Neuro E2- Cognitive disorders
1/92
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
93 Terms
Delirium or Dementia?
acute onset
responds to some stimuli appropriately
appear sleepy, disoriented, and inattentive
level of consciousness may be impaired
Delirium
Delirium or Dementia?
chronic onset, worsening over time
usually appear normal but confused
normal level of consciousness
impairment in the content of consciousness
Dementia
What is the generalized loss of memory, psychogenic or organic in nature, with inability to learn new material?
Amnesia
What score on Folstein’s MMSE requires additional testing?
less than 24/30
What is disorder of articulation where basic language is intact (issue w/ speaking, not the content)?
Dysarthria
What is a true language disturbance that demonstrates impaired production and/or comprehension of spoken language?
Aphasia
What area of the brain is the center for language use, that processes input from both visual and auditory sources (reading/hearing)?
Wernicke’s area
What is the language pathway?
visual or auditory cortex (listening) → wernicke’s area (understanding) → Broca’s area (speaking ) → motor cortex (speaking)
What aphasia results form a lesion in the posterior temporal region (receptive aphasia)?
Wernicke’s aphasia
What aphasia results from a lesion in the frontal lobe (expressive aphasia)?
Broca’s aphasia

What type of aphasia?
does not understand what is said or written
unable to repeat what they hear
speech is fluent (grammatical) but disordered
can’t convert thoughts into meaningful language
unaware that their responses are nonsense
receptive
Wernicke’s
What type of aphasia?
understands what they hear but produces few words with many pauses
unable to repeat what is said to them
intonation is flat and monotone
repetition of words and phrases are impaired
normal content with no grammar
aware of deficit
expressive
Broca’s
What type of aphasia?
both receptive & expressive elements
loss of ability to comprehend spoken/written language & express language
may retain some comprehension & fluency
usually correlates w/ infarction of MCA
can be early manifestation of neoplastic, inflammatory, or degenerative disorder
Global
What kind of amnesia?
can’t remember emotionally charged events
can remember objective facts and events, but not the whole trauma
Psychogenic amnesia
What kind of amnesia?
can’t remember objective facts
Organic amnesia
What kind of amnesia?
loss of memory for events immediately prior to the disorder
ex: occurs with head trauma
Retrograde amnesia
How would the acutely confused patient respond to the recall & memory portion of MMSE?
unable to learn new material due to impaired level of attention or consciousness
How would the demented patient respond to the recall & memory portion of MMSE?
problem with recent memory, remote memory is intact
What are red flags symptoms?
progressively declining neuro exam or LOC, pupillary asymmetry, seizures, repeated vomiting, double vision, worsening headache, disorientation, unusual behavior / confused or irritable, slurred speech, unsteady on feet, weakness/numbness in arms or legs
What are causes of delirium?
Dementia
Electrolyte disorders
Lung, liver, kidney, brain dysfunction
Infx
Rx drugs
Injury, pain, stress
Unfamiliar environment
Metabolic
How does alcohol intoxication present?
nystagmus, dysarthria, limb, gait ataxia (drunk = delirium)
Does alcohol level predict symptoms?
no
What symptoms are seen with alcohol withdrawal?
early (w/in 6 hrs): insomnia, tremulousness, mild anxiety, GI upset, HA, diaphoresis, palpitations
day 2: generalized tonic clonic seizures & hallucinations
day 2-4: delirium tremens (DTs) - hallucination, disorientation, tachycardia, HTN, hyperthermia, agitation, diaphoresis (lasts 1-5 days)
What is the treatment for alcohol withdrawal?
benzodiazepines- Diazepam
correct fluid, electrolyte, glucose, & thiamine abnormalities
What endocrine emergencies can cause delirium (altered level of consciousness)?
hypothyroidism (tx w/ levothyroxine)
hyperthyroidism (tx w/ antithyroid drugs, BBs)
hypoglycemia (tx w/ IV dextrose)
hyperglycemia (tx w/ insulin, IVF, and K if DKA)
What electrolyte abnormalities can cause delirium?
Hyponatremia: +HA, N, V, seen in athletes who replace fluids w/ only water
Hypocalcemia: +paresthesias, Trousseau & Chvostek signs
What is the treatment for hyponatremia?
water restriction & IV hypertonic saline; slowly raise level to 125-130
***avoid central pontine myelinolysis
What is the treatment for hypocalcemia?
