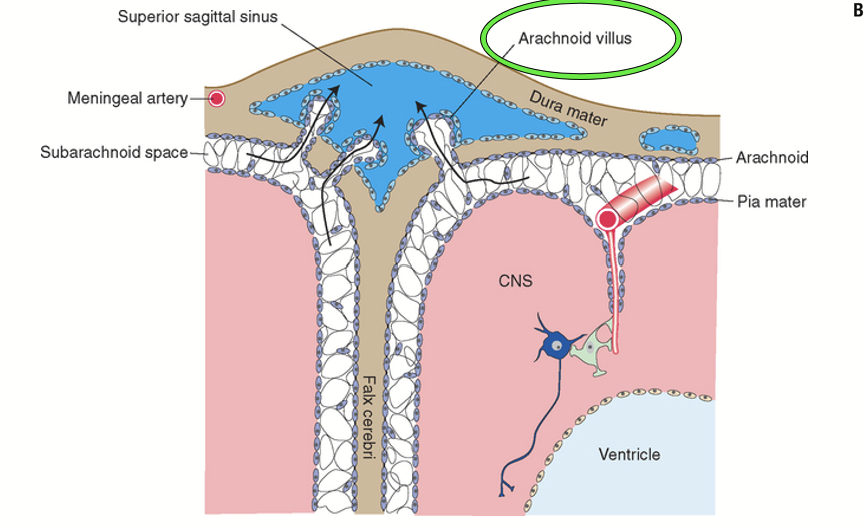
venous sinus
A “collection pouch” found within the dura mater at the top of the brain that collects excess CSF from the sub-arachnoid space released by the arachnoid villus.
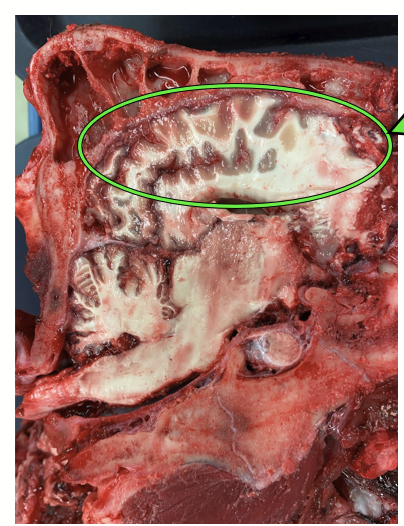
cerebrum
Left + right pairs, contains the cerebral cortex and the basal nuclei. The most superficial part of the brain and is involved in conscious control.
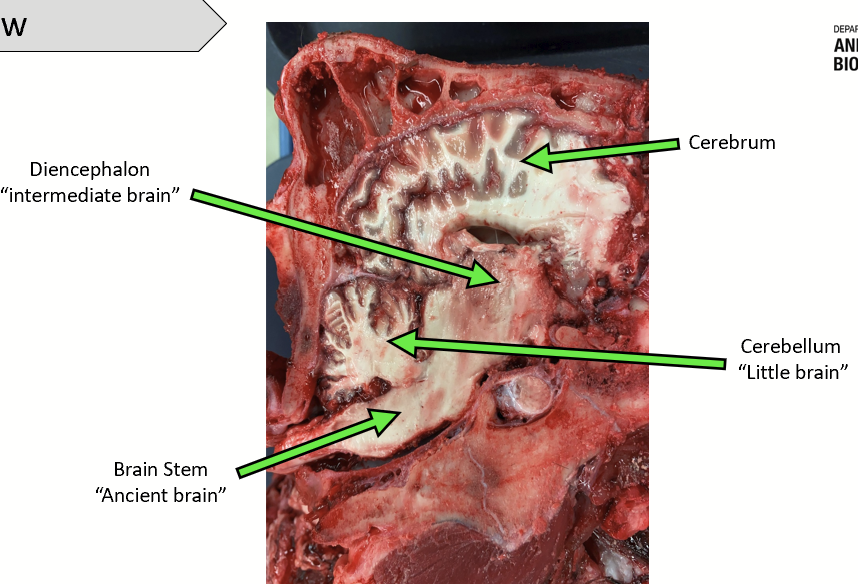
cerebellum
Not paired, looks like an “accessory brain”.
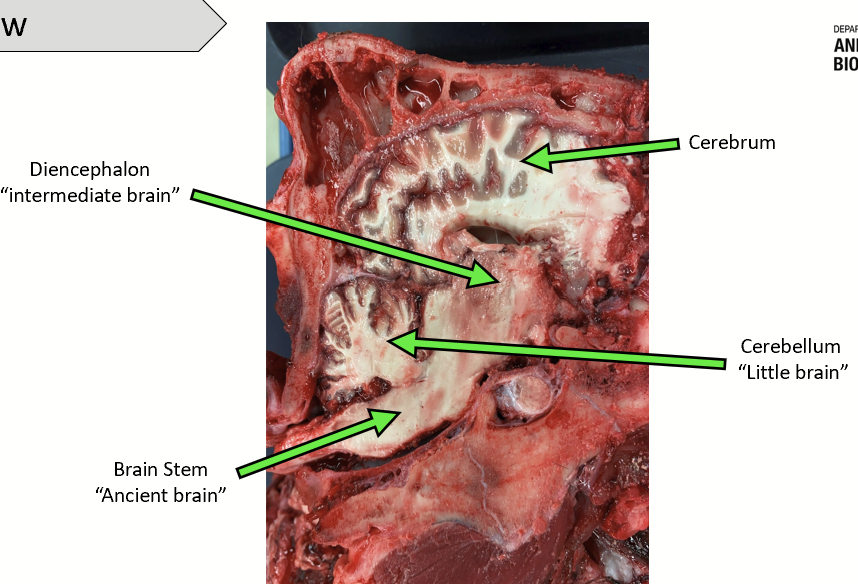
diencephalon
The mid-brain. Not paired. Composed of the epithalamus, thalamus, hypothalamus, and pituitary.
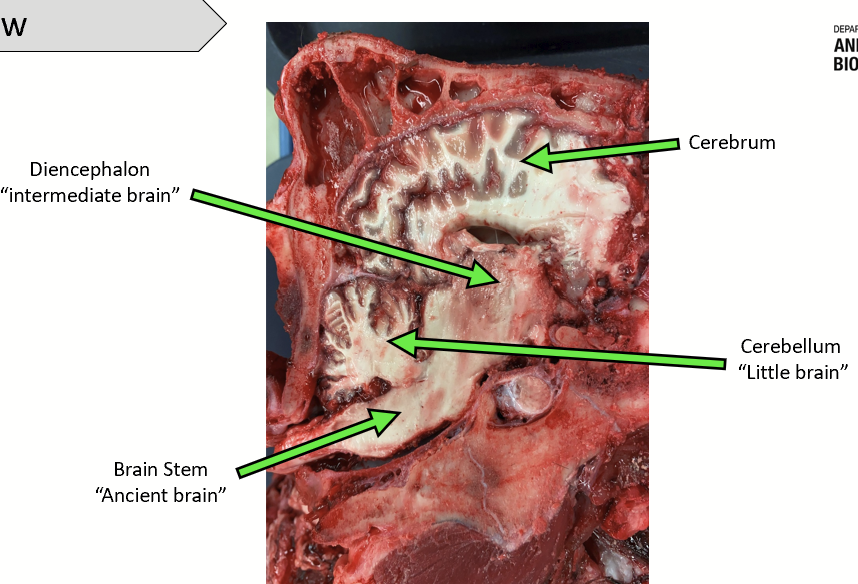
brain stem
The “ancient brain”. Not paired. Composed of the mesencephalon, pons, and medulla oblongata.
cerebral cortex
The most superficial layer of the brain, found in the cerebrum. Involved in the conscious treatment of sensory information and elaboration of complex conscious motor activity.
The site of a high level of association (communication between multiple parts) and educability (learning and memorizing).
Highly convoluted but corresponds to a single layer folded over and over to maximize use of space under the skull - if flat, would look like a pancake with gray layer on top and white layer underneath.
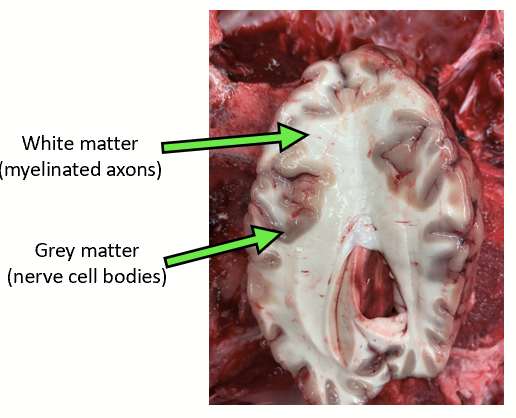
grey matter
Corresponds to nerve cell bodies. Found in cerebrum + spinal cord.
Where the integration of information occurs.
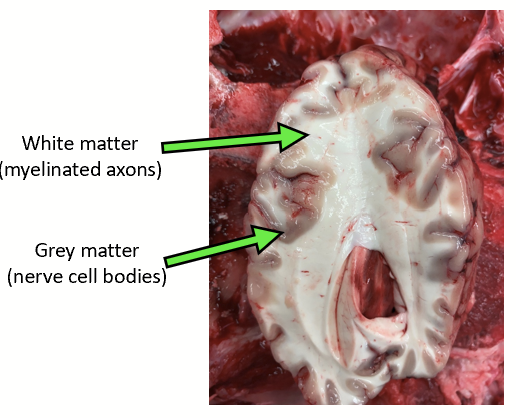
white matter
Corresponds to myelinated axons.
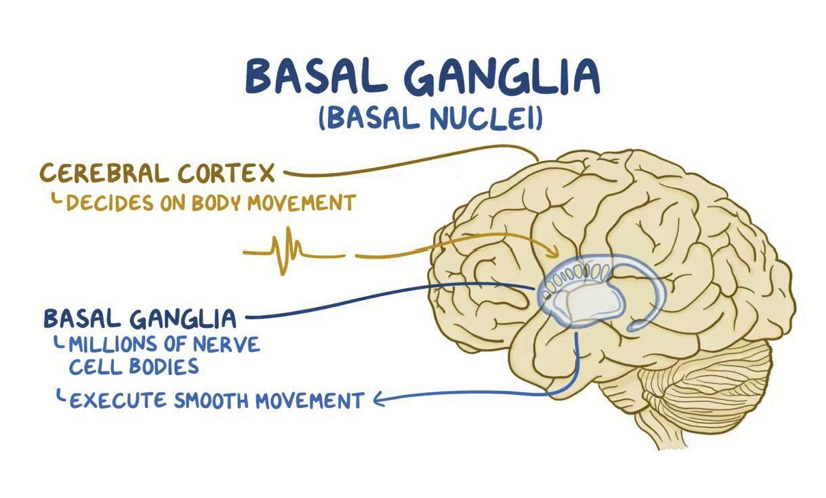
basal nuclei
Paired structures located under each cerebral cortex hemisphere. Responsible for semi-voluntary movement (e.g. walking, running, and jumping) which, although initiated consciously, rely on predefined (learned) sequences of muscle contractions.
