Muscles and tendons
1/198
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
199 Terms
Describe the typical vasculature of muscles and tendons
Muscles: - generous blood supply (1+ arteries)
more than 1 artery is advantageous for metabolic demand (doesn’t reduce risk of damage if supply is interrupted)
Arteries branch in the perimysium and capillaries follow the endomysial sheaths of the individual fibres.
Veins are satellite (paired) to arteries.
When muscles contract it causes the vessels to be squeezed, if prolonged it can interrupt circulation
Tendons
poorly vascularised - advantage = no haemorrhaging
disadvantage = slow healing
what is it called where the artery meets the muscle tissue
anastomose
Describe the typical innervation of muscles and tendons.
Muscles:
motor neurones are found in ventral horns of grey matter of the spinal cord.
Reach the muscle in a single nerve
ramify within the fascia
variable ratio of motor to sensory fibres
tendons: aneural
what are the different kinds of muscle motor fibres?
Large alpha (supply main mass)
smaller gamma (supply modified muscle cells w/in muscle spindles)
non-myelinated vasomotor fibres (supply blood vessels)
sensory fibres (supple spindles, tendon organs and other receptors)
What do muscles do when activated, what happens to tension?
try to shorten
tension will increase/decrease/stay the same depending on external forces
what is meant by isometric activity
if the muscle can’t shorten, tension increases e.g. trying to move a static object such as a wall
examples:
Yielding - contraction opposed by resistance e.g. holding a weight steady at arms length
Overcoming = muscle contraction opposed by an immovable object e.g. pushing against a wall
What role do muscles and joints play in locomotion?
muscles attach to fulcra (joints)
joints act as levers
position of muscles around a joint affect suitability for starting/completing movement
what is meant by actively insufficient muscles
muscles that are incapable of resulting in a full range of movement over more than one joint that they’re spread over
can’t fully shorten
Outline the muscles and their roles in lifting the dogs head
Sternocephalicus - moves head up and down, side to side
Rhomboideus muscle - lifts neck (draws scapula up, backward and forward)
brachiocephalicus - pulls leg forwards, neck and head down and to one side
Omotransverarius muscle - moves limb forwards and neck to the side
Splenius muscle - move head backwards and forwards
Why are the main muscle groups in the proximal limb rather than the distal limb
decreases overall muscle mass enabling a higher capacity for both force and power
a small movement of the upper limb will result in a large movement of the lower limb (less effort needed to move the whole limb?)
What is meant by an antagonistic pair, give an example
One muscle acts as an agonist/prime mover producing a certain effect
The other muscle is an antagonist - opposes the movement of the agonist.
brachialis and triceps brachii (extend and contract the elbow).
what is meant by a synergist muscle
a muscle that may modify the action of the agonist but not directly be agonistic/antagonistic.
what is meant by a fixator
a muscle that stabilises a joint.
Often involves co-contraction of muscles that oppose each other when the joint moves
what does ‘origin’ mean
a proximal/central attachment
what does insertion mean
denotes a more distal/peripheral attachment
What is the action of epaxial muscles
extension of the vertebral column
what is the function of the hypaxial muscles
flexion of the neck and tail
what is the function of the sternocephalicus
flexion of the neck
what are the functions of the supraspinatus, infraspinatus and subscapularis
initiates the movement of the arms away from the body
externally rotate the humerus
internal rotation of the humerus and shoulder joint
what is the function of the triceps brachii
extension of the forearm at the elbow
what is the function of the biceps brachii
contraction of the forearm at the elbow
what is the function and location of the extensors of the carpus and digit
in the forelimb
extension of the carpus and digit
what is the function of the flexors of the carpus and digit
contraction of the wrist and fingers (carpus and digit)
what are the functions of the gluteal muscles
hip extension, abduction and rotation
what are the functions of the semimembranous and semitendinosus
extension of the hip and knee
assists the popliteus muscle rotating the leg internally
what is the function of the quadriceps femoris
moves the femur cranially and caudally
what is the function of the extensors of the tarsus
extension of the tarsus
what’s the role of the flexors of the tarsus
flexion of the tarsus
what is the role of the flexors of the digits
flexion of digits
what is meant by isotonic contraction
if an animal is able to move an object, the activated muscles will shorten as they develop force
what kinds of isotonic contraction are there
Isotonic = same force
Eccentric = muscle lengthens e.g. breaking down a steep slope, the horse extends its forelimbs to slow itself down
Concentric = muscle shortens e.g. bicep curl/tugging in dogs.
