Immunodiagnostics: Molecular Techniques, Immunohistochemistry, ELISA, PCR & Western Blot
1/100
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
101 Terms
What is molecular diagnostics?
A technique used to analyze biological markers in the genome and proteome to diagnose and monitor disease, detect risk, and determine effective therapies.
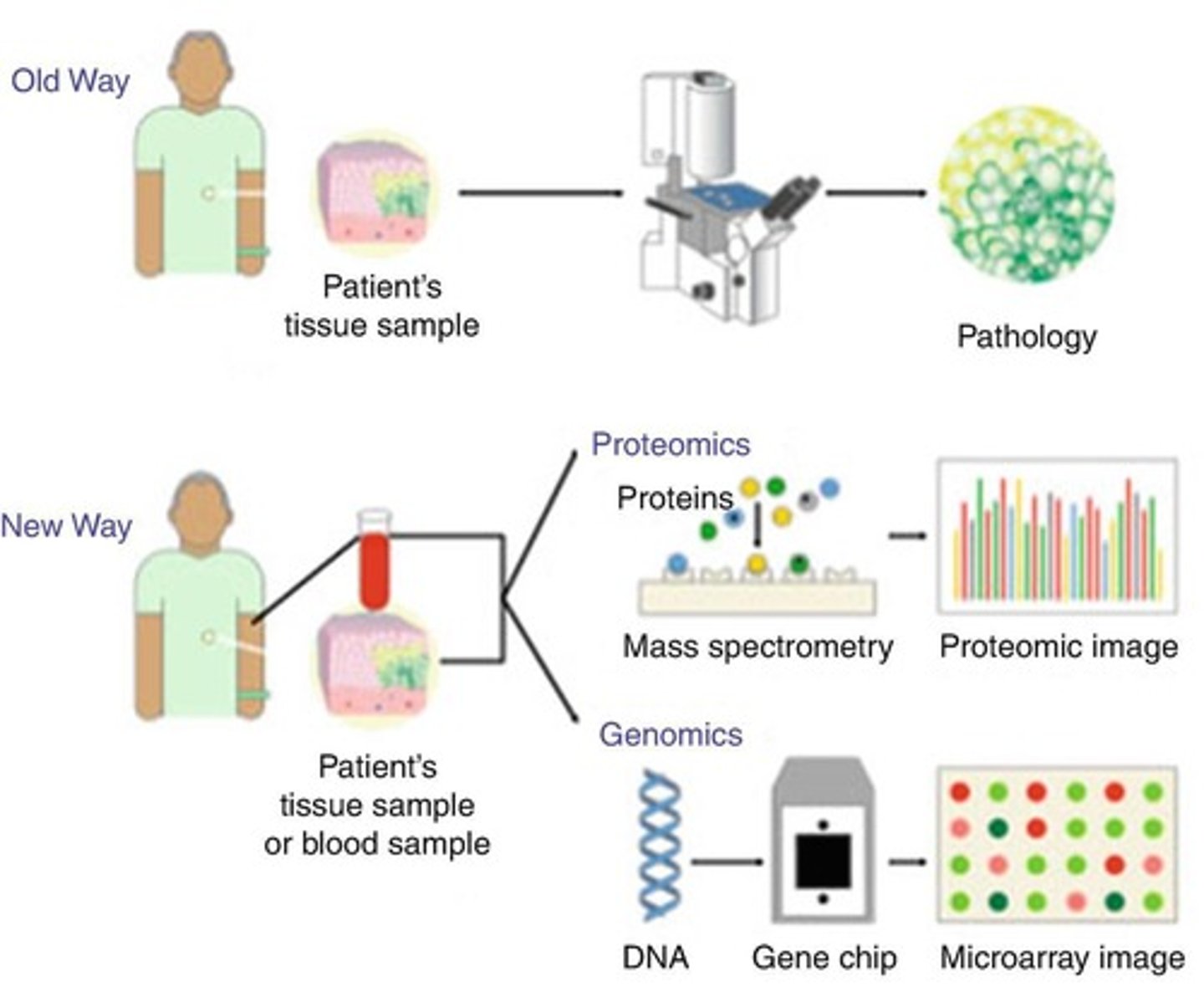
What are the general approaches to diagnosis in molecular diagnostics?
1. Direct detection (Microscopy, Staining) 2. Serological tests (Detects antibodies or antigens) 3. Nucleic acid methods 4. Protein methods.
What are the three types of diagnostic tests?
