Ch. 66 Digestion and Absorption in the GI Tract
1/28
Earn XP
Description and Tags
A comprehensive set of flashcards covering key concepts, enzymes, transporters, anatomical adaptations, and clinical correlations related to gastrointestinal digestion and absorption, formatted as question-and-answer for effective exam review.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
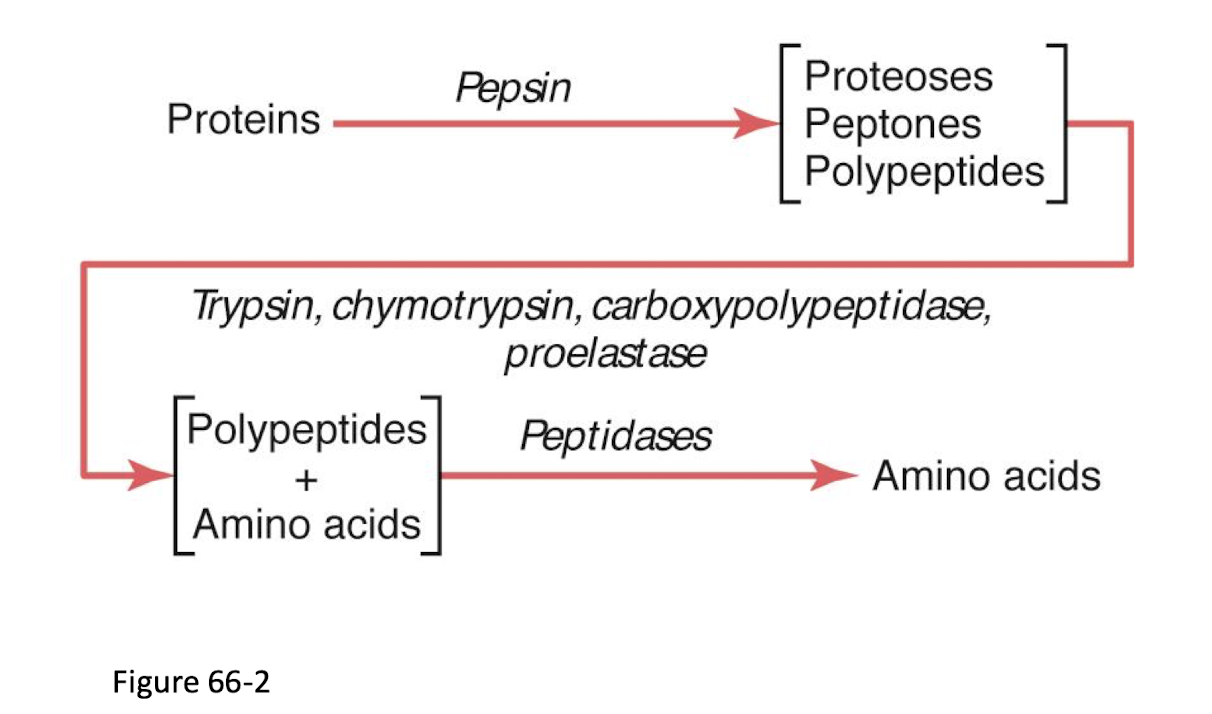
What chemical process is the basis for digestion of macronutrients?
Hydrolysis—the addition of water to break large molecules into absorbable units.
