neural substrates exam 2 (chapters 5-8)
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
spinal cord form (external)
housed in boney vertebral column
5 sections
cervical, thoracic, lumbar, sacral, and coccygeal
spinal nerves emerge from the spinal cord
spinal cord form (internal)
information superhighway conveying motor (efferent) and sensory (afferent) information between brain and body
4 fiber types
GSE fibers: to skeletal muscles
GVE fibers: to smooth muscle, heart and glands
GSA fibers: from skin
GVA fibers: from lungs and digestive tract
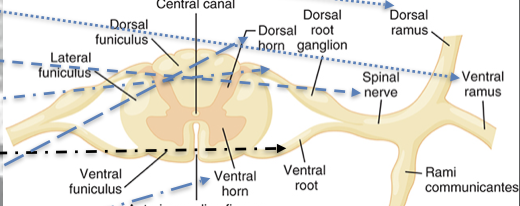
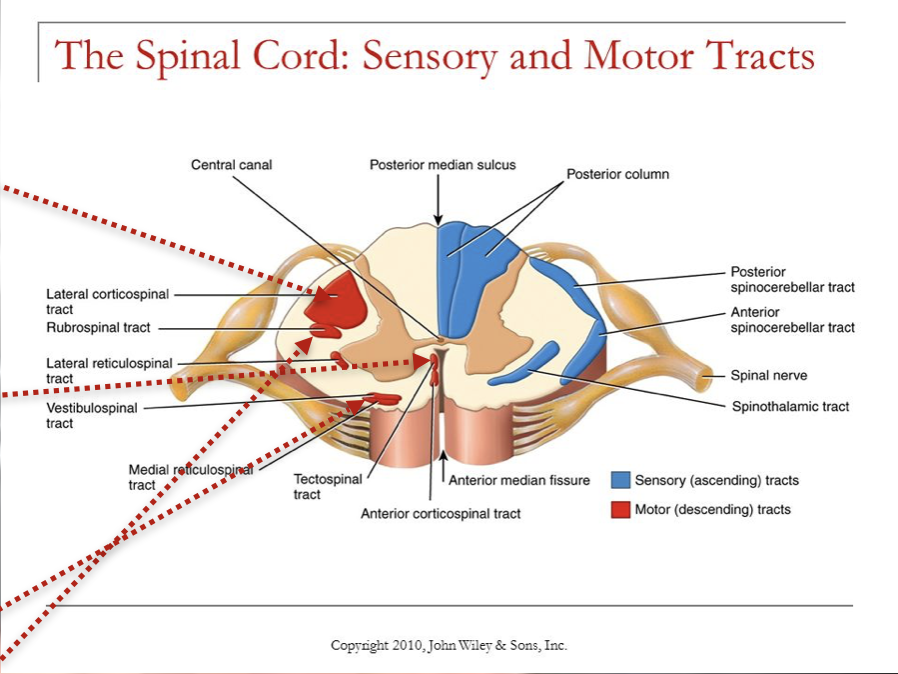
major landmarks of spinal cord
dorsal ramus
ventral ramus
spinal nerve
dorsal root
ventral root
dorsal horn
ventral horn
anterior median fissure
dorsal funiculus
lateral funiculus
ventral funiculus
major motor tracts
lateral corticospinal- contralateal body movement
anterior (or ventral) corticospinal: trunk muscles
rubrospinal: flexor tone
vestibulospinal: extensor tone
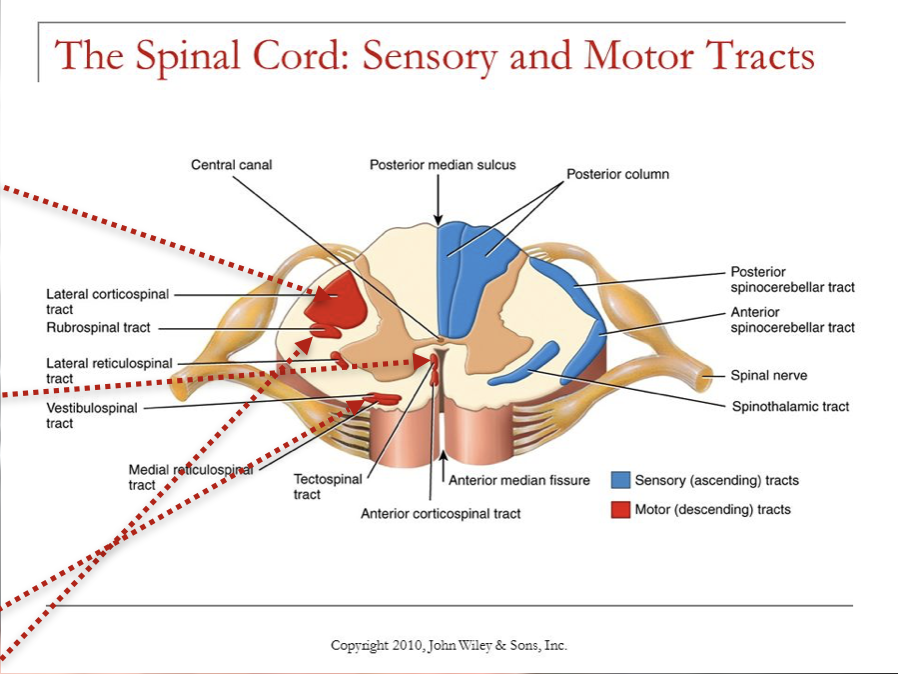
major sensory tracts
dorsal columns: fine touch, pressure, proprioception
spinothalamic : pain, temperature, crude touch
spinocerebellar: proprioception
function of the spinal cord
relaying efferent and afferent information between body and brain and mediating reflexes through the reflex arc

paraplegia/paraparesis
involves legs
quadriplegia/quadriparesis
involves arms and legs
spina bifida
neural tube defect that occurs during development in the womb
multiple severities
results in lower spinal cord damage
paraparesis and bowel and bladder issues
myelitis
inflammation of the spinal cord
can be caused y virus, bacteria, fungi, parasites, and toxic agents
different types:
poliomyelitis: affects gray matter (motor loss)
leukomyelitis: affects white matter (sensory loss)
transverse myelitis: affects both gray and white matter (motor and sensory loss)