1. Screening tests: performed in clinically healthy patients. 2. Diagnostic tests: carried out in clinically diseased patients to confirm diagnosis. 3. Confirmatory tests: check if the patient is truly diseased, usually the gold standard.
What is the difference between sensitivity and specificity in diagnostic testing?
Sensitivity is the true positive rate, indicating the proportion of patients correctly identified by the test. Specificity is the true negative rate, indicating the proportion of disease-free patients correctly identified.
What is a gold standard test?
A test that is considered the most accurate and is used to compare the results of other tests.
What is a false positive result?
A test result indicating that a person has a specific disease when they actually do not.
What is a false negative result?
A test result indicating that a person does not have a disease when they actually do.
Why is it important to double check test results?
To confirm the accuracy of a diagnosis, especially in critical tests like HIV testing, which uses both screening and confirmatory tests.
What is the window period in testing?
The time between first infection and when the test can reliably detect that infection.
What are antigens?
Foreign molecular structures that can cause an immune response, classified into microbial and nonmicrobial antigens.
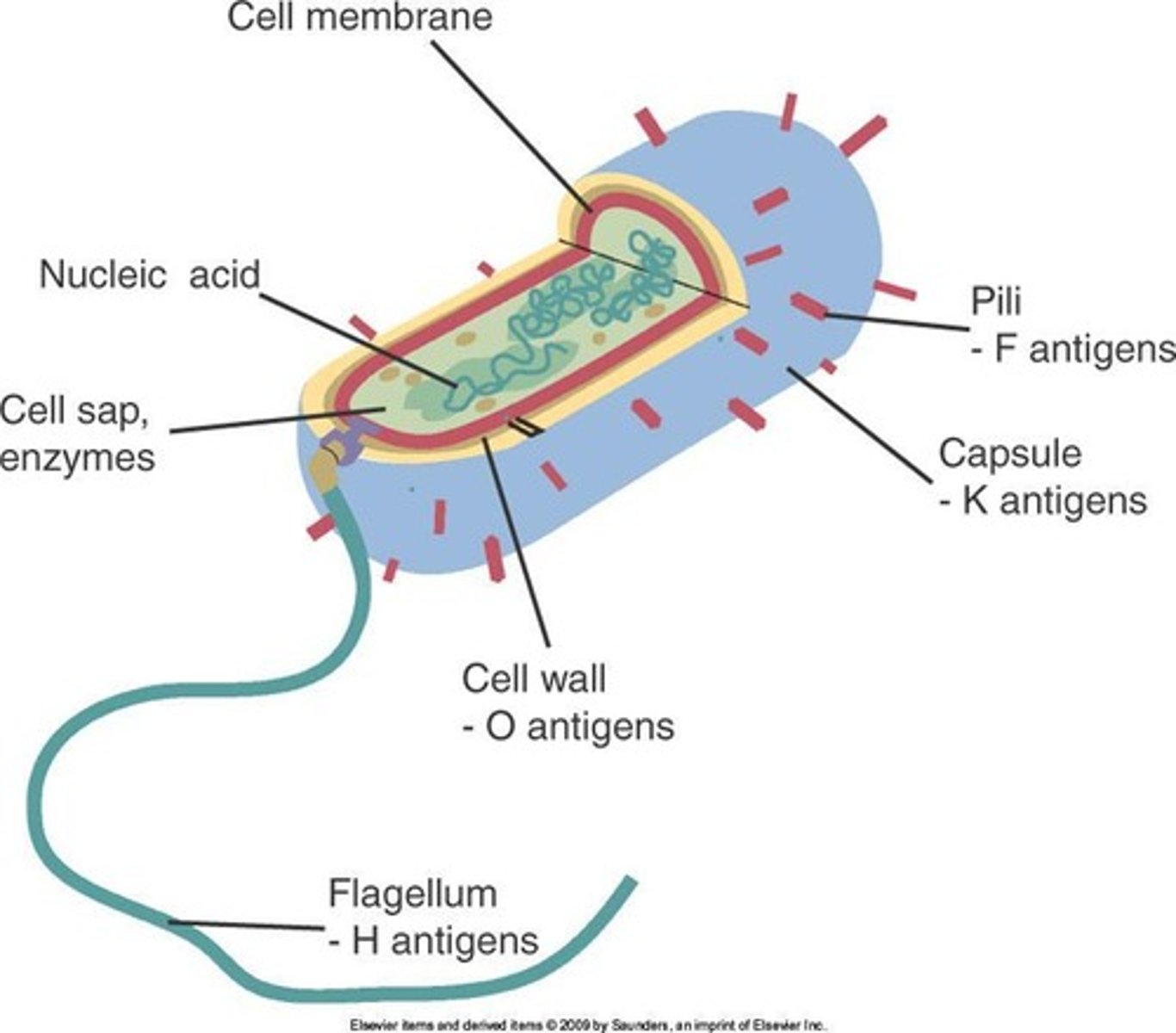
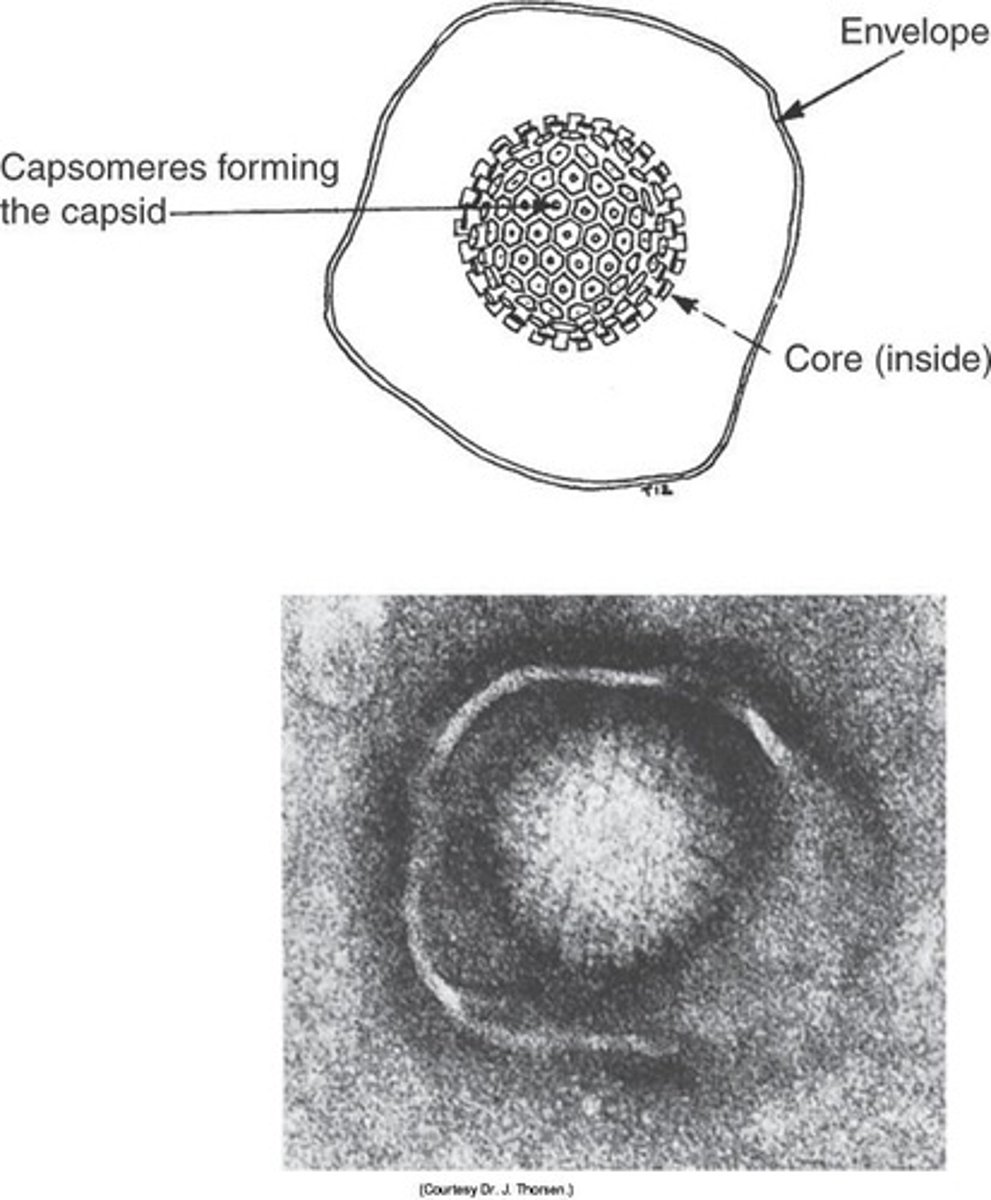
What are microbial antigens?
Antigens that include bacterial, viral, fungal, and protozoal and helminthic parasite antigens.
What are nonmicrobial antigens?
Antigens that include cell surface antigens and autoantigens.
What is the purpose of screening tests?
To determine whether clinically healthy patients are true positive or true negative for a disease.