Use information that feeds from the cerebral cortex and cerebellum.
epithalamus
Part of the diencephalon. Contains some of the olfactory correlation centers and it is more or less developed depending on species.
Also contains the pineal gland (endocrine gland), which produces melatonin.
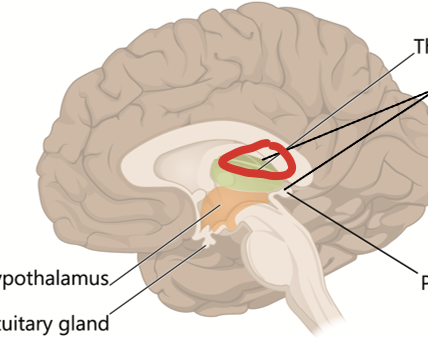
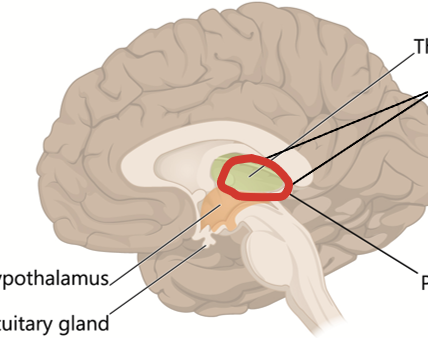
thalamus
Part of diencephalon. The key relay station for ALL sensory information which is then shared with the appropriate brain parts. It is a key link between the cerebrym (specifically the cortex and basal nuclei) and the cerebellum.
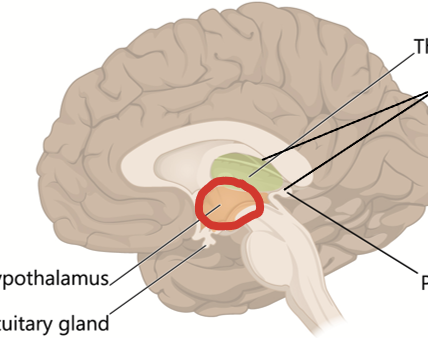
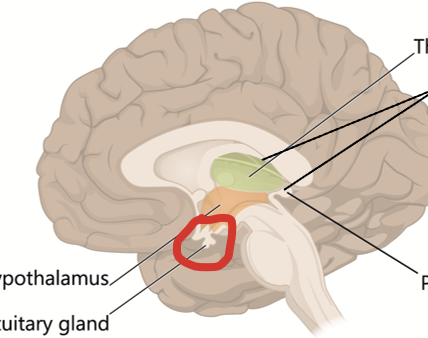
hypothalamus
Composed of multiple areas (or nuclei) with neurons organized for specific control functions. Key area where some homeostatic (such as thermoregulation) and body functions are controlled.
Of specific interest is the direct control over the pituitary gland thus regulating growth, metabolism, stress, and reproduction.
pituitary gland
Follows the pituitary stem. Located in a bony cavity (pituitary fossa in the sphenoid bone) at the base of the brain and is heavily vascularized.
Main function is to release hormones to mediate the brain control to target organs. Composed of two lobes: anterior (entirely endocrine) and posterior (corresponds to projections of hypothalamic neurons).
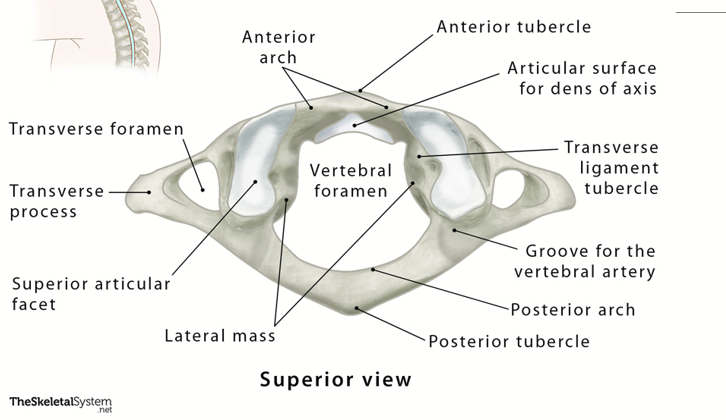
atlas (C1 vertebra)
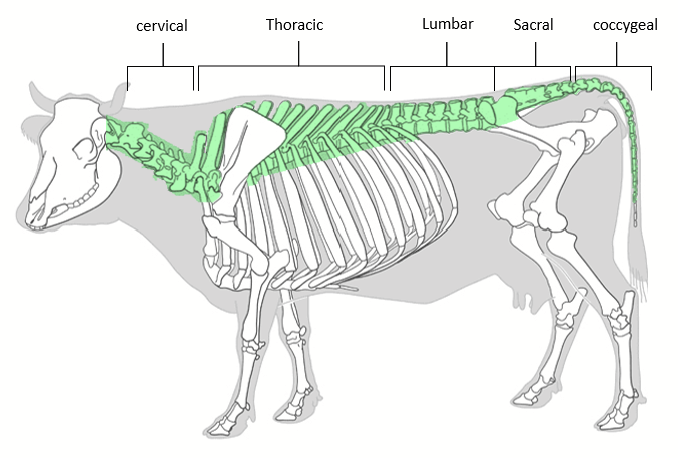
vertebral column
Set of individual bones that protect the spinal cord. Runs from the base of the skull to the end of the tail. Number of vertebrae vary amongst species.
Divided into five regions:
Cervical/neck
Thoracic/chest
Lumbar/lower back
Sacral or pelvis (vertebrae fused together to form the SACRUM)
Coccygeal/tail region (vertebrae fused together to form COCCYX)
vertebral flexibility
Vertebral column must allow for body movement.
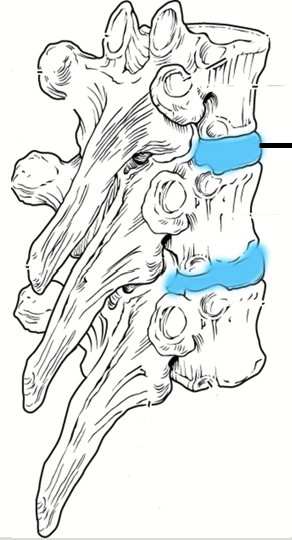
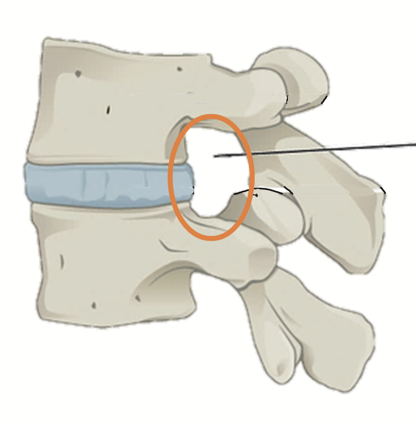
intervertebral discs
Found in between adjacent vertebrae. Composed of fibrous cartilage. Help form a slightly moveable joint, facilitate movement of the spine and acts as a cushion to absorb shocks from movements such as walking and running.
vertebrae
Each is comprised of:
A cylinder-shaped mass forming the ventral part, called the vertebral body (purple).
Processes: small bony projections on the transverse and dorsal sides (orange and blue).
A vertebral canal which contains the spinal cord (green).
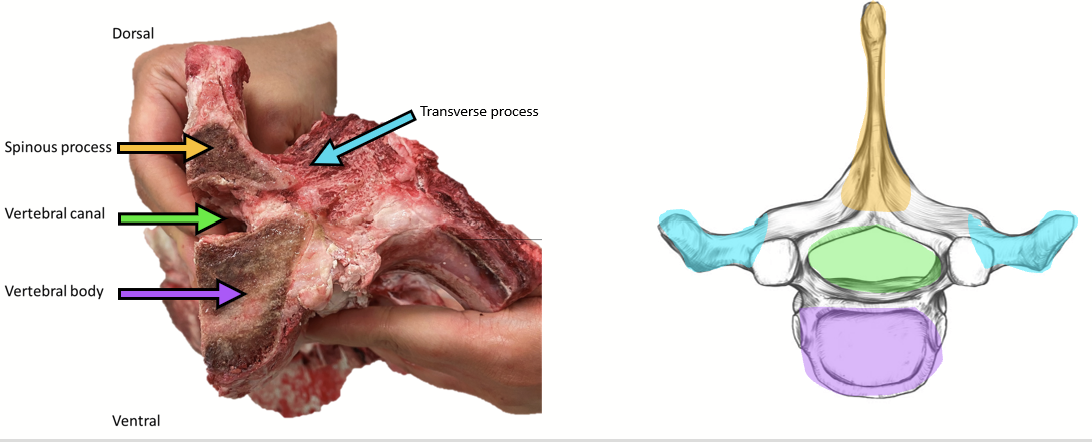
intervertebral foramen
In between each pair of vertebrae, where a pair of nerves (spinal nerves) exit and enter the spinal cord to innervate distinct sections of the body.