IV calcium gluconate and seizure precautions
What environmental conditions can cause delirium?
heat exhaustion & heat stroke
What condition?
thiamine deficiency in chronic alcoholic
causes delirium, ophthalmoplegia/nystagmus, gait ataxia
ataxia may not be fully reversible
deficits in learning & memory can follow
Wernicke’s encephalopathy
What is the treatment for Wernicke’s encephalopathy?
Thiamine replacement (give BEFORE glucose bolus)
What should all patients with undiagnosed AMS, oculomotor disorders, or ataxia receive?
Parenteral thiamine
What nutritional disorder?
due to poor intake, often w/ pernicious anemia
presents with mild confusion to dementia to psychosis
Vit B12 deficiency
What condition?
accumulation of ammonia in liver failure
delirium, asterixis, seizures, coagulopathy
requires lactulose & correct coagulopathy
Hepatic encephalopathy
What condition?
renal failure
causes delirium
requires dialysis & renal transplant
Uremia (elevated BUN)
What psychiatric disorders can present with delirium?
psychoses, severe depression, acute anxiety
What condition?
infection of meninges- invasion of bloodstream, crosses BBB
direct contiguous spread- sinusitis, OM, lungs, UTI, wounds
MC- s. pneumoniae
Meningitis
What is the classic triad of meningitis?
fever, nuchal rigidity (neck stiffness), mental status change
What is the workup for meningitis?
Kernig’s & Braduzinki’s tests
MRI- edema, inflammation
LP- cloudy CSF, high protein, high lactate, low glucose, many WBCs
What condition has the following CSF analysis?
Opening pressure: 200-300
WBC: 100-5000; >80% PMNs
Glucose: < 40
Protein: > 100
Microbiology: specific pathogen demonstrated in 60% of gram stains & 80% of cultures
Bacterial Meningitis
What condition has the following CSF analysis?
Opening pressure: 90-200
WBC: 10-300; lymphocytes
Glucose: normal or reduced in LCM & mumps
Protein: normal or slightly elevated
Microbiology: viral isolation, PCR assays
Viral meningitis
What condition has the following CSF analysis?
Opening pressure: 80-200
WBC: 0-5; lymphocytes
Glucose: 50-75
Protein: 15-40
Microbiology: negative findings
Normal values
What is the MCC of meningitis?
viral
What type of meningitis?
slower onset & less severe sx
MC enterovirus, also HSV, VZV, mumps, HIV
CSF: slightly elevated WBC w/ inc lymphocytes (not neutrophils); normal glucose; slightly elevated CSF protein
viral meningitis
What is the treatment for meningitis?
begin abx ASAP if bacterial suspected (regardless of what it is)
if viral suspected - acyclovir
considere steroids w/ first dose - decadron
airway support, O2, intubate, fluid hydration, Tylenol for fever
What should be done BEFORE starting treatment for meningitis?
blood cultures & LP
What condition?
infection of brain tissue; MC viral
AMS, personality changes, hemiparesis, focal seizures, autonomic dysfunction, ataxia, dysphagia
Encephalitis
What kind of encephalitis?
fecal - oral transmission
MC in summer & fall
herpangina: hand, foot, mouth; mild sx (except for enterovirus 71- assoc w/ rhomboencephalitis)
low mortality (except for enterovirus 71)
Enterovirus encephalitis
What kind of encephalitis?
MCC of fatal encephalitis in US
human-human transmission or reactivation of latent virus
HSV, VZV
start tx as early as possible - acyclovir
HSV encephalitis
What kind of encephalitis?
transmitted by birds and mosquitoes
late summer & early fall
increased severity w/ advanced age
supportive treatment
West Nile virus encephalitis
What kind of encephalitis?
relatively common world wide
transmission through infected animal bites
presents w/ encephalitis or paralysis
fatal unless vaccine & antiserum administered before sx occur
Rabies encephalitis
What is the workup for encephalitis?
Head CT +/- contrast; MRI
LP - search for elevated ICP, obstructive hydrocephalus, mass effect
EEG- diffuse slowing
CSF analysis- protein normal or slightly increased, lymphocytes present, glucose usually normal
What should be performed before LP in encephalitis evaluation bc of risk of brain herniation?
