Cells and Cytokines
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
14 Terms
What is Hematopoiesis?
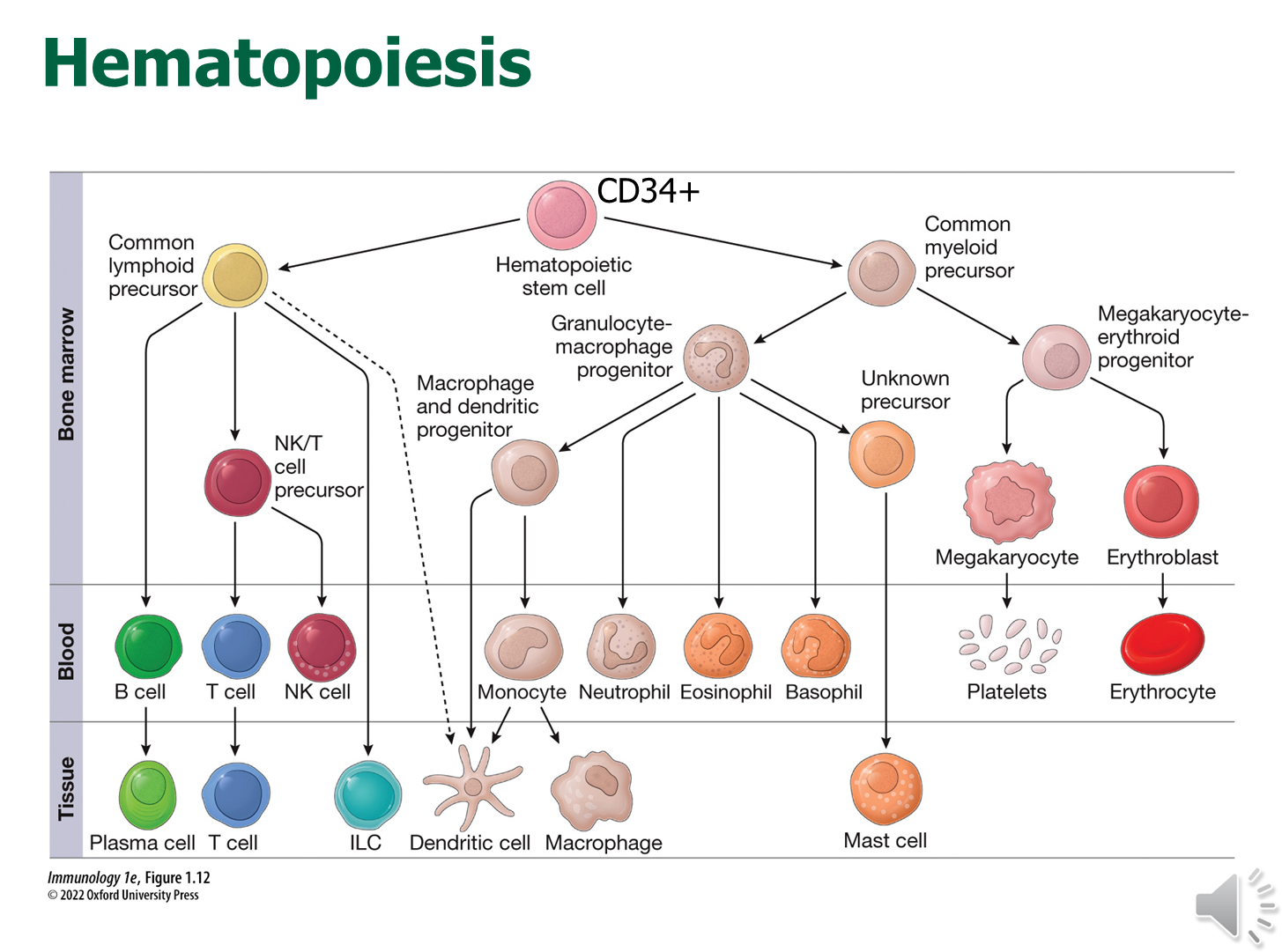
All immune cells and cytokines originate from a hematopoietic stem cell identifiable by the expression of CD34+
→ these stem cells can self-renew and can differentiate into the common lymphoid or myeloid pathways creating precursor cells that will generate cells along those lineages
1) Importantly, the development process is initiated in the bone marrow
→ T-cells however will traffic to the thymus in order to continue development
2) Following development they will enter circulation
What are the types and function of the cells of the innate immune system?