peripheral neuropathy
inflammation of the peripheral nervous system
results in degeneration of the spinal nerves, typically in the feet
caused by untreated diabetes, toxins, infections, and nutritional issues
paresthesia or anesthesia
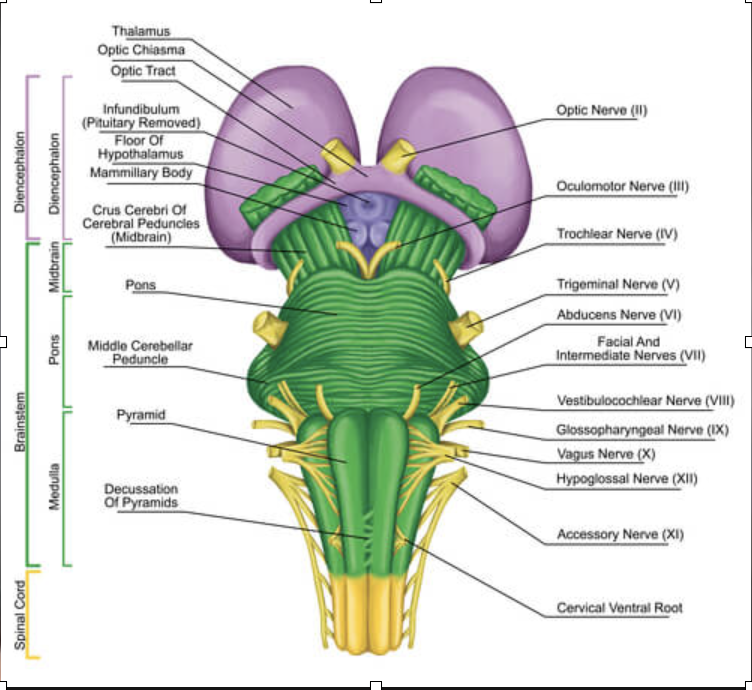
function of the brainstem
regulating major life functions, mediating head and neck reflexes via cranial nerve, regulating alertness and wakefulness
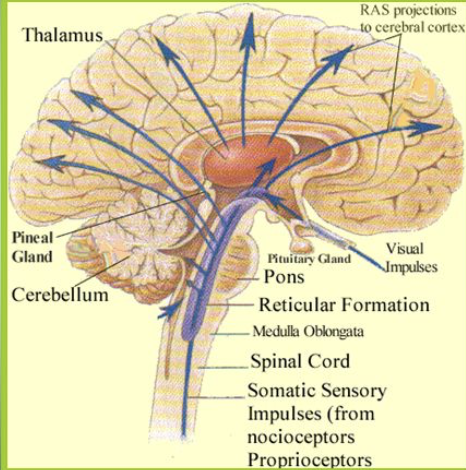
ARAS (ascending reticular activation system)
receives fibers from the sensory pathways via long ascending spinal tracts
alertness, maintenance of attention and wakefulness
emotional reactions, important in learning processes
tumor or lesion- sleeping sickness or coma
tegmental regions (brainstem)
reticular formation- consciousness
inferior olivary nucleus- motor movement control/coordination
red nucleus- flexor tone
nontegmental regions (brainstem)
tectum- superior (vision) and inferior (hearing) colliculi
cerebral peduncles
ventral pons- motor movement error correction
“ On Old Olympus Towering Top A Fin And German Viewed Some Hops”
olfactory
optic
oculomotor
trochlear
trigeminal
abducens
facial
vestibulocochlear
glossopharyngeal
vagus
spinal accessory
hypoglossal
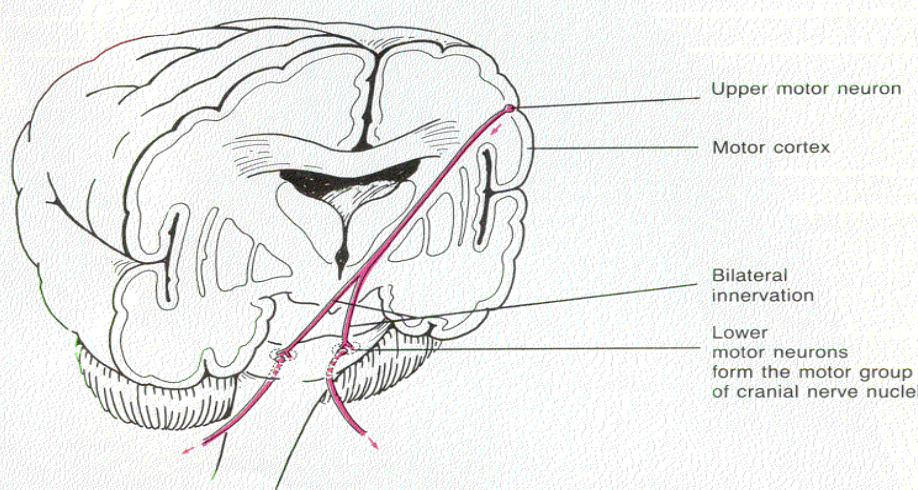
motor cranial nerves are composed of 2 major neurons which are:
upper motor neuron and lower motor neuron
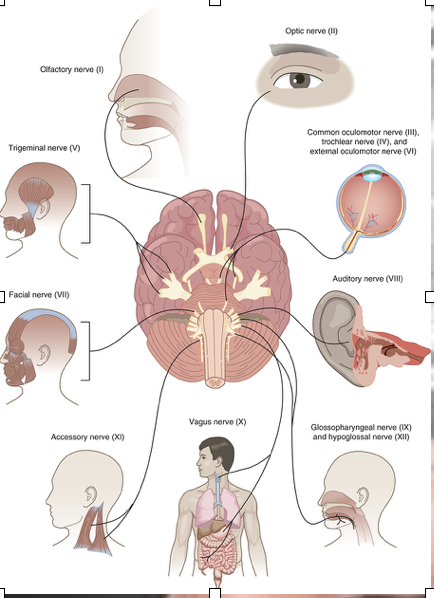
olfactory nerve
origin: olfactory bulb
function: smell
problems: anosmia
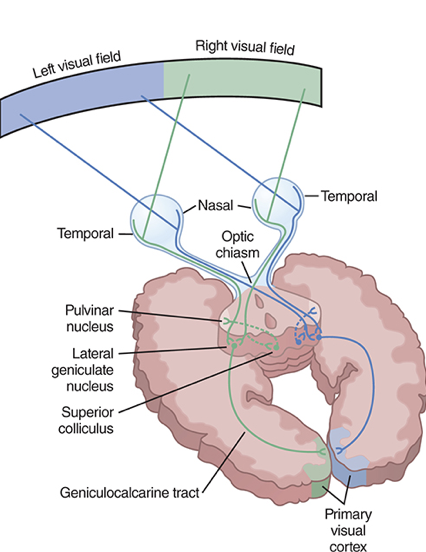
optic nerve
origin: retina
function: vision
problem(s): visual disturbances and loss of vision
right homonymous hemianopsia
loss of right visual field in both eyes
oculomotor nerve
origin: midbrain
function:
GSE: moves eyes left and right; control eyelid
GVE: pupil constrictor