What is the purpose of diagnostic tests?
To confirm the diagnosis among clinically diseased patients.
What is the purpose of confirmatory tests?
To verify if a patient is truly diseased, often considered the gold standard.
What is the role of the ELISA test in HIV testing?
It is a screening test used to detect HIV antibodies.
What tests are typically used as confirmatory tests for HIV?
Western blot or immunofluorescence tests.
What must happen for a person to be given a positive result in HIV testing?
Both initial and confirmatory tests must have reactive (positive) results.
What can happen during the window period of infection?
An infected person may not be detected as infected but can still transmit the infection.
What is the significance of understanding sensitivity and specificity?
It helps in evaluating the accuracy and reliability of diagnostic tests.
What is the difference between screening and diagnostic tests?
Screening tests are performed on healthy individuals to identify potential diseases, while diagnostic tests are used to confirm diseases in symptomatic patients.
What is the importance of protein methods in molecular diagnostics?
They are used to analyze proteins for disease diagnosis and monitoring.
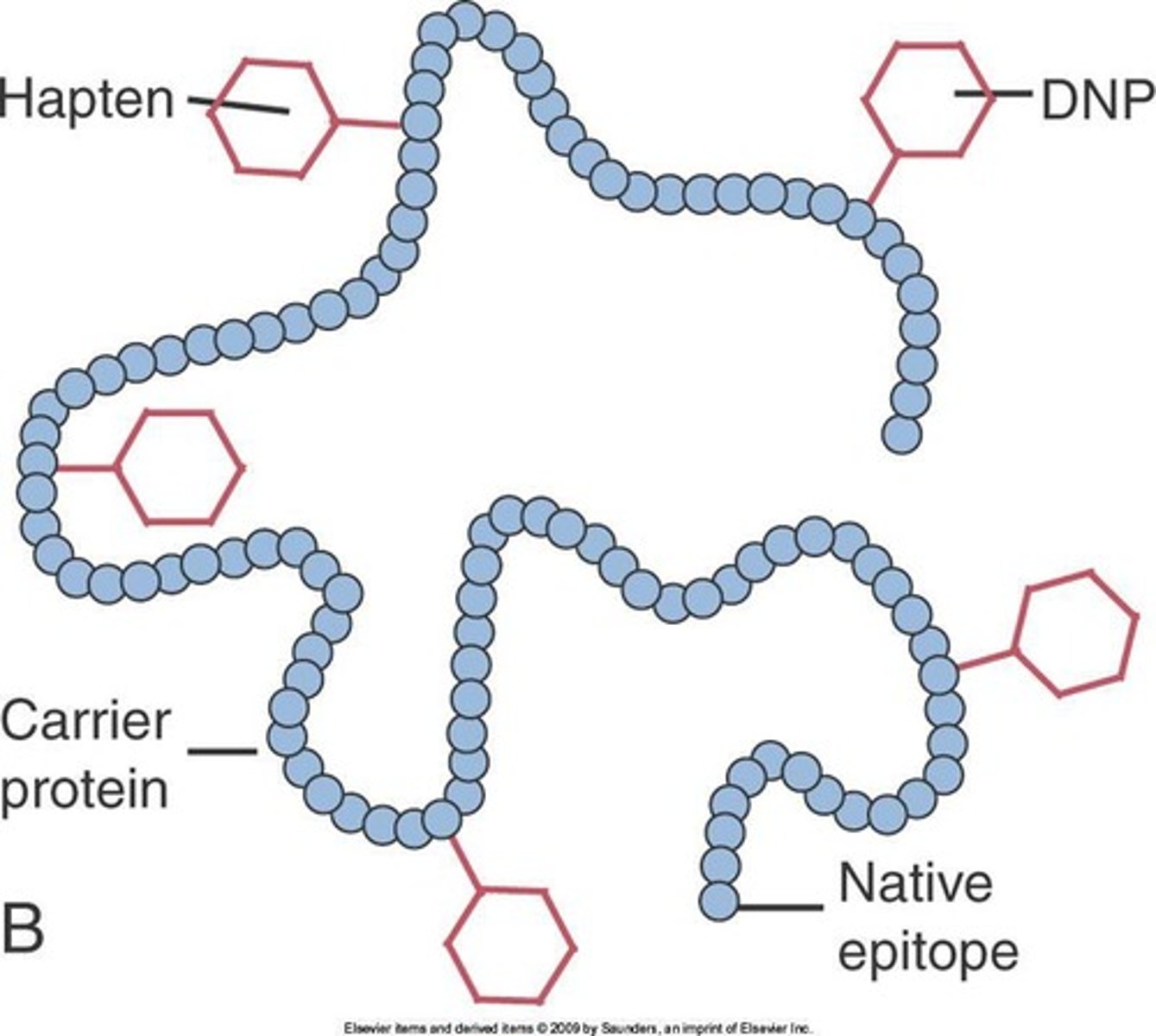
What are epitopes?