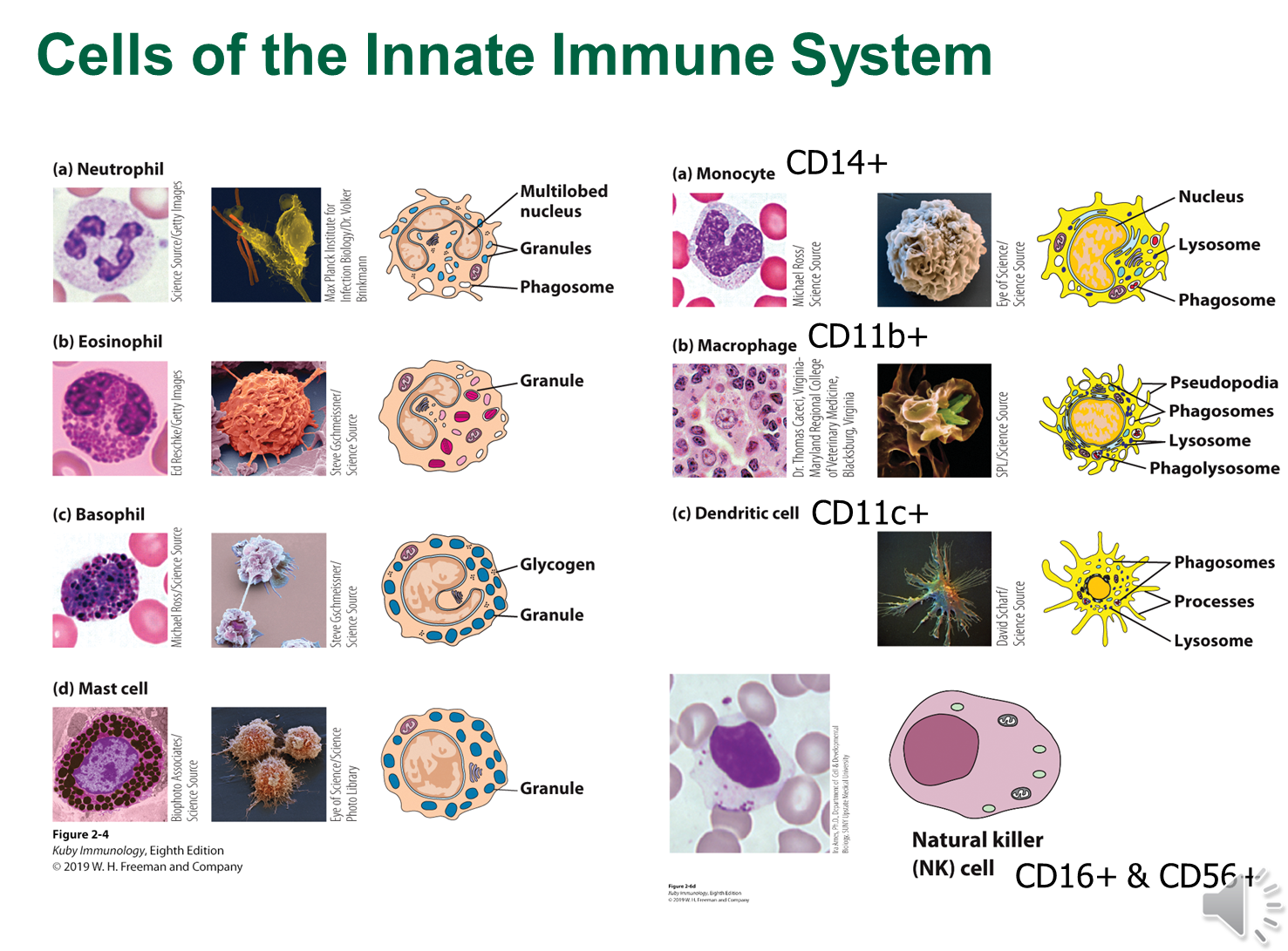
Innate Immune System is responsible for rapid recognition of foreign invaders through pattern recognition receptors
1) Macrophages and Dendritic Cells (CD11b+ and CD11c+)
→ sentinel cells in vascularized tissue and act as antigen presenting cells
→ macrophages can either be tissue resident macrophages or develop from monocytes (CD14+) that are located in circulation
→ Phagocytic cells will digest tissue and then present antigens via MHC molecules to naive T-cells
2) Neutrophils are the most numerous and will be recruited to sits of inflammation
3) Eosinophils, Basophils, and Mast Cells
→ involved in allergic inflammation
→ Mast cells are resident cells in vascularized tissue and trigger the release of histamine
4) NK Cells
→ positive for CD16+ and CD56+
→ responsible for finding abnormal cells and killing them
→ CD16 is a functional receptor that is capable of activating the NK Cells
What are the two kinds of cells in the adaptive immune system?
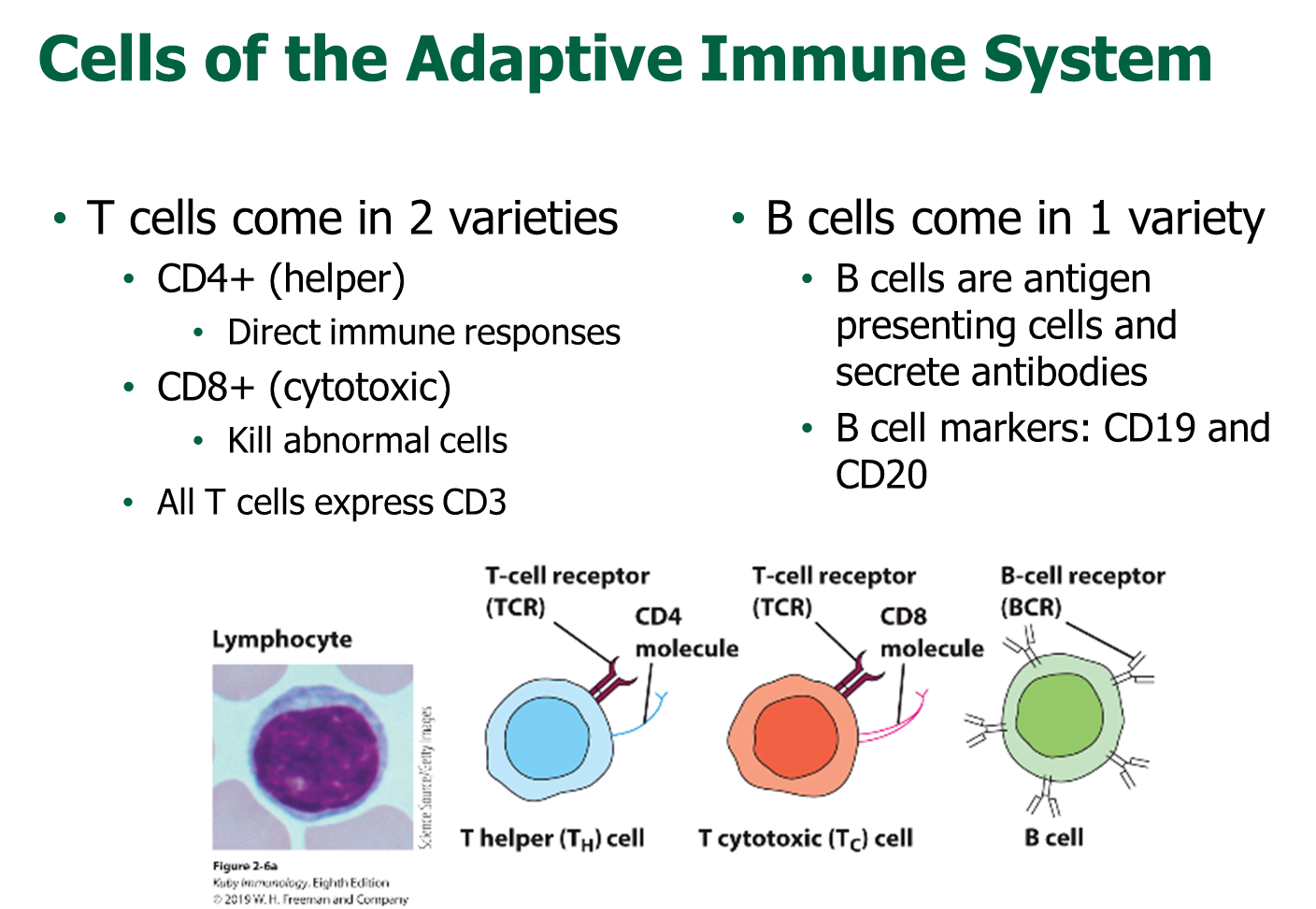
T Cells and B Cells are the two cells involved in adaptive immune response
1) T-cells come in two types with all expressing CD3
