Class 12 - Diversity & Ethical Considerations in Acquired Cognitive-Communication Disorders
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
What is diversity?
a term that can be defined in many ways, & it can include a variety of characteristics & ideas
(Diversity) Individual characteristics:
Race, gender, age, religion, sexual orientation, ethnicity, national origin, socioeconomic status, language, & physical ability
(Diversity) Collective characteristics:
Different ideas, perspectives, & values
(Diversity) Other dimensions:
Education, marital status, veteran status, & physical appearance
Diversity in Healthcare:
Diversity in healthcare refers to providing high-quality care for everyone by acknowledging & respecting diverse cultures, religious beliefs, genders, ages, socioeconomic statuses & all other diverse perspectives
It also empowers every patient & healthcare professional to have a voice in the type of care they receive & need
“Diversity is being invited to the party; Inclusion is being asked to dance.”
Diversity related issues in TBI:
Racial/ethnic minorities are at increased risk for TBI & poor health outcomes after TBI
African Americans have higher annual TBI-related hospitalization rate
American Indian/Alaska Natives have the highest annual TBI-related mortality rate followed by African Americans
Minorities have poorer functional outcomes on all measures at hospital discharge & one-year post-injury compared w/ Caucasians after TBI
Women & LGBTQ+ individuals in general, & especially w/ ABI, are more likely to be victims of abuse & violence. They are faced w/ greater social & economic disparities, as well as general & technological accessibility issues
Diversity related issues in Dementia:
While African Americans are about 2x more likely than whites to have Alzheimer’s & other dementia, they are only 34% more likely to have a diagnosis
Hispanics are about 1 & 1.5 times more likely than whites to have Alzheimer’s & other dementias, but they are only 18% more likely to be diagnosed
There are 2.7 million LGBTQ+ people over age 50 in USA (2017), & that # will likely double over the next 15 years
LGBT older adults are often marginalized & face discrimination
An LGBT person may not reach out for services & support because they fear poor treatment due to their LGBT identity, bc they fear the stigma of being diagnosed w/ dementia, or both
Several studies document that LGBT elders access essential services, including visiting nurses, food stamps, senior centers, & meal plans, much less frequently than the general aging population
The LGBTQ Caregivers:
The typical LGBTQ Caregiver is young (42.4 years old) & unmarried
LGBTQ Caregivers are most often caring for a parent or grandparent
LGBTQ Caregivers report high-intensity caregiving situation spending 28 hours a week assisting w/ care needs
They are more often the Primary Caregiver of their care recipient
Most LGBTQ Caregivers report high-intensity caregiving situation spending 28 hours a week assisting w/ care needs
They are more often the Primary Caregiver of their care recipient
Most LGBTQ Caregivers work while providing care & more often report financial strain related to caregiving
LGBTQ Caregivers more often report being in fair or poor health than non-LGBTQ Caregivers
Care for LGBTQ+ w/ Dementia:
The provision of quality of care requires a complete picture of a persons everyday life & support systems. For lesbian & gay seniors, this means providing an opportunity to ‘come out’ by affirming sexual orientation & gender identity to health or home care providers
Intake forms which provide an opportunity to declare a partner of either sex & brochures & other promotional material about a service which use inclusive images can help reassure people that a service accepts & acknowledges all significant relationships
Care standards may be compromised as a consequence of negative & ill-informed staff attitudes. Education & training is critical.
