Exercise Considerations for Clinical Populations
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
1.Define and provide examples of cardiovascular disease
2.Describe the physiology and functional consequences of stroke
3.Explain how exercise can be beneficial to stroke survivors
4.Describe the physical activity recommendations for stroke survivors and compare/contrast with those for healthy older adults
5.Design physical activity programs for stroke survivors, based on recommendations
6.Identify barriers and motivators for exercise in stroke survivors and develop example exercise plans
Cardiovascular Disease
-a class of diseases affecting the heart and/or blood vessels
Examples:
-Heart attack
-Stroke
-Heart failure
-Peripheral artery disease
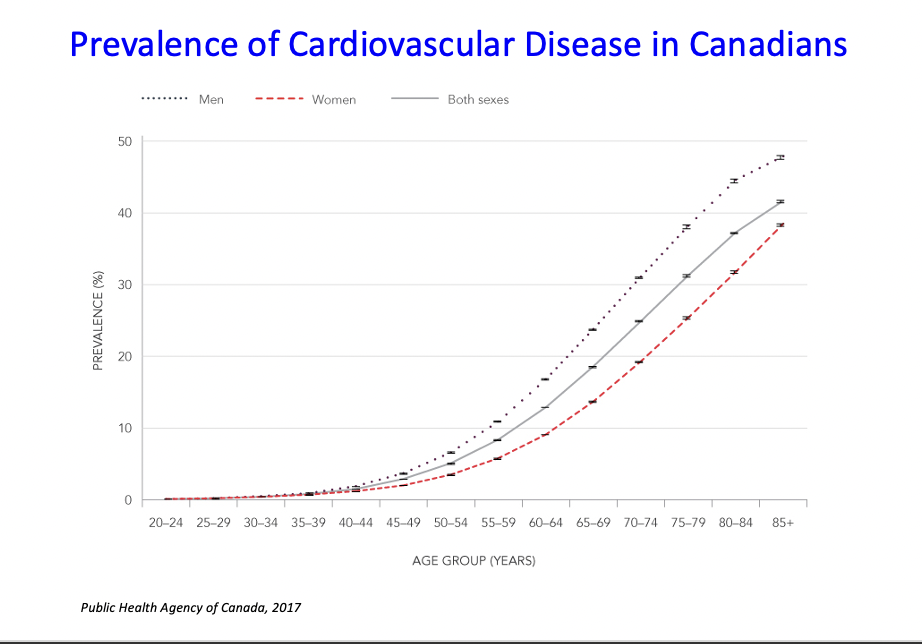
Prevalence of Cardiovascular Disease in Canadians
-once we hit our 50s there is an expential increase
Ontario Exercise Heart Trial
-started the canadian center for activity and aging
-after a heart attack, they should not just be lying around they should be doing exercise
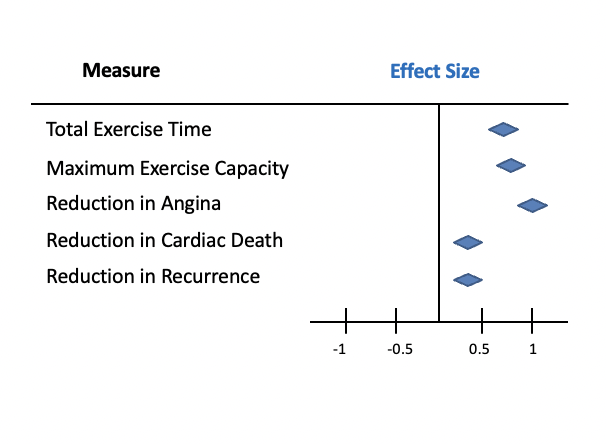
Effect of Physical Activity on Cardiac Rehab Patients
-lots of evidence stating that exercise beneficial for cardiac rehab patient
-reduction in chest pains (angina) reduction in death and reoccurrence
Stroke
•damage to brain cells
–due to a lack of oxygen
•Ischemic (bloodflow blocked by a clot or smtg else in brain) or Hemmorhagic (a blood vessel bursts and blood supply goes out of the area
ischemic more common- not get blood flow for a period of time
•Symptoms:
–depends on location and extent
-very
F-facial drooping
A-arms (numbness, tingling, weakness usually on one side of body)
S- speech impairment or nonsense talk
T-time is critical for treatment
*every 10 minutes in Canada someone has a stroke
-14,000 Canadians will die from stroke each year
-after age 55 your risk of stroke doubles every 10 years
*aged related condition because incidence increases with age
*motor, speech and congitive deficits as well
What happens if there is reduced blood flow?