→ CD4+ T-cells are helper T-cells and are responsive to MHCII and are involved in secretion of cytokines to regulate immune response
→ CD8+ T-cells are cytotoxic and kill abnormal cells and are responsive to MHC I
2) B-cells are positive for CD19 and CD20
→ are antigen presenting cells and secrete antibodies
→ fluid from the local peripheral tissue is trafficked to the lymph node where B-cells can interact with whole antigens
3) B-cells can interact with with all different kinds of structures (nucleic acids, sugars, etc) whereas T-cells can only recognize peptides
What is the developmental process for B and T-cells
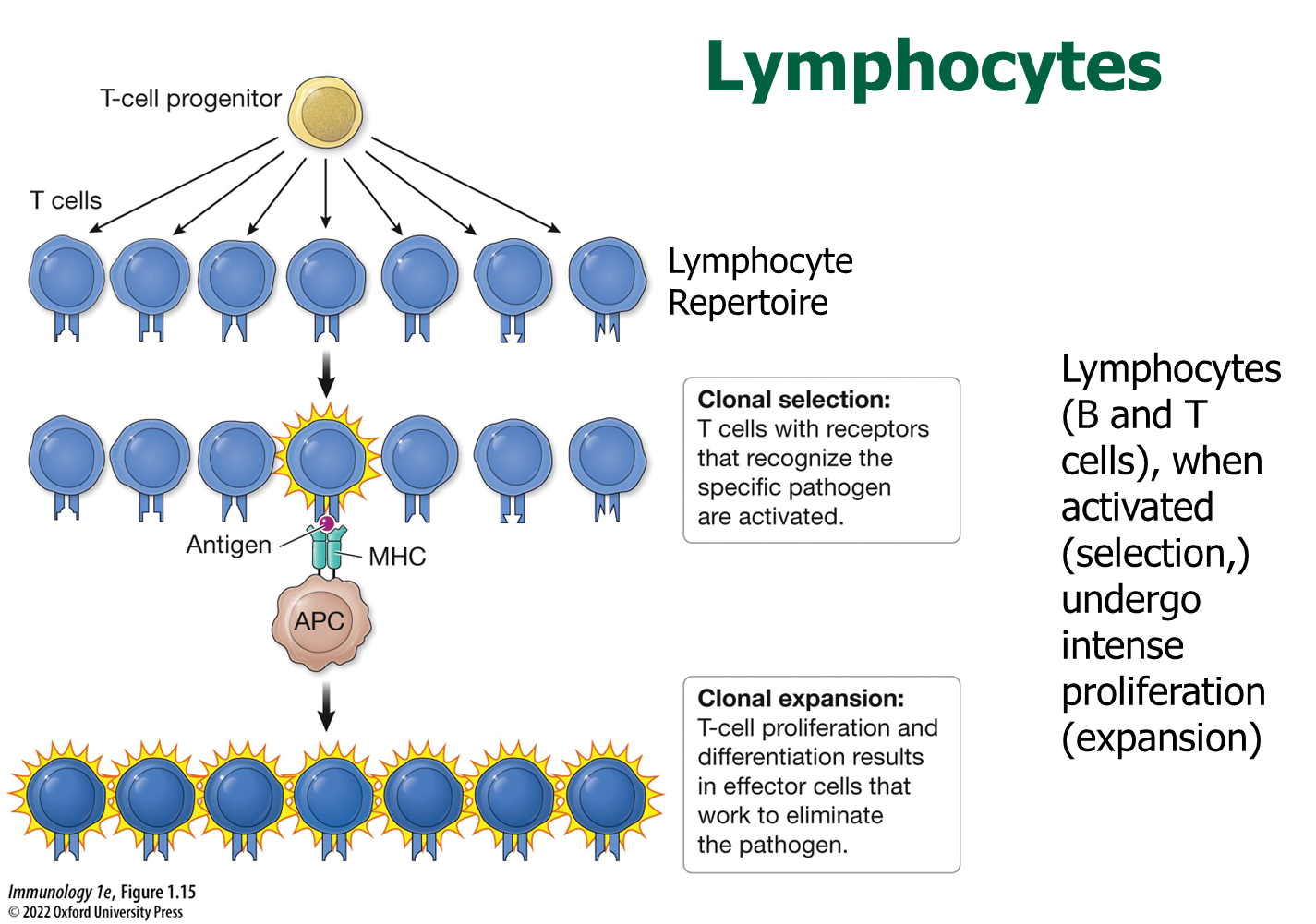
During development, B and T-cells undergo rearrangement to develop a unique B and T-cell receptor
1) The developed B or T-cell will recognize a very specific pathogen in a randomly generated pattern
→ Cells that do have a receptor capable of recognizing the pathogen are selected (clonal selection)
→ the selected cell is then proliferated in a process called clonal expansion
2) At the end of the response, these cells will undergo apoptosis except for a few cells which remain as memory cells
How are B-cell and T-cell receptors randomly generated?
