CNP III: Sx Management
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Points to remember
Wait for 6/12 stability before Sx
Conservative management in the interim
Post-op care should and will involve conservative
treatment
Don’t forget this
Surgery to regain BSV/improve
function/psychosocial
Pharmacological
Botulinum Toxin (pg187 A&D)
Weaken un-opposed antagonist
Prevent contracture
Maintain BV
Unsuitable for Sx
Diagnostic
Mimics surgery
Bupivacaine
Local Anaesthetic – has a myotoxic effect
Strengthen u/a muscle
Shortens and stiffens muscle
Up to 10^ of deviation
Combined with BT
Surgery Re-cap
Aims
Straighten the eye : functional or non-
functional
Restore/maintain concomitance
Relieve symptoms
Minimal number of procedures
Reversible surgery if possible
Changes in position of insertion or muscle length
results in change in magnitude or direction of force
• Weakening procedures
– Recession
– Myectomy
– Fadenisation
– Disinsertion
• Strengthening procedures
– Resection/ Advancement
– Tuck
Surgery: III - Complete
Total- difficult!
Treat the exotropia
Patient expectations
Ptosis
Ansons and Davis
SO anterior medial transposition
LR medial transposition
Horizontal muscle Sx with or without traction sutures
Partial
Dependent on residual function and muscles affected
Pilocarpine 1% for photophobia
Importance of Orthoptic investigation to this planning
7
III CNP
What are we left with.......
Complete/Inferior Div/Superior Div
Exotropia - could be large
Hyper or Hypo
Combination of H & V
May need to tackle one at a time multiple
procedures
Advice to patient
Complete total III CNP difficult:
Large recession of MR and resection of LR
Traction sutures to anchor eye in new position
Expect post-op diplopia
Exo can re-occur
III – Traction Sutures
Traction Sutures (Kahir, Dawson and Lee, 2008)
LR recess, MR resect
Adduction traction suture (6/52)
30/33 left with ‘good alignment’ based on patient satisfaction
Mean improvement – 47PD
Yonghong et al (2008)
Isolated or combined muscle surgery where appropriate
Good alignment
No treatment yields consistently excellent results
Flanders et al (2012)
Good functional and cosmetic outcome
Muscle involvement dependent
Residual muscle function
Complications of horizontal and vertical deviation
III CNP – Divisional
Superior Division
Mild u/a
Weaken contralateral IO
If small angle in pp
Recess contralateral SR (balancing the deviation)
Recess contralateral SR and ipsilateral IR (if large angle in pp)
Marked u/a or limitation
Transposition of horizontal recti
III CNP – Divisional - inferior
Similar to Complete III
Exotropia MR recess, LR resect
Vertical deviation
SR recession
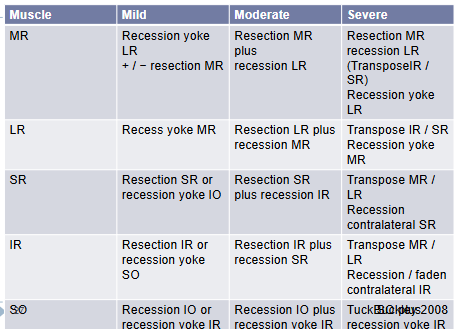
IV Surgery decisions e.g. Scott/Knapp
What are we left with......
Hyper
Torsion
Decision based on
Deviation in pp
Position of maximum deviation
Position of maximum symptoms
Measurement
Motility
IV Surgery decisions e.g. Scott/Knapp
Class 1- 7 not all use this system
Based on tackling the largest deviation/ motility problem
Hyper
Strengthen SO
Weaken IO
Balance out recess contralateral IR
Torsion
Harada Ito
Surgery: IV
Hatz, Brodsky and Killer (2006)
Isolated IO Sx
Favourable up to 15PD in pp
Durnian and Marsh (2011)
SO Tuck
71% success with one procedure
Vertical and torsion improved
‘One tightness fits all’
Nishimura and Rosenbaum (2002) – Harada Ito
Reduction from 10.7o 1.0 o 2 months post-op (p<0.05)
Regression between 2 months and 2 years follow-up (5.3o)
Murray, Marsh and Newsham (2021)
Reduction in torsion post-op (p<0.01), remained for 12/12
Regression to pre-op measurement
Significantly reduced V-eso pattern (p<0.05)
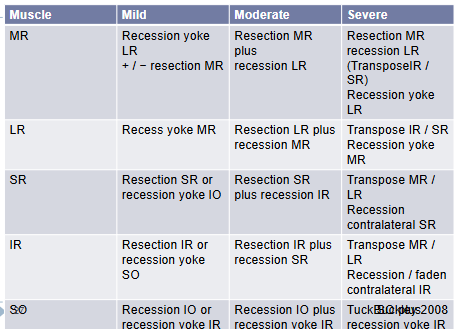
6th sx
Esotropia-
Worse for distance
Total vs Partial
LR resect, MR recess
Transpositions
Partial VI – Ansons and Davis (2014)
Concomitant
Recess / Resect (poss x3 muscles if >30^)
Incomitant (pp)
Pt has dev in pp, worse in lat gaze
Recess / Resect with Faden’s
Incomitant (lat gaze)
Pt has no dev in pp but dev in lat gaze
Contralateral MR Faden
Recession contralateral MR
Surgery: VI
Role of BT here in planning
Leiba et al (2010)
Vertical transpositions and MR BT
Pre-op (38PD) to 3/12 post op (4PD) – p =0.0004
Pre-op to final follow-up (8PD) – p = 0.003
73% no diplopia pp at final follow-up
32% did have vertical deviation at final follow-up (n=3)
Holmes et al (2002)
Long term outcomes chronic VI (24/12)
52% fully successful
75% partially successful
Concluded chronic VI require 2 surgical
procedures
Total VI – Ansons and Davis (2014)
No residual function of LR
Full muscle transposition
Less risk of anterior segment ischemia
Partial muscle transposition
Hummelsheim’s (lateral trans of vertical recti)
Jensen’s (union of vertical to lateral recti)
General Surgical Principles: Isolated muscle paresis
Summary of Management
Indications for further investigations are aetiological
dependent
6/12 waiting time for recovery before Sx or other
permanent options
Vascular palsies tend to recover well
BT may be an adjunct to surgery
Post-operative care
Back to Conservative!!