Effect on neurons?
reduced oxygen → reduced atp
reduced or no oxygen going to the brain, no energy for those neurons, highly oxidative they need that oxygen
neurons will starve
-neuron will die
Symptoms:
motor (hemiparesis)
cognitive
speech/language
*if not a major blockage or caught quickly- can suffer a minie stroke who wont experience as many symptoms
-but most ppl will experience symptoms are treatment of a stroke
Stroke Rehabilitation
~10% patients - complete spontaneous recovery (first 2 weeks)
*if you have a stroke in a large vessel all the minor ones will be cut off versus if you were to have stroke in a minor one
~10% patients - no benefit from rehab -can participate in years but do not see improvement in recovery
~80% patients - benefit from rehab- almost always the rehab program involves PA or exercise
Why would exercise be beneficial for stroke survivors?
-neurogeneis, blood flow, neuroplasticity (forming new connections)
decreased risk factors (decrease blood pressure)
increased blood flow
-Repair damaged neurons
- decrease inflammation
Exercise Barriers in Stroke Survivors
-stroked related impairments (cognitive, motor, speech/language) e.g. not being able to understand instructions,
-fatigue- get tired sooner
-embarrassment of stroke related impairments e.g. hemiparesis
-fear of another stroke (historical thinking that it is dangerous)
Exercise Motivators in Stroke Survivors
-social support (meeting other stroke survivors) e.g. exercise classes with others
-resumption of activities of daily living e.g. drivers licence might be suspended- might be a major motivator
Exercise phases
Acute- during hospitalization
-physical therapist
Rehab
-hospital or home, but no longer in acute care
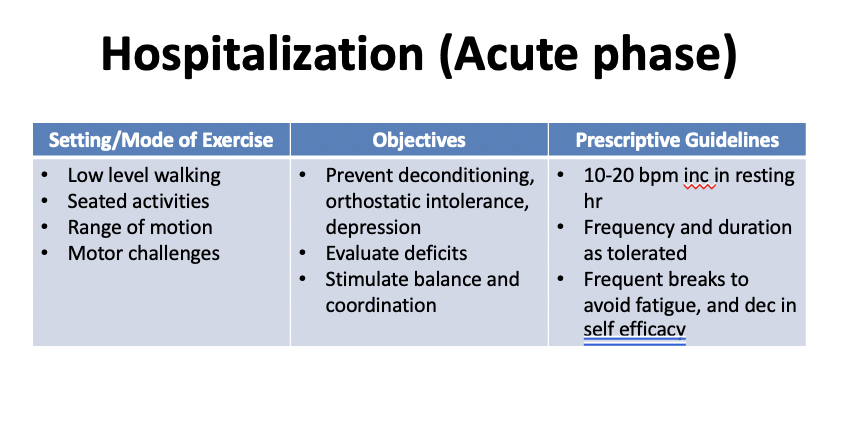
Hospitalization (acute phase_
-still in hospital, recently stabilized
-might move them through gentle rom, pre
-social- seeing someone everyday
-evaluate the deficits and functions they still have
balance and coordiantion if they are able to stand and walk
inc hr from 10-20 bpm from resting heart rate
Goals: inpatient/ outpatient rehab
-inc function
-inc ability to perform activities of daily living
inc independence
improve health- reduce risk of another stroke from occurring
*may work with speech language pathologist, etc depending on their impairments