Epitopes are specific parts of antigens that can stimulate an immune response.
What are haptens?
Haptens are small molecules that are too small to be processed and presented to the immune system.
What is the order of immunoglobulin concentrations in serum?
IgG > IgM > IgA > IgD > IgE.
What is the primary role of immunoglobulin G (IgG)?
IgG plays a major role in antibody-mediated defense mechanisms and is the smallest immunoglobulin, allowing it to easily escape blood.
What is the significance of immunoglobulin M (IgM)?
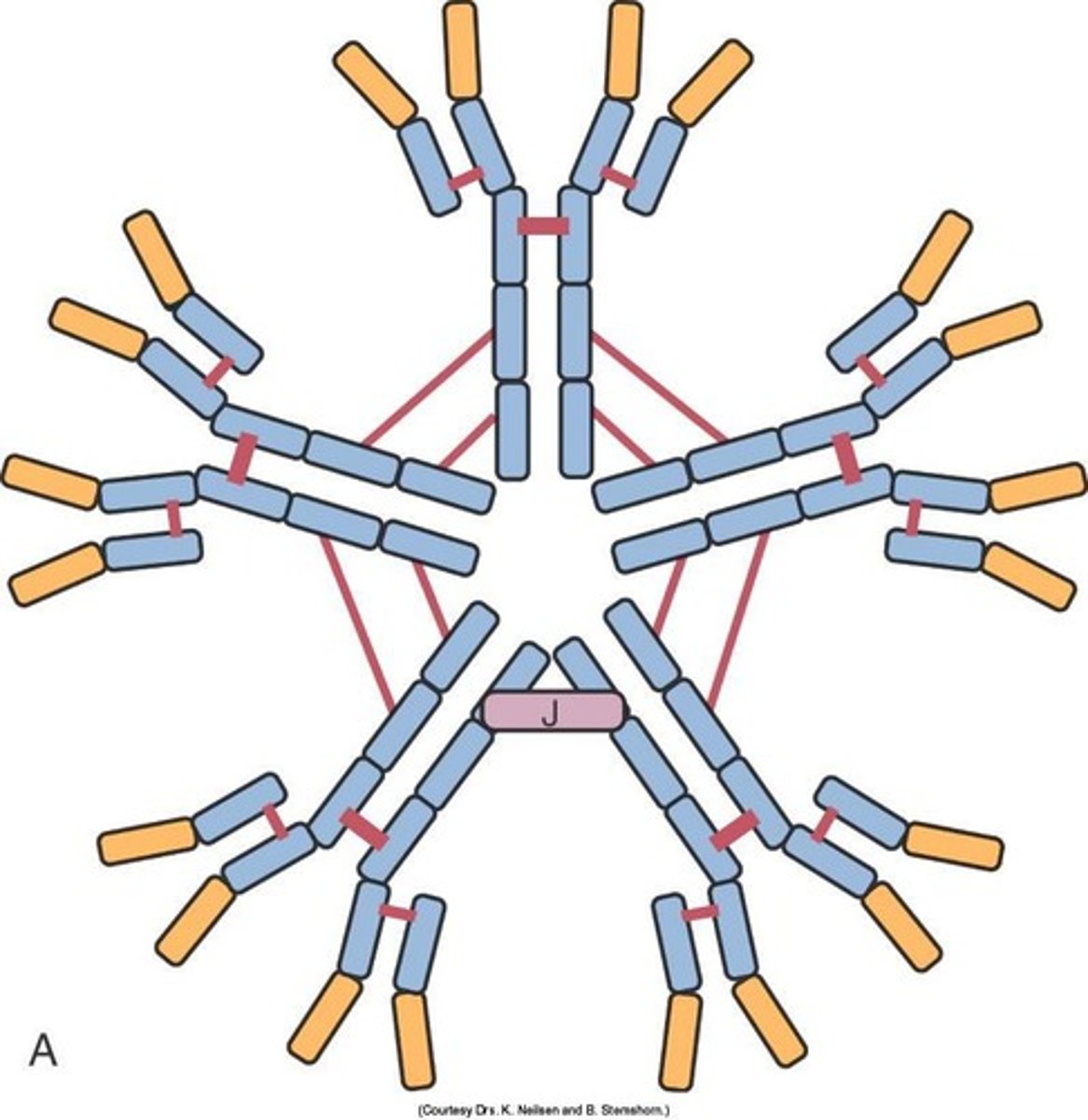
IgM is the major immunoglobulin produced in a primary immune response and is rarely found in tissue fluids.