Carbos become monosaccharides
proteins become small peptides and amino acids
fats become 2-monoglycerides and fatty acids
What are the two types of digestion? Describe both
Luminal or cavity
occurs in lumen of GI trat
enzymes from salivary glands, stomach, pancreas
Membrane or contact
come in contact with brush border of enterocytes for absorption to occur
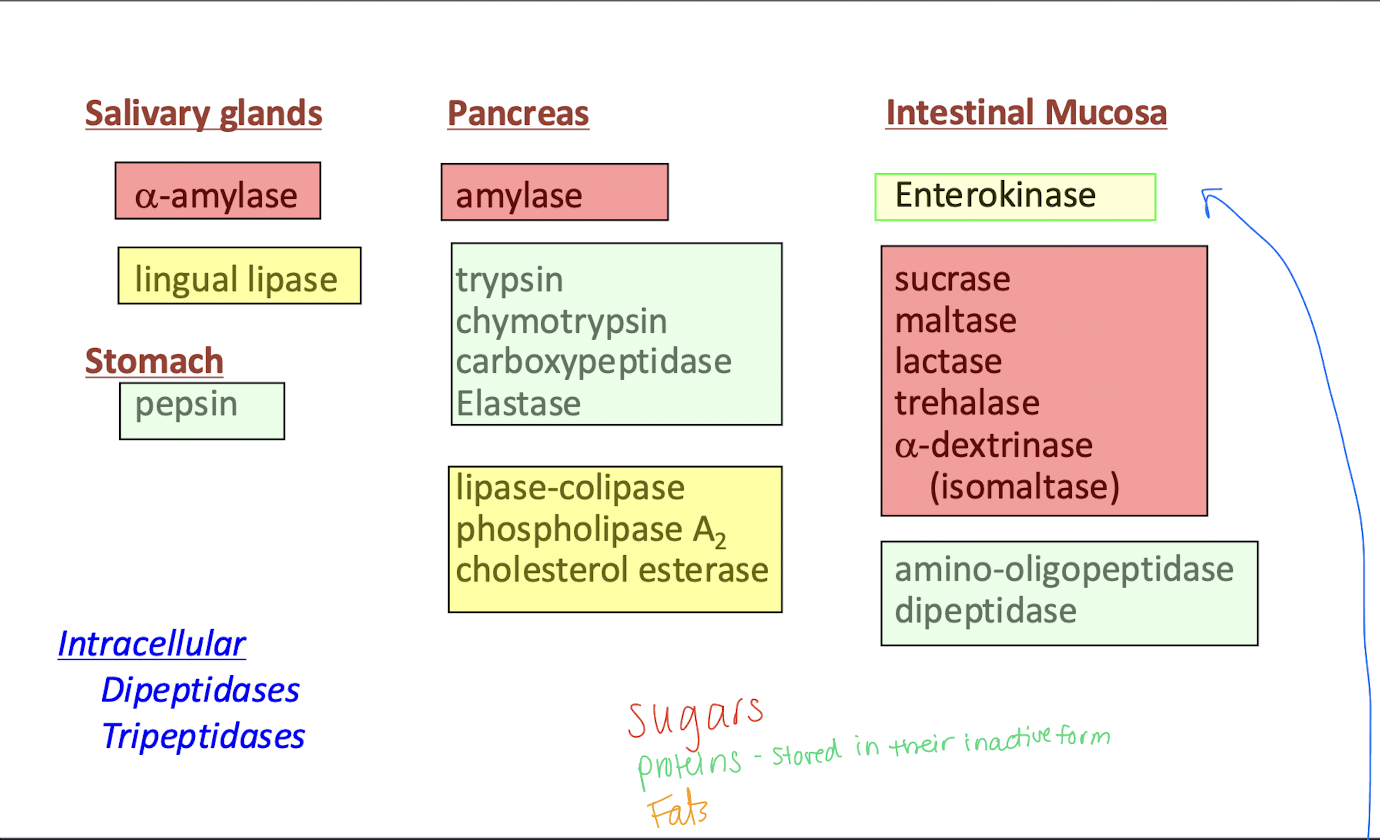
During luminal (cavital) digestion, where do the digestive enzymes originate?
Salivary glands, stomach, and pancreas.
Which phase of digestion occurs on the brush-border surface of enterocytes?
Membrane (contact) digestion.
Where can you find the enzymes listed and what do they breakdown?
Pepsin
Amylase
Enterokinase
a-amylase
elastase
stomach - proteins
pancreas - sugars
intestinal mucosa - fats and proteins
salivary glands - sugars
pancreas - proteins
What brush-border enzyme converts trypsinogen to trypsin?
Enteropeptidase (enterokinase).
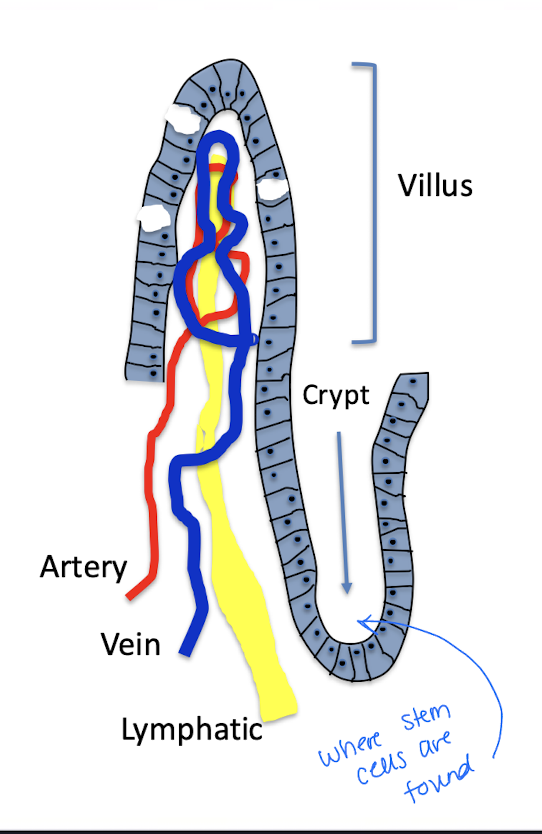
Name the three macroscopic/microscopic structures that together increase small-intestinal surface area ~1,000-fold.
