83-93 Abdomen
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Abdomen. Antero-Lateral Abdominal Wall. Regions. Layered Topography – Fasciae, Muscles.
🗺 Abdominal Regions (based on surface anatomy)
Divided by two vertical and two horizontal planes:
Vertical: Midclavicular lines (right and left)
Horizontal: Subcostal plane (L2) and transtubercular plane (L5)
Nine regions:
Right hypochondriac
Epigastric
Left hypochondriac
Right lumbar (flank)
Umbilical
Left lumbar (flank)
Right iliac (inguinal)
Hypogastric (pubic)
Left iliac (inguinal)
🧱 Layered Topography of the Antero-Lateral Abdominal Wall
1. Skin
2. Superficial Fascia (subcutaneous tissue)
Above umbilicus: single layer
Below umbilicus: two layers
Camper’s fascia: superficial, fatty layer
Scarpa’s fascia: deep, membranous layer (important surgically)
3. Muscular Layer
Three flat muscles (lateral abdominal wall):
External oblique - Fibers run inferomedially ("hands in pockets")
Internal oblique - Fibers run superomedially (perpendicular to external oblique)
Transversus abdominis - Fibers run horizontally
One vertical muscle (anterior abdominal wall):
Rectus abdominis
Lies in the rectus sheath, has tendinous intersections
Bordered by linea alba (midline) and linea semilunaris (lateral margin)
Pyramidalis muscle (small, triangular; present in some individuals anterior to rectus abdominis)
4. Rectus Sheath
Formed by the aponeuroses of the three flat muscles
Encloses the rectus abdominis and pyramidalis
Sheath composition differs above and below the arcuate line
5. Transversalis Fascia
Thin, deep fascia lining the internal surface of the abdominal wall
6. Extraperitoneal Fat
Variable in thickness; separates fascia from parietal peritoneum
7. Parietal Peritoneum
Serous membrane lining the abdominal cavity
⚙ Function
Protects abdominal viscera
Assists in forced expiration, coughing, urination, defecation, childbirth
Helps maintain posture and increase intra-abdominal pressure
⚠ Clinical Relevance
Hernias (inguinal, umbilical) occur through weak points in the abdominal wall
Surgical incisions must respect muscle/fascial layers and neurovascular planes
Knowledge of fascia (Scarpa’s) important in drainage and suturing
Inguinal Canal.
Inguinal Canal
📍 Location & Structure
Oblique passage (~4 cm long) in the lower anterior abdominal wall
Runs above the medial half of the inguinal ligament, from deep inguinal ring (lateral) to superficial inguinal ring (medial)
🧠 Walls of the Inguinal Canal
Anterior wall: aponeurosis of external oblique, reinforced laterally by internal oblique
Posterior wall: transversalis fascia, reinforced medially by conjoint tendon
Roof: arching fibers of internal oblique and transversus abdominis
Floor: inguinal ligament and lacunar ligament
📦 Contents
In males: Spermatic cord (ductus deferens, testicular artery, pampiniform plexus, etc.)
In females: Round ligament of the uterus
In both: Ilioinguinal nerve
⚠ Clinical Relevance
Common site for inguinal hernias (direct and indirect)
Deep inguinal ring = potential weak point in abdominal wall
Rectus Abdominis Sheath
📍 Definition
Fibrous sheath enclosing the rectus abdominis and pyramidalis muscles
Formed by aponeuroses of external oblique, internal oblique, and transversus abdominis
🧱 Structure
Above arcuate line (≈1/3 of the way from umbilicus to pubic symphysis):
Anterior layer: external oblique + ½ internal oblique aponeurosis
Posterior layer: ½ internal oblique + transversus abdominis aponeurosis
Below arcuate line:
All three aponeuroses pass anterior to rectus abdominis
Posterior wall absent → only transversalis fascia and peritoneum behind muscle
⚠ Clinical Relevance
Important in abdominal incisions (e.g., C-section, hernia repair)
Weak area below arcuate line more prone to herniation
Linea Alba.
📍 Definition
Midline fibrous raphe formed by the interlacing aponeuroses of the abdominal wall muscles
Extends from xiphoid process to pubic symphysis
🧱 Structure
Lies between the two rectus abdominis muscles
Relatively avascular (useful for midline surgical incisions)
⚙ Function
Provides attachment and reinforcement for abdominal wall muscles
Maintains structural integrity of anterior abdominal wall
⚠ Clinical Relevance
Diastasis recti: separation of rectus muscles along linea alba (common post-pregnancy)
Midline incisions preferred here to reduce bleeding and nerve damage
Abdominal Cavity. Walls, Regions.
