Gram Positive Cocci
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
50 Terms
Family: Micrococcaeae includes genera ___, but Staphylococcus is now __.
Micrococcus, Rothia, Staphylococcus;
it’s own family = Staphylococcaceae
Staphylococceae general characteristics
GPC
single, pairs, tetrads, or clusters
catalase + except Rothia
col entire, smooth, opaque / white & butyrous growth
What test diff Staph from Strep? How does it work
catalase test
reagent = 3% H2O2
+ → production of O2 and H2O (bubbles)
- → no bubbles
Which genera are catalase + and -?
catalase + = Staphylococcus & Micrococcus
catalase - = Streptococcus & Enterococcus
What can cause a false +?
if pick up blood/rbc from agar → contains catalase → false +/bubbles
Which bacti is catalase + besides Staphylococcus? How to diff b/t other Staphylococceae?
Rothia mucilaginosa (sticky staph)
Rothia can’t grow in 5% NaCl
once catalase +, what test is done next to determine if S. aureus?
slide coagulase
media = rabbit plasma w/EDTA
rapid
tests for coagulase enzyme (which alters fibrinogen → clot), specifically clumping factor/cell-bound coagulase
if (-) → confirm w/ tube coag test
if (+) → S. aureus
why does slide coagulase test need negative control? what to do to if this occurs?
neg control checks for bacti that auto-agglutinate in saline → if auto-agglut → tube coag test
when is tube coagulase test done? what is it and what to look out for?
when (-) from slide coag test → will test for free coagulase
inoculate loop of bacti into 0.5 mL of rabbit plasma → incubate 35C for 4 hr → observe at 4 hr mark in case of staphylokinase which lyses clot → if (-), incubate overnight
pos = clot formation or aggulatination
neg = none
Staph Latex / hemagglutination test
detect what?
advantage/disadvantages?
detect: clumping factor, protein A (all S. aureus have virulence factors), and antigenic proteins
rapid & more definitive, if + → call it S. aureus
false - b/c some strains don’t produce enough of ^^^
false + from certain Strep A, C, and G
get + from other Staph sp like S. lugdenesis, schleiferi, etc…
S. aureus
infects where
usually founds in __
produces enterotoxins ___
in skin (furuncles, carbuncles, cellulitis, impetigo), pneumonia, meningitis, endocarditis
thermostable enterotoxin (food poisoning): projectile vomiting & fast incubation time
TSST-1 → toxic shock syndrome
exfoliatin → scalded skin syndrome in kids
ID of S. aureus
grows in 18-24h at 37C
turns golden yellow w/ age
typically beta-hem rxn
coagulase +
S. aureus epidemiology
Most are resistant to __?
a significant nosocomial pathogen (hospital acquired)
95% resistant to penicilin due to Beta-lactamase or cell wall binding protein
MRSA stands for
what happens if pt is + for MRSA?
Methicillin/oxacillin resistant S. aureus due to mecA or mecC gene → codes for PBP2A (penicillin binding protein)
Why is cefoxitin disk better for detecting MRSA than oxacillin disk or agar?
What will it look like?
cefoxitin (= a cephalosporin, also has beta-lactam ring) → detects heteroresistant strains of MRSA (=don’t express Abx-R genes)
MRSA → cefoxitin-R → report 6mm ZOI
What does MRSA look like on chromogenic media?
Spectra MRSA → denim blue col
CHROMagar MRSA → mauve col
Methods to rapidly detect MRSA?
detection of mecA gene via PCR/probe, fluorescence tests, or slide latex agglutination
MRSA are resistant to ___ →
methicillin, oxacillin, nafcillin (semisynthetic penicillins) → other beta-lactam drugs are reported as resistant even if in vitro tests appear sensitive
What may be misID’d as S. aureus?
S. lugdunensis is misID’d b/c can look + on slide coag test (but is coag -) bc may have clumping factor and yellow pigment col
confirm w/tube coag test that it’s coag -
part of normal skin flora (toe or inguinal fold) → but can cause soft tissue infns
AST interpretation reported like a S. aureus, NOT CNS
ornithine decarboxylase +
Coagulase-negative Staph (CNS)
significant species and when to w/u?