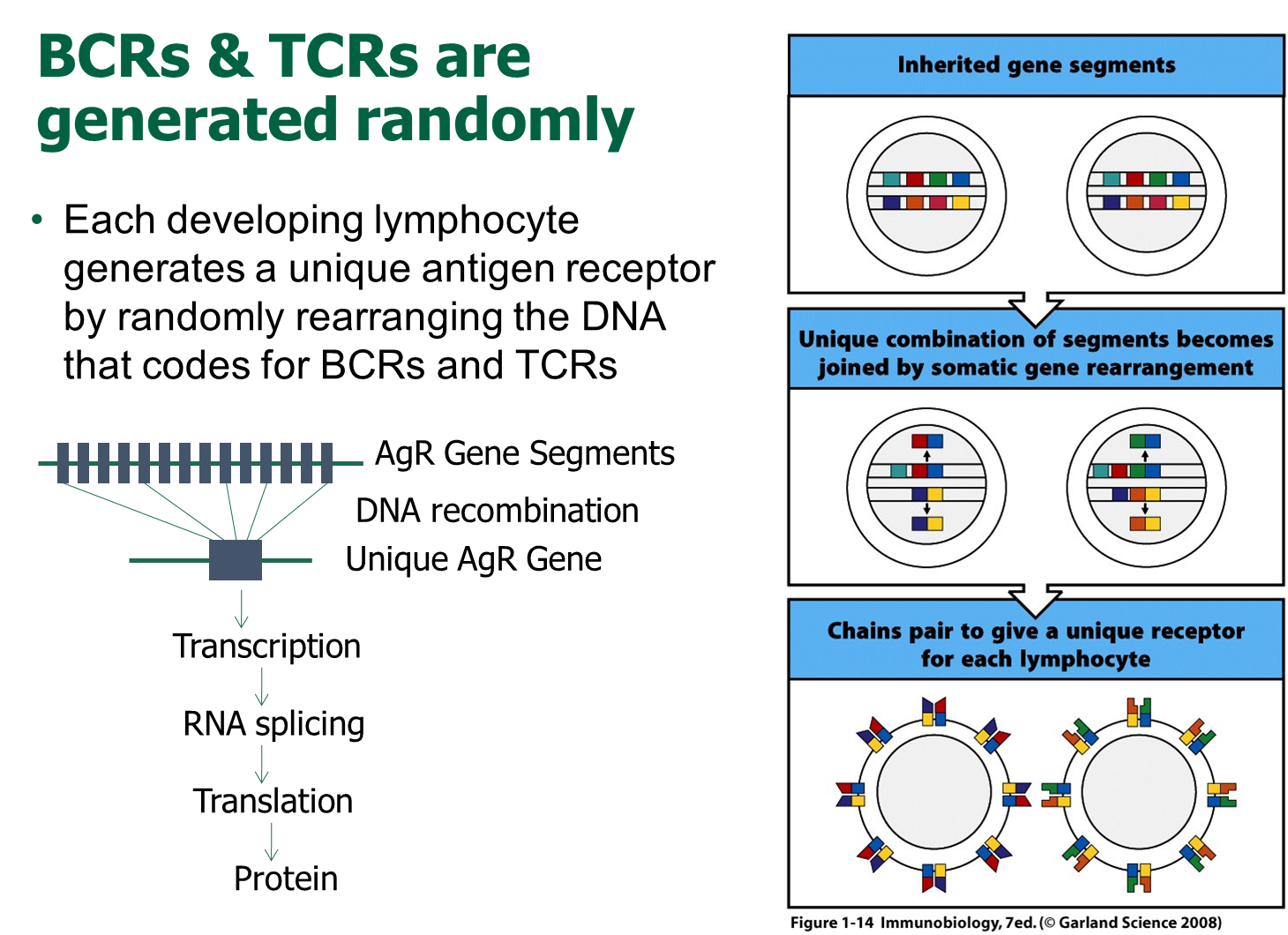
We inherit gene segments that are randomly cobbled together in order to create a unique gene for an antigen receptor
1) This gene is then transcribed and then translated into a protein that forms the receptor on B-cells and T-cells
→ this allows for us to create a bunch of different random B and T-cells
How does B-cell immunity work? What are the kinds of antibodies
B-cell or antibody mediated immunity
1) B-cells following exposure to an antigen can develop into plasma cells
→ these plasma cells will loser their B-cell receptor and will solely become responsible for antibody secretion
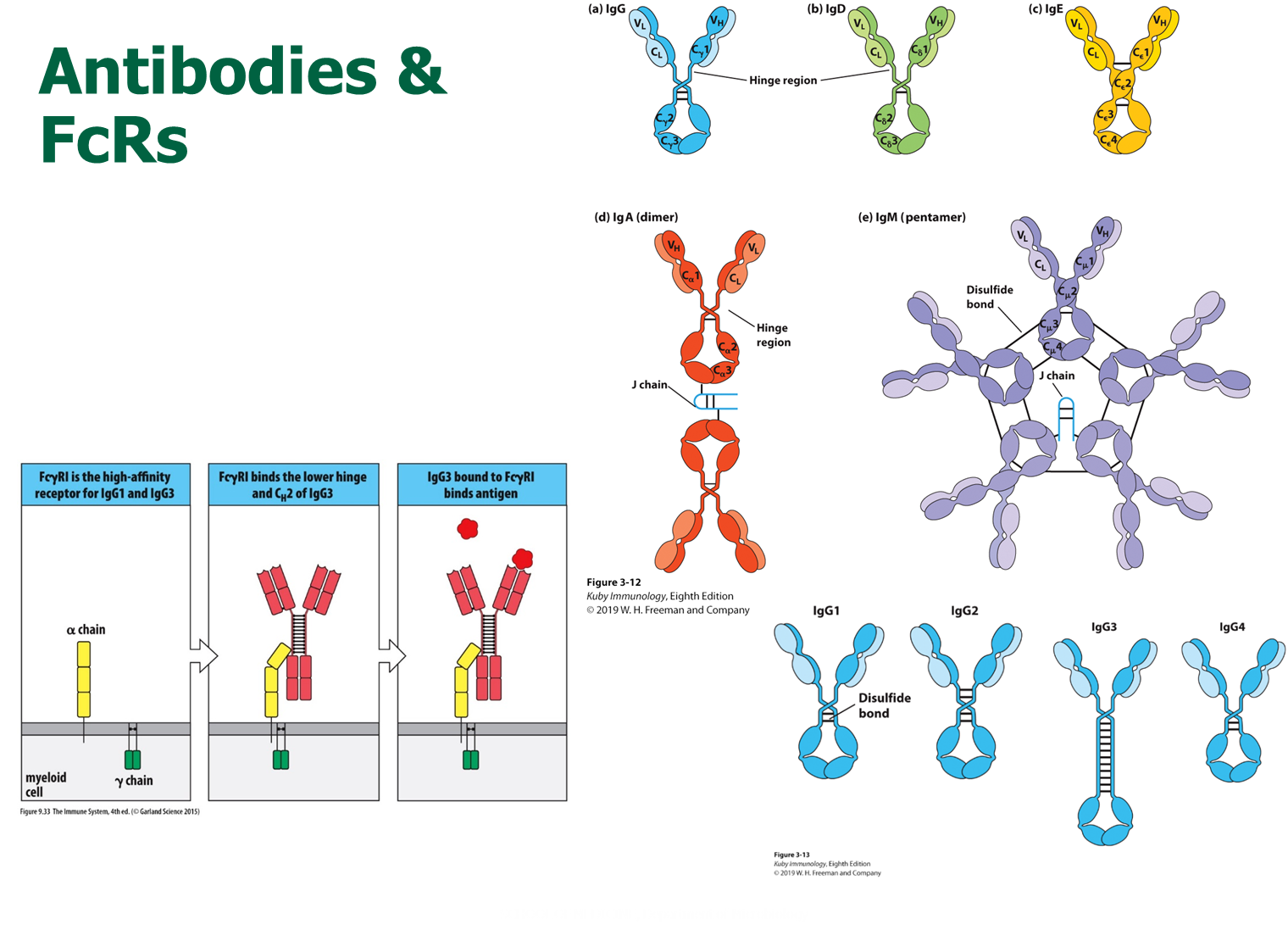
2) There are five kinds of antibodies that differ in their Fc region: IgG, IgD, IgE, IgA, IgM
→ IgA is importantly a dimer through interaction of the J-chain
→ IgM is a pentamer through interaction of the J-chain
→ IgG is a monomer and has four different subclasses with slightly different Fc regions, allowing for it to bind to a wider variety of Fc receptors
3) Antibodies will interact with Fc receptors which allow the antibodies to leave their antigen binding sites open
→ important for mediating antibody functions and regulating antibody-mediated activation of cells
What are several functions of the antibodies?

Antibodies exhibit their action primarily through interaction with the Fc receptor
→ neutralizers - binding to antigens and preventing them from reaching target (good with IgA and IgM due to their dimer and pentameric structure)
→ agglutination - clumping (good with IgA and IgM due to their dimer and pentameric structure)
→ opsonization - enhance phagocytosis (primarily IgG)
→ complement activation - leading to cell lysis via complement activity
→ antibody-dependent cell mediated cytotoxicity - activation of NK cells
→ degranulation - degranulation of mast cells (primarily IgE)
What is Naive T-cell activation? What happens to developed T-cells?