problem: loss of pupillary light reflex; ptosis
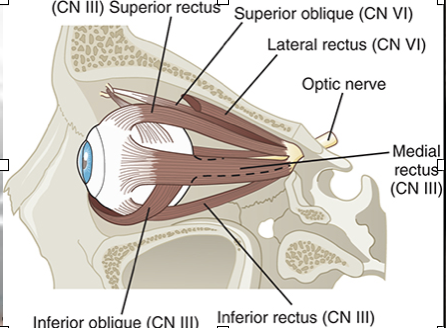
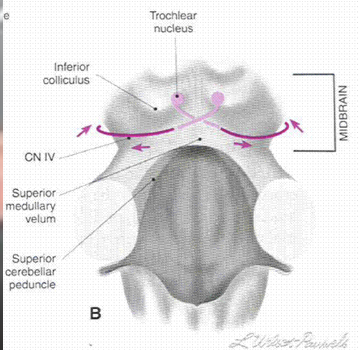
trochlear nerve
origin: midbrain
function:
GSE: moves eyes up and down
problem(s): nystagmus; difficulty moving eyes up and down
trigeminal nerve
origin: pons
function:
GSA: touch, pain, temp. and vibration for face, anterior 2/3 of tongue
GSE: muscles of mastication
problem(s): loss of facial sensations (trigeminal neuralgia); difficulty chewing; abnormal jaw-jerk reflex
3 branches:
ophthalmic
maxillary
mandibular

abducens nerve
origin: pons
function:
GSE: rotates eyes out
problem(s): eye rotates in (strabismus) and diplopia; nystagmus
facial nerve
origin: pons
function:
GVE: muscles of facial expression
GVE: salivary glands (sublingual, submandibular) and lacrimal glands (tears)
GSA: sensation near ears
SVA: taste in anterior 2/3 of tongue
problem(s): facial paralysis/paresis; taste loss
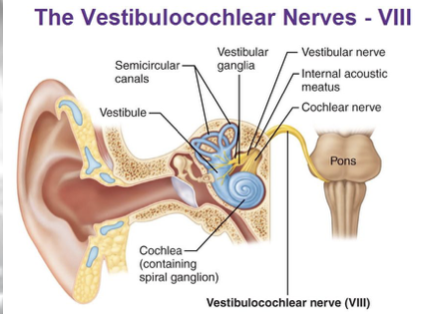
vestibulocochlear nerve
origin: pons/medulla junction
function:
SSA: hearing and balance
problem(s): hearing loss; balance problems; acoustic neuroma
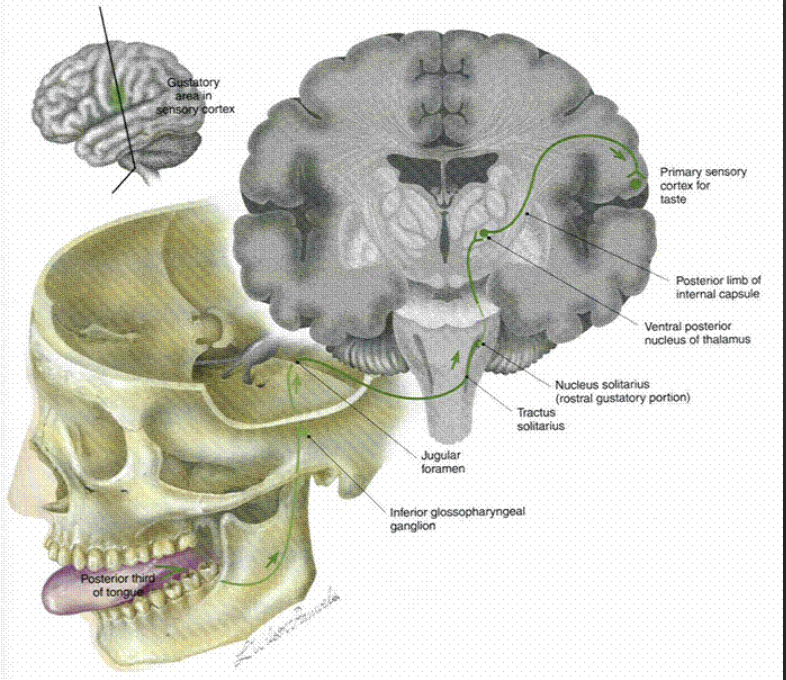
glossopharyngeal nerve
origin: pons/medulla junction
function:
SVE: pharyngeal movement
GVE: parotid gland (salivation)
GVA: middle ear, pharynx, posterior 1/3 of tongue
SVA: taste on posterior 1/3 of tongue
problem(s): absent gag and swallow reflex; loss of taste; loss of pharyngeal movement
SVE
innervates muscles of swallowing
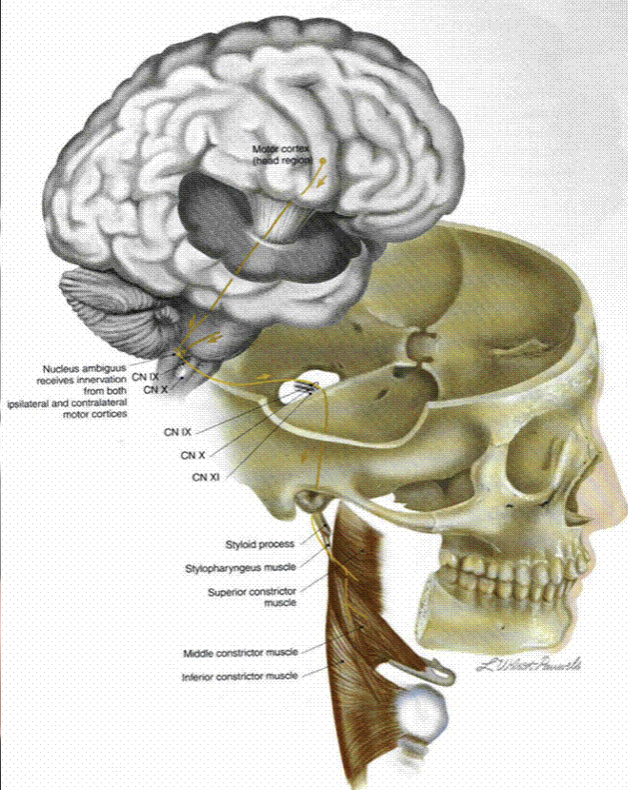
GVE
innervates parotid gland
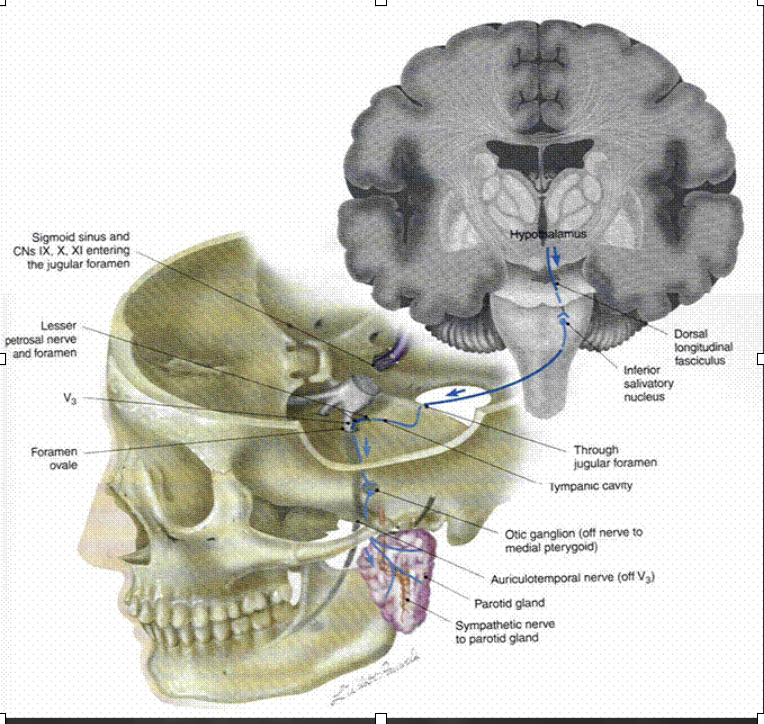
GVA
middle ear, pharynx, posterior 1/3 of tongue
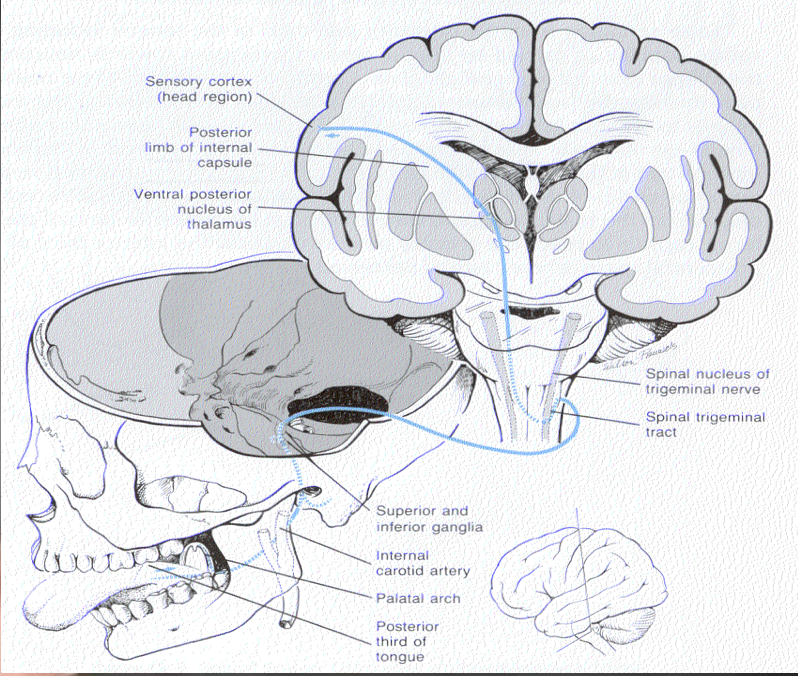
SVA
taste on posterior 1/3 of tongue
vagus nerve
origin: medulla
function:
SVE: Supplies the voluntary muscles of the pharynx and most of the larynx, as well as one extrinsic muscle of the tongue.