🧱 Walls of the Abdominal Cavity
Anterior wall: Formed by abdominal muscles — rectus abdominis, external and internal obliques, transversus abdominis
Posterior wall: Lumbar vertebrae, psoas major, iliacus, quadratus lumborum, and transversus abdominis
Lateral walls: Continuation of anterior and posterior muscles
Superior boundary: Inferior surface of the diaphragm
Inferior boundary: Continuous with the pelvic cavity (no physical separation)
🗺 Regions of the Abdomen
Divided into 9 regions using:
2 vertical planes: midclavicular lines
2 horizontal planes: subcostal (L2) and transtubercular (L5)
Regions:
Right hypochondriac
Epigastric
Left hypochondriac
Right lumbar
Umbilical
Left lumbar
Right iliac (inguinal)
Hypogastric (pubic)
Left iliac (inguinal)
Peritoneum - Structure, Blood and Nerve Supply.
Peritoneum
🧬 Structure
Serous membrane lining the abdominal cavity
Two continuous layers:
Parietal peritoneum – lines internal surface of abdominal wall
Visceral peritoneum – covers abdominal organs
Peritoneal cavity: Thin potential space between the two layers containing peritoneal fluid
💉 Blood Supply
Parietal peritoneum: Supplied by vessels of the abdominal wall (e.g., intercostal, lumbar arteries)
Visceral peritoneum: Supplied by the same blood vessels that supply the organ it covers (e.g., celiac trunk, SMA, IMA)
🧠 Nerve Supply
Parietal peritoneum:
Somatic innervation → sharp, localized pain
Supplied by intercostal nerves, lumbar plexus
Visceral peritoneum:
Autonomic innervation → dull, poorly localized pain
From sympathetic and parasympathetic fibers (depending on organ)
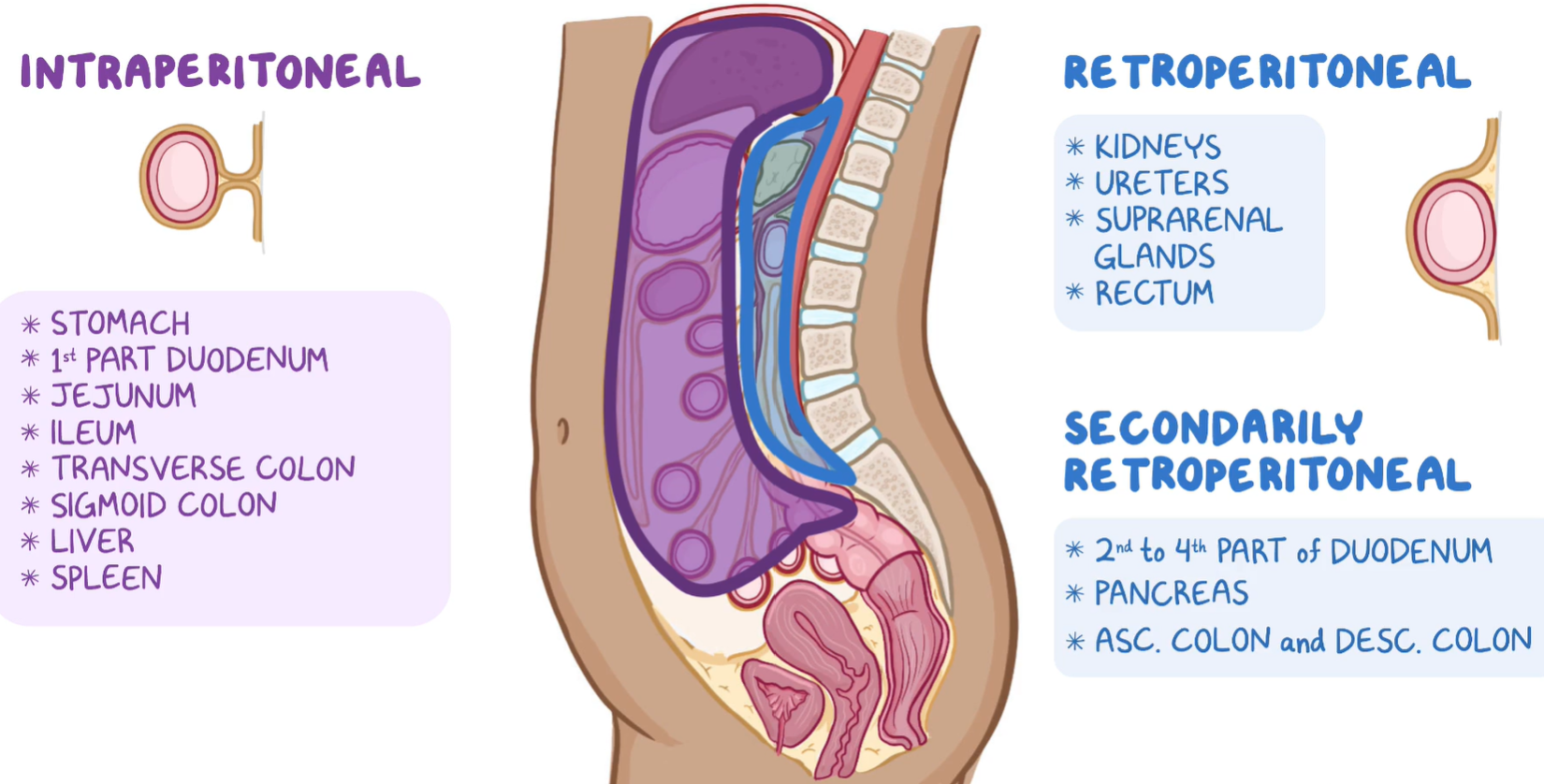
Peritoneal Compartment of the Abdominal Cavity.