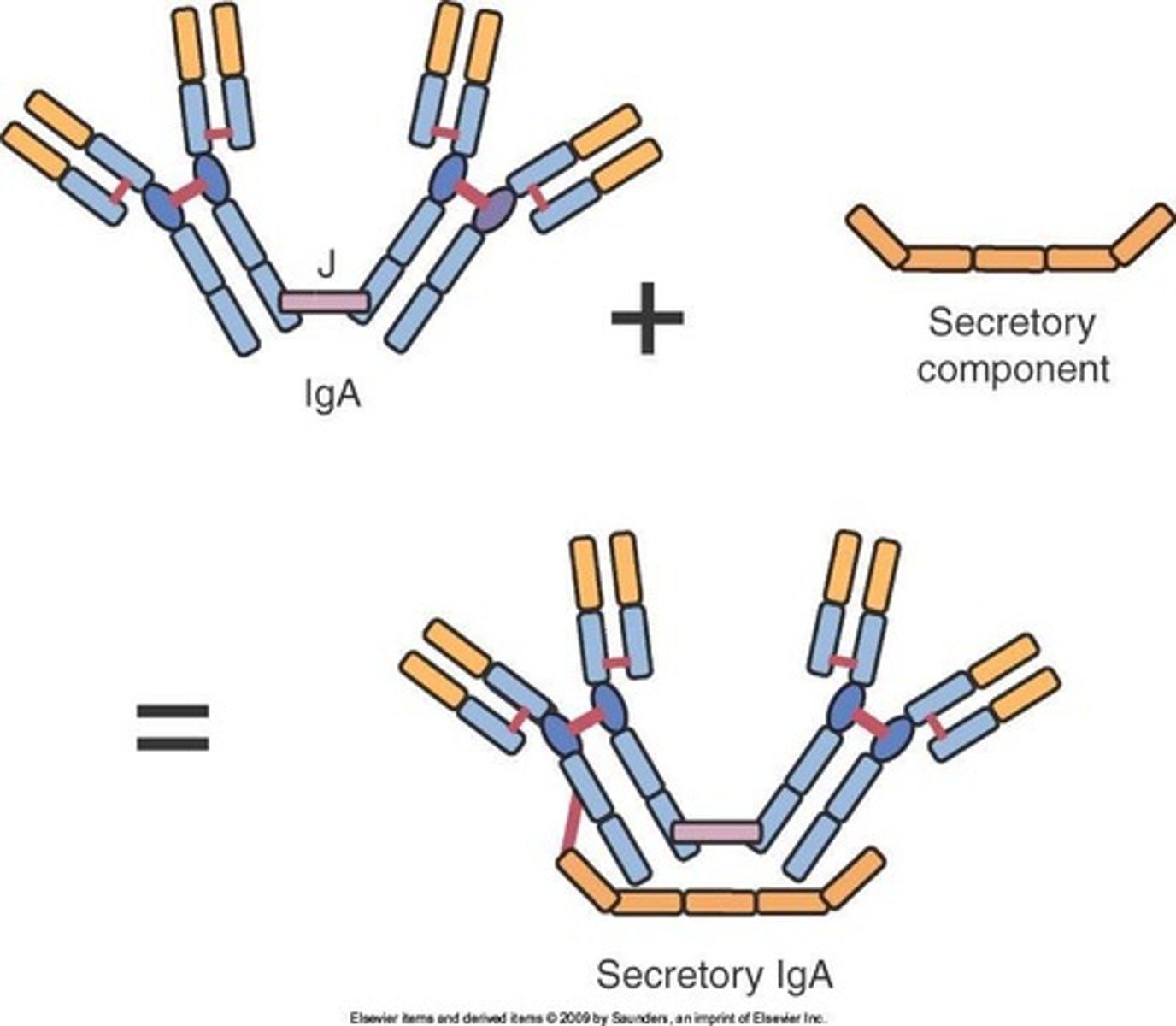
Where is immunoglobulin A (IgA) secreted?
IgA is secreted by plasma cells located under body surfaces, including the intestines, respiratory tract, urinary system, skin, and mammary gland.