Folds of Kerckring - controlled by muscularis mucosa
villi
microvilli
What is the average total surface area of the small intestine?
Approximately 250–400 m² (about a tennis court).
Which small-intestinal crypt cell type secretes antimicrobial compounds?
Paneth cells.
What are the cells of the cypt of Lieberkuhn?
Mucous cells - secrete mucus lubricating and protecting the intestinal surfaces
Intestinal stem cells - differentiate into the specialized cells of intestinal epithelium (renew throughout life)
Paneth cells - secrete antimicrobial compounds to protect against pathogens - maintains gastrointestinal barrier
Describe the life cycle of the small intestine enterocytes
Live within the villi and have cell turnover 3-6 days
cell types in villus: secretory cells, endocrine cells, goblet cells, mature absorptive epithelial cells
cells in enterocyte divide and migrate up the crypts become mature absorptive cells
enterocytes are shed into lumen to become part of ingesta to be digested and absorbed
List the four main mechanisms for transporting substances across the intestinal epithelium.
Active transport
Primary active transport
secondary active transport
Passive diffusion
facilitated diffusion
endocytosis - allows large proteins (immunoglobulins) to be absorbed in babies (does not occur in adults except in ileum for B12 absorption)
Where are bile salts and vitamin B₁₂ predominantly absorbed?
Ethanol, NSAIDS, aspirin
water and electrolytes
nutrients, vitamins, ions, water, electrolytes
Ileum
stomach
colon
duod and jejunum
Which step is rate-limiting in carbohydrate assimilation?
Absorption across the enterocyte membrane.
What enzyme initiates starch digestion in the mouth?
Salivary α-amylase.
Where does final enzymatic breakdown of lactose and sucrose occur?
At the brush border of enterocytes.
Describe carbohydrate breakdown in the small intestine
Starches
Lactose
Sucrose
Starches are broken down by a-amylase enzyme in the saliva and pancreatic amylase and become glucose
Lactose is broken down in the brush border by lactase and becomes glucose and galactose
Sucrose is broken down in the brush border by sucrase to fructose
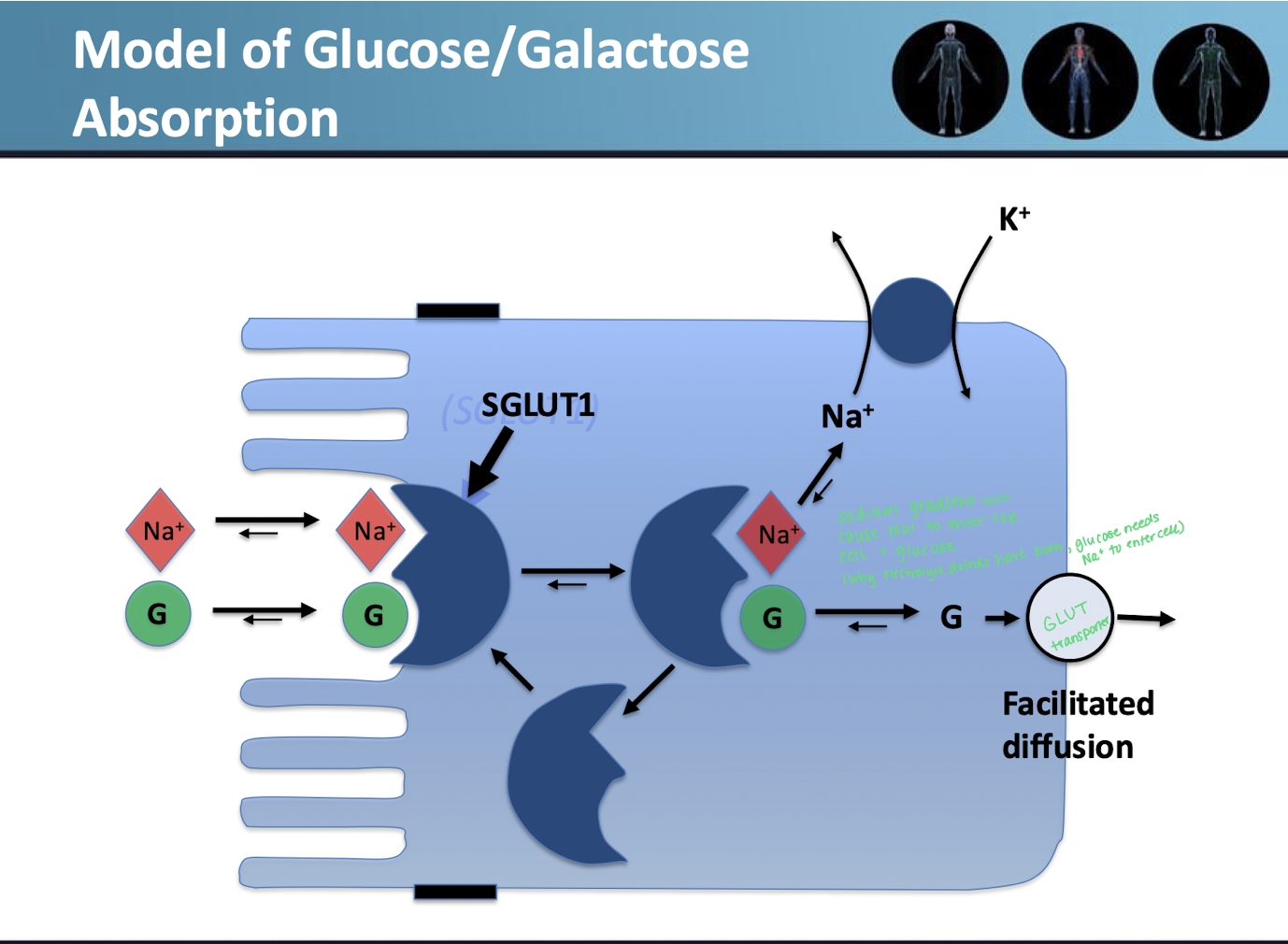
Describe carbohydrate absorption
Glucose and galactose
Fructose
both are absorbed by secondary active transport using the energy from the Na/K pump
the two will compete for a spot in the membrane carrier SodiumGLUT (SGLUT) 1
Fructose diffuses through facilitated diffusion with GLUT-5 using the concentration gradient
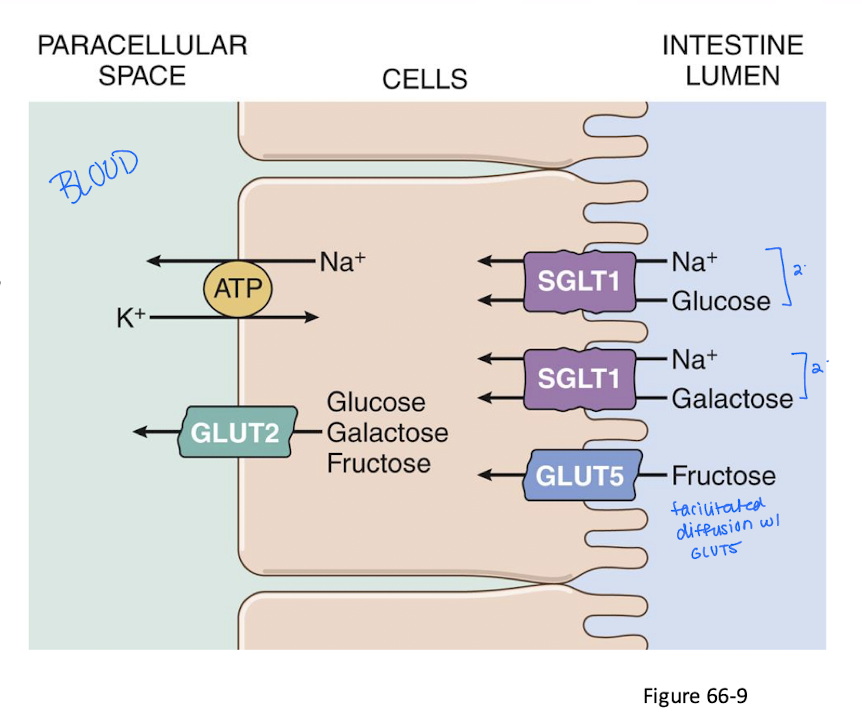
Which transporter mediates Na⁺-dependent uptake of glucose and galactose?