GVE: Parasympathetic innervation of the smooth muscle and glands of the pharynx, larynx, and viscera of the thorax and abdomen.
GSA: Provides general sensory information from the skin of the back of the ear and external auditory meatus, parts of the external surface of the tympanic membrane, and the pharynx.
GVA: Provides visceral sensory information from the larynx, esophagus, trachea, and abdominal and thoracic viscera, as well as the stretch receptors of the aortic arch and chemoreceptors of the aortic bodies
SVA: Taste from epiglottis and pharynx
problem: absent gag and swallow reflex; loss of velar movement; loss of voice
3 major branches of the SVE
pharyngeal branch
superior laryngeal nerve
recurrent laryngeal nerve
pharyngeal branch
Superior constrictor muscle
Middle constrictor muscle
Inferior constrictor muscle
Levator palatini muscle
Salpingopharyngeus muscle
Palatopharyngeus muscle
Palatoglossus muscle (of the tongue)
superior laryngeal nerve
External Laryngeal Nerve:
Inferior constrictor muscle
Cricothyroid muscle
Internal Laryngeal Nerve:
Sensory to the larynx
recurrent laryngeal nerve (RLN)
All intrinsic muscles of the larynx (except Cricothyroid)
These muscles control the movements of the vocal folds.
right RLN
hooks posteriorly around the subclavian artery and also ascends in the groove between the esophagus and trachea.
left RLN
Longer; nerve loops posteriorly around the aortic arch and ascends to enter the groove between the esophagus and trachea.
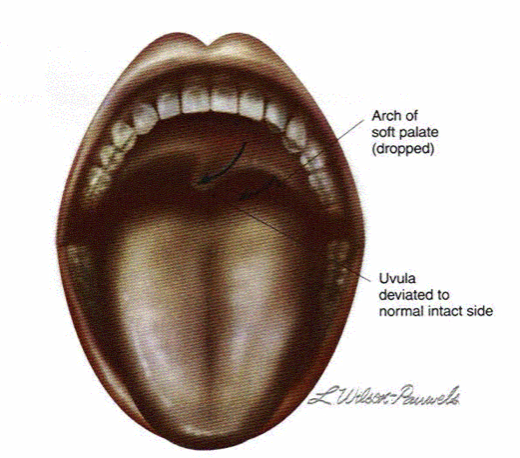
consequences of LMN (lower motor neuron) damage
difficulty swallowing
inability to elevate soft palate on affected side; paralysis of levator palatini muscle; pharyngeal muscles
soft palate droops on affected side and uvula deviates opposite affected side
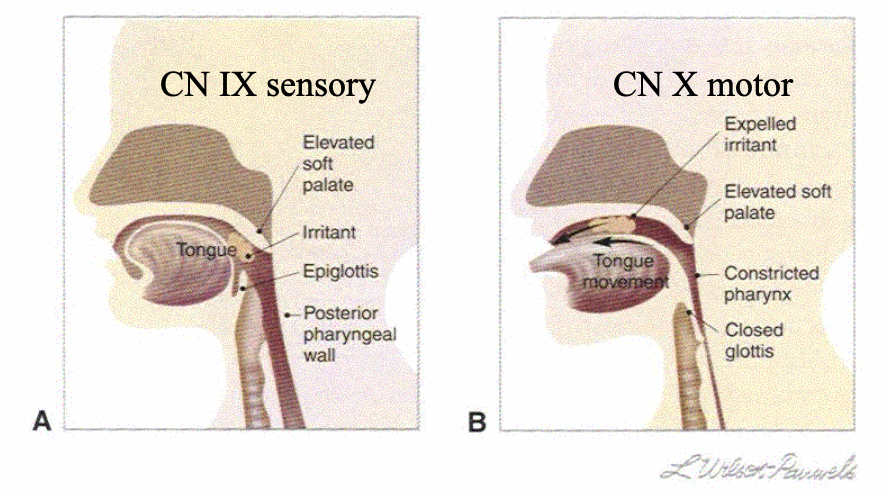
gag reflex process
Sensory input → Glossopharyngeal nerve → Medulla → Motor output via Vagus nerve → Gag response
Stimulus: The gag reflex is triggered when something touches the back of the throat, soft palate, or the back of the tongue.
Afferent Pathway: Sensory receptors in the throat (e.g., pharyngeal and palatal areas) send signals to the glossopharyngeal nerve (CN IX).
CNS Processing: The signal is relayed to the medulla oblongata (brainstem), which processes the sensory input.
Efferent Pathway: The motor response is carried via the vagus nerve (CN X) to the muscles of the soft palate, pharynx, and larynx, causing contraction and the reflexive gagging response.
Action: This causes a rapid contraction of the muscles, leading to a gagging sensation, which helps expel or prevent the object from entering the airway.