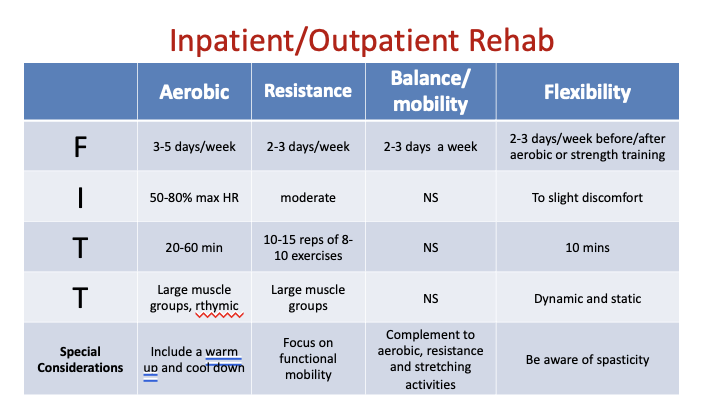
Inpatient/outpatient goals
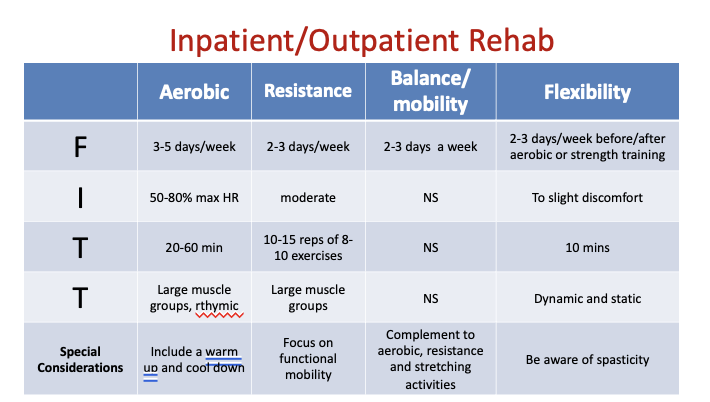
Spasticity
-abnormal muscle tightness due to prolonged muscle contraction
-difficulty with movement
*rlly tight, unrelaxed postures of the hands or feet- seems to be adaption wit hSC. motor neurons in spinal cord get over excited- not activated when you are trying to activate them
-dont want to force things because it can cause injury, mvmt patterns might be different because of spasticity e.g. in hands dont give them dumbbells
-not all stroke survivors have it but its very common in stroke versus neurological disorders
Comparison between aging adults and stroke adults
no number but intensity a little different - just moderate for RT for stroke survivors
Balance and mobility- dont have time for stroke\
Intensity of aerobic- upper limit for health oa is 85% hr max, stroke is 80%
*a lot of it is the same though
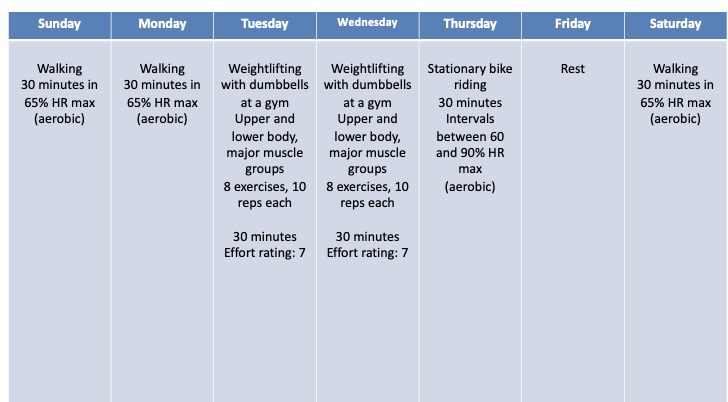
Your client is a 68-year old female who had a stroke 3 months ago. She is recovering, but still has some mild cognitive and motor function impairments. For this reason, she is currently unable to drive. She lives with her 68 year-old husband, who is relatively healthy and is able to drive. Prior to her stroke, she walked for 30-60 minutes daily. Her biggest motivation for engaging in exercise is to regain her ability to drive. Design an exercise program for this client, specifying the ITT (of FITT) for each day of the week.
-days of week versus fitt table dont care what you use as long as you complete everything
Aerobic- walk Monday Wednesday and Friday, 15 minutes
-include a 5 minute warm up and 5 minute cool down
Sunday- Walking 10 min 50% hr max, 2 min warm (dynamic) up 2 min cool down (static)
Monday- sit on chair resistance e.g. toe lifts (for driving function)- move ankles through ROM, 7 reps, 3 exercises, moderate intensity
Tuesday- cognitive games (*balance and for driving), 20 minutes
Wednesday- rest
Thursday- same as Sunday
Friday- upper body resistance training e.g. resistance bands, 7 reps, 3 exercises, moderate intensity
Saturday-rest
make sure you hit on the special considerations we learned about
High blood pressure is a major risk factor for stroke.