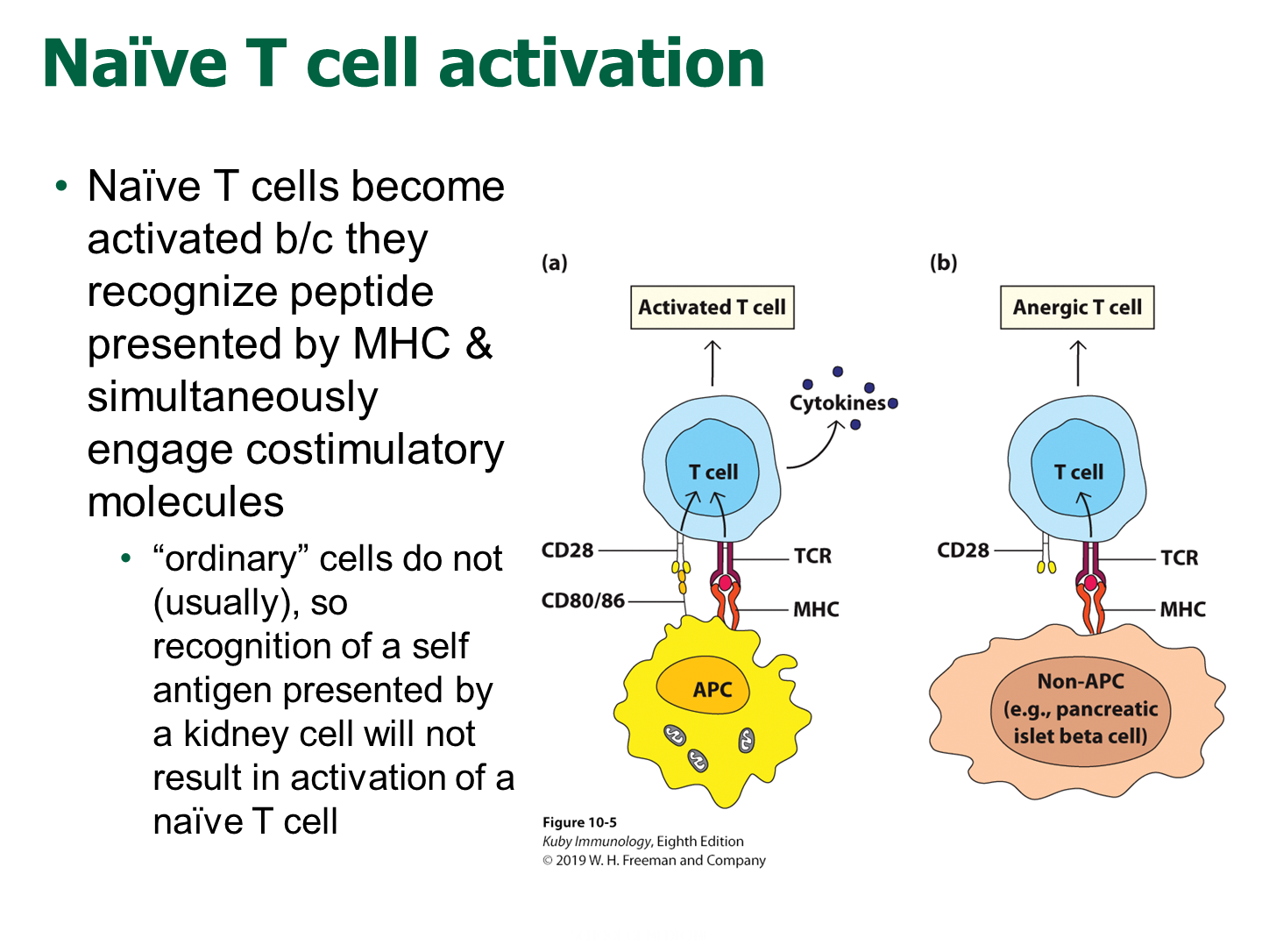
Naive T-cells are fully develop T-cells from the thymus that will travel to secondary lymphoid tissue awaiting to encounter antigen presenting cells that carry a antigen
1) Antigen Presenting Cells will also have costimulatory molecules along with their respective MHC class
→ Antigen Presenting Cells will have CD80/86 (B7 proteins) on the surface that interacts with CD28 on the T-cells that aid in activation of naive T-cells
2) Once the T-cell is activated, it can circulate and then no longer requires costimulation that is found on antigen presenting cells
→ useful in preventing autoimmunity
What are the MHC genes?

MHC are antigen presenting proteins and our body has several genes that work to present peptides
1) Our body contains three different types of MHC class I and II respectively
→ HLA-A, B, or C for MHC Class I (only has a alpha chain)
→ HLA-DP, DQ, or DR for MHC Class II (has both an alpha and beta chain
2) There are thousands of alleles in the human population for each of these HLA genes called MHC polymorphisms
→ these polymorphisms influence the kind of peptide they bind to which determines which T-cells are activated