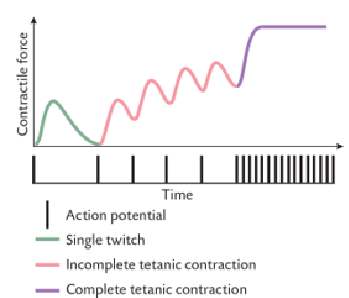
Explain what is meant by tetanic contraction
A series of rapid succession action potentials that result in persistent contraction of the muscle fibres
AP lasts 1-2ms, causing a twitch once twitch subsides a new AP is generated
If AP intervals are shorter than the duration of a single twitch, fibre remains contracted (sustained constant force) = Complete Tetanic contraction
incomplete tetanic contraction = partly fused contractile force fluctuates at same fq as APs
maximum contraction = Ca ion concentration i cytosol is maintained above level required to unlock all actin binding sites
maximum force = 3 - 5x higher than during a single twitch (Ca ion level is higher)
what must happen before the muscle can develop external force?
the elastic elements must be taut
single contraction is too brief for complete tautening
why is it important to routinely vaccinate horses against tetanus (MSK relevance)
What does tetanus do?
releases toxins that block the neural pathway from spine to muscles
disrupts nervous system and causes spasms = pathological tetanic contractions
high mortality - spasms in any muscle, affect digestion, walking, breathing etc.
Why vaccinate?
weakens tetanus
results in a faster immune response
horses are at high risk due to environment
horses are more sensitive to this disease
Cause:
clostridium tetani
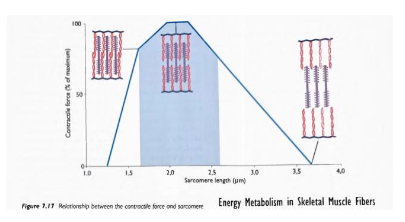
Explain the relationship between contractile force and sarcomere length
Overstretched muscle: - reduces overlap of myosin and actin, resulting in less contraction and less force produced. (tendons that attach muscles to bone help reduce the risk of this)
Too short muscles: - actin and myosin overlap too much preventing myosin binding to actin (may occur post injury if muscle isn’t used)
What is muscle power output
Work per unit of time
product of velocity and muscle shortening and external load
Why is power output as a function of the external load an inverted U-shape?
when external load requires less than the maximum contractile force the power output will be generated
Power output will increase with external load until max optimum output is reached (when load is about 1/3 of max contractile force)
If the external load continues to increase, the power output will decrease due to fatigue
How can you use the relationship between power output and external load to your advantage?
the larger the animal’s mass, the greater the power output needed to move the animal (independent of external load)
There’s an optimal muscle mass that enables optimum power output (load should be around 1/3 of max contractile force)
Important to consider for certain animals e.g. race horses - they’re trained for max optimum power output with a specific weight of jockey.
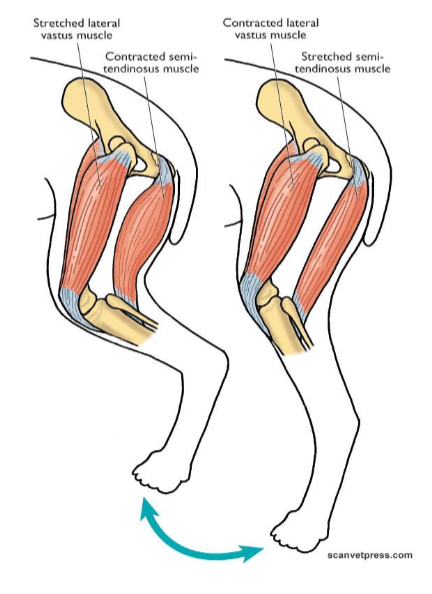
Describe the interaction of muscle, tendon and bones in the movement of the limb e.g. stifle joint
work in antagonistic pairs
In the stifle joint:
semi-tendinous muscle contracts so the lateral vastus stretches to bend the hind leg at the stifle (opposite to straighten the leg). Must be in pairs to stretch as it requires contraction
When muscle shortens, attachment points of tendons move together to move the bones
Semi-tendinous muscle is connected to the tibia by pes anserinus tendon.