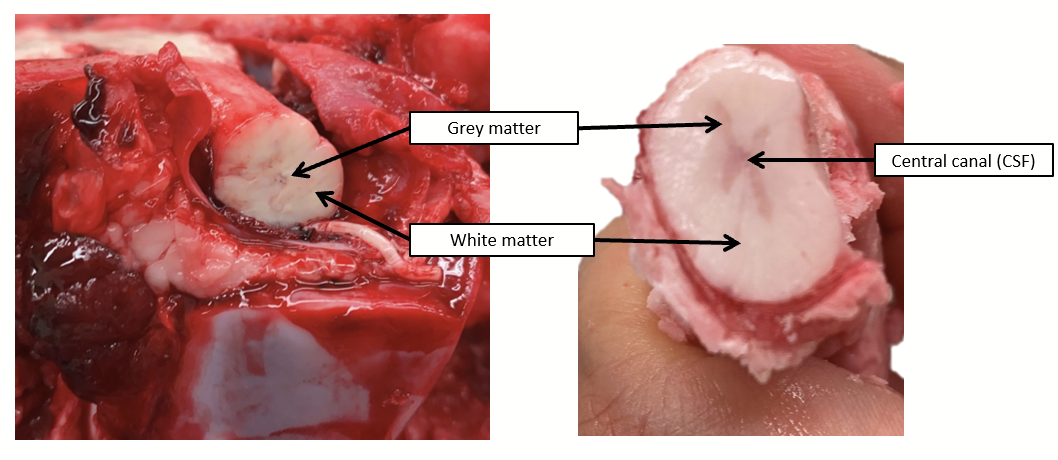
spinal cord
Its grey matter is found at the center of the cord, forming a butterfly shape on cross-section. Surrounding this core are the myelinated axons called white matter.
Part of the CNS, carries information to and from the brain by connecting to the PNS via spinal nerves.
Meninges project around the outside.
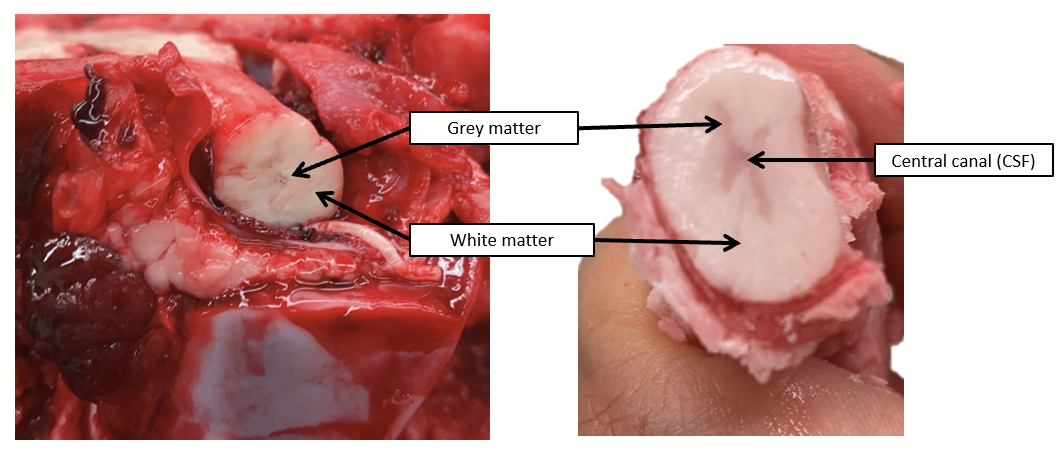
central canal
Located at the center of the spinal cord, where cerebrospinal fluid is found.
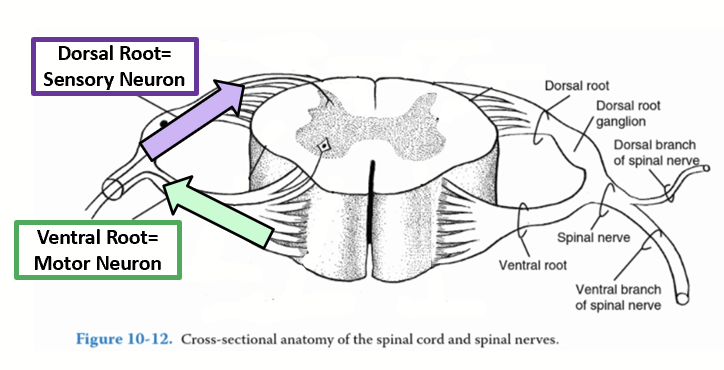
spinal nerves
Connect the CNS to the PNS. Each branches in a ventral and dorsal root carrying different information:
The SENSORY information (AFFERENT information) is carried FROM the PNS to the CNS and enters the spinal cord through the DORSAL root.
The MOTOR information (EFFERENT information) is carried OUT from the CNS to the PNS and exits the spinal cord via the VENTRAL root of the spinal nerve.
spinal taps / lumbar punctures
Collect cerebrospinal fluid from the sub-arachnoid space in the spinal cord.
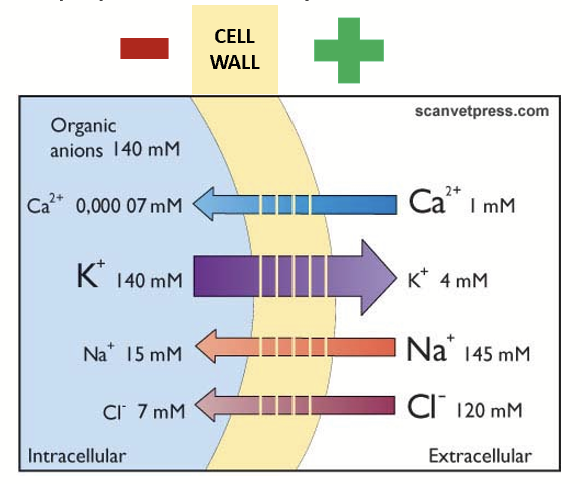
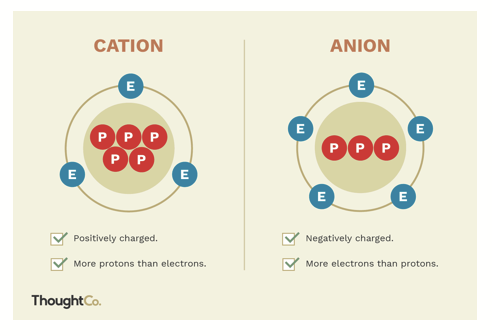
resting membrane potential (RMP)
Results from a difference in charge across the cell membrane (average = -70 to -90 mV).
To maintain:
Selective permeability (diffusion)
Ion pumps
Large anions trapped on the inner surface of the membrane
selective permeability (diffusion)
Passive leakage of ions through channels (via concentration gradient - PASSIVE). Resting membrane is permeable to K+ and barely permeable to Na+, Ca2+, and Cl- (therefore, positive charges accumulate outside → positive charge on outside of cell, negative charge on inside of cell).
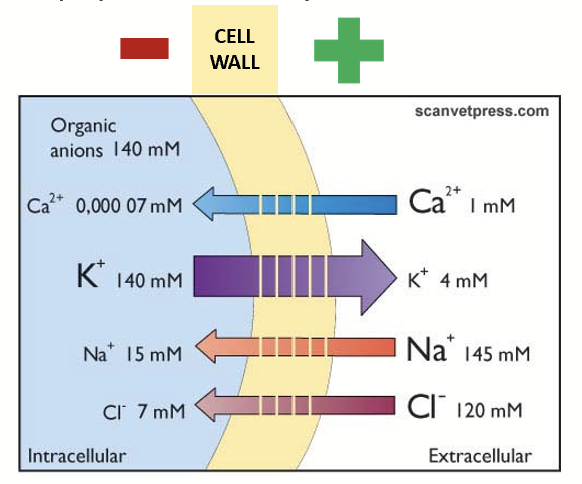
diffusion leak
Ions may move across the membrane, unbalancing the charge.
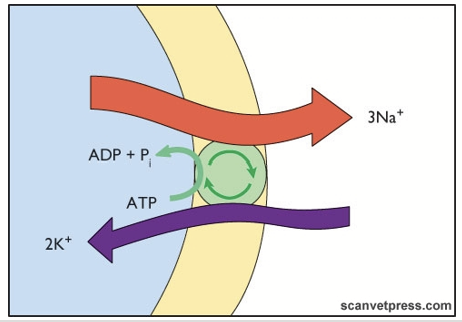
ion pumps
Concentration of ions remains relatively constant inside the cell. Compensates for diffusion leakage.
Na+/K+ pump: for every 3 Na+ pumped out, 2 K+ are brought in. Creates net positive on the outside by removing an ion from the inside.
Requires a lot of energy (ACTIVE PROCESS) - up to 40% of available ATP.
large anions trapped on the inner surface of the cell membrane
Organic anions mostly in proteins and amino acids. Found in higher concentrations inside the cell. Cannot pass through the membrane freely. Attracted to the outside positive charges.
excitable cells
Cells that can generate electrical impulses (action potentials). Can change their membrane polarity → use specialized ion channels with gates that open and close, in nerve cells the gate is controlled by voltage (voltage-gated ion channels). At rest, the gate is closed (needs stimulation to reach threshold, provoking the opening of the gate).
generation of action potentials in neurons
Depolarization
Repolarization
Hyperpolarization
Refractory Period
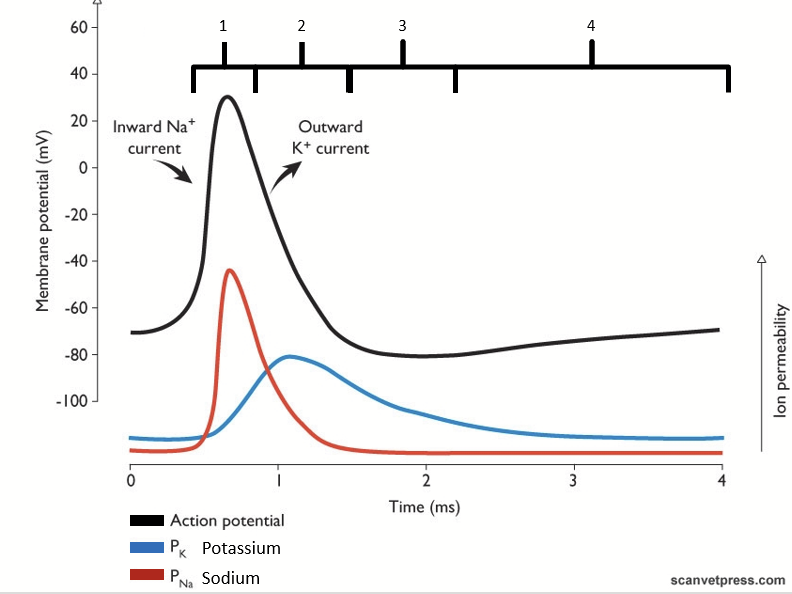
depolarization
Initial stimulation reaches threshold, provoking the opening of Na+ voltage-gated channels.
