Cartilage Histology
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
What type of cells make up cartilage? Describe its matrix
Composed of chondrocytes and a highly specialized extracellular matrix (95%).
Describe the characteristics of cartilage
(vascularity? matrix? stress? why is it in joints? Template)
avascular.
firm but pliable matrix.
bear mechanical stress
smooth, slick surface, → used in joints
template for developing long bones.
Describe the supportive framework that cartelage forms around
Cartilage forms a supporting framework around:
Certain organs, e.g., larynx, trachea
Articulating surfaces of bone
fetal skeleton (most will be replaced by bone later)
What are the three types of cartilage?
Hyaline, Elastic, Fibrocartilage
Describe the characteristics of Hyaline Carilage (matrix property? Template? Function in growing bones? Location?)
homogenous amorphous matrix.
long bone formation template
forms epiphyseal plate in growing bones.
Location:
epiphyseal plates,
articular surfaces of synovial joints,
costal cartilages of ribcage,
cartilages of nose and larynx, tracheal rings, and bronchi.
Describe the matrix of Hyaline Cartilage
(throughout? Within? Consists of?)
Throughout matrix are lacunae
within = chondrocytes → produces hyaline cartilage matrix
Consists of:
type II collagen,
Proteoglycan aggregates containing GAGs,
Multiadhesive glycoproteins.
Describe the role of collagen in Hyaline’s cartelage
(What types makes up this?)
Four types of collagen participate in formation of a 3D meshwork of the relatively thin (~20-nm diameter) and short matrix fibrils.
Type II collagen constitutes the bulk of the fibrils.
same refractive index as ground substance.
Types IX, X &XI are also found in the matrix of hyaline cartilage.
Collagen type II refractive index + small fiber size= matrix appears as non-fibrillar, homogenous mass under light microscope.
What type of GAGs makes up ground substance of Hyaline Cartilage? function? What do glycoproteins do?
hyaluronan, chondroitin sulphate and keratin sulphate.
Aggrcan = Chondroitinn Sulphate + Keratin Sulphate; most abundant in hyaline cartilage
Negative charge = high affinity for water
Highly hydrated = gives resilience and diffusion of small metabolites.
Multiadhesive glycoproteins: influence interactions between chondrocytes and the matrix molecules,
e.g., chondronectin, fibronectin.
Describe Mesenchyme cells of Hyaline Cartilage. What happens in areas where hyaline cartilage will form
pluripotential undifferentiated cells → developes into specialized cells of cartilage
present only during early embryonic stages
In areas where hyaline cartilage will form → cells retract their stellate processes, round up, and congregate with many other mesenchyme cells.
Describe Chondroblasts of Hyaline Cartilage. (where are they derived from? Function?
From mesenchyme cells
secretes matrix material of cartilage.
As this keeps happening → surrounds themselves within matrix → now in matrix cavities called lacunae
get pushed away from each other due to continual matrix secretion.
Describe Fibroblasts of Hyaline Cartilage
(From what cells? Found in where?)
from mesenchymal cells at peripheral edge of the developing cartilage.
found in the outer fibrous layer of perichondrium.
Describe Chondrogenic cells of Hyaline Cartilage (where are they from? What do they become? Where are they found)
From mesenchyme cells
becomes chondroblasts
Found in inner cellular layer of the perichondrium
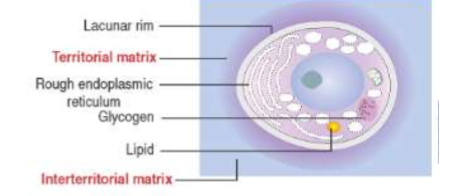
Describe Chondrocytes of Hyaline Cartilage; Differentiate between territorial and interterritorial matrix.
former chondroblasts that are surrounded by compartmentalized ECM
Territorial matrix = matrix that encloses isogenous groups
forms blueish structure w/ hematoxylin and eosin stains
Interterritorial matrix: surrounds the territorial matrix; seperates isogenous groups
NOTE: Chondrocyte cell body fills the space of the lacuna in vivo, but shrinkage of the cell bodies occurs during tissue preparations for light microscopy. This results in each lacuna appearing as a cavity with a cell body and much empty space.
What are isogenous groups? What do they represent? What happens as the matrix is being produced?
Chondrocytes are distributed either singularly or as clusters of chondrocytes within lacunae; these are isogenous groups.
Chondrocytes in isogenous groups represent the recently divided cells.
As the newly divided cells produce the matrix that surrounds them, they are dispersed.
NOTE: Chondrocytes that are active in matrix production stain
intensely basophilic due to many Golgi apparatus, rER,
secretory granules, vesicles, etc
Describe the perichondrium of Cartilage
(characteristics?, layers? How does it form)
Dense, irregular, collagenous, CT membrane that surrounds cartilage
has outer fibrous layer and inner chondrogenic layer.
Formation: outermost area of mesenchyme condenses → forms a fibrous sheath around the developing cartilage.
What does the fibrous (outer) layer of perichondrium consists of?
collagen fibers( type 1) and associated fibroblasts.
What is the Chondrogenic layer of periosteum? Consists of?
inner cellular layer of perichondrium
consists of chondroblasts and chondrogenic cells.
Chondrogenic cells → chondroblasts → secrete cartilage matrix → surround themselves → now called chondrocytes
It is from this layer that cartilage grows
appositionally.
What is the first indication of cell differentiation; describe the location of cartilage differentation during developemt stage.
rounding up of mesenchymal cells → multiply rapidly → densely packed.
During embryonic development, cartilage differentiation takes place from center outwards,
central cells = chondrocytes,
peripheral cells = chondroblasts.
NOTE: both chondrocytes and chondroblasts have basophilic cytoplasm rich in rER for collagen synthesis
What are the two ways in which cartilage tissue grow? Compare/contrast them
interstitial growth
mitotic division of preexisting chondrocytes from within the cartilage (inside the lacunae)
occurs in cartilaginous regions within long bones
important for increasing the length of the long bones.
appositional growth,
chondroblast differentiation from progenitor cells in the perichondrium.
seen mostly during postnatal development
In both cases, the synthesis of the matrix contributes greatly to the growth of the cartilage.
What is articular cartilage? Characteristics?
(what two things does it lacks?)
Hyaline cartilage that covers the articular surfaces of movable joints
Lacks an epithelial lining.
Lacks a perichondrium.
What is the 2 function of Articular cartilage
(what is the lubrication fluid made up of? What produce this?)
shock absorber.
Provides a lubricated surface for movable joints.
lubrication fluid = hyaluronic acid + immunoglobulins + lysosomal enzymes, (particularly collagenase) + glycoproteins
produced by the synovial lining of joint capsule
Why is the renewal process of mature articular cartilage slow? What type of growth occurs here? What needs to happen as articular surfaces becomes worn out
because of stable collagen type II fibers and the long half-life of proteoglycan molecules
Interstitial growth occurs in articular cartilage because no perichondrium.
As articular surfaces become worn out, interstitial growth is needed for cartilage replacement
Define epiphyseal plate. Define endochondral bone
Epiphyseal plate: where long bone increases in length during development by interstitial growth
Endochondral bone: begins as a cartilaginous model (template) that grows via interstitial growth
Why does cartilage have limited ability to repair? Exception? What happens in older people
Avascular
Immobility of chondrocytes
Limited ability of mature chondrocytes to proliferate.
Exception: repair can occur if defect involves perichondrium,
perichondrium has pluripotent progenitor cells
involves production of dense collagenous connective tissue, and a few cartilage cells may be produced.
Hyaline cartilage is prone to calcification, can be seen in
older individuals.