Staph epidermidis - bad bc produce slime → adhere to catheters & prosthetics
S. saprophyticus - ID from novobiocin-R, UTI in young females
only do w/u if multiple + BC or +BC AND +catheter tip
S. saprophyticus is resistant to ___.
novobiocin
< 16 mm ZOI
How to diff Micrococcus luteus from Staph spp.?
bright yellow col, coag neg
diff from Staph
glucose oxidizer (Staph ferm glucose)
bacitracin-S (Staph are R)
Streptococcus & related general traits
GPC in pairs and chains
facultative anaerobes
translucent, shiny, grey col
catalase -
What is the Lancefield Grouping system?
used for beta-hemolytic Streptococci
based on carbohydrate cell wall Ag → detected by kits via heat, chemical, enzyme
groups include:
A and B - can use biochem tests to ID
C, F, G - need serology tests to ID
D = Enterococcus?
Group A Strep aka __. Colony morph? Virulence mechanism?
Strep. pyogenes
tiny, beta-hemolytic, with larger zone of hemolysis
can be elongated cocci in chains
Streptolysin O (oxygen labile ie breaks down in O2) → if stab into agar → enhanced zone of beta-hemolysis
GAS clinical manifestations
spread via droplets or direct contact
most common cause of pharyngitis
impetigo, erysipelas
necrotizing fasciitis (got thigh swab from unknowns!)
strep toxic shock syndrome
after infection (sequelae) →
rheumatic fever: Ab from infn attack heart tissue
glomerulonephronitis - Ab/Ag complex deposits in kidneys
Media used for GAS?
Bacitracin → ?
PYR → ?
SXT or SSA
bAcitracin-S (A on disk is for group A strep)
PYR + (pink throat)
GAS rapid tests
use throat specimen
positives are conclusive, but neg must have culture
Group B Strep (Strep. agalactiae)
colony morph
found where?
clinical manifestations
larger col w/ narrow zone of beta-hemolysis (or diffuse zone)
normal flora of GI & genitourinary tracts
GBS is screened for in pregnant women in 3rd trimester → neonatal pneumonia, septicemia, meningitis
in adults: UTI, bacteremia, endocarditis, pneumonia, osteomyelitis
media for GBS?
Hippurate hydrolysis → ?
CAMP test → ?
use CNA & LIM broth (contain colistin & nalidixic acid)
hippurate hydrolysis + (hippy girls/bros like camping and gardening)
CAMP test + (like to camp in the vag/rectal area)
**hip gals (galactiae) camp positive
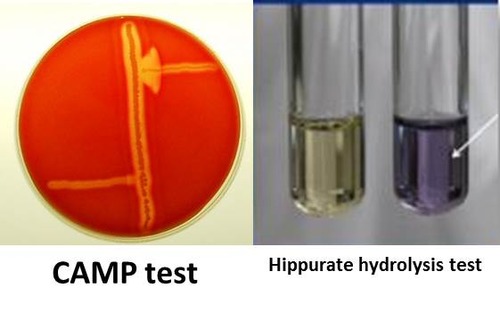
hippurate hydrolysis test
principle
steps
result
sodium hippurate → benzoic acid + glycine
glycine + ninhydrin → purple complex
inoculate bact in 0.5 mL distilled water in tube → add sodium hippurate disk → 35C for 2hr → 0.2 mL ninhydrin reagent
pos = blue/purple w/in 5 min
neg = no color change
Hippurate hydrolysis test is positive for
GBS, Listeria monocytogenes, Gardnerella vaginalis, Campylobacter jejuni
“Hippy Girls Like Camping & Gardening”
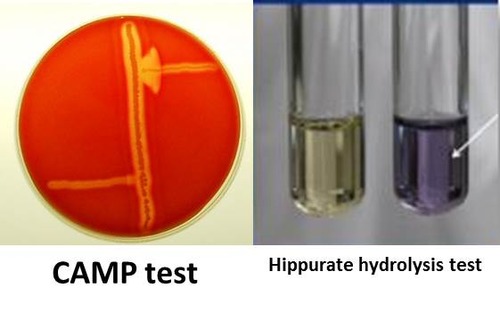
CAMP test
principle
steps
results
ID for GBS
free CAMP factor reacts w/Staphylococcal beta lysin to lyse rbcs
single straight streaks of test bact & CAMP S. aureus are made perpendicular to each other on SBA
pos = enhanced zone of beta hemolysis in shape of arrowhead pointing toward S.aureus
neg = no enhanced zone of hemolysis
Group C, F, and G Streptococcus
sources
clin manif?
how to ID?
still beta-hemolytic
normal flora of skin, nasopharynx, GI and genital tracts
infns in immunocompromised pt → similar infn as GAS and GBS, but no sequelae like GAS
ID w/kits
Group D Strep includes __
morphology
clinical significance
intrinsically resistant to __?