Influx of Na+ into the cell, increasing the membrane potential.
After ~0.5 ms, Na+ channels close rapidly.
repolarization
K+ voltage-gated channels open → outflow of K+ outside of the cell, bringing the membrane potential back down.
These channels are less coordinated and so they close slower.
hyperpolarization
Excess outflow of K+. K+ voltage-gated channels are slower to close, creating hyperpolarization of the membrane.
This process generates energy, however, there is now an imbalance of ions inside and outside of the cell.
refractory period
Resting membrane potential (RMP) restored through diffusion and Na+/K+ pumps. Neurons cannot be restimulated until restored.
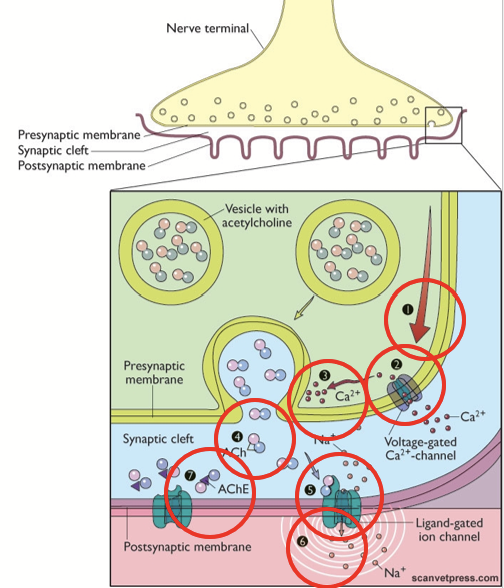
synaptic transmission
Continuation of signal between a neuron and the following cell (another neuron or target cell) as AP cannot be generated across multiple membranes.
neuronal junction
Transmission between two neurons.
neuromuscular synapse
Transmission between a neuron and skeletal muscle cell.
Synapse transmitter: Acetylcholine (ACh).
Post-synaptic folding is common to increase surface area.
neurotransmitter
Molecule responsible for passing the information in synaptic transmission. Converts the electrical signal (AP) into a chemical signal.
acetylcholine (ACh)
Neuromuscular synapse transmitter.
neuromuscular synapse mechanism of action
AP in pre-synaptic neuron
AP opens voltage-gated Ca2+ channels → influx of Ca2+
Ca2+ triggers exocytosis of Acetylcholine (ACh)
ACh diffusion in the cleft
ACh binds to specific receptors (ligand-gated ion channels)
Depolarization of post-synaptic cell
Na+ channels open, Na+ flows into the cell
Neurotransmitter inactivated (termination of signal)
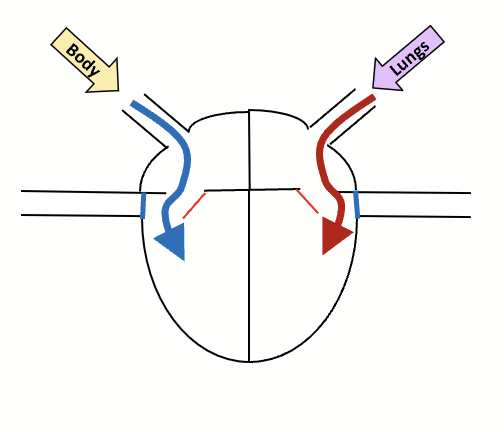
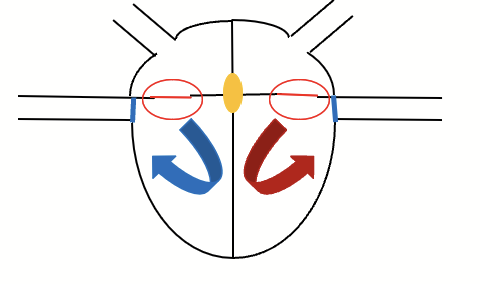
atria
Where blood is pumped into in the heart.
heart ventricles
Where blood is pumped out of the heart.
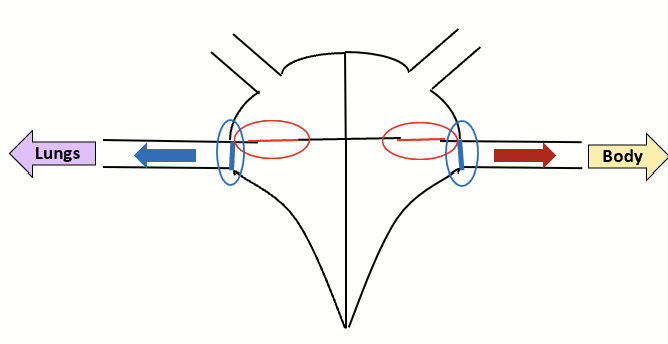
arteries
Blood vessels leaving the heart.
veins
Blood vessels arriving at the heart.
aorta
Major artery of the heart that takes blood to systemic circulation.
pulmonary artery
Major artery of the heart that takes blood to the lungs for oxygenation.
superior vena cava
Major vein of the heart bringing blood back to the heart from the upper body.
inferior vena cava
Major vein of the heart bringing blood back to the heart from the lower body.
pulmonary veins
Major veins of the heart that brings blood back to the heart from the lungs.
coronary arteries
How the blood receives oxygen and nutrients. Run around the outside of the heart.
pericardium
Layer of tissue that encapsulates the heart.
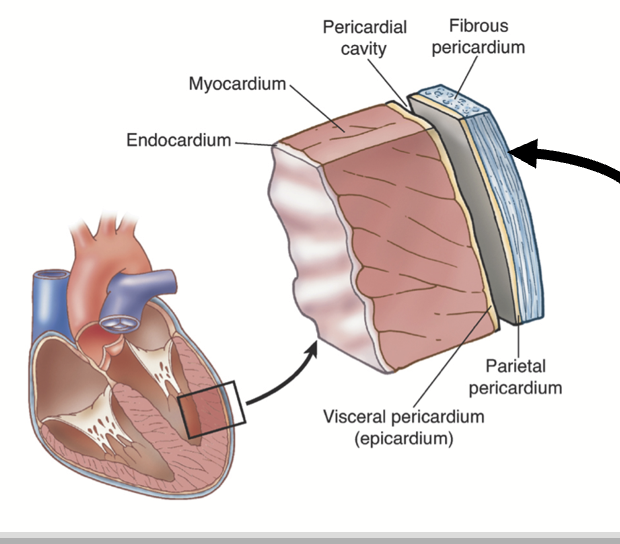
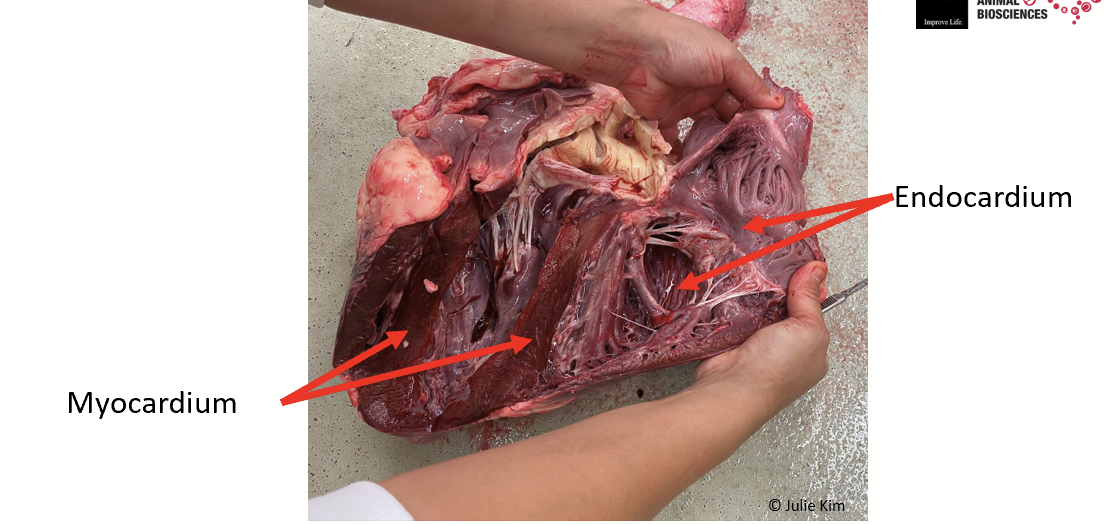
endocardium
Tissue that lines the inside of the heart chambers.
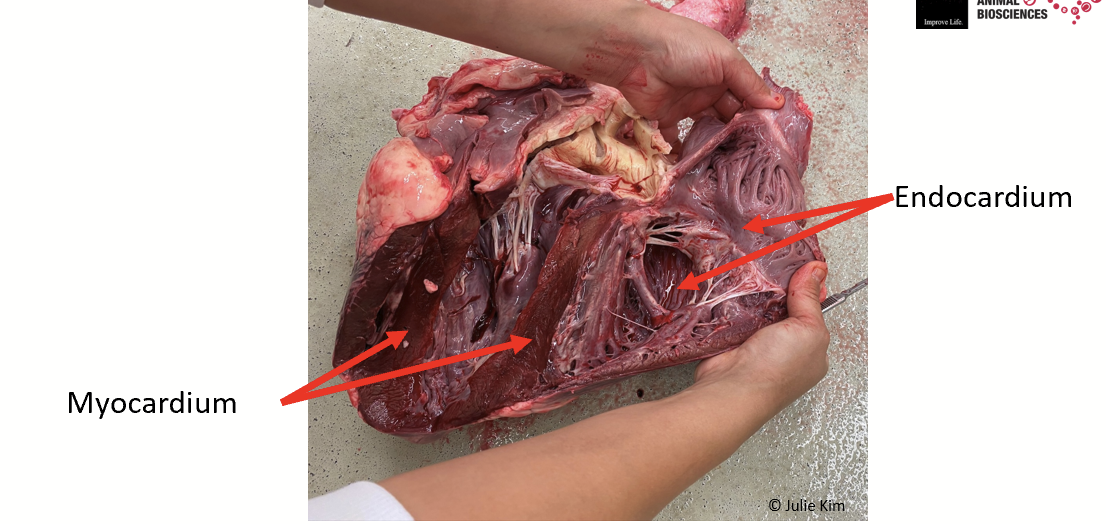
myocardium
Muscle of the heart. Myocardium is composed of 99% contractile cells that must be stimulated/excited to contract.