Quadriceps tendon connects the lateral vastus muscle to tibial tuberosity
Origin moves the least, insertion moves the most.
What is a musculoskeletal exam?
A thorough and systematic physical examination of the MSK system that includes:
taking a history
static evaluation
dynamic evaluation
diagnostics
what is meant by a static and dynamic evaluation?
Static = assessment of the animal at rest
Dynamic = assessment of the animal in motion
what are the principles of equine MSK examination
For it to be adequate:
horse must be safe to handle and appropriately restrained
shod/have appropriately trimmed feet for a dynamic exam
Area:
quiet, away from other people/horses/traffic
flat, even, non-slippy surface, ideally a hard and soft area for lunging
Before starting:
detailed history (NO POSSIBLE TRAUMA/FRACTURE (can lead to catastrophic injury))
if in doubt do a fully physical exam first
don’t trot if clearly severely lame/obvious injury
What does a static exam involve (outline)
Assess:
conformation
hoof conformation and balance
muscle development and symmetry (back and pelvis)
palpation
joint range of motion
palpation of limbs when weight bearing/non-weight bearing
What do we palpate in a horse
Forelimb: Shoulder, elbow and antebrachium, carpus
Distal foreblimb: Extensor and flexor tendons, metacarpophalangeal (fetlock) joint, proximal interphalangeal (pastern) joint and distal interphalangeal (coffin) joint
Foot: Hoof, frog, sole, white line (can use hoof testers)
Hind limbs: pelvis and coxofemoral joint, stifle, tarsal
Distal hindlimb: same as forelimb, except metatarsophalangeal joint instead.
Outline what’s involved in a dynamic exam
walking and trotting in straight lines in hand
lunging
ridden?
How do we test the flexing of the joints of the distal limb
start with the distal limb and work up the leg (for testing all joints)
looking at the 3 distal joints - fetlock, pastern and coffin
apply pressure just above the fetlock (so rest of leg doesn’t affect it), and bring the toe up as far as you can
hold for 30-60s, should get the heel bulb back onto the fetlock.
greater flexion in hindlimb
How do we do a flexion test of hock and stifle
these two joints work together called reciprocal apparatus, linked so flex and extend together - peroneus tertius muscle
Bend knees and straighten back, bring up gently so the horse gets used to it, want to get the metatarsus parallel to the ground, fetlock tends to have some flexion (hold just above)
should be able to get a degree of lateral movement, caused by the ball and socket joint of the hip
hold for 30-60s part of a lameness exam/vetting
How do we flexion test the carpal, elbow and upper forelimb?
carpus separately:
let distal limb hang loose, bring metacarpus up as close as possible to radius and ulna, should be able to bring them together completely (no gap_
Elbow and upper forelimb:
Let lower limb hang as loosely as possible
bring up in front of the horse
should be able to get the radius parallel
do gradually (tend to not enjoy this as much)
What points of a horse are we looking at for conformation?