Peritoneal Compartments of the Abdominal Cavity
1. Intraperitoneal Space
Organs suspended by mesenteries, completely surrounded by visceral peritoneum
Examples: stomach, liver, jejunum, ileum, transverse colon, sigmoid colon
2. Retroperitoneal Space
Organs lie behind the peritoneum, only anterior surface covered by it
Examples: kidneys, pancreas (except tail), duodenum (parts 2–4), ascending/descending colon, abdominal aorta
3. Subperitoneal (Infraperitoneal) Space
Organs located beneath the peritoneum, mostly in the pelvis
Examples: urinary bladder, rectum, reproductive organs
🧠 Additional Compartments & Recesses
Greater sac: Main peritoneal cavity
Lesser sac (omental bursa): Posterior to stomach and lesser omentum
Omental foramen (of Winslow): Connects greater and lesser sacs
Subphrenic and subhepatic spaces: Important for fluid accumulation
Paracolic gutters: Pathways for fluid spread along colon sides
⚠ Clinical Relevance
Ascites: fluid accumulation in the peritoneal cavity
Peritonitis: inflammation due to infection or perforation
Intraperitoneal injections use the peritoneal cavity for drug absorption
Surgical anatomy (e.g., laparotomy or laparoscopy) relies on peritoneal reflections and compartments
Upper Region of the Peritoneal Cavity. Organs, Peritoneal Structures
📍 Boundaries
Located above the transverse colon and mesocolon
Lies primarily in the epigastric and hypochondriac regions
Includes the supracolic compartment of the peritoneal cavity
🧠 Main Organs in the Upper Peritoneal Cavity
Liver
Gallbladder
Stomach
Spleen
Superior part of the duodenum
Pancreas (only tail is intraperitoneal)
Esophagus (abdominal part)
🧬 Peritoneal Structures - Ligaments and Omenta
Lesser omentum: from liver to lesser curvature of stomach and duodenum
Contains: hepatic artery proper, portal vein, common bile duct
Greater omentum: hangs from greater curvature of stomach over intestines
Falciform ligament: connects liver to anterior abdominal wall
Coronary and triangular ligaments: suspend liver from diaphragm
Gastrosplenic ligament: connects stomach to spleen (contains short gastric vessels)
Splenorenal ligament: spleen to left kidney (contains splenic vessels, tail of pancreas)
🔄 Peritoneal Recesses/Spaces
Lesser sac (omental bursa): posterior to stomach and lesser omentum
Greater sac: main part of peritoneal cavity
Subphrenic spaces: between diaphragm and liver
Subhepatic space (Morrison’s pouch): between liver and right kidney — site of fluid accumulation
Upper Region of the Peritoneal Cavity. Topographic Relations of the Organs, Vessels and Nerves
🔍 Topographic Relations of Organs
🏷 1. Liver
Right hypochondrium, extending to epigastric region
Anterior: diaphragm and anterior abdominal wall
Posterior: inferior vena cava, esophagus, stomach, right kidney, and adrenal gland
Related vessels: portal triad in hepatoduodenal ligament
Innervation: celiac plexus, vagus nerves
🏷 2. Stomach
Left hypochondrium and epigastric region
Anterior: anterior abdominal wall, left lobe of liver, diaphragm
Posterior (stomach bed): pancreas, spleen, left kidney, adrenal gland, transverse mesocolon
Supplied by: left gastric, right gastric, right and left gastroepiploic arteries
Innervation: vagus nerves, celiac plexus
🏷 3. Spleen
Left hypochondrium, intraperitoneal
Anterior: stomach
Posterior: diaphragm, ribs 9–11
Inferior: left colic flexure
Vessels: splenic artery and vein (within splenorenal ligament)
Innervation: celiac plexus
🏷 4. Gallbladder
Lies on inferior surface of liver, in right hypochondrium
Contacts anterior abdominal wall at tip of 9th costal cartilage (Murphy’s point)
Drains into common bile duct
Innervation: celiac plexus, right phrenic nerve (referred pain to shoulder)
🏷 5. Duodenum (superior part)
First 2 cm is intraperitoneal, then retroperitoneal
Located in epigastric region, just right of midline
Close relations to liver, gallbladder, and pancreas
🏷 6. Pancreas (mostly retroperitoneal)
Lies posterior to stomach, across epigastric region
Tail enters splenorenal ligament (intraperitoneal)
Related to splenic artery, superior mesenteric vessels, and portal vein
Innervation: celiac and superior mesenteric plexuses
Omental Bursa.