What is the function of immunoglobulin D (IgD)?
IgD is evolutionary labile, shows many structural variations, and can be destroyed by mild heat treatment.
What role does immunoglobulin E (IgE) play in the immune system?
IgE triggers acute inflammation and responds to parasitic infections, but is present in extremely low concentrations in serum.
What is immunohistochemistry?
Immunohistochemistry is a technique that uses antibodies conjugated to enzymes to visualize and localize specific antigens in tissue samples.
What is the difference between immunohistochemistry and immunocytochemistry?
Immunohistochemistry applies to biological tissues, while immunocytochemistry applies the same process to individual cells.
Why is localization of specific proteins important in diagnostics?
Localization of specific proteins is crucial for diagnostics in fields such as cancer or infectious diseases, as it can provide evidence about a patient's condition.
What is the significance of HER2 receptor overexpression in breast tissue?
Overexpression of the HER2 receptor in breast tissue is often correlated with breast cancer development.
What are polyclonal antibodies?
Polyclonal antibodies result in greater staining and excellent signal but can give false positives by binding to unwanted sites.
What are monoclonal antibodies?
Monoclonal antibodies have high specificity, reducing false positives, but often produce a weaker stain.
What are pooled monoclonal antibodies?
Pooled monoclonal antibodies provide excellent staining and high specificity, although they have limited availability.
What should a secondary antibody be against?
The secondary antibody should be against the species in which the primary antibody was developed.
What is the role of secondary antibodies in immunohistochemistry?
Secondary antibodies are labeled with enzymes like HRP or biotin for staining or amplifying the signal.
What is ELISA?
ELISA (Enzyme-Linked Immunosorbent Assay) is a technique used to detect and quantify proteins, antibodies, and hormones.
What is the purpose of an ELISA test?
To identify a substance using antibodies and color change.
What type of assay is commonly used in ELISA?
Solid phase enzyme immunoassay (EIA) to detect the presence of a substance.
In what industries is ELISA used?
In diagnosis and quality control.
What is the role of antibodies in ELISA?
Antibodies bind to specific regions called epitopes.
What are the two main variations of ELISA?
Detecting the presence of antigens and detecting the presence of antibodies.
What is a Direct ELISA?
It involves the attachment of the antigen from the sample to the solid phase, followed by the addition of enzyme-labeled antibody.
What are some problems associated with Direct ELISA?
Measurement of crude samples is difficult, and contaminating proteins can compete for plastic binding sites.
What is an Indirect ELISA?
An ELISA variation that uses a secondary antibody to detect the primary antibody bound to the antigen.
What is a Competitive ELISA?
An ELISA variation where the amount of labeled antigen is inversely proportional to the amount of antigen in the sample.
What is a Sandwich ELISA?
An ELISA variation that uses two antibodies to capture and detect the antigen.
What is a Labeled Antigen ELISA?
An ELISA variation where the antigen itself is labeled and used to compete with the sample antigen.
How is the result of an ELISA interpreted qualitatively?
Results can be positive, negative, or indeterminate based on optical density (OD) readings.
What does an OD reading greater than 0.500 indicate?
A positive result.
What does an OD reading between 0.300 and 0.499 indicate?
An indeterminate result.
What does an OD reading less than 0.300 indicate?
A negative result.
What are some key considerations in test kit design for ELISA?
Know what you are detecting (antibody or antigen), check possible proteins for detection, and study the disease in question.
What is PCR?
A rapid procedure for in vitro enzymatic amplification of a specific segment of DNA.
What principle does PCR rely on?
The denaturation of double-stranded DNA at high temperatures and the synthesis of new DNA by DNA polymerase.
What is the result of increasing cycles in PCR?
An exponential increase of double-stranded DNA.
What is the function of a PCR machine (thermal cycler)?
It automates the changes in temperature needed for different steps in PCR, including denaturation, annealing, and extension.
What is the optimal magnesium concentration for PCR?
1 to 3 mM; excess free Mg can reduce enzyme fidelity and increase non-specific amplification.
What is the recommended enzyme concentration for Taq polymerase in a 50 µL reaction?
1.25 U of Taq polymerase.
What are the key considerations for primer design in PCR?
Primers should be 15 to 30 bases long, avoid 3 G or C in a row near the 3' end, have 40 to 60% GC content, and should not form secondary structures.
What is the importance of template DNA quality in PCR?
The quality of DNA template is crucial as contaminants like salts and organic solvents can affect PCR performance.
What is the maximum amount of template DNA recommended for PCR?
Less than 10 ng/µL of DNA.