spinal accessory nerve
origin: medulla and spinal cord
function:
GSE: neck and shoulder muscles
problem(s): droopy shoulder; movement of neck
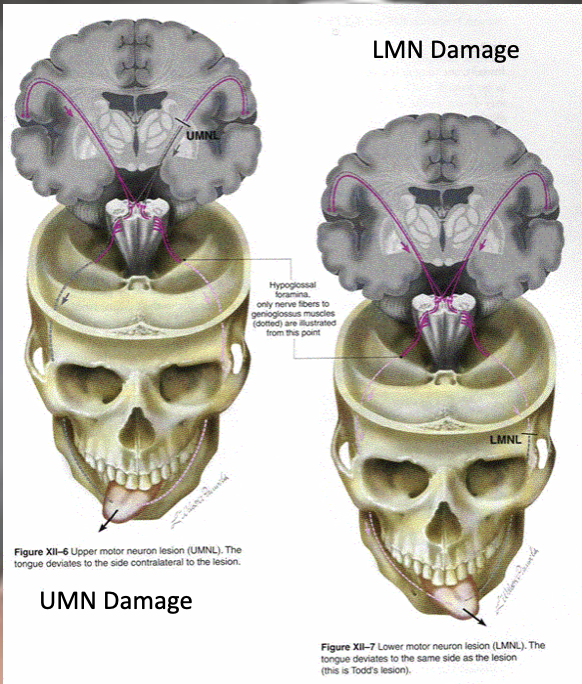
hypoglossal nerve
origin: medulla
function:
GSE: muscles of tongue
UMN innervate predominantly the contralateral hypoglossal nuclear
problem(s): loss of tongue movement; tongue fasciculations, tongue atrophy
consequences of UMN and LMN damage
deviated tongue
cerebellum functions
motor
planning, monitoring, and correction of motor movement using sensory feedback
fine motor activity
monitors head and body position
learning new motor skills
linguistic
perception of speech/language, verbal working memory, verbal fluency, grammar processing, writing, and reading
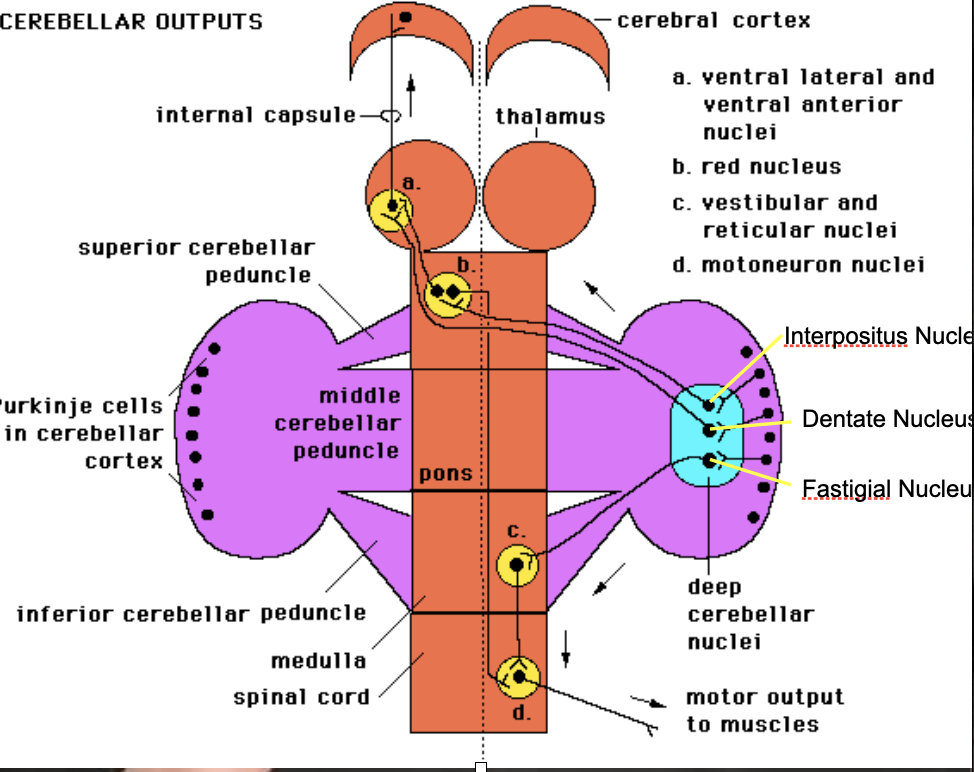
cerebellar peduncles
superior cerebellar peduncle: connects cerebellum to midbrain
middle cerebellar peduncle: connects cerebellum to pons
inferior cerebellar peduncle: connects cerebellum to medulla
ataxia
discoordinated, “clumsy” movements
dysmetria
over- or under- shooting touching a target
disdiadokinesia
inability to perform rapid, alternating movements of hand or mouth
nystagmus
fast involuntary eye movements (side-side, up-down)
ataxic dysarthria
“scanning speech” (syllable by syllable)
hypotonia
reduced muscle tone and reflexes
intention tremor
tremor that is worse with movement and attenuates with rest
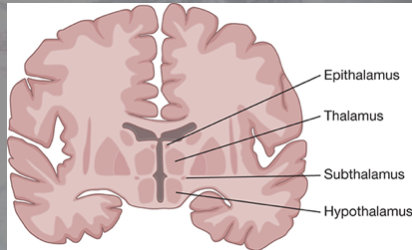
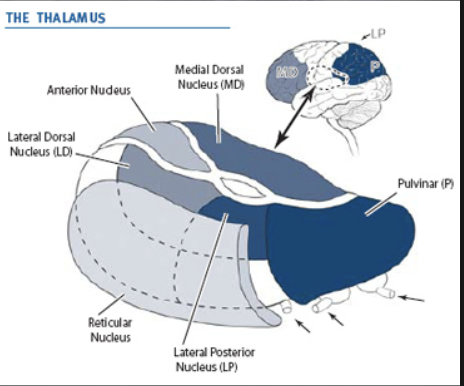
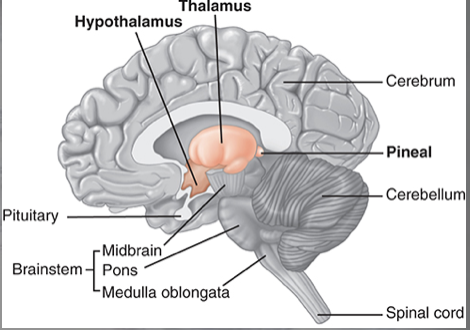
diencephalon substructures
thalamus: sensorimotor relay station
epithalamus: autonomic motor functions
sub thalamus: motor functions
hypothalamus: autonomin functions
thalamus
two lobes connected by mass intermedia
GREAT relay station between cortical and subcortical structures
3 functions of the thalamus
channeling projections of sensation information (pain, taste, temperature, audition, and vision) to specific cortical areas
integration of sensorimotor information before the projection to the primary and premotor cortices
regulation of assertional cortex as well as cortically mediated cognitive functions
nuclei groups
specific relay: from cortex
sensory relay: somatosensory, hearing, vision
motor really: basal ganglia and cerebellum
association (multimodal): receive indirectly via other thalamic nuclei
nonspecific: arousal and consciousness
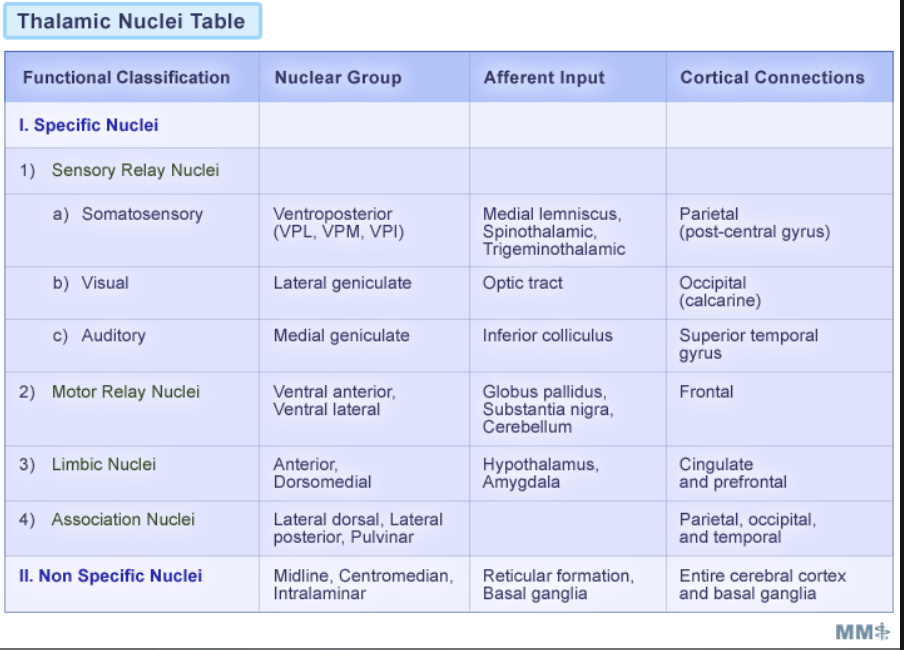
thalamus afferents
basal ganglia
cerebellum
sensory body
sensory head and face
sensory optic
sensory hearing
thalamus efferents
motor cortex
prim motor cortex
prim sensory cortex
prim sensory cortex
occipital lobe
auditory cortex
dorsomedial nucleus
functions: reverberating circuits:
development emotion, judgment, reason, memory, language, cognitive function, sensory and motor learning
afferents:
prefrontal cortex, hippocampus, centromedianus nucleus, and orbital cortex
efferents:
prefrontal and orbitofrontal cortices and limbic structures
lesions:
memory loss (Wernicke-Korsakoff syndrome) and altered personality
surgical lesions- amelioration of anxiety-related disorders
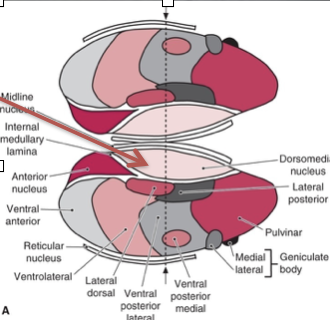
reticular nucleus
origin: part of the ventral thalamus that forms a capsule around the thalamus laterally
function: integration and regulation of thalamic neuronal activity
thalamic problems
thalamic pain syndrome
hemiparesis/hemiplegia
dysesthesia (pain)
slight ataxia
cognition, speech, and language intact
thalamic aphasia
fluent verbal output with semantic paraphasia
mild auditory comprehension issues
mild to normal repeating skills
hypothalamus
origin: in the pituitary gland
function:
autonomic nervous system control
metabolism
water balance
sleep-wake mechanism
body temperature
food intake regulation
secondary sex characteristics
pituitary gland problems
Cushing disease:
endocrine hormone disorder caused by tumor on pituitary gland
causes high cortisol levels
symptoms:
moon facies
emotional disturbances
hypertension
osteoporosis
buffalo hump
obesity
amenorrhea
muscle weakness
abdominal stripes
Acromegaly:
“extreme largeness” caused by pituitary tumor
causes the pituitary gland to produce too much human growth hormone
symptoms:
large stature
large nose and jaw
large hands
hypertension
peripheral neuropathy
epithalamus
connects limbic system to forebrain and other parts