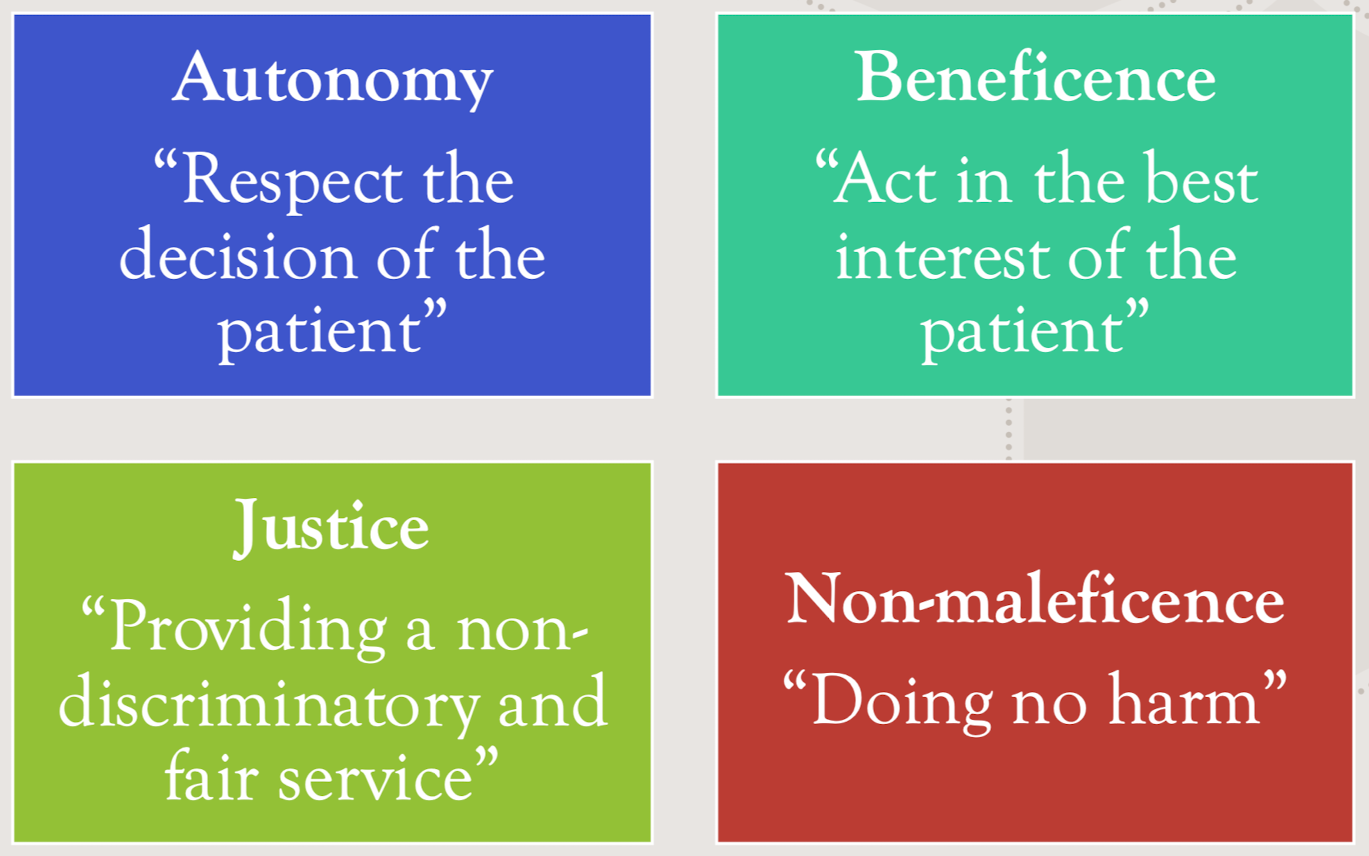
Ethics in Healthcare:
_____ is a generic term that covers several different ways of examining, understanding, & applying moral principles that guide behavior & actions to address specific problems or dilemmas.
Ethical principles provide guidance for how people reason, problem-solve, & respond
Codes of ethics from ASHA:
Ethical issues in TBI:
Ethical issues regarding TBI has largely focused on medical management, particularly concerning individuals w/ disordered consciousness & end of life considerations after TBI
Less has been written or discussed on ethical issues pertaining to living & participating in the community w/ chronic moderate to severe TBI
When making clinical decisions, do we consider the chronic challenges, & related expenses, the individual & family will face?
Ethical care demands that we avoid solutions that may be clinically ideal but practically unattainable due to expense, accessibility, or sustainability. Clinicians must also balance the potential benefits of therapy with the risk of creating unrealistic expectations for recovery, which strain both the patient & their support network
Do our clinical & research priorities align w/ the perspective of those living w/ the effects of chronic TBI?
In many cases, what is “best” for a patient living w/ TBI is tempered considerably by the resources available. Services are often “front-loaded” & often not sufficient for the potential long-term physical, behavioral, & emotional consequences one may experience over a lifespan
“Deciding what to tell a patient & family regarding prognosis”
Ethical Issues in Dementia:
Ethical difficulties arising in dementia include
Deciding when & how to communicate a diagnosis
Balancing a person’s safety w/ their need for independence & freedom
Deciding what is in the best interests of the person w/ dementia, for example when making decisions about their care & treatment
Recognizing that the needs of the person w/ dementia may sometimes conflict w/ the needs of others, especially carers
Tackling discrimination against people w/ dementia
Allocating resources to support people w/ dementia
Deciding what priority to give dementia research