look for vertical lines through the centre of each joint, thus equal loading is present
unequal loading can predispose to injury
Look at:
different angles
Legs: fore and hind
Hip: tuber coxae
What does hoof conformation involve
Viewed from the front:
Medio-lateral balance (slope of medial and lateral walls is identical)
Viewed from the side:
hoof pastern angle should be ~45 degrees to the ground
ground hoof wall angle parallel at heed and toe
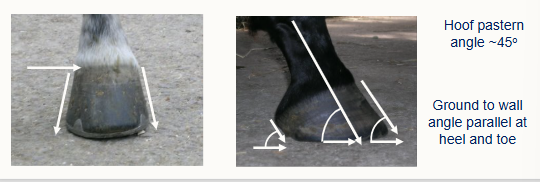
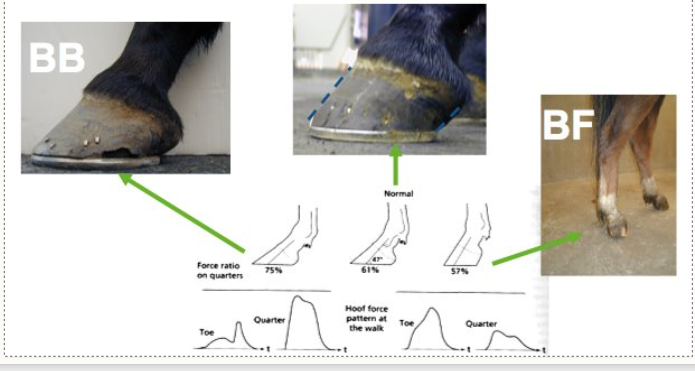
What is some terminology for hoof balance when it’s not quite right
broken back = BB
broken forward = BF
see image for what they look like
Outline the process of palpating a forelimb
Find scapula - cartilage, bridge and point (use finger pads and 4 flat fingers)
Find the humerus at the scapular point, find the cranial division and cusp (working ventrally)
follow the humerus down (find the deltoid tuberosity where apex of the ‘A’ shape of muscles)
Follow to the elbow: feel the radius and the olecranon (extension of the ulna)
Feel down radius (feel muscle difference on the lateral and medial sides) to the carpus
Feel down to the metacarpus and styloid process, just above the fetlock (on either side there are accessory carpal bones, remnant of previous digits)
Feel around the fetlock joint, down the phalangeal joints.
Same applies for the distal limb, except looking at the hip, femur, tibia, hock and tarsus.
How do we palpate a hoof?
Use hoof palpaters
Hold the hoof between your knees
Use the tool to apply pressure along the white line, across the heel bulbs, on the hoof and opposite side of the frog (on both sides).
bash the hoof too
observing for any tenderness, swelling or localised heat.
Define conformation and outline what lines of weight-bearing, symmetry and posture we’re looking at
Physical appearance and outline of a horse as dictated by bone and muscle structure
from the front - does the weight run vertically through the middle of the limb
side: does vertical line down back of hock, straight metatarsal, back of fetlock?
don’t be too judgemental - legs may be ok even if not perfectly straight.
What is done for a dynamic physical exam
Observe the horse in:
walk, trot and canter
in a straight line in walk and trot, in hand
on the lunge (both directions then on a hard then a soft surface, walk, trot and canter)
From the lateral aspects
From cranial/caudal aspects
always in hand (often ridden too)
what are we looking at in a dynamic exam?
gait symmetry
symmetrical movement of poll
symmetrical movement of tuber coxae
joint flexion
hoof landing
hoof tracking up
How can the head position be used to identify lameness
should be held in a steady position
If the horse does swing its head whilst moving, as long as it’s symmetrical it’s ok
Does the horse raise its head on one limb and lower on the other?
raise up = ouch
raise down = sound
How does the position of the tuber coxae tell us about lameness
as long as there’s symmetry it’s generally ok
is one side dropping more than the other?
the side that’s dropping/swinging more= the lame limb
Why is observing at a trot better than at a walk?
trot = 2 beat footfall therefore 50% chance of spotting
walk = 4 footfall beat.
why do we hold flexion tests for 30-60s?
aim is to walk/trot the horse immediately after
if there’s discomfort, it will be easier to see after having held it in this way.
why do we use lunging?
the limb on the inside of the circle take more load bearing
the limbs on the outside must extend more
what tendons can we palpate in the distal limb of the horse
flexor tendon - runs down the back just under the skin, DDFT is just underneath
extensor tendon runs down the side
suspensory ligament runs down both sides
What are 3 examples of diseases/problems that cause recumbency in cows
calving paralysis
fracture of the femur
toxic E.coli mastitis
What does DAMNIT-V stand for
D- degenerative
A - anomalous
M - metabolic
N - neoplastic, nutritional
I - idiopathic, infectious, inflammatory
T - toxic, traumatic
V - vascular
What do we use DAMNIT-V for?
classifying diseases
what does degenerative mean?
a disease that’s characterised by progressive deterioration and loss of function of tissues/organs
what does anomalous mean?