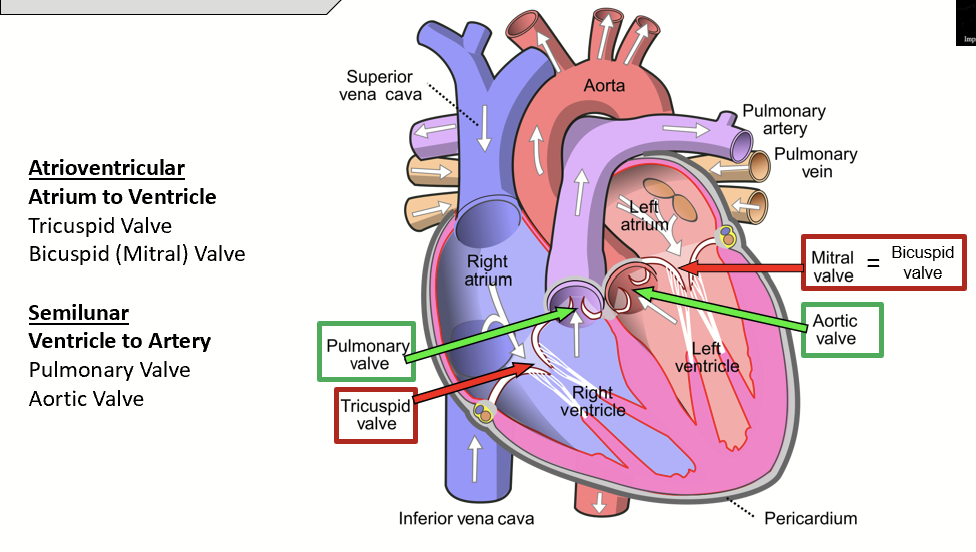
atrioventricular valves
Two valves that separate the atrium and the ventricles. Include the tricuspid and bicuspid valves.
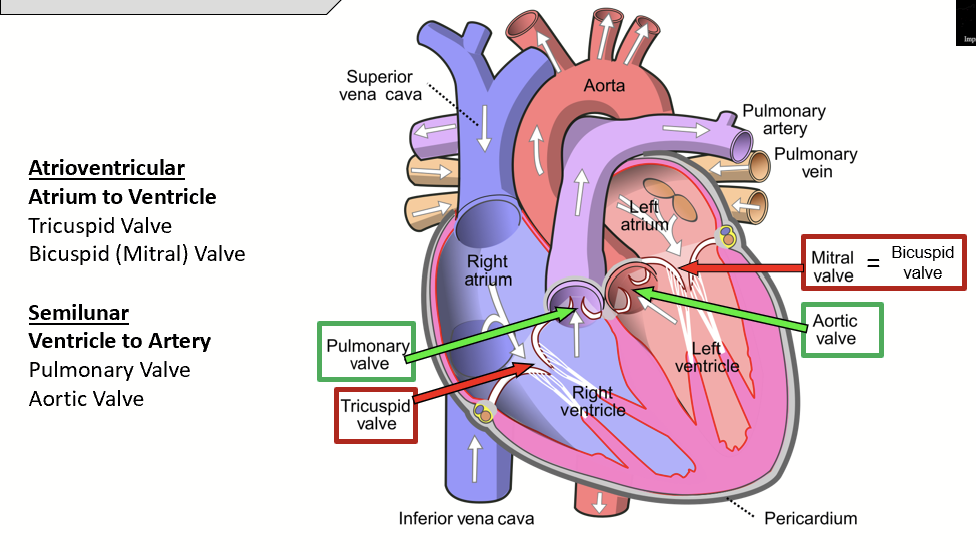
tricuspid valve
Atrioventricular valve that separates the right atrium and right ventricle. Made up of three flaps.
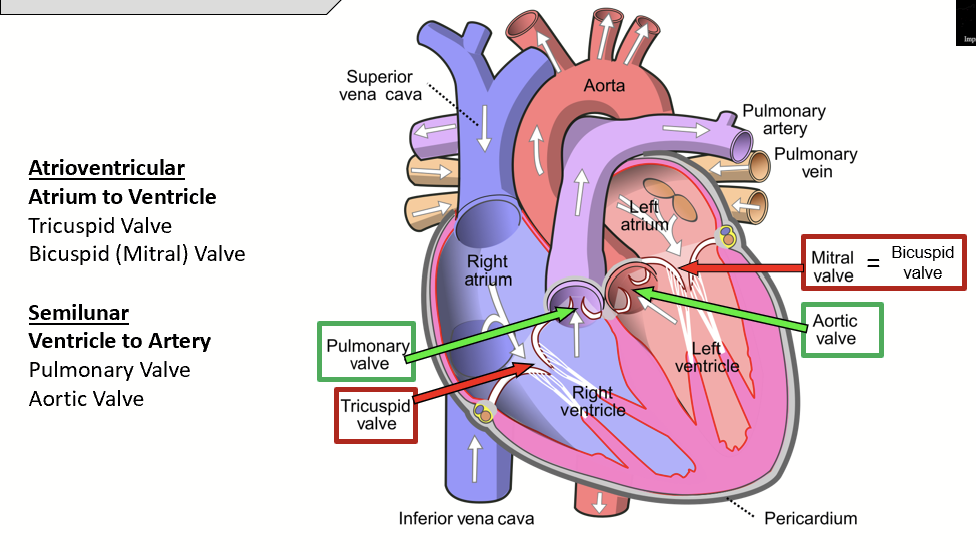
bicuspid valve (mitral valve)
Atrioventricular valve that separates the left atrium and the left ventricle. Made up of two flaps.
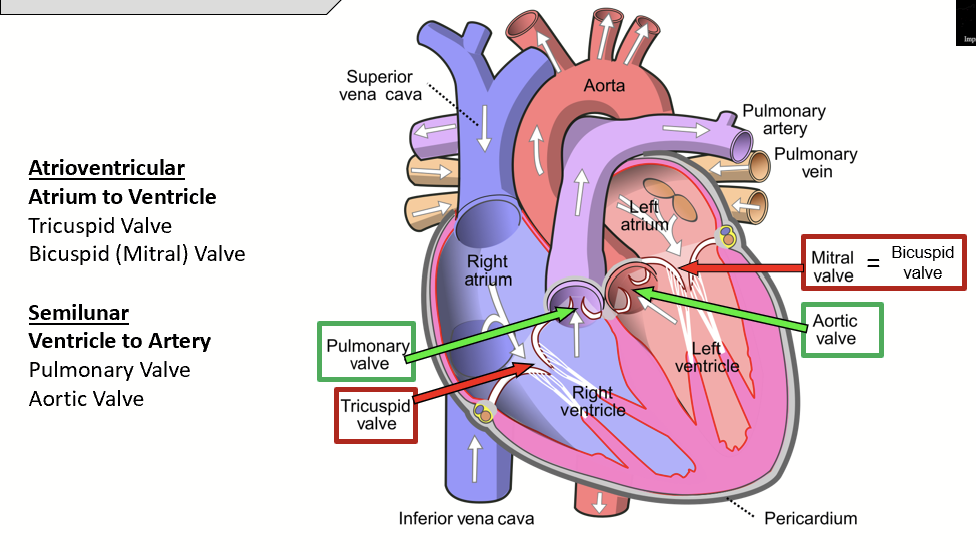
semilunar valves
Two valves that separate the ventricles and the arteries. Much thicker than the valves separating the atrium and the ventricle.
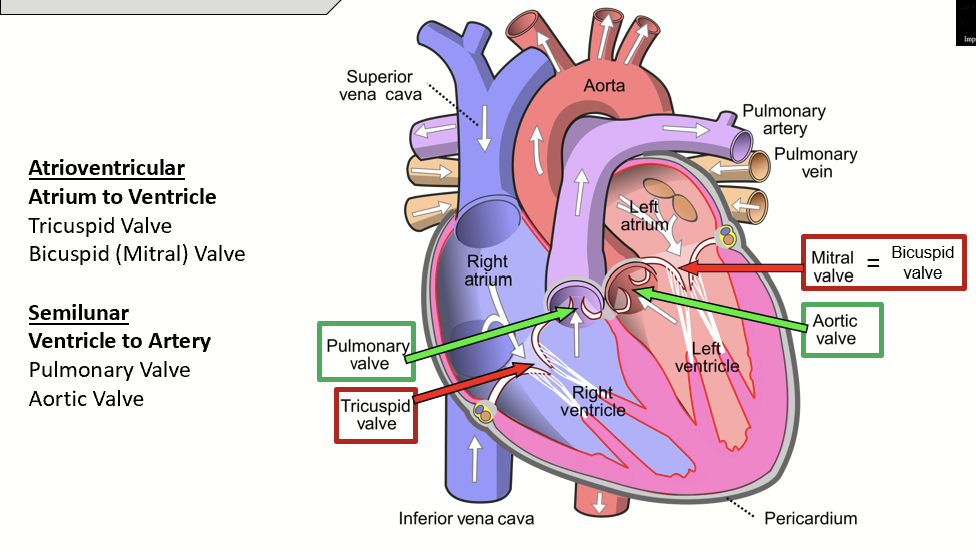
pulmonary valve
Semilunar valve that separates the right ventricle from the pulmonary artery.
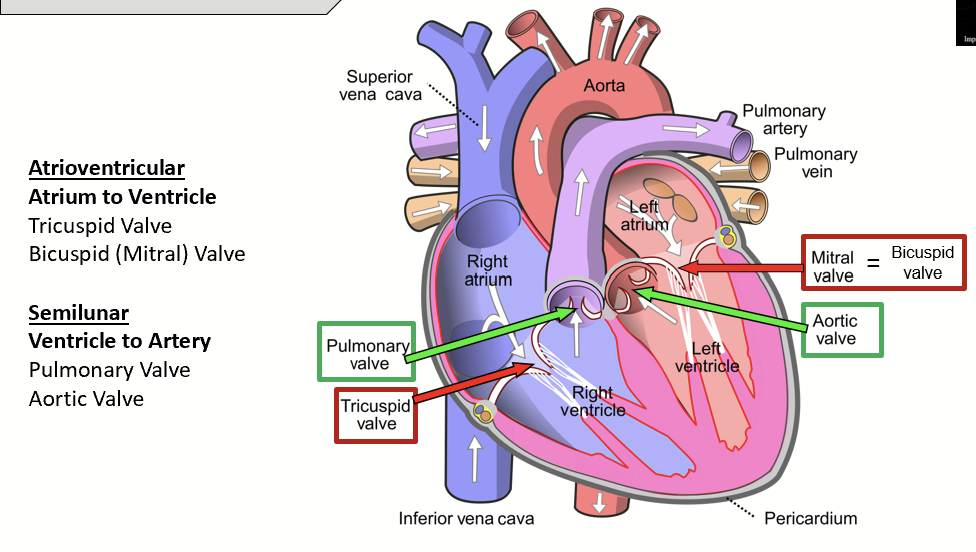
aortic valve
Semilunar valve that separates the left ventricle from the aorta.