🟨 Omental Bursa (Lesser Sac)
📍 Definition
A peritoneal recess located posterior to the stomach and lesser omentum
Part of the supracolic compartment of the peritoneal cavity
🧱 Boundaries
Anterior:
Lesser omentum (hepatogastric ligament)
Posterior wall of stomach
Gastrocolic ligament (part of greater omentum)
Posterior:
Pancreas
Left kidney and suprarenal gland
Peritoneum covering posterior abdominal wall
Superior:
Caudate lobe of the liver
Inferior:
Fused layers of greater omentum
Left:
Gastrosplenic and splenorenal ligaments
Right (entry point): Omental (epiploic) foramen of Winslow
Connects lesser sac to greater sac
Bounded by:
Anterior: hepatoduodenal ligament (with portal triad)
Posterior: inferior vena cava
Superior: caudate lobe of liver
Inferior: first part of duodenum
⚙ Function
Allows free movement of stomach and pancreatic expansion
Provides a space for surgical access to posterior stomach and pancreas
Greater Omentum – Formation, Parts.
🟧 Greater Omentum
📍 Definition
A large peritoneal fold hanging like an apron from the greater curvature of the stomach
Drape-like structure covering the anterior surface of the intestines
🏗 Formation
Develops from the dorsal mesogastrium during embryogenesis
Folds over itself to form four layers of peritoneum:
2 layers descend from the stomach
Fold back and ascend to fuse with the transverse colon and its mesocolon
📦 Parts of the Greater Omentum
Gastrocolic ligament:
Largest part
Connects stomach to transverse colon
Covers intestines like an apron
Gastrosplenic ligament:
Connects stomach to spleen
Contains short gastric vessels
Gastrophrenic ligament:
Connects stomach to diaphragm
⚙ Functions
Fat storage
Immune defense – contains lymphoid aggregates (milky spots)
Limits spread of infection (“policeman of the abdomen”)
Mobility allows sealing of inflamed areas (e.g., in appendicitis)
⚠ Clinical Relevance
Site of fluid accumulation in peritonitis
Used in omentum flaps for surgical reconstruction
May adhere to inflamed organs and isolate infections
Portal Vein. Formation, Position. Anastomoses with the Superior and Inferior Venae Cavae.
Portal Vein (Vena Portae Hepatis)
📍 Formation
Formed by the union of the:
Superior mesenteric vein (SMV)
Splenic vein
This union typically occurs behind the neck of the pancreas at the level of L2 vertebra
📍 Position
Ascends posterior to the pancreas and duodenum, then runs within the hepatoduodenal ligament (part of lesser omentum)
Lies posterior to the common bile duct and proper hepatic artery (in the portal triad)
Enters the liver at the porta hepatis, dividing into right and left branches to supply respective lobes
Not a true vein: does not drain into the heart directly; instead, it brings nutrient-rich blood from the gastrointestinal tract to the liver for processing
🧠 Function
Carries 75% of liver's blood supply
Transports nutrients, toxins, and metabolites from:
GI tract (stomach, intestines)
Pancreas
Spleen
Gallbladder
🔄 Porto-Caval Anastomoses
(Anastomoses between the portal and systemic (caval) venous systems)
🩸 Sites of Anastomoses
Esophageal veins
Portal: left gastric vein
Caval: esophageal veins → azygos → SVC
Clinical relevance: esophageal varices in portal hypertension
Rectal veins
Portal: superior rectal vein
Caval: middle and inferior rectal veins → internal iliac → IVC
Clinical relevance: internal hemorrhoids
Paraumbilical veins
Portal: paraumbilical veins (from left branch of portal vein)
Caval: superficial epigastric veins → femoral vein → IVC
Clinical relevance: caput medusae (dilated periumbilical veins)
Retroperitoneal veins
Portal: veins of colon, duodenum, pancreas
Caval: lumbar and renal veins → IVC
Clinical relevance: hidden site of bleeding in portal hypertension
⚠ Clinical Relevance
Portal hypertension (e.g., in liver cirrhosis) → blood diverted through anastomoses → varices and bleeding
Transjugular intrahepatic portosystemic shunt (TIPS): procedure to reduce portal pressure by connecting portal vein to hepatic vein
Lower Region of the Peritoneal Cavity. Organs. Peritoneal Structures,
Lower Region of the Peritoneal Cavity (Also called the infracolic compartment)
📍 Boundaries
Located below the transverse colon and transverse mesocolon
Divided by the mesentery of the small intestine into:
Right infracolic space
Left infracolic space
🧠 Organs in the Lower Peritoneal Cavity
Jejunum and ileum (intraperitoneal)
Ascending colon and descending colon (secondarily retroperitoneal)
Sigmoid colon (intraperitoneal)
Cecum and appendix (intraperitoneal)
Upper part of rectum (partially peritonealized)
🧬 Peritoneal Structures
Mesentery of the small intestine
Suspends jejunum and ileum
Contains superior mesenteric vessels, lymph nodes, fat, and nerves
Transverse mesocolon
Suspends the transverse colon
Separates supracolic and infracolic compartments
Sigmoid mesocolon
Suspends sigmoid colon
Contains inferior mesenteric vessels
Paracolic gutters (right and left)
Allow communication between upper and lower peritoneal cavity
Important in spread of infection or fluid (e.g. in peritonitis)
⚠ Clinical Relevance
Peritoneal recesses and gutters direct spread of fluid, infection, or metastasis
Knowledge of mesenteric root and paracolic gutters is critical in surgery and imaging
Important in procedures like peritoneal dialysis and laparoscopy
Lower Region of the Peritoneal Cavity. Topographic Relations of the Organs, Vessels and Nerves.