1)Describe one age-related change in the cardiovascular system that contributes to high blood pressure, including two theories of aging that explain the change
-atherosclerosis- the buildup of plaques on the inside of arteries = narrowing of arteries
inc in inflammation that immune system isnt able to steal with in combination with an increase in ROS, leads to inhibition of decalcification processes (immunological theory) Wear and tear theory with increased ROS, inc ROS leads to reduction in removal or plaques. both together is what inhibits the decalcification process
Describe the change, describe 2 theories that explain that process
inc release of nt caused by calcium, results in inc depolarization adn inc atp use of post neuron, releases more neurotransmitter, causes more cell death, inc in calcium is rlly helping spread cytotoxic events in a stroke
2)Describe the role of calcium in the process of a stroke
3)Explain why exercise is beneficial after stroke
-blood flow to repair neurons that are damaged, reduces inflammation, decreased bp to reduce the risk of another stroke
An individual 8 months post-stroke has been walking 30 min/day, 3 days/week at 65% HR max. They would like to improve their strength and endurance so they can safely lift and carry their 2 year-old grandchild.
1)List two problems with the exercise program outlined for this individual on the next slide
2)Describe two mechanisms by which strength would be increased following 2 months of training
Direct pathway
-to initaite movement
what would happen if dopamine was reduce
Indirect pathway
-end of the pathway the same- excitatory outputs to motor areas of the brain to the thalamus and inhibitory pathways from globus pallidus
Tonic from subthalamus
*same stuff from the direct is same as indirect (above)
Neurons from SN releasing dopamine but dopamine is acting as an inhibitory path (direct it was excitatory)
indirect does not right through globus pallisus
less activity from neuron in the striatum, more activity in inhibitory neuron means more inhibition and less activity in the next neuron. if less activity in inhibitory neuron means more activity in the next neuron because yo have removed some of the inhibition.
less activity in inhibitory neuron means less inhibition of the next neuron meaning more activity out of thalamus to those motor areas
you need a stronger cortical input to because you have competing forces
-inhibitory and excitatory- whichever one is slightly louder will win
-if you are not thinking about stopping mvmt it will happen
WHAT ABOUT SOMEONE WITH PARKINSONS DISEASE
-damage to neurons in substantia niagra, end up with less dopamine being released (less inhibitory neurotransmitter)
-less activity in SN, less dopamine, means less inhibition of neuron in striatum- what happens to its activity= more activity in inhibitory neuron= less actiity in that neuron, less activity in inhibition in inhibitory neurons= more activity in next neuron= more activity in excitatory neuron= more excitation- more activity in next neuron= more inhibition= less activity coming out of the thalamus
*does. not mean we have completed stopped moved, results in SLOWED movements, not like stepping on the brakes more like easing up on the gas pedal, means less input from regions to stop a mvmt- easier activation of pathway from cortical- involved in freezing of movements
e.g. narrow mvmt we will all slow down but pd will completing stop bc they alr ened less activation so it will be enough
need direct pathway to initate movement- but once they initate it they can continue it
Parkinson’s Disease Treatment
How improve symptoms?
1.Pharmacological:
–L-Dopa (synthetic dopamine replacing dopamine that was lost) -cant target dopmaine to neurons in the striatum it will affect the entire brain, does take careful monitoring to get the right dosage
*most common and initial form of treatment
2.Physical aid:
–Trick the brain
e.g. laser beam on walker, mvmt initiation are with movements that are internally generated, so using external cues thats their cue to start moving they can initiate walking sooner
3.Surgical:
–Deep brain stimulation
-implant electrodes around globus pallidus sometimes in thalamus, and it is kind of like a pacemaker for the brain, sends impulses regularly to regulate impulses from the thalamus, very invasive
4.Exercise!
-Why?
-cant reverse or cure the disease but treat the symptoms and slow progression of the disease
-inc in neurotransmitters (dopamine), increased blood flow to the brain, reduces inflammation
*blood flow repair processes and removing byproducts.