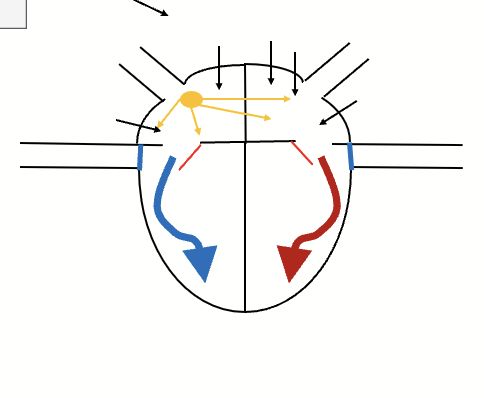
autorhythmic cells
Cells in the heart are connected with gap junctions, which allow electrical activity to jump from cell to cell without a synapse. Myocardium = 99% of contractile cells, which require stimulation.
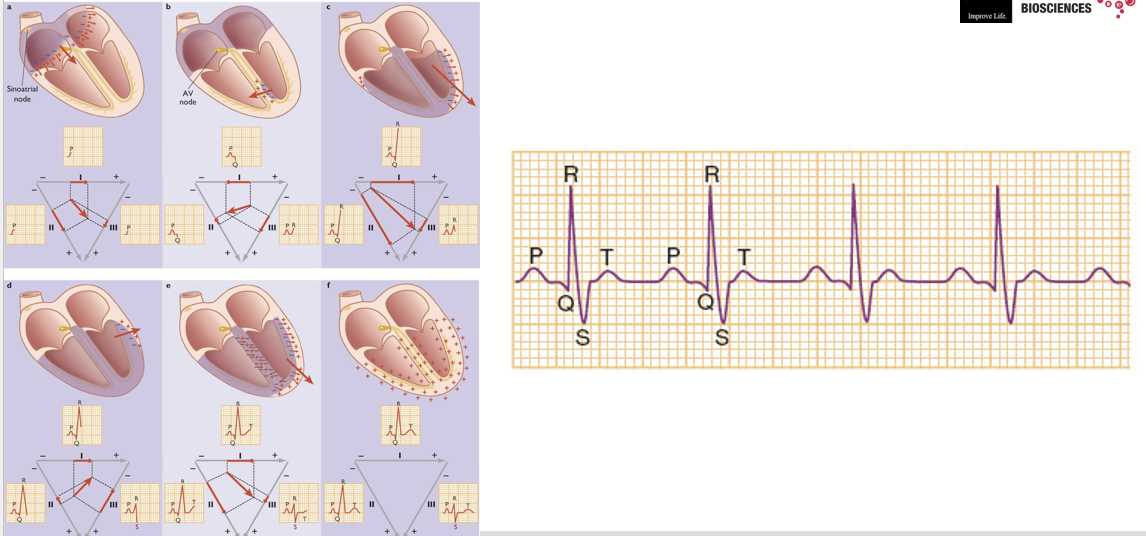
Cells that stimulate contraction provide initial rhythmic action potential (depolarization). Found in the autorhythmic structures (sinoatrial and atrioventricular nodes, Bundle of His, Purkinje fibers).
self-depolarization
Autorhythmic cells can self-depolarize without stimulation due to a drifting resting membrane potential (increase Na+ permeability and decreased K+ permeability) - SA node fastest, then AV node, bundle of His, Purkinje fibers.
SA node → contractile cells of atria → AV node → bundle of His → Purkinje fibers → stimulates contractile cells of ventricles (start at apex, moving upwards).
Insulation between atria and ventricles so AV node needed for transmission. AV node is slower, so lag between atria and ventricles.
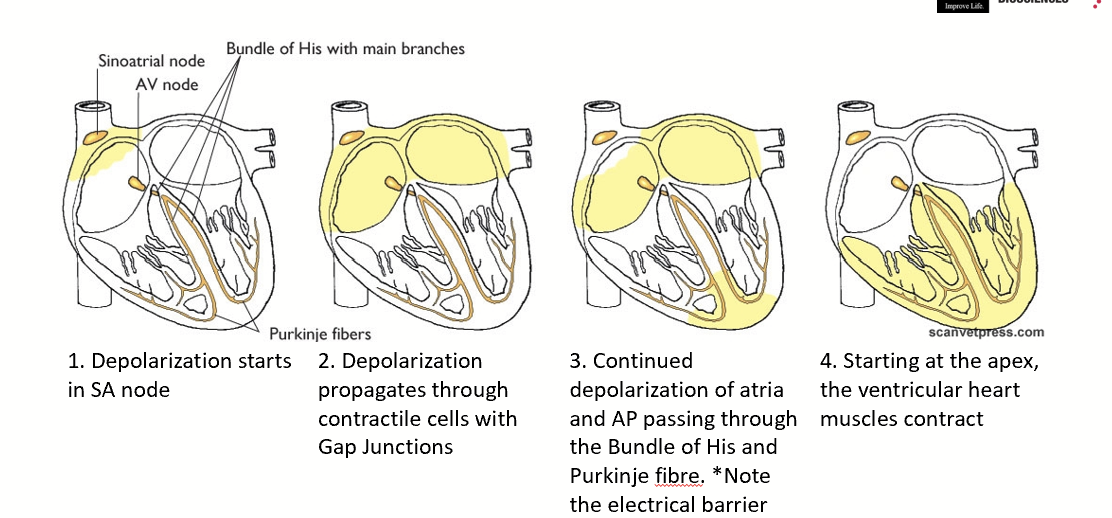
sinoatrial node (SA node)
Autorhythmic node in heart that dictates heart rate because it depolarizes the fastest.
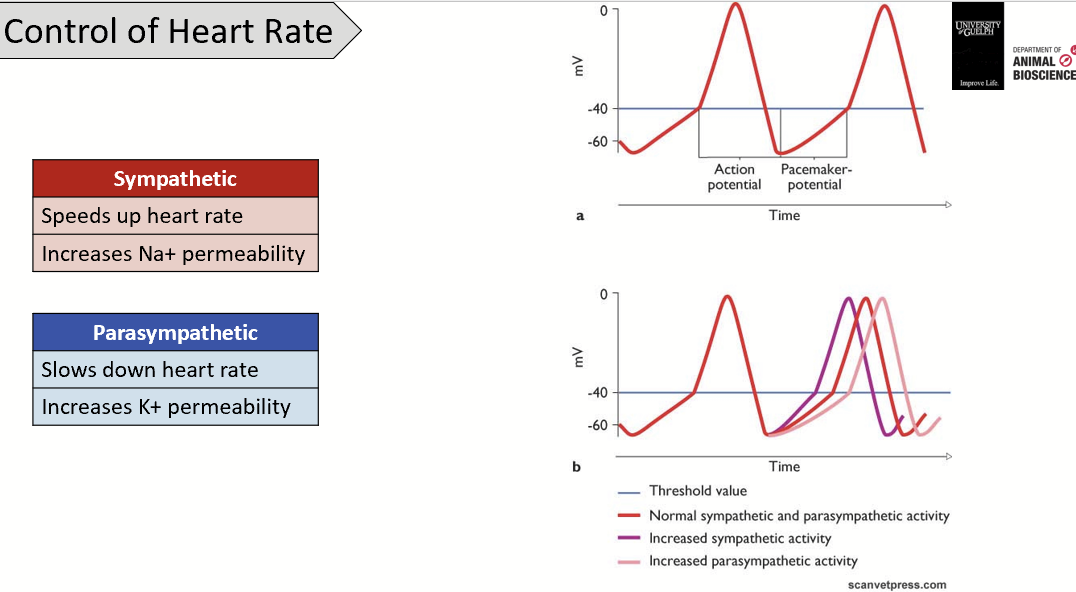
control of heart rate
Sympathetic activation will lead to increased heart rate (increased Na+ leakage shortening the potential drift).
To maintain coordination between atrial and ventricular contraction, the sympathetic input proportionally increases the velocity of the AV node (reduces lag in conduction).
Parasympathetic activation will lead to decreased heart rate (increase K+ permeability).
can the heart cramp?
The heart is made of cardiac muscle, which contracts involuntarily and rhythmically. Skeletal muscle cramps usually come from sudden, uncontrolled contractions due to electrolyte imbalance, fatigue, or nerve firing.
The heart has a built-in rhythm - heart’s contraction is driven by its autorhythmic system, not random nerve discharges like skeletal muscles.
The heart has a continuous blood supply (cardiac muscle has a very rich oxygen and nutrient supply to prevent fatigue under normal conditions).
Cramp occurs when there is an extra stimulation sent while the muscle is contracting - NOT POSSIBLE cardiac muscle due to prolonged refractory period.
refilling of the heart (diastole)
Heart is relaxed. Venous return fills the atria via vena cava. Pressure pushes the AV valves open. Blood flows in the ventricles. Not enough pressure to open the semilunar valves.
atrial contraction
SA node fires. Atrial contraction. Blood packed in ventricles through the AV valves which are pushed open. Pressure in ventricles not sufficient to force the semilunar valves open.
isovolumic contraction
AV node transmits the AP between the atria and ventricles with a lag. Atria finished contracting, ventricles waiting for the AP wave. Blood packed in ventricles, all valves are closed.
In between atrial and ventricular contraction.
ejection (systole)
AP passed on to the bundle of His and Purkinje fibers. Ventricles depolarize and contract. Pressure in ventricles increased, sufficient to force open the semilunar valves. Blood rushes out of the ventricles into arteries.