SGLUT-1 (secondary active cotransport).
Fructose enters enterocytes primarily via which transporter and mechanism?
GLUT-5 via facilitated diffusion (no energy required).
What carbohydrate malabsorption disorder is most common worldwide? What causes it?
Lactose intolerance (primary adult hypolactasia).
Casued by absense of brush border lactase
What are the 3 locations of digestion of proteins to amino acid occuring?
Intestinal lumen
stomach - pepsin digest collagen
Small intestine
Brush border (of intestinal lumen)
Cytoplasm of mucosal cells
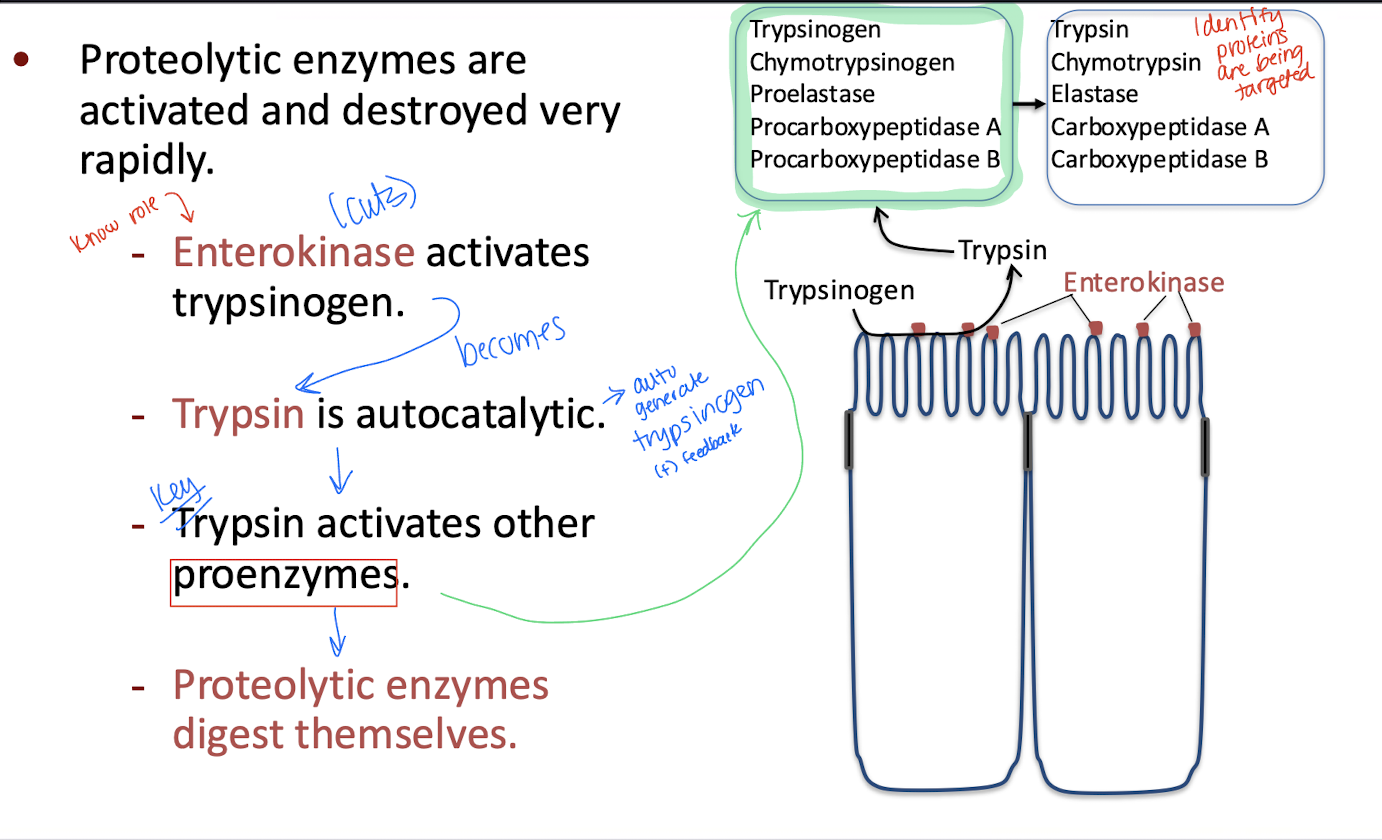
Describe the activation and destruction of proteases (enzyme that breaks down peptides and proteins)
In general, proteolytic enzymes are activated and destroyed rapidly
Enterokinase is activated by trypsinogen
Trypsinogen becomes trypsin and is autocatalytic (it can autogenerate trypsinogen (positive feedback loop)
Trypsin (THE KEY) activates other proenzymes (green box)
Proteolytic enzymes digest themselves
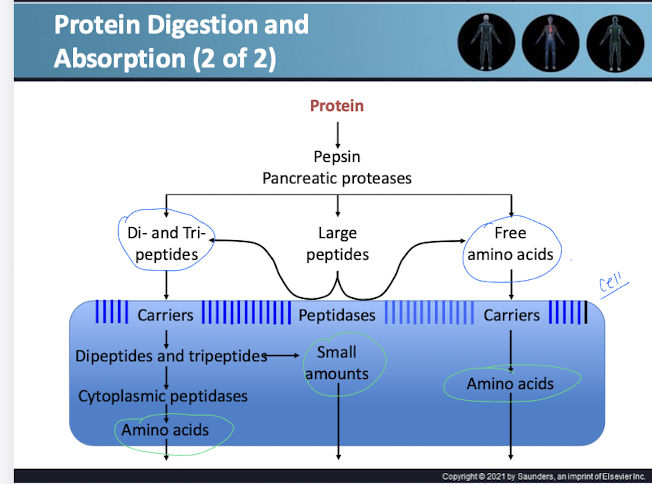
Describe the process of protein digestion
Protein is broken down by pepsin and pancreatic proteases into Di- and Tri- peptides, large peptides, and free amino acids
Di and Tri peptides enter the cell through carriers and can leave as amino acids or in small amounts
Large peptides enter the cell with peptidases and leave in small amounts
free amino acids enter the cell with a carrier and leave as amino acids