🔍 Topographic Relations
🏷 Small Intestine (Jejunum and Ileum)
Occupy umbilical, lumbar, and hypogastric regions
Jejunum: mostly upper left abdomen
Ileum: mostly lower right abdomen and pelvis
Suspended by mesentery from posterior abdominal wall, root runs obliquely from L2 to right sacroiliac joint
🏷 Cecum and Appendix
Cecum: right iliac fossa, intraperitoneal
Appendix: variable position (most commonly retrocecal)
Supplied by ileocolic artery (branch of SMA)
Innervation: sympathetic (T10-T12) and vagal parasympathetic
Pain from appendicitis often starts periumbilically (T10), then localizes to McBurney's point
🏷 Ascending and Descending Colon
Retroperitoneal
Ascending: right lumbar region
Descending: left lumbar region
Blood supply:
Ascending colon: right colic artery (SMA)
Descending colon: left colic artery (IMA)
🏷 Sigmoid Colon
Intraperitoneal, located in left iliac and hypogastric regions
Suspended by sigmoid mesocolon
Blood supply: sigmoid arteries from inferior mesenteric artery
🏷 Rectum (Upper Part)
Lies partly within peritoneum (upper third only)
Peritoneum covers anterior and lateral surfaces in upper part
Supplied by:
Superior rectal artery (from IMA)
Venous drainage includes portal-systemic anastomosis
🔌 Vessels and Nerves
🩸 Arterial Supply
Superior mesenteric artery (SMA): small intestine, cecum, ascending and proximal 2/3 of transverse colon
Inferior mesenteric artery (IMA): distal 1/3 of transverse colon, descending colon, sigmoid colon, rectum
🔄 Venous Drainage
Follows arteries → drains into portal vein via:
Superior mesenteric vein
Inferior mesenteric vein (may join splenic vein)
🧠 Innervation
Sympathetic: from thoracic and lumbar splanchnic nerves via superior and inferior mesenteric plexuses
Parasympathetic:
Vagus nerve: up to mid-transverse colon
Pelvic splanchnic nerves (S2–S4): for distal colon and rectum
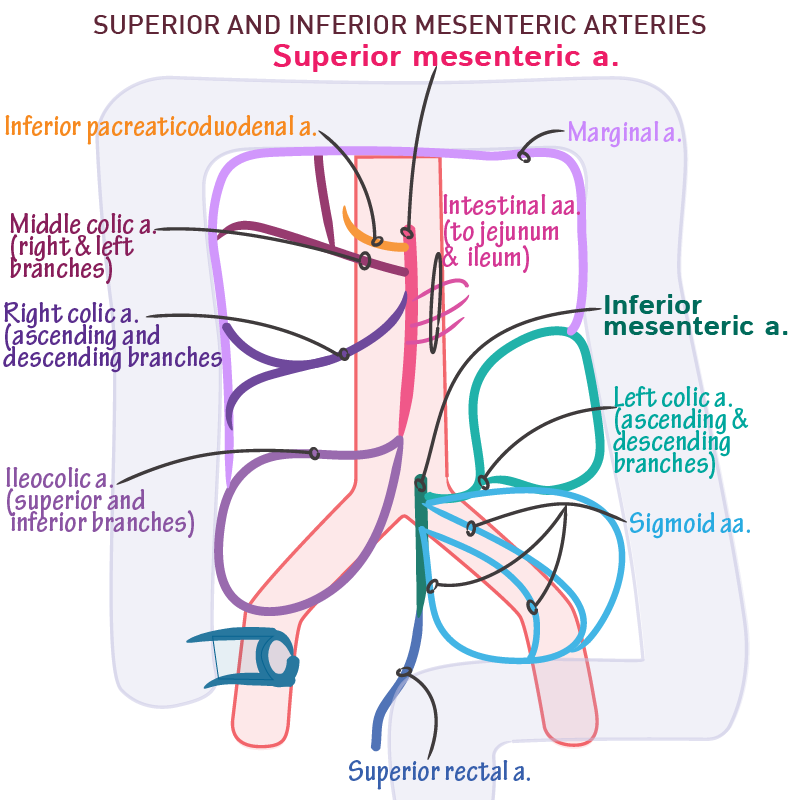
The Unpaired Visceral Branches of the Abdominal Aorta - the Coeliac Trunk, the Superior and Inferior Mesenteric Arteries. Position and Branches.