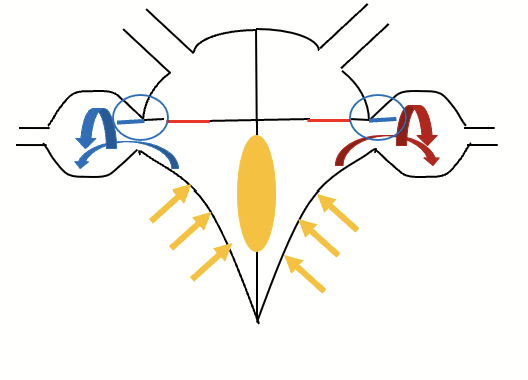
isovolumic relaxation
Contraction is over. Heart is empty. Low pressure throughout, all valves are closed. Blood starts accumulating in the atria.
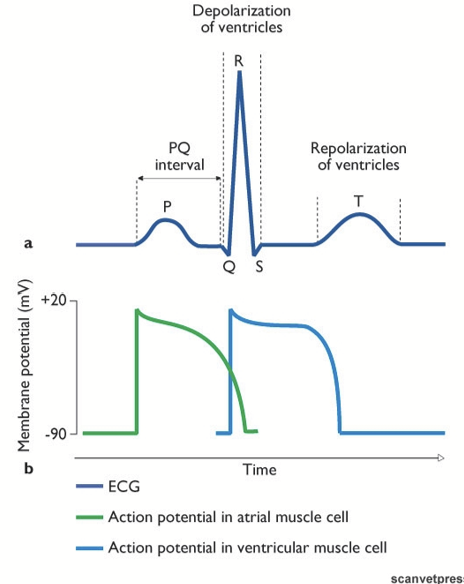
electrocardiogram (ECG)
Heart = large muscle with many cells depolarizing at the same time, creates an excessive amount of electrical current in the thoracic cavity that we are able to measure using electrodes strategically placed on the body..
Standard: electrode on each of front paws, one electrode on hind left paw. Most basic = two electrodes at base of heart, then at apex.
The resultant vector rotates as the depolarization wave progresses.
P wave
Atrial depolarization (when the atrial muscle is being stimulated).
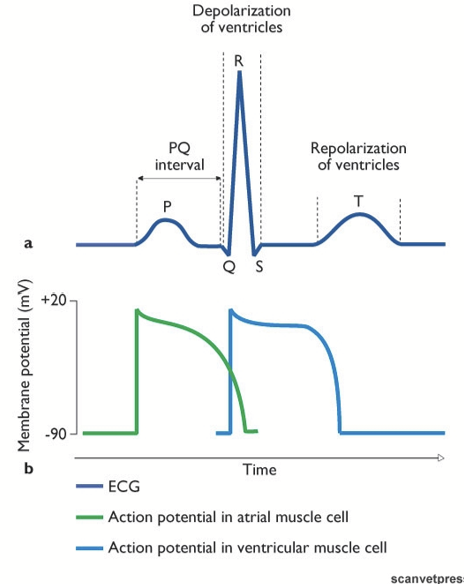
PQ interval
Time taken by the AP to pass through the AV node (lag time).
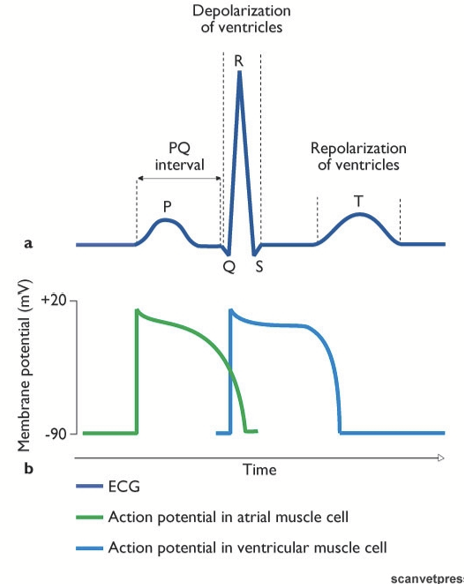
QRS peak
Ventricle depolarization (ventricular muscle stimulated).
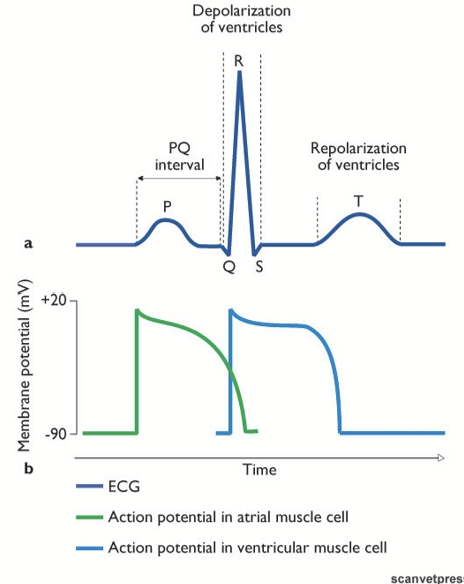
T wave
Ventricle repolarization after the blood has been pumped out of the heart.
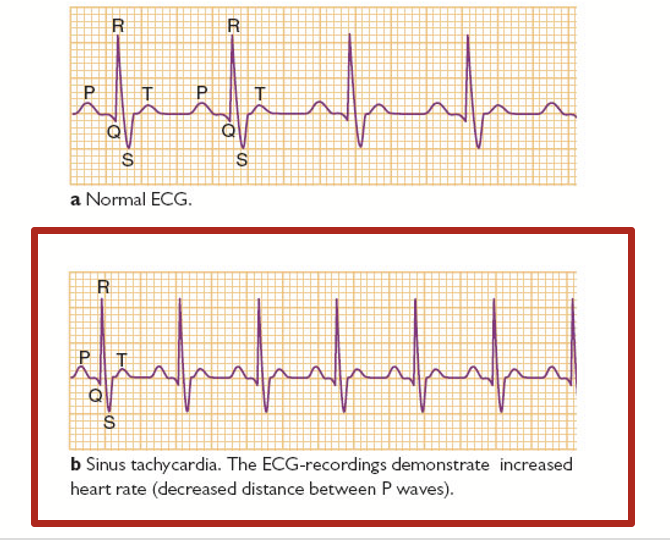
normal ECG
sinus tachycardia
Happens when the sinoatrial node sends impulses more quickly than normal. Can be triggered by exercise, caffeine, or stress.
Marked by decreased distance between P waves.
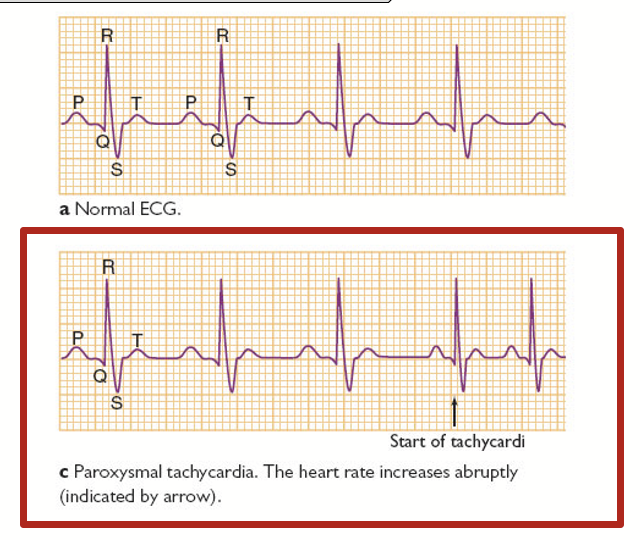
paroxysmal sypraventricular tachycardia
Occurs when a short circuit rhythm develops in the upper chamber of the heart. Heart rate increases abruptly.
→ a fit, attack, or sudden increase or recurrence of symptoms.
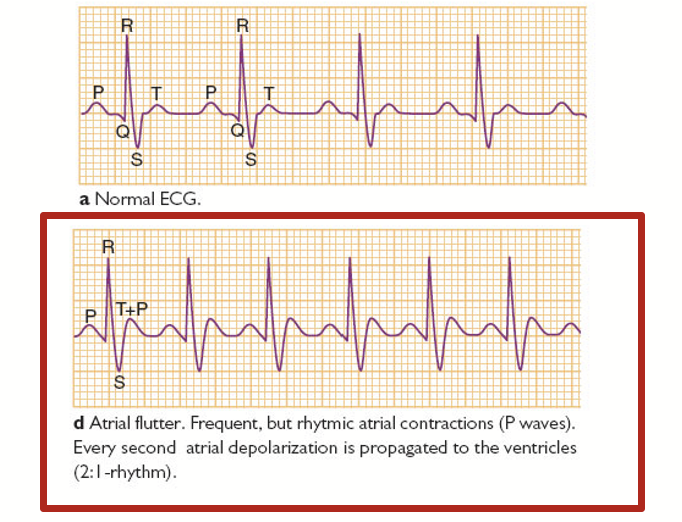
atrial flutter
Happens when a short circuit in the heart causes the upper chambers to pump very rapidly. Frequent, but rhythmic atrial contractions (P waves). Every second atrial depolarization is propagated to the ventricles.