structures:
pineal gland: produces melatonin
habenula
stria medullar is
functions: sleep-wake cycle, olfactory reflexes
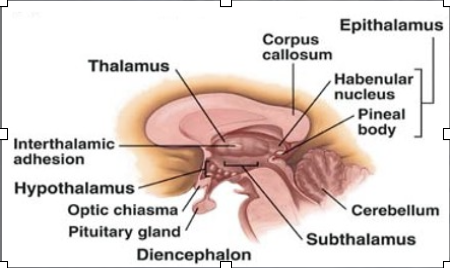
sub thalamus
origin: under thalamus
function: connects basal ganglia to motor cortex; more related to basal ganglia than thalamus
damage to sub thalamus can cause hemiballismus
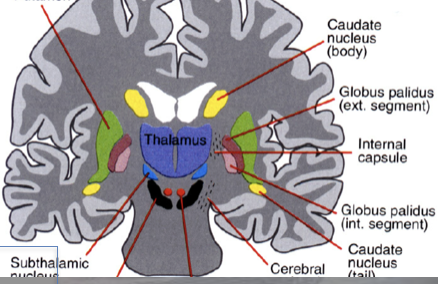
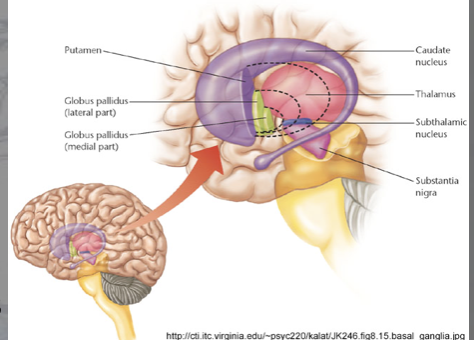
basal ganglia
structures:
globus pallidus
external
internal
putamen
caudate nucleus
sub thalamic nucleus
substantia nigra
function: regulates complex motor functions
symptoms:
hypokinetic: limited movement
rigidity
dystonia
bradykinesia
hypokinesia
resting tremor
hyperkinetic- excessive movement
tremors
athetosis
chorea
ballismus
tics
Parkinson Disease (PD) (“shaking palsy”)
a progressive idiopathic neurological disease first described by Dr. James Parkinson in 1817
caused by degeneration of midbrain’s substantia nigra and loss of dopamine to BG
Parkinson Disease (PD) facts (maybe extra credit)
effects 20 million worldwide
effects 1 million people in the US
every year 600,000 people are diagnosed
greater in males (1.2-1.5x)
41/100,000 get it in their 40s
1,900/100,000 get it 80s+
may triple in 5 years
costs the US $25 billion per year
meds cost $2500 per year
surgery costs $100,000
Parkinson Disease (PD) risk factors
aging
genetics
environmental
Parkinson Disease (PD) symptoms
rest tremor
rights
bradykinesia
hypokinesia
postural instability
masked face
shuffling gait
hyperkinetic dysarthria
reduced voice volume
dysphagia
depression/anxiety (40-50%)
dementia (15-32%)
Parkinson Disease (PD) Treatment (medicine)
levodopa/carbidopa meds
Sinemet
Parcopa
Stalevo
dopamine agonists
mirapex
equip
parlodel
anticholinergics
Artane
cognetine
MAO_B inhibitors
eldepryl
zelapar
COMT inhibitors
comtan
tasmar
Parkinson Disease treatment (surgical)
deep brain stimulation (DBS): surgical insertion of a brain pacemaker ate stimulates the subthalamic nucleus, reducing PD limb rotor symptoms, detrimental effects speech
pallidotomy: cells in the globes pallid us are selectively destroyed using a heated probe reducing the PD symptoms
hyperkinetic disorders
Involuntary Movements: abnormal often bizarre, rhythmic or irregular and unpredictable, rapid or slow
likely caused by too much dopamine
types of hyperkinetic disorders
DYSKINESIA
abnormal, uncontrollable, involuntary movements. There are many different types of dyskinesia each with different causes
typically, it is associated with brain injury, antipsychotic medications (Tardive Dyskinesia), or the long-term use of levodopa (PD dyskinesia)
TICS, TOURETTE’S
Rapid, stereotyped coordinated or patterned movements under partial voluntary control associated with irresistible urge to perform them
Tourette’s most common form
CHOREA
Rapid, involuntary, purposeless movements of a body part. Present at rest, during sustained postures and voluntary movement
Inflammatory or infectious (Sydenham’s chorea, encephalitis) Degenerative (Huntington’s)
Athetosis
Slow writhing purposeless movements that tend to flow into one another
Considered a major category of Cerebral Palsy
Dystonia
Slow involuntary abnormal postures resulting from excessive co-contraction of antagonistic muscles
Can affect one body part, or generalized
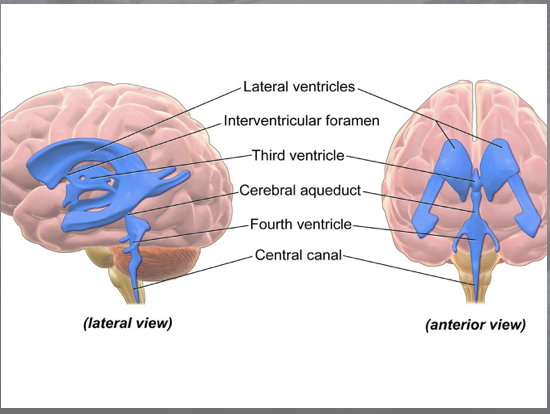
ventricles
function:
cerebral spinal fluid circulation and storage
central nervous system protection during excessive accelerating and decelerating head movements
anatomy:
2 lateral ventricles, 1 third ventricle, 1 fourth ventricle
each ventricle contains choroid plexus that produces cerebral spinal fluid
cereal spinal fluid (CSF)
produced by choroid plexus
origin:
brain ventricles
arachnoid space: brain and spinal cord
functions:
protections
buoyancy
removes waste
transports nutrients and hormones
production
500mL is generated every day, 25 mL an hour
125-150 mL is present at any one time
reabsorption
CSF return to the vascular system by entering the dural venous sinuses via arachnoid granulations
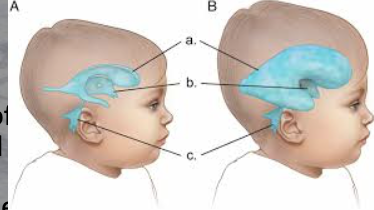
hydrocephalus
“water on the brain”
accumulation of CSF caused by an imbalance in production and drainage of fluid
symptom: large head
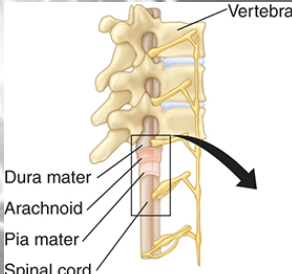
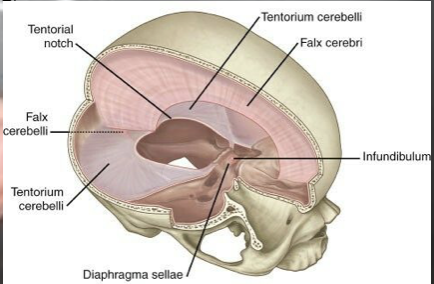
meninges