a congenital anomaly, birth defect or congenital malformation
what does metabolic in DAMNIT-V mean
disrupts the body’s ability to convert food/drink into energy
what does Neoplastic mean in the DAMNIT-V
a tumour, benign or malignant
what does idiopathic mean in DAMNIT-V
a disease of which the cause is unknown
What are some examples of diseases in cows that we can classify into DAMNIT-V?
metritis - uterine infection
acidosis - abnormally low pH
blaot - excessive gas accumulation or rumen, leading to distension and potential organ damage
exhaustion - a metabolic disorder that affects fed cattle
peritonitis - inflammation of the lining of the abdominal cavity (often caused by a compromised gut wall enabling opportunistic bacteria to enter).
Bacterial Spongiform Encephalopathy - mad cow disease
what is the most common cause of recumbency in recently calved dairy cows?
Hypocalcaemia - a metabolic condition
why does hypocalcaemia occur in recently calved cows?
a large amount of calcium is diverted to the udder for milk production
what is hypocalcaemia also know as and why does it cause recumbency?
milk fever
cows can’t mobilise calcium from the bone or increase absorption from the gut quick enough
Ca ions are needed for muscle contraction, so with the reduced amount, muscles can’t contract as much.
what clinical signs may we see with milk fever
recumbency
weakness
bloat
dystocia
ataxia
stiff, dry faeces
retained foetal membranes
dry muzzle
lack of rumen contractions
‘S’ shaped bend in the neck
weak heart sounds
how can we diagnose milk fever?
clinical signs (the abnormal findings you identify on an examination)
clinical pathology (results from samples collected from the patient and analysed).
When taking a blood sample, why do the vacutainers contain a vacuum?
physical mechanism to draw blood out
sterile
What are some considerations when taking a blood sample from a cow tail vein?
keep needle away from me (zoonotic risk)
keep needle in its sterile tube until ready to insert
once needle is inserted, don’t remove until all vacutainers are filled
be careful removing vacutainers so the needle isn’t pulled out
may need to subtly adjust the tail position to ensure continuous blood flow.
what method is the best way to administer calcium salts for milk fever treatment?
IV - transported around the body fastest and bypasses the slow digestive system
also give a s/c - this enables a more long lasting effect (sudden introduction of lots of Ca could lead to problems in the brain)
what do we use to treat milk fever
20% calcium solution when s/c (a more gradual, prolonged effect, done in addition to IV)
40% calcium solution when IV
How do we administer treatment for milk fever
via a ‘flutter valve’ to the jugular vein
administer slowly (over 5-10mins), rapid administration can interfere with cardiac rhythm leading to death.
Rate of flow can be controlled by raising or lowering the bottle
long, large gauge needles should be used (14 gauge, 2” or 16 gauge 1.5”)
Why can milk fever cause calf death
low calcium levels interfere with contraction of the uterus and the cows ability to strain. this delay can result in a still birth.
What 3 kinds of muscle are there
smooth
striated
cardiac
Outline skeletal muscle in mammals and some functions
around 400-600 skeletal/striated muscles (40-60% total body weight)
Functions
locomotion and breathing
postural support
heat protection during cold stress
largest protein store
energy store
Describe the structure of skeletal muscle fibres
striated
a true syncytium (single cells with multiple nuclei)
nuclei are peripheral
muscle fibres are very large (10-100micrometres diameter, very long length, arranged in bundles called fascicles.
connective tissue: epimysium, perimysium, endomysium
Microstructure:
sarcolemma, myofibrils, myofilaments
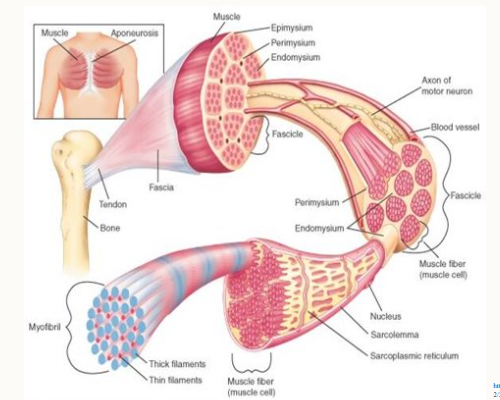
outline the connective tissue we find in skeletal muscle
Epimysium: surrounds the entire muscle
Perimysium: surrounds bundles of muscle fibres - fascicles
Endomysium: surrounds individual muscle fibres
Function:
Functional: transfer information to the bone which affects movement
Protective: Strong, helps support muscle when under force and tension
too much connective tissue = dangerous e.g. can lead to fibrosis.