→ the difference in the alleles are concentrated on the binding groove of the MHC, changing the affinity of the MHC molecule for a protein peptide
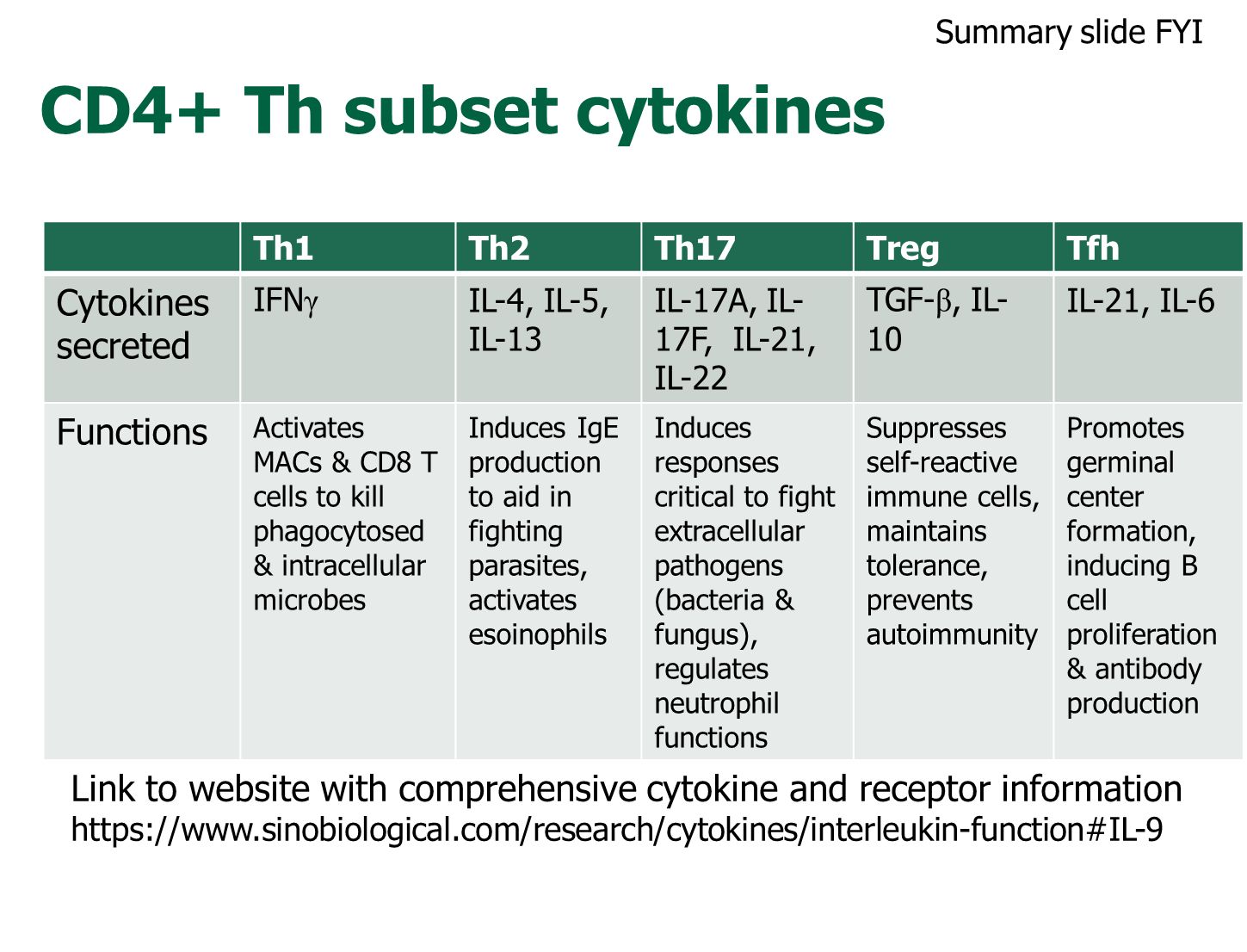
What are the subsets of CD4+ T-cells

CD4+ T-cells have the ability to differentiate into specialized subsets of T-cells in the presence of specific cytokines. Fully differentiated CD4+ T-cells secrete specific cytokines to direct activity
1) Th1
→ combats intracellular pathogens and activates macrophages via secretion of IFN-gamma and TNF
2) Th2
→ responsible for fighting worms (helminths) and activates eosinophils
→ secretes IL-4, IL-5, and IL-13
3) Th17
→ secretes IL-17A, IL-17F, and IL-22 and is used in bacterial/fungal response
4) Treg
→ secrete IL-10 and TGF-beta to suppress immune response
5) Tfh
→ secretes IL-4 and IL-21 to promote B-cell activation and germinal center formation in secondary lymphoid tissue
Which cytokines are proinflammatory, anti-inflammatory, and immunoregulatory?
Proinflammatory
→ IL-1, TNF-Alpha are master regulators of inflammation
→ IL-6 regulates the acute phase of inflammation
→ IFN-gamma makes macrophages mean (activates macrophages)
→ IL-8
→ IFN-alpha and beta - used in viral response
Anti-Inflammatory