a three layered membrane that surround the brain and spinal cord and act as a barrier
dura matter: most outer layer
arachnoid: middle layer
pia mater: inner layer
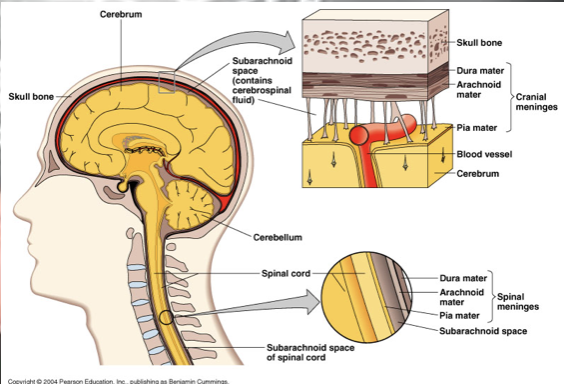
dura mater
most outer layer
strong thick and dense membrane
surrounds the Venus channels carrying blood from brain to heart
3 septa:
falx cerebri: lies between the two hemispheres of the brain
tentorium cerebelli: gives a strong membranous roof over the cerebellum
falx cerebelli: projects downward from the tentorium cerebelli between the two cerebellar hemispheres
arachnoid
“middle layer”
thin transparent membrane
large number of filaments (arachnoid trabecular) pass from arachnoid through the subarachnoid space to blend with tissue of Pia mater
arachnoid subspace contains blood vessels CSF
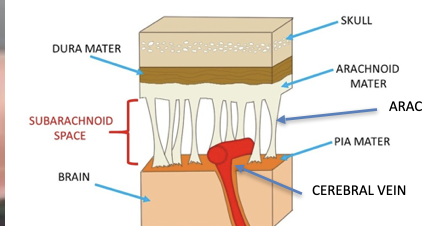
pia matter
“inner most layer”
thin me brane that adheres to surface of brain and spinal cord (covering gyri and descending into suli)
pierced by blood vessels that travel to the brain and spinal cord
meningitis
acute inflammation of the meninges
causes:
bacterial causes: pneumonia, streptococcus, etc.
viral causes: echovirus, poliovirus, and coxsackie
treatment
bacterial: antibiotics/antinflammatory products and vitamins; vaccine
viral: no specific treatment but antivirals are helpful
complications
bacterial: hearing loss, brain damage, learning disability; untreated can be fatal; spreads through fluid contact from nose or mouth
viral: rare to have complications but can occur in patients with diseases or weak immune systems; spreads through saliva or stool
blood brain barrier (BBB)
coordinated by physical, transport, and metabolic properties possessed by the endothelial cells that form the walls of the blood vessels
Protects CNS from toxins, pathogens, inflammation, injury, and disease.
Tightly regulates CNS homeostasis
Provides an obstacle for drug delivery to the CNS
Loss of some, or most, of these barrier properties during neurological diseases including stroke, multiple sclerosis (MS), brain traumas, and neurodegenerative disorders, is a major component of the pathology and progression of these diseases
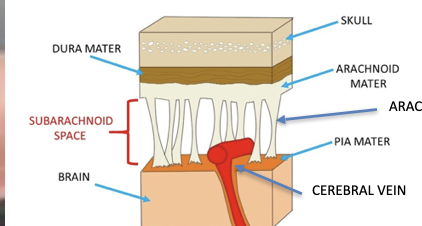
The Circle of Willis
feeds the brain oxygen through:
anterior cerebral artery
middle cerebral artery
posterior cerebral artery
cerebral vascular accident (CVA)
3 types:
ischemic: occlusion of blood vessels
thrombosis: narrowing of arterial lumen due to focal and gradual accumulation of lipids, platelets, calcium deposits, & fatty particles
embolism: A broken plaque away from a thrombus; Blocking of distal and smaller arteries; Occurring during period of activity
transient ischemic attack (TIA): Temporary blood interruptions resolving in minutes to hours’ Occurring during inactivity; Indicative of larger stroke in progress; Sites of arterial bifurcation or at sites with injury
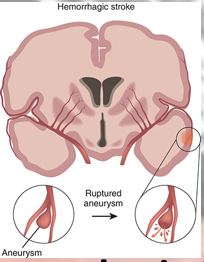
hemorrhage
ruptured blood vessel caused by high blood pressure
Arteriovenous Malformations (AVM)
congenital or fetal circulatory vascular malformation involving tangled dilated arteries or veins; blood bypasses brain tissue

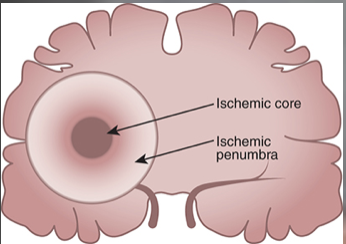
ischemic CVA
ischemic penumbra idle cells die within 20 minutes without collateral circulation
survival is 6-8 hours
hemorrhagic CVA
intraaxial: hemorrhage inside the brain
extraaxial: hemorrhage outside the brain
CVA symptoms
Anterior Cerebral Artery:
Paralysis of legs & feet
Prefrontal lobe symptoms
reduced thinking, reasoning, & impaired planning
Middle Cerebral Artery:
Contralateral hemiplegia
Impaired sensory functions
Aphasia (dominant hemisphere)
Temporal-visual-spatial deficit (non-dominant)
Homonymous hemianopia,
Involuntary movements (lenticulostriate arteries)
Posterior Cerebral Artery:
Homonymous hemianopia
Pontine & cerebellar symptoms
Cortical blindness and visual agnosia (bilateral occipital lesions)
modifiable and non-modifiable risk factors of a stroke
modifiable: high blood pressure, heart diseases, diabetes, medications, smoking, drinking
non-modifiable: age, gender, family
stroke facts (maybe extra credit)
-4th cause of death in U.S. 1st cause of disability worldwide
-Prevalence in U.S.
roughly 3% of the adult population, ~7 million individuals
someone dies of a stroke every 4 minutes in the U.S.