outline the microstructure of skeletal muscle
sarcolemma - muscle cell membrane
myofibrils - tubular structures that pack the fibres
myofilaments - threadlike strands within myofibrils, actin (thin filament, with troponin and tropomyosin) and myosin (thick filament)
Describe the interaction between actin and myosin
found in repeat units called sarcomeres.
Work together to cause muscle contraction
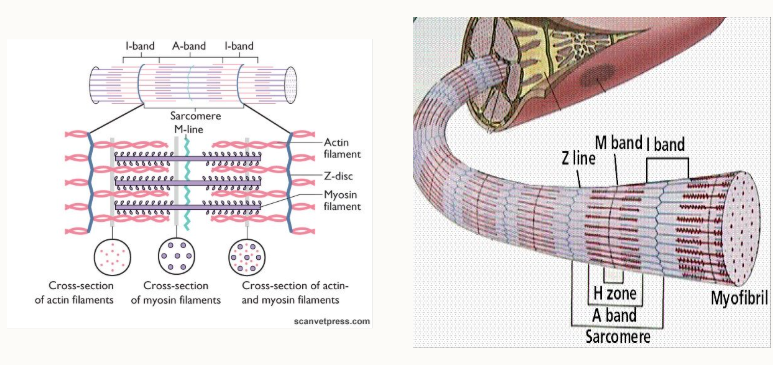
Outline the structure of sarcomeres
2 Z-lines = one sarcomere:
Z-line = ends of sarcomere, boundary
I-band = actin only
A band = from edges of myosin, zone that contains whole of myosin
H zone = only myosin
M band = transverse line that binds the myosin filaments in the middle of the sarcomere
What do myosin and actin look like/structure
Myosin = fibrous tail and globular head
Actin = globular protein, 2 chains that are coiled around each other with tropomyosin twisted around and troponin spaced at regular intervals.
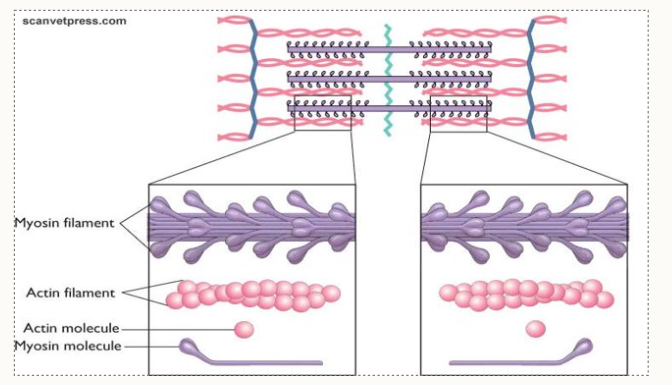
outline the sliding filament theory
muscle shortening occurs due to the movement of the actin filament over the myosin filament
formation of cross bridges between actin and myosin filaments
reduction in the distance b/w Z-lines of the sarcomere
Give 3 reasons why knowing about skeletal muscles is helpful
know how they work, so know when it goes wrong
know which work in groups
know how different drugs affect different muscles
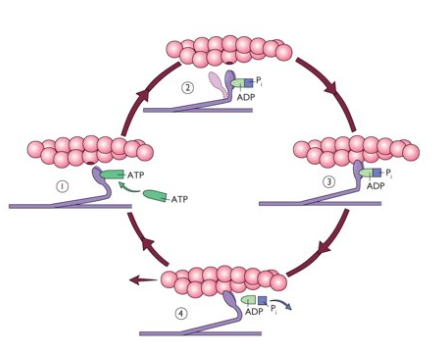
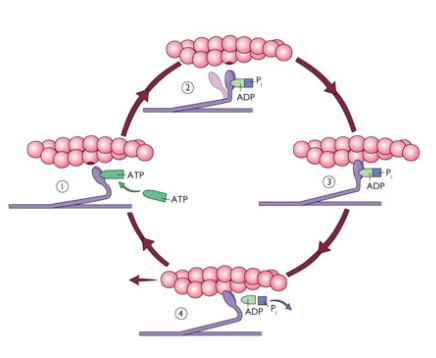
How to the cross-bridges form?