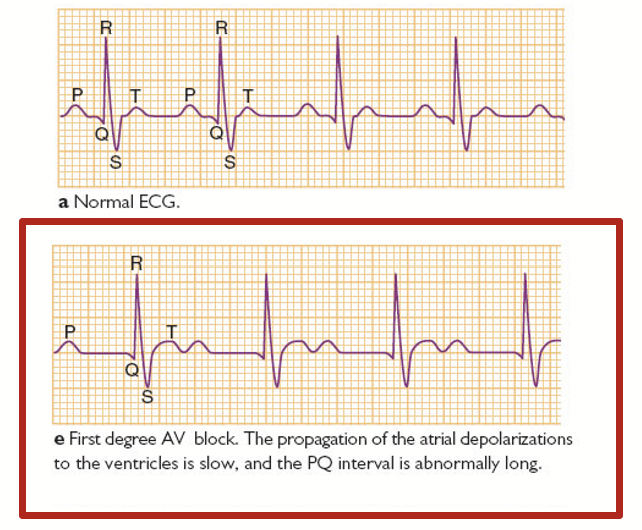
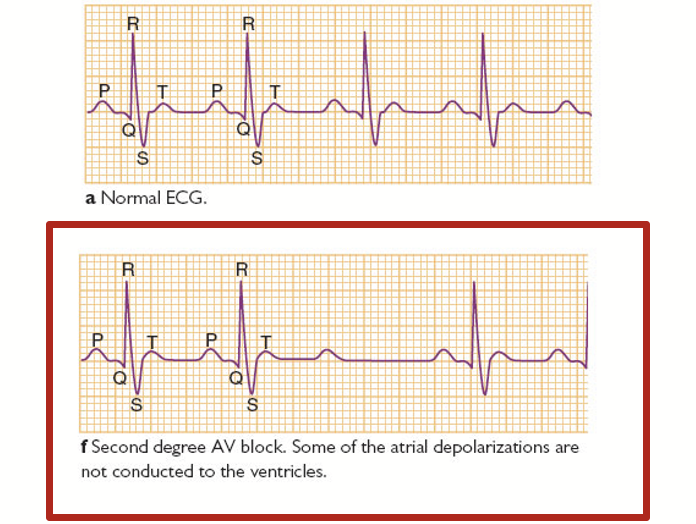
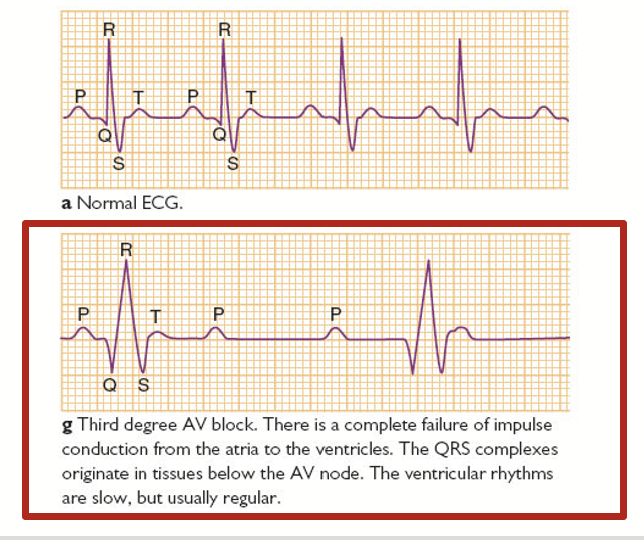
AV block
Malfunction of the AV node. Affects the PQ interval.
first degree AV block
Condition of abnormally slow conduction through the AV node. Generally asymptomatic and only discovered on routine ECG.
There is a dysfunctional of the heart where there is a long lag after atrial contraction. We can usually see an abnormally long gap between the P and Q waves here.
second degree AV block
A condition where signals between atria and ventricles can intermittently fail to conduct. Example: the QRS wave for ventricular contraction is missing (some of the atrial depolarizations are not conducted to the ventricles).
third degree AV block
A condition where the signals do not go from the atria to the ventricles. No connection between the parts of the heart, no electrical conduction.
In this case, an animal would not be able to survive this type of heart dysfunction. In humans, technology has reached a point where we can use pacemakers to synchronize the electrical conduction in the heart.
Ventricular rhythms are slow, but usually regular.
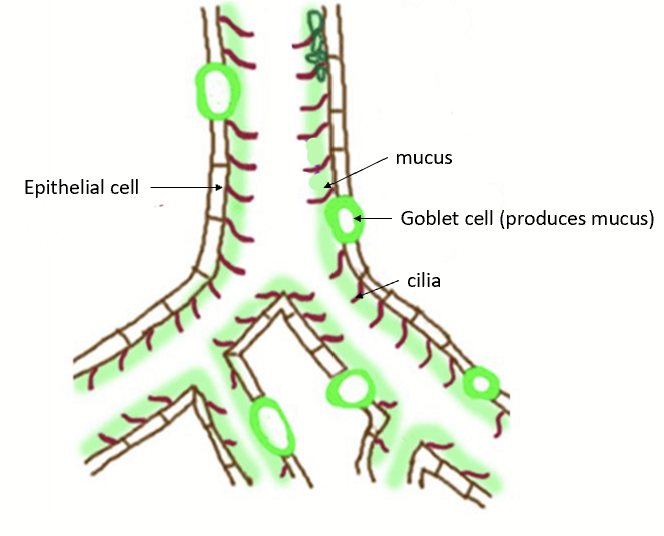
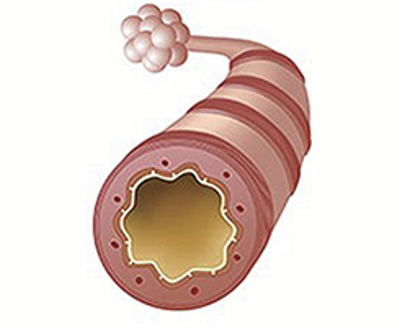
muco-ciliary escalator
The trachea and primary bronchi are lined by a layer of epithelial cells (goblet cells) that often have minute hair-like structures, called cilia, projecting from their surface.
These cells also secrete mucus that is continuously transported like an escalator in an upward direction (away from the lungs) by the coordinated movement of the cilia.
This process serves as an efficient filter for dust particles that attach to the walls, as the turbulent air flows in and out of the air passage.
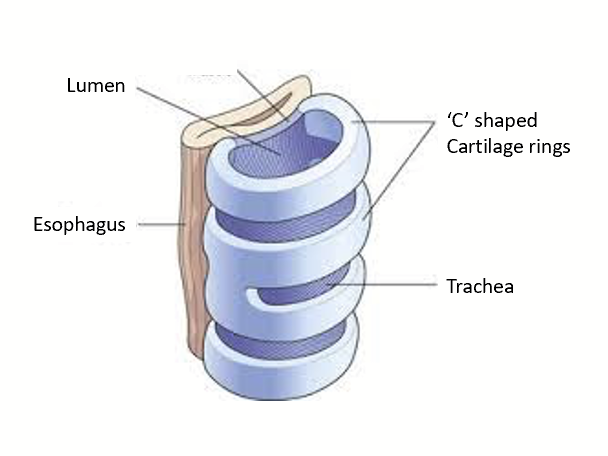
trachea
Primary function: deliver air to the respiratory zone for gas exchange.
Has full C-shaped cartilage rings (with an open part along the esophagus to allow food to move down), which allows for flexibility while preventing collapse. Cartilage is there to keep airways open when subjected to drastic pressure changes.
primary bronchi
The cartilage changes to plates as the imposed pressure difference slightly drops and, as we move deeper and deeper, the cartilage disappears.
bronchi
Embedded in the lung tissue and will rely on the lung’s recoil to remain open (you cannot collapse lungs under normal conditions, like a sponge).
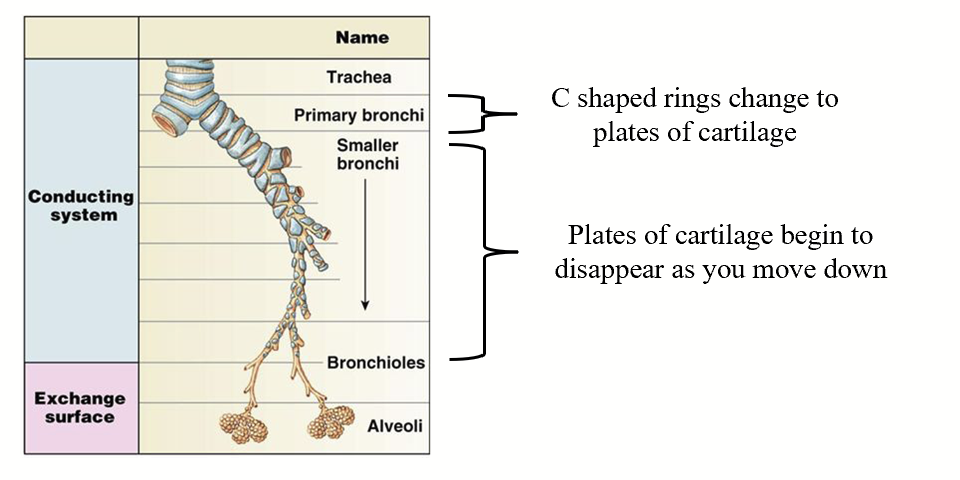
bronchioles
Made up of only smooth muscle and are the site of regulation. Depend on lung recoil to remain open.
With constriction, they reduce the diameter, increase the resistance, and therefore reduce the flow to the alveoli.
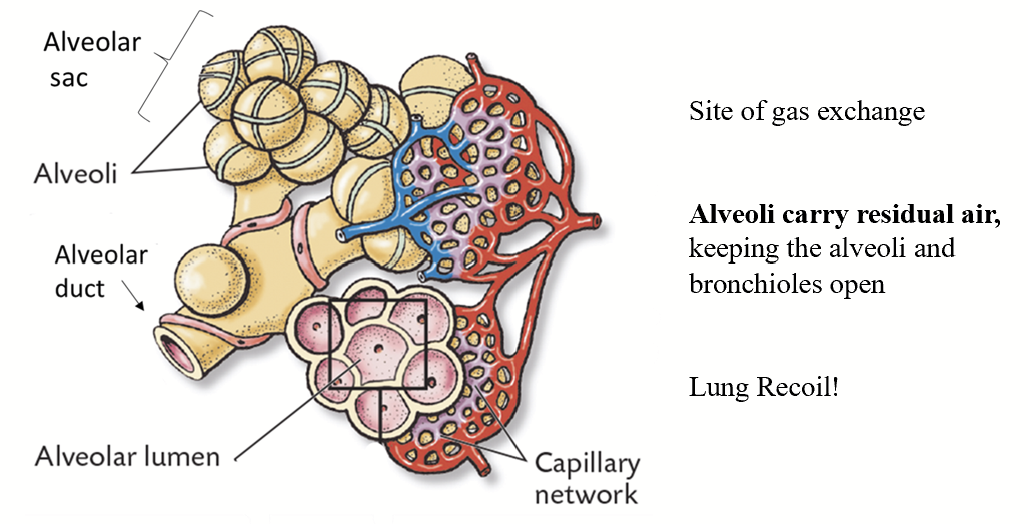
alveoli
The functional unit of the lung - site of gas exchange. They are VERY small - microscopic!
Look like a grape cluster made of a single layer of epithelial cells. Surrounded by a network of tiny blood vessels (capillaries). Carry residual air, which helps in the assistance to keep themselves and bronchioles open - lung recoil.
Oxygen-rich air in alveoli and capillaries that bring de-oxygenated blood to the alveolus → filtering, detoxification of blood.
Terminal bronchiole ends with alveolar duct.