-Incidence in U.S.:
Approximately 800,000 primary (first-time) or secondary (recurrent) strokes occur each year, majority being primary strokes (roughly 600,000)
Rapidly increases with age, doubling for each decade after age 55
In adults ages 35 to 44, incidence is 30 - 120 / 100,000 per year
In adults ages 65 to 74, incidence is 670 - 970 / 100,000 per year
-Geography:
Higher rates in the Southeastern U.S. (the so-called “Stroke Belt”), especially along the coasts in Georgia and the Carolinas (so-called “Stroke Buckle”).
-Race/Ethnicity
2- to 4-fold higher among African Americans and occur at an earlier age
2-fold higher among Hispanics and occur at an earlier age
-Cost
The estimated direct and indirect cost of stroke for 2007 is $62.7 billion
6.4 million stroke survivors living in the U.S.
stroke treatment
ischemic blood clot: clot busting drug given through vein to break up blood flow and maintain blood flow
must be given within 3-6 hours of stroke to be helpful
must have CT R/O hemorrhage or stroke could worsen
types of blood thinners: heparin, warfarin, aspirin, clopidogrel
hemorrhage: surgery to remove blood around the brain and to fix damage blood vessels
waste removal: moves deoxygenated blood away from the brain
removed through 4 sinuses in meninges
superior sagittal transverse
occipital sigmoid
superficial and deep cerebral veins then remove waste
major layers of the cerebrum
surface gray matter: cerebral cortex, neuron somas
white matter: axons
deep gray matter: thalamus, basal ganglia
ventricles: 4 ventricles
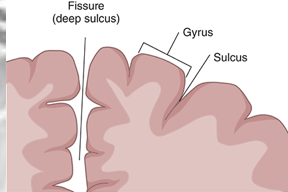
features of cerebral cortex
gyri
sulci
fissures (deep sulci)
longitudinal
central sulcus (Rolandic fissure)
lateral sulcus (Sylvian fissure)
cortical cellular organization
Three major types of cells in cortex:
Pyramidal (with descending projections)
Granular/Satellite (with projections to association cortex)
Interneurons (local circuits to facilitate or inhibit information)
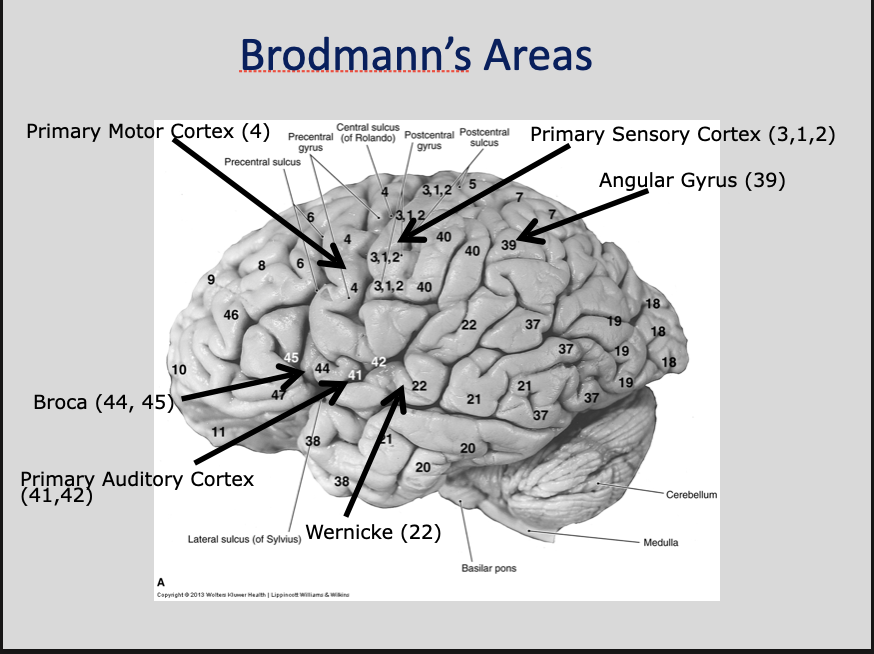
Brodmann’s Areas
frontal lobe
primary motor cortex
4
premotor cortex
6, 8
cognitive association cortex
9-11
frontal association language cortex; Broca area
44, 45
parietal lobe
primary sensory cortex
1, 2, 3
somatosensory association cortex
5, 7
reading and writing
41, 42
temporal lobe
posterior association language cortex: Wernickes area
22
primary auditory cortex
41, 42
occipital lobe
primary visual cortex
17
visual association cortex
18, 19
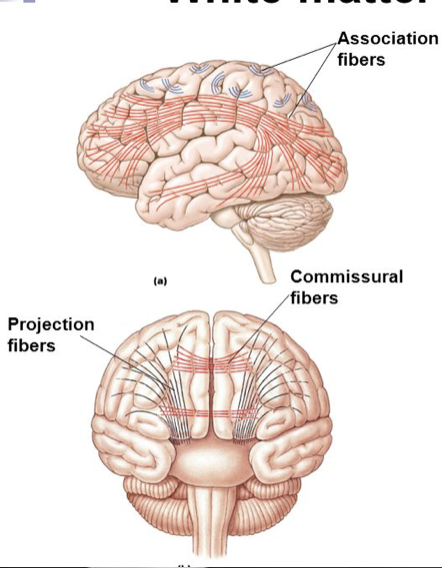
types of connection of Cortical White Matter
association fibers: connect gyro in same hemisphere
commissural fibers connect gyro in opposite hemispheres
projection fibers: connect cerebrum with other parts of brain and spinal cord
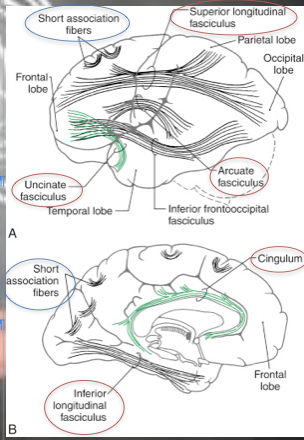
association fibers
Long Association Fibers:
Superior Longitudinal Fasciculus: Connects frontal, occipital, parietal, & temporal lobes
Inferior Longitudinal Fasciculus: Connects occipital lobe to temporal pole
Arcuate Fasciculus: Connects gyri in frontal lobe (Broca’s area) to temporal lobe (Wernicke’s area)
Uncinate Fasciculus: Connects frontal lobe to temporal lobe
Cingulum: Connects frontal & parietal lobes to para-hippocampal gyrus & adjacent temporal gyri
Short Association Fibers: Connect adjacent gyri
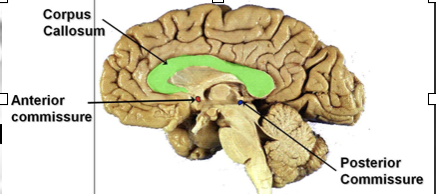
commissural fibers
Corpus Callosum
Large bundle of axons that connect the two hemispheres, except the Temporal lobe which are connected by the anterior commissure