CT
What is the treatment for encephalitis?
airway management, fluid/elyte balance, nutrition, avoid & tx secondary infx, tx hyperpyrexia, manage ICP (head elevation, diuresis, mannitol, steroids, seizure precautions)
What condition?
plasmodium species infx
can present with delirium, seizures, focal neurological abnormalities
organisms seen in thick & thin blood smear
treatment based on geography,
high mortality if seizures or coma
Cerebral malaria
How does CSF in cerebral malaria appear?
increased pressure, slightly elevated protein, monocytes
What condition?
due to a sudden increase in BP
if NO hx of HTN, sx appear at lower BP than a patient w/ HTN
BP readings does not necessarily correlate w/ sx
Hypertensive encephalopathy
What is the treatment for hypertensive encephalopathy?
lower BP w/ labetalol or nitroprusside (avoid in stroke pts)
What condition?
trauma induced alteration in mental status ± LOC
severity of trauma associated with severity of symptoms
hallmark symptoms: confusion & amnesia, can last minutes-hours
early sx: HA, dizziness, lack of awareness of surroundings, N, V
later sx: mood/cognitive disturbances, sensitivity to light and noise, sleep disturbances
Concussion
What increases morbidity in post-concussion syndrome?
repeat concussions
What are risk factors for delirium?
advanced age, preexisting cognitive deficit, prior episode of delirium, polypharmacy, alc/drug dependence, psychoactive drugs (benzos, anticholinergics, narcotics), vision/hearing deficits, preoperative complications, immobility, severe comorbidity
What should be given for hyperactivity in acutely confused patients?
Haloperidol (Haldol)
What condition?
progressive decline in cognitive function beyond what might be expected from normal aging
normal level of consciousness
recent memory usually markedly affected
sx involve diminution of cognitive skills & learned tasks and slowly progress to include personality changes & intellect
Dementia
What is the MC form of dementia?
Alzheimer’s disease
What is the workup for dementia?
non contrast CT or MRI, screen for depression, check vit B12 levels, thyroid function tests, syphillis testing if suspicion high, genetic markers to confirm if strong fhx
(apolipoprotein E epsilon 4 allele not currently recommended)
The following DSM V criteria is for what condition?
cognitive impairment in at least 1 of the following: learning/memory, language, executive function, complex attention, perceptual motor function, social cognition
must be acquire, represent significant decline, & interfere w/ independence
does not occur exclusively during course of delirium (always present)
not better accounted for by another disorder
Dementia (Major neurocognitive disorder)
Who is Alzheimer’s disease MC in?
F > M; prevalence 50% by age 85
What condition?
progressive degenerative disorder (over 5-20 years)
major sx: gradual development of forgetfulness
progresses to disorientation to time, then place
mobility, behavior, temperament, & conduct decline
restless & agitated → depressed
Alzheimer's disease (AD)
What is the only way to definitively diagnose AD?
postmortem
What 3 microscopic changes are seen with AD?
neurofibrillary tangles (tau), cortical atrophy (pyramidal layer of hippocampus), & amyloid plaques
How does the brain appear in advanced stages of AD?
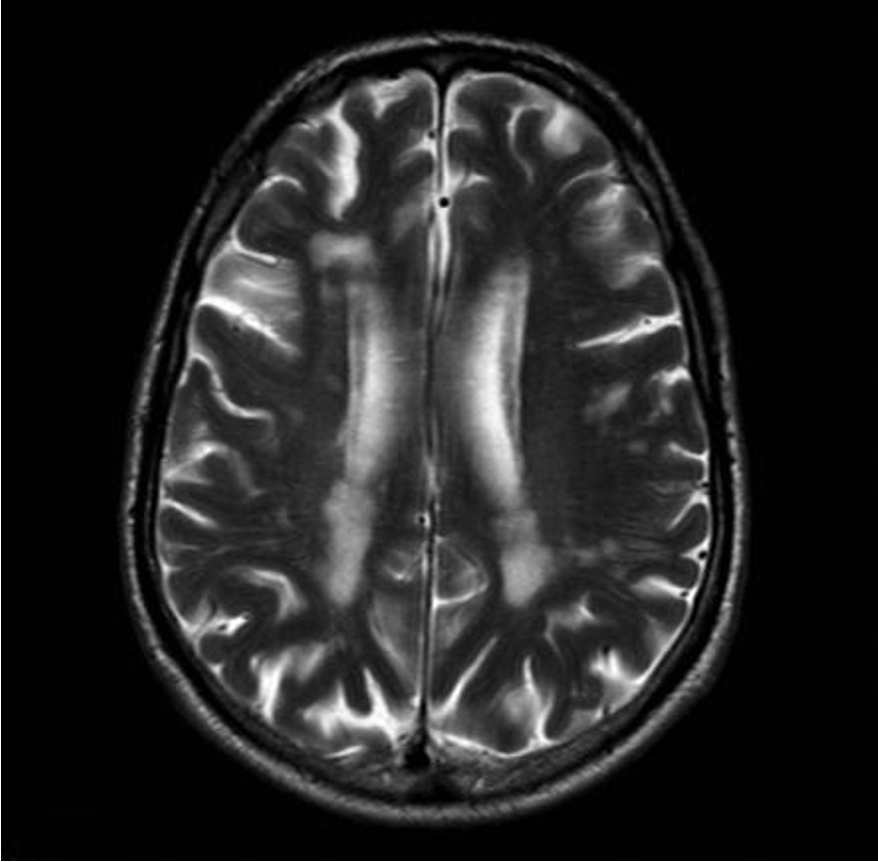
diffusely atrophied & weight reduced by ≥20%
ventricles enlarged, cerebral atrophy w/ cerebral sulci widened
How do AD patients appear early on in the disease?