🔴 Unpaired Visceral Branches of the Abdominal Aorta
These arteries supply the abdominal gastrointestinal tract and associated organs, and arise anteriorly from the aorta.
Celiac Trunk (Coeliac Artery)
📍 Position
Arises at the level of T12, just below the aortic hiatus of the diaphragm
Very short (~1–2 cm), trifurcates immediately
🌿 Branches
Left gastric artery
Smallest branch
Ascends to esophagus → follows lesser curvature of the stomach
Splenic artery
Tortuous; runs along superior border of the pancreas to spleen
Gives off:
Short gastric arteries (to fundus of stomach)
Left gastroepiploic artery (to greater curvature)
Common hepatic artery
Courses to the right toward liver
Divides into:
Proper hepatic artery → right and left hepatic arteries
Gastroduodenal artery → right gastroepiploic artery + superior pancreaticoduodenal artery
Right gastric artery
🧠 Supplies
Liver, stomach, spleen, pancreas, esophagus, duodenum (proximal to major papilla)
Superior Mesenteric Artery (SMA)
📍 Position
Arises at L1, ~1 cm below celiac trunk
Passes behind pancreas and over the third part of the duodenum
Enters mesentery of the small intestine
🌿 Branches
Inferior pancreaticoduodenal artery Anastomoses with superior pancreaticoduodenal (from celiac trunk)
Jejunal and ileal branches - 12–15 branches to small intestine; form arterial arcades and vasa recta
Ileocolic artery Supplies ileum, cecum, appendix
Right colic artery Supplies ascending colon
Middle colic artery Supplies transverse colon
🧠 Supplies
Lower duodenum, jejunum, ileum, cecum, appendix, ascending colon, proximal 2/3 of transverse colon
Inferior Mesenteric Artery (IMA)
📍 Position
Arises at L3, just above aortic bifurcation
Descends to the left toward pelvic brim
🌿 Branches
Left colic artery Supplies descending colon
Sigmoid arteries - 2–4 branches to sigmoid colon
Superior rectal artery - Continuation of IMA; supplies upper part of rectum
🧠 Supplies
Distal 1/3 of transverse colon, descending colon, sigmoid colon, and upper rectum
🩸 Clinical Note: Marginal Artery (of Drummond)
Formed by anastomoses between branches of SMA and IMA (e.g., middle and left colic arteries)
Provides collateral blood flow to colon
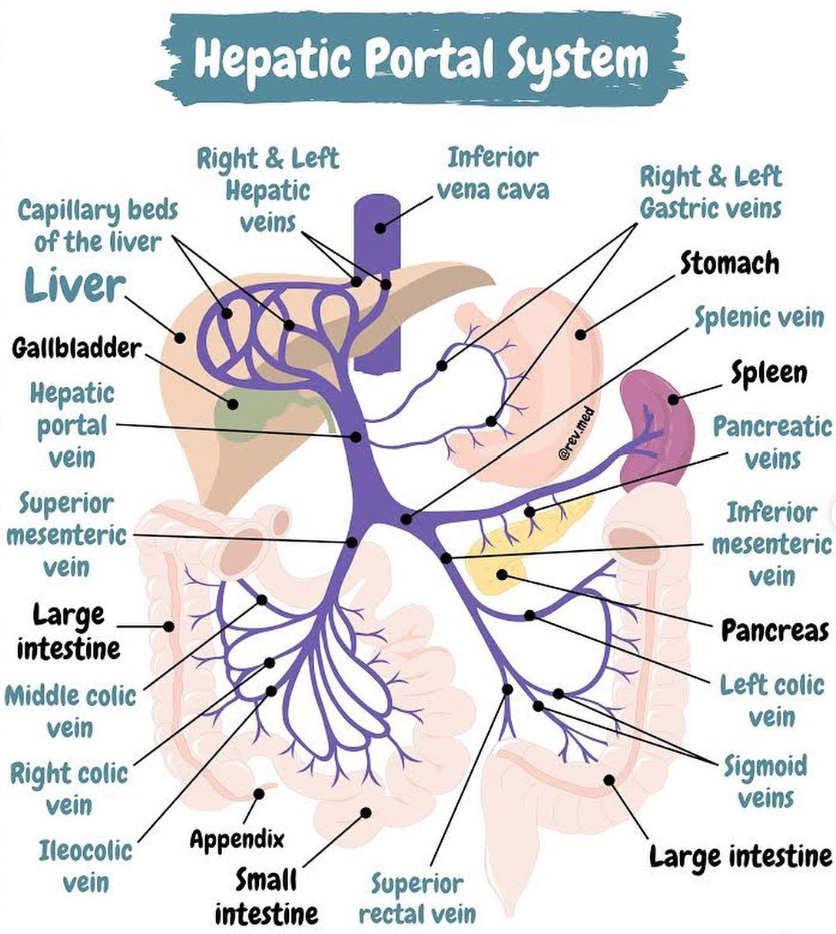
The Hepatic Portal System - Constituting Veins. Position of the Portal Vein. Anastomoses Between the Portal and Systematic Circulation