Ca2+ ions bind to troponin which causes a conformation change in shape which exposes the binding sites on actin
ATP binds to the head of myosin causing the myosin head to move
ATP is hydrolysed to ADP + Pi and the energy released from this reaction causes the cross bridge to form
ADP + Pi detach from the myosin head, which causes the myosin head to slide back, which in turn pulls the actin with it.
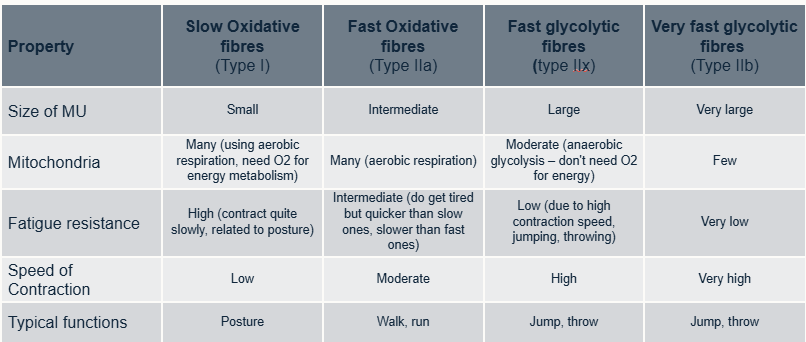
what are the 2 groups of fibre types and examples of each
Slow fibres: - type 1, slow oxidative fibres
Fast fibres:
Type IIa, fast-oxidative
Type IIb - fast-glycolytic fibres
Type IIx- intermediate properties
How is fibre type composition analysed?
Immunochemistry
each fibre has a specific myosin isoform
ATPase activity
fibres have specific metabolic profiles
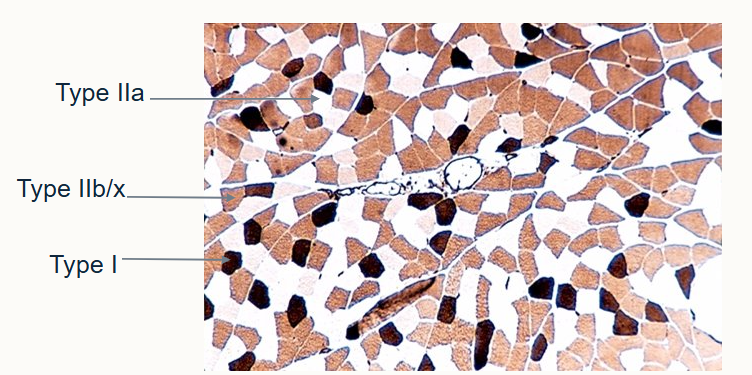
How do the different fibre types look histologically?
Type IIa - white
Type IIb/x - brown, grainy
Type I - black
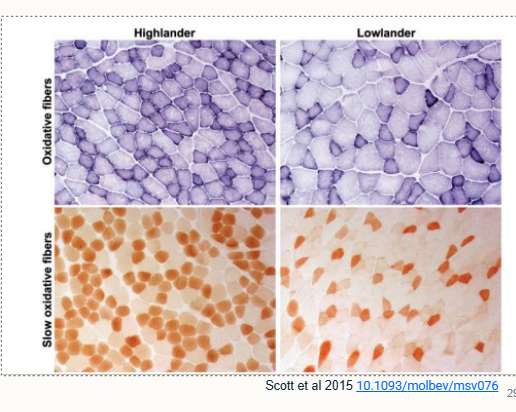
give one reason why fibre type composition may vary within species
live at different altitudes e.g. highlander vs lowlander mice
Outline the properties of the fibre types
What is muscle fatigue
a decrease in maximum contractile force
ATP is required for formation of cross bridges, an increase in inorganic phosphates (often during sudden, strenuous work) and a decrease in Ca2+ ions
A reduction in ATP - leads to rigor.