non focal neuro exam: short term memory abnormal, speech hesitant, apraxia/visuospatial disorientation (gets lost easily)
& short, slow. shuffling steps, flexed posture, wide base, & difficulty initiating walking
How do AD patients appear later in the disease?
language & cognition decline; paranoia, hallucinations, delusions, pt becomes mute, bedbound, & incontinent; seizures, extrapyramidal rigidity/bradykinesia,
primitive reflexes emerge (sucking & grasping)
What workup can be done for AD?
MRI, CT, EEG (diffuse slowing), PET scan (diminished activity in temporal lobe), neuropsych testing (dec executive function)
correct dx made 90% of time w/ clinical data, time course, & CT/MRI
What are treatment options for AD mild-mod sx?
acetylcholinesterase inhibitors: donepezil, rivastigmine, galantamine
antipsychotics, antidepressants, anxiolytics
What are treatment options for AD severe sx?
memantine (Namenda)- glutamate receptor antagonist
Can treatment reverse existing deficits or arrest progression in AD?
no
What are SEs of acetylcholinesterase inhibitors?
N/V/D, dizziness, elevated LFTS (*get LFT before starting)
What are alternative therapies for AD?
Vit E, selegiline, ginkgo biloba
What occurs 5-20 years after AD onset?
death- infection & inanition (loss of social, moral, or intellectual vitality/vigor)
What are Lew bodies?
intracytoplasmic inclusions in cortex & brainstem associated with dementia (no tangles or plaques)
What condition?
progressive dementia- alzheimers & late parkinsonian features
TRAP, amnesia, visuospatial disorientation, aphasia, fluctuations in alertness, etc
diffuse involvement of cortical neurons w/ lewy body inclusions & absence of inconspicuous number of tangles/plaques
psychotic features- hallucinations, delusions
Dementia w/ lewy bodies
What is the 2nd MCC of dementia?
dementia w/ lewy bodies
What should be avoided in dementia with Lewy bodies?
antipsychotics (more sensitive)
Psychotic features such as confusion, hallucinations, & paranoid delusions are seen in which condition?
dementia w/ Lewy bodies
What is the treatment for Dementia w/ Lewy bodies?
L-dopa for PD features for a limited time (can cause delirium/hallucinations or not have a consistent response)
What is the 3rd MCC of dementia?
vascular (multi-infarct) dementia
What condition?
multiple infarcts in subcortical white matter, basal ganglia, or thalamus
usually have hx of HTN or CV risk factors
step wise progression; new infarct = new deficit
memory loss, slow thinking, balance issues, dysarthria, emotional lability, absent mindedness, etc
Vascular / Multi-Infarct Dementia
How was vascular/multi infarct dementia appear on MRI?
small subcortical lucencies / lacunar infarcts
What is the treatment for vascular dementia?
Donepizil, Memantine
manage HTN/CV risk factors- CCBs (nimodipine), anti-platelet drugs, regular exercise & healthy diet
What condition is most commonly mistaken for dementia?
depression
Dementia or depression?
unaware of extent of deficits
no complaints of memory loss (don’t know they forgot)
few vegetative sx (up & moving when they are able)
worse at night
abnormal neuro exam & labs
Dementia
Dementia or depression?
aware of deficits
complains of memory loss (knows they forgot)
prominent vegetative sx
not worse at night
normal neuro exam & labs
Depression