🟣 Hepatic Portal System
📍 Function
Collects nutrient-rich, oxygen-poor blood from the digestive tract and associated organs
Delivers it to the liver for metabolism, detoxification, and storage
Does not drain directly into the heart — returns blood to the heart via hepatic veins → IVC
🧱 Constituting Veins of the Portal System
The portal vein is formed by the union of:
Superior mesenteric vein (SMV)
Splenic vein
The splenic vein often also receives:
Inferior mesenteric vein (IMV) - May join splenic vein or drain directly into SMV
Additional tributaries of the portal vein:
Left and right gastric veins (stomach)
Cystic vein (gallbladder)
Paraumbilical veins (from anterior abdominal wall)
🔵 Portal Vein – Position
Begins posterior to the neck of the pancreas (L2 level), where SMV and splenic vein join
Ascends posterior to the first part of the duodenum
Enters the hepatoduodenal ligament (with common bile duct and hepatic artery proper)
At the porta hepatis, it divides into right and left portal branches to supply liver lobes
🔄 Porto-Systemic (Porto-Caval) Anastomoses
Sites where portal circulation communicates with systemic venous circulation
→ Important in portal hypertension (e.g., cirrhosis), where blood is redirected through these alternate routes
1. Esophageal Anastomosis
Portal: left gastric vein
Systemic: esophageal veins → azygos → SVC
⚠ Esophageal varices — can rupture and cause fatal bleeding
2. Rectal Anastomosis
Portal: superior rectal vein
Systemic: middle and inferior rectal veins → internal iliac → IVC
⚠ Internal hemorrhoids
3. Paraumbilical Anastomosis
Portal: paraumbilical veins (from left portal vein)
Systemic: superficial epigastric veins → femoral vein → IVC
⚠ Caput medusae — dilated periumbilical veins
4. Retroperitoneal Anastomosis
Portal: veins of colon, duodenum, pancreas
Systemic: lumbar and renal veins
⚠ Usually clinically silent, but can contribute to hidden hemorrhage
⚠ Clinical Relevance
Portal hypertension → blood backs up into systemic channels → varices, ascites, splenomegaly
TIPS procedure: shunt created between portal and hepatic veins to reduce portal pressure
Hepatic encephalopathy may result from toxins bypassing liver via anastomoses
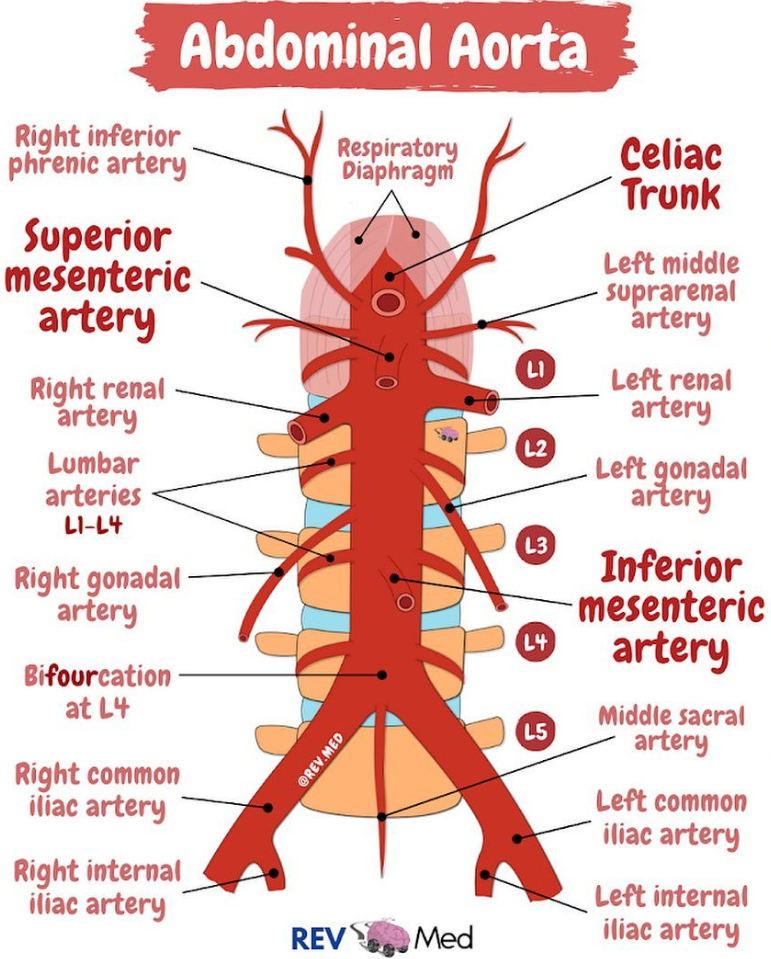
The Abdominal Aorta. Parietal (Lateral) and Paired Visceral Branches.