Enterococcus & Group, non-Enterococcus
grey-white, translucent, alpha or non-hemo, some rare beta-hemo
found in soil, food, water, normal flora of birds, animals, human (GI and female GU tract) → can cause UTI, bacteremia, endocarditis, mix wound infn
cephalosporins and aminoglycosides → need to treat w/multiple Abx for synergistic effect
How to distinguish Enterococcus spp vs Group D non-Enterococcus?
bile esculin
PYR
salt broth 6.5% NaCl
both have group D Ag
bile esculin → all group D + (black → dlack)
PYR → only Enterococcus + (pink)
salt broth → only Enterococcus + (purple or yellow growth)
bile esculin slant
reaction
results
40% bile → inhibits most G+ → used to diff Group D from non-group D strep
esculin → esculetin + dextrose → esculetin + ferric citrate → black pigment
pos = >1/2 slant turned black
neg = <1/2 slant black
PYR test
principle
steps
result
used to diff Enterococcus spp from Group D, non Enterococcus
PYR enzyme made by GAS & Enterococcus.
PYR -L pyrglutamyl aminopeptidase → free beta-naphthylamine —cinnamaldehyde → red complex
moisten substrate disk w/sterile water → touch colony to disk → incubate 2 min → add cinnamaldehyde
pos = red color on disk → GAS or Enterococcus spp.
neg = no color change
PYR + organisms
GAS → r/o Group B, C, F, G Strep, S. viridans
Enterococcus spp. → r/o S. gallolyticus
(some Staphylococcus strains, Micrococcus, Gemella, Lactococcus)
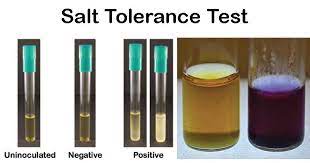
6.5% NaCl test
used to ID Enterococcus spp
inoculate and incubate overnight 35C
pos = growth (w or w/o change to yellow)
neg = no growth
Enterococcus faecalis
causes most human enterococcal infn
non-hemo
** Cali = huge population, most infns, non-hemo bc californians are chill → not resistant ie VRE
Enterococcus faecium
alpha-hemo
causes 10-15% enterococcal infn
more commonly vancomycin-R (VRE)
Enterococcus gallinarum/cassliflavus
motile
intrinisically vancomycin intermediate
Group D non Enterococcus aka
Streptococcus bovis (old name) → S. gallolyticus
assoc’d w/colon cancer
Strep pneumoniae
morphology
clin manif
GPC in pairs, lancet shaped, may have capsule
always alpha-hemo, older colonies may be donut-shaped (autolysing)
leading cause of bact meningitis and pneumonia; bacteremia, sinusitis, otitis media
ID’ing Strep pneumoniae
bile solubility
Optochin test
Quellung reaction
bile solubility → +, colony dissolves → can see alpha-hemo
Optochin → S
Quellung rxn (only for epidemiology) → capsule is enhanced for certain S. pneumo strains
Viridans Group Streptococcus
morphology
clinical signifance
typically alpha-hemo, but can be non or beta (viridans vAries)
butterscotch odor (sweet → viridans (veneers) → endocarditis)
opportunistic pathogens, normal flora of oral cavity, GI tract, female genital tract → poor dental care → bacteremia, endocarditis, meningitis
Viridans Group Strep ID
PYR and salt
bile esculin
optochin
bile solubility
all negative!
w/u only if multiple +BC
Abiotrophia spp aka ___
requires ___ to grow → grows on __ agar not SBA.
Will grow on SBA if?
PYR → ?
Granulicatella spp.
pyridoxal or thiol cmpds or cysteine; choc
linked to endocarditis (normal oral cavity flora)
beta-hemolytic Staph on SBA → B-hemo → sattelite streptococci in lysed region
PYR → +
other catalase - GPC