What happens during the denaturation step of PCR?
The double-stranded DNA melts open to form two single strands.
What occurs during the annealing step of PCR?
Primers bind to the single-stranded template DNA.
What is the purpose of the extension step in PCR?
DNA polymerase synthesizes new DNA strands by extending from the primers.
How does the number of target DNA fragments change during PCR?
It increases exponentially; for example, 30 cycles can produce 2^30 copies, or approximately 1 billion copies.
What are some general applications of PCR?
Applications include screening for mutations, rapid genotyping, assays for known mutations, and gene expression analysis (RT-PCR).
What is the impact of primer dimers in PCR?
They reduce amplification efficiency, lead to inaccurate quantification, and can result in misleading expression levels.
What is gel electrophoresis used for?
It is a technique for analyzing nucleic acids and proteins by separating molecules based on their movement through a gel under an electrical field.
How does DNA behave in agarose gel electrophoresis?
DNA is negatively charged and migrates toward the positive pole (anode) when placed in an electrical field.
What is the role of agarose in gel electrophoresis?
Agarose creates a porous matrix that slows the movement of DNA and allows separation by size.
What is the effect of high enzyme concentrations in PCR?
High amounts of enzymes can lead to artifacts in PCR products without significantly increasing yield.
What should be done to magnesium chloride before use in PCR?
It should be completely thawed and vortexed to prevent precipitates.
What is the significance of verifying the purity of DNA samples?
Purity affects PCR performance; contaminants can inhibit the reaction.
What is one method to remove contaminants from DNA samples?
Ethanol precipitation.
What does the acronym ARDRA stand for in PCR applications?
Allelic discrimination by size or susceptibility to restriction enzyme.
What is the role of Taq polymerase in PCR?
It is the enzyme that synthesizes new DNA strands during the extension phase.
What is the consequence of inefficient amplification in PCR?
It results in wasted reagents, time, and labor.
What is the typical migration direction of DNA in gel electrophoresis?
DNA migrates toward the positive pole due to its negative charge.
What factors affect DNA migration in agarose gel electrophoresis?
Applied voltage, size of DNA, type of agarose, concentration of agarose, electrophoresis buffer, conformation of DNA, and presence of marker dyes.
What is the relationship between DNA size and migration speed in agarose gel?
The smaller the DNA, the faster it moves in agarose gel.
What components are included in the 6X sample loading buffer?
Bromophenol Blue (for color) and Glycerol (for weight).
What is the purpose of the 6X sample loading buffer in DNA electrophoresis?
It allows the samples to be seen when loading onto the gel and increases the density of the samples, causing them to sink into the gel wells.
What is ethidium bromide used for in gel electrophoresis?
It binds to DNA and fluoresces under UV light, allowing visualization of DNA on a gel.
What precautions should be taken when using ethidium bromide?
It is a powerful mutagen and moderately toxic; gloves should be worn at all times.
How can ethidium bromide be applied to the gel?
It can be added to the gel and/or running buffer before the gel is run or the gel can be stained after it has run.
What is SYBR gold/green and how does it work?
It is an asymmetrical cyanine dye for nucleic acid staining that binds ds DNA, resulting in a DNA-dye complex that absorbs blue light and emits green light.
What is the detection limit of SYBR gold/green?
20 pg of DNA.
What is Gel Red and how does it compare to ethidium bromide?
Gel Red is structurally related to EtBr, fluoresces orange under UV, and is marketed as a less toxic and more sensitive alternative.
What is Western blotting?
An analytical technique used to detect specific proteins in a sample of tissue homogenate or extract.
What is the general procedure for Western blotting?
It typically involves separating proteins by SDS-PAGE, transferring them to a membrane, and probing with specific antibodies.
What is the role of SDS-PAGE in Western blotting?
SDS-PAGE separates proteins based on their size before they are transferred to a membrane for detection.
What is the purpose of using a DNA ladder standard in electrophoresis?
It serves as a size reference for estimating the size of DNA fragments in the samples.
What are the types of PCR mentioned in the notes?
Traditional PCR, Gradient PCR, Reverse transcription PCR, and Quantitative PCR.
What is the significance of buffer presence in electrophoresis?
The electrophoresis buffer maintains pH and ionic strength, facilitating the migration of DNA.
What is the effect of agarose gel density on DNA migration?
Higher density agarose gels slow down the migration of DNA fragments, while lower density gels allow faster movement.
What is the function of marker dyes in DNA electrophoresis?
Marker dyes help visualize the progress of DNA migration during electrophoresis.