🔴 Abdominal Aorta
Continuation of the thoracic aorta beginning at the aortic hiatus of the diaphragm (T12)
Descends anterior to the vertebral column
Ends at the level of L4, where it bifurcates into the right and left common iliac arteries
🧱 Paired Visceral Branches
(Supply internal organs)
1. Middle Suprarenal Arteries
Arise at level L1
Supply adrenal (suprarenal) glands
2. Renal Arteries
Arise at level L1–L2 (just below SMA)
Pass laterally to each kidney
Right renal artery is longer and passes behind the inferior vena cava (IVC)
3. Gonadal Arteries
Testicular arteries (males) / Ovarian arteries (females)
Arise at level L2, below renal arteries
Descend along psoas major muscle into pelvis
Testicular arteries enter inguinal canal, ovarian arteries go to ovary and uterine tube
🧱 Parietal (Lateral & Posterior) Branches
(Supply body wall, muscles, vertebrae)
1. Inferior Phrenic Arteries
First paired branches, arise just below diaphragm at T12
Supply the diaphragm and give superior suprarenal branches to adrenal glands
2. Lumbar Arteries (usually 4 pairs)
Arise from posterolateral surface of aorta at L1–L4
Supply posterior abdominal wall muscles, skin, vertebrae, and spinal cord
3. Median Sacral Artery (unpaired but related)
Small artery arising near aortic bifurcation (L4)
Descends in midline over sacrum
Supplies sacrum, coccyx, and lower vertebral column
⚠ Clinical Note
Abdominal aortic aneurysm (AAA) often occurs below renal arteries
Renal artery stenosis may lead to secondary hypertension
Paired arteries must be carefully identified in abdominal surgery (e.g. nephrectomy)
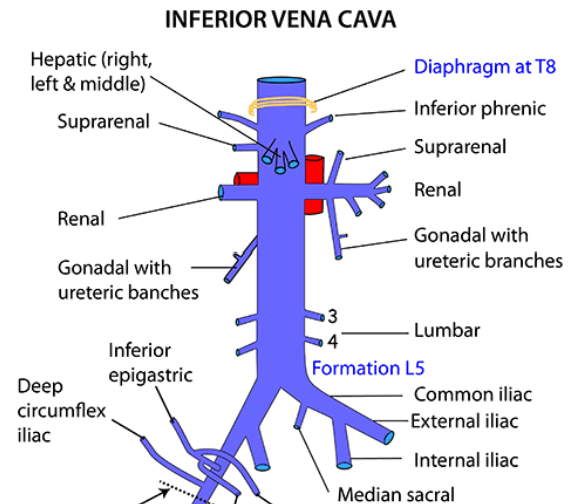
The Superior and Inferior Vena Cava. Position. Main Tributaries. Anastomoses Between the Two Caval Veins.
🟦 Superior Vena Cava (SVC)
📍 Position
Formed by the union of the right and left brachiocephalic veins (at the level of the first costal cartilage, behind the right sternoclavicular joint)
Descends vertically in the superior mediastinum, right to the ascending aorta and trachea
Opens into the right atrium of the heart at the level of the third costal cartilage
🔄 Main Tributaries
Brachiocephalic veins (right and left) — formed by subclavian and internal jugular veins
Azygos vein (drains thoracic wall and mediastinal structures)
Internal thoracic veins
Thoracoepigastric vein (important in collateral circulation)
🟩 Inferior Vena Cava (IVC)
📍 Position
Formed by the union of the right and left common iliac veins at the level of L5 vertebra
Ascends on the right side of the vertebral column, posterior to the liver and diaphragm
Passes through the caval opening of the diaphragm at T8 level
Empties into the right atrium
🔄 Main Tributaries
Common iliac veins
Lumbar veins
Renal veins (right and left)
Hepatic veins
Gonadal veins (right drains directly, left drains into left renal vein)
Inferior phrenic veins
🔄 Anastomoses Between SVC and IVC
Collateral Pathways for venous return if either vena cava is obstructed:
Azygos–hemiazygos system - Connects IVC tributaries (lumbar veins) with SVC tributaries (azygos vein)
Thoracoepigastric vein - Connects superficial epigastric vein (tributary of femoral vein/IVC system) to lateral thoracic vein (tributary of axillary vein/SVC system)
Vertebral venous plexuses - Provide communication along the vertebral column between SVC and IVC systems
Internal thoracic and inferior epigastric veins
⚠ Clinical Relevance
Obstruction of IVC or SVC leads to development of collateral venous pathways to maintain venous return
These anastomoses become dilated and visible in cases of SVC syndrome or IVC obstruction