*can reduce their L-Dopa intake because getting release of dopamine naturally
*inflammation when damage to neurons, slow down the progression of the disease
Parkinson’s Outcomes Project
Longitudinal study of >13,000 patients in 5 countries
Exercise is most effective if:
•starts early in disease progression
•at least 2.5 hours of activity per week
*most of this is aerobic, but usally as we will see, there are additional compoentns built in to target the specific concers of PD (balacne)
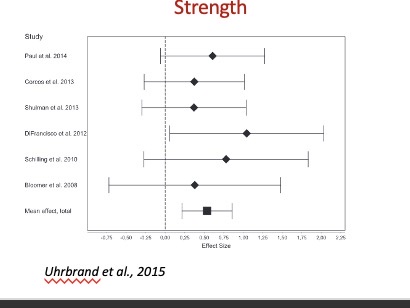
Effects of Exercise in Patients with Parkinson’s Disease
Increased or maintained:
-Strength (particualrly lower body strength can help with mobility and baalnce)
-Balance & mobility
üADL performance
üExercise capacity/fitness
üCognition
üSleep
üQuality of life
*sometimes maintaining your level is acc a good things, PD is a progression disease and expect it to get worse over time, even if no improvement but maintenance of symptoms that is a win
Benefits often not as great as for healthy age matched individuals.
Decreased or maintained:
-Tremor
Exercise Barriers and Motivators in Patients with Parkinson’s Disease
Barriers
fatigue easily
depression
cognitive impairment (BG involved with cognitive function)
embarrassment
fear of falling (balance is a big challenge)
motivation (lack of motivations)
medication effects -it works great but has a short half-life, when initially take it you might see no symptoms at all depending on disease progression. but after a few hours (3,4,5) start to see symptoms worsen again but they cant take too much meds bc it will throw off dopamine in other areas of brain
-symptoms are quite bad hour before their next dose
Considertions
1.exercise near peak drug effects
2.day to day variability is high and disease is progressive, masking progress
3.increased supervision and/or adapation may be necessary
4.reduced distractions, repeated demonstrations and more attentional cues can be helpful
5.difficulty regulating body temperature
6.difficulty swallowing- muscles around vocal cords and trachea, choking occurs at a much higher rate e.g. while exercising take a break so they can drink their water
7.autonomous dysregulation
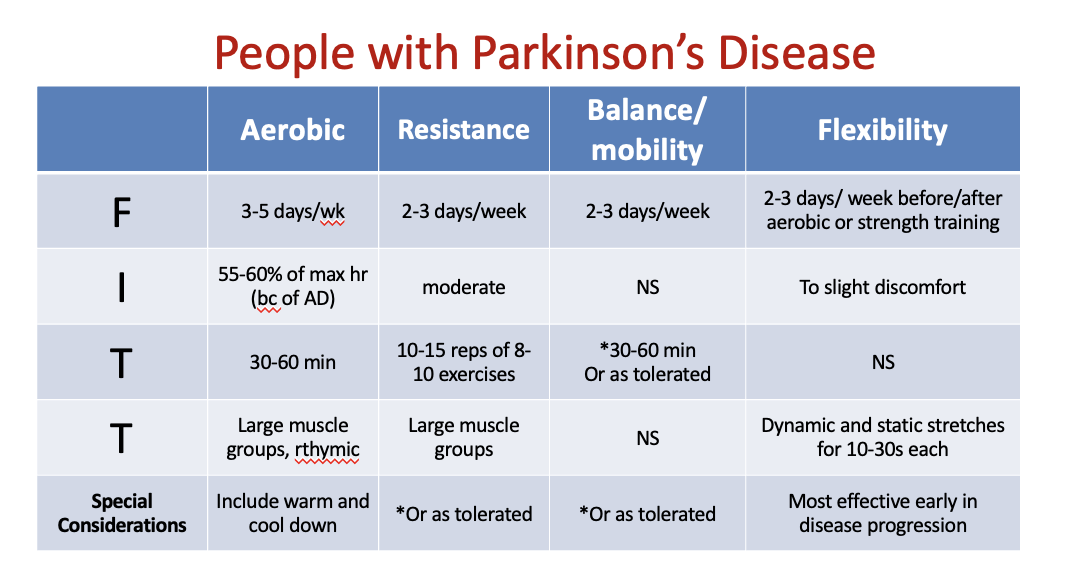
Your client is a 65 year-old male, who was diagnosed with Parkinson’s Disease 6 months ago. He was active in recreational sports until about 3 years prior to his diagnosis. He finds that he becomes fatigued quite easily when he attempts to be physically active now. Design an exercise program for this client, specifying the FITT for each day of the week.
-sometimes all can combined into one activity do ont have to seperately do aerobic, rt and balance etc, without making them do PA for 400 mins a week