→ IL-4 and IL-5 are antagonistic to proinflammatory cytokines
→ IL-10 and TGF-beta are immunosuppressive
Immunoregulation
→ IL-2 proliferation
→ IL-3 myelopoiesis
→ IL-7 lymphopoeisis
How do cytokines work through the JAK/STAT pathway?

Some cytokines can signal by binding to a receptor chain that is associated with a Janus kinase
→ cytokine binding will dimerize the receptor activating the Janus-kinases in order to phosphorylate the receptor chains
→ this will act as a docking site for STAT monomers in the cytoplasm, which will associate with the receptors
→ allows for STAT monomers to dimerize which will enter the nucleus and affect transcription
What are chemokines?
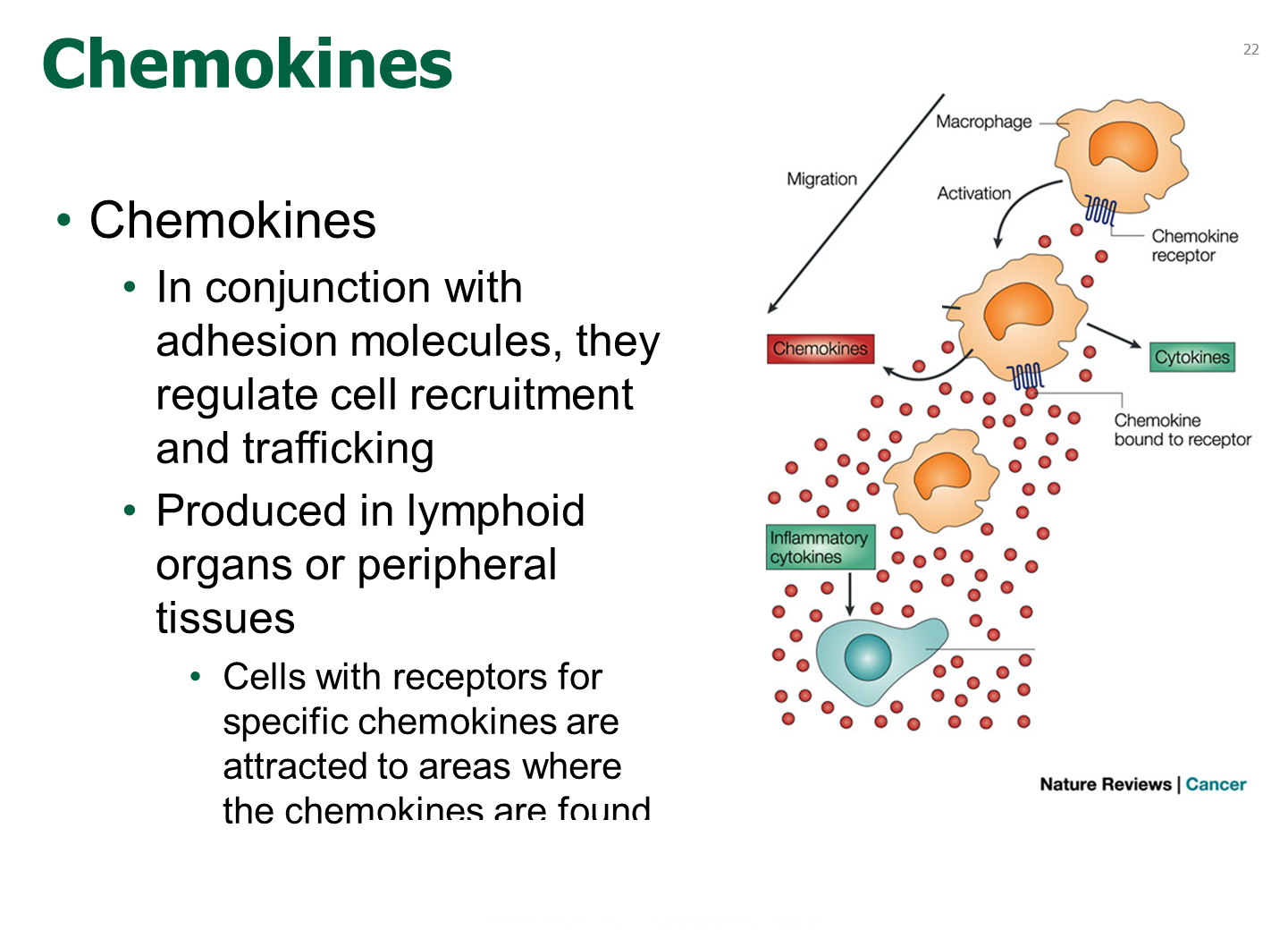
chemokines are a subset of cytokines that direct cells on where to go via chemotaxis
→ cells express chemokine receptors and will trigger cells to move based on the highest concentration of the chemokine
How do CD8+ T-cells work?
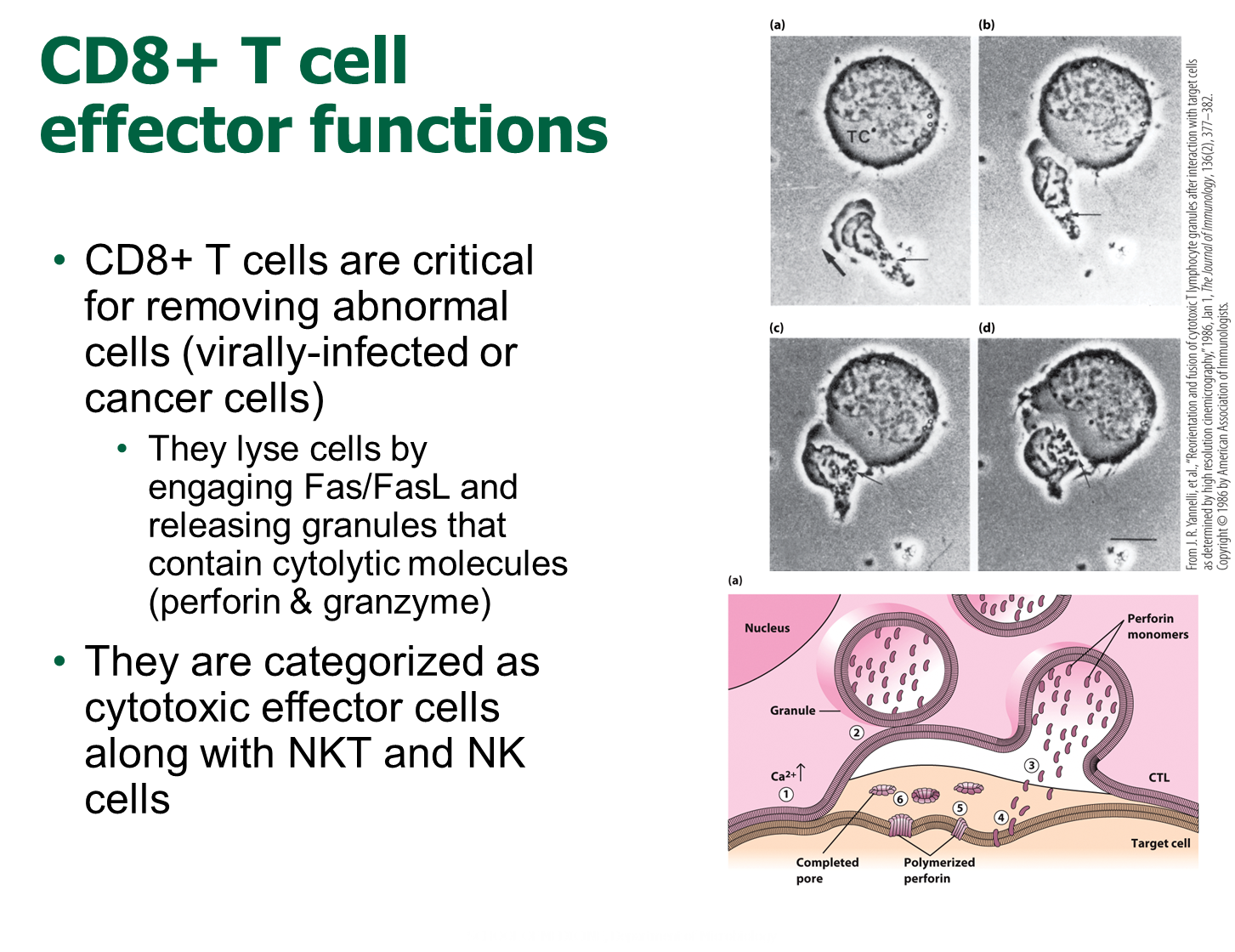
CD8+ T-cells are involved in removing virally infected cells and cancer cells
→ lyse cells via engaging Fas/FasL and releasing granules like perforin (forms pores in the cell) and granzyme (induces cell death) to kill the cells