Which disease is characterized by inability to absorb neutral amino acids yet still absorbs them as di-/tri-peptides?
Hartnup disease.
Name the 3 abnormalities of protein assimilation
Pancreatic insufficiency
pancreatitis or CF
Decreased absorption leading to increased N in the stool from increased protein contents
Congenital absence of trypsin
no trypsin causes protein malabsorption
Hartnup disease
can’t absorb neutral amino acids (tryptophan) but can still be absorbed as di and tri peptides and absorbed with a carrier into the cell
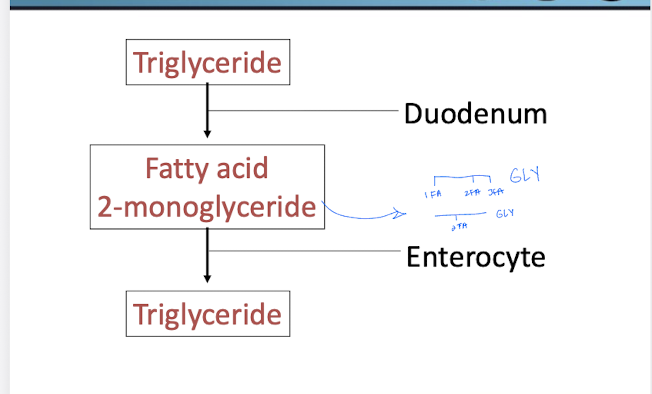
How are lipids assimilated?
Triglyceride in the duodenum will be broken down into fatty acid and 2-monoglyceride.
In the enterocyte it will be put back together as a triglyceride
MORE DETIAL
For triglycerides to be absorbed, first they are emulsified - broken down to increase surface area.
Enzymatic digestion - to become the monoglyceride and fatty acid so they can diffuse into the enterocyte
Reconstitution in enterocyte
Will bind to apoprotein and enter the lymph vessel
Which two molecules act as main emulsifying agents for dietary fat?
Bile salts and lecithin (a phospholipid).
Familial lipoprotein lipase deficiency
is a genetic disorder that results in the impaired breakdown of triglycerides due to a lack of the enzyme lipoprotein lipase. This leads to elevated levels of triglycerides in the blood, increasing the risk of pancreatitis.
hypertriglyceridemia