Pulmonary and Peripheral Systems
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
The hearts supply to itself is part of the
systemic circulation
Deoxygenated (O2-poor) blood return enters ______________with small amount from coronary sinus
RA via SVC and IVC
In pulmonary circulation where does blood go from RA?
to RV via TV
From the right ventricle where does blood go?
Pulmonary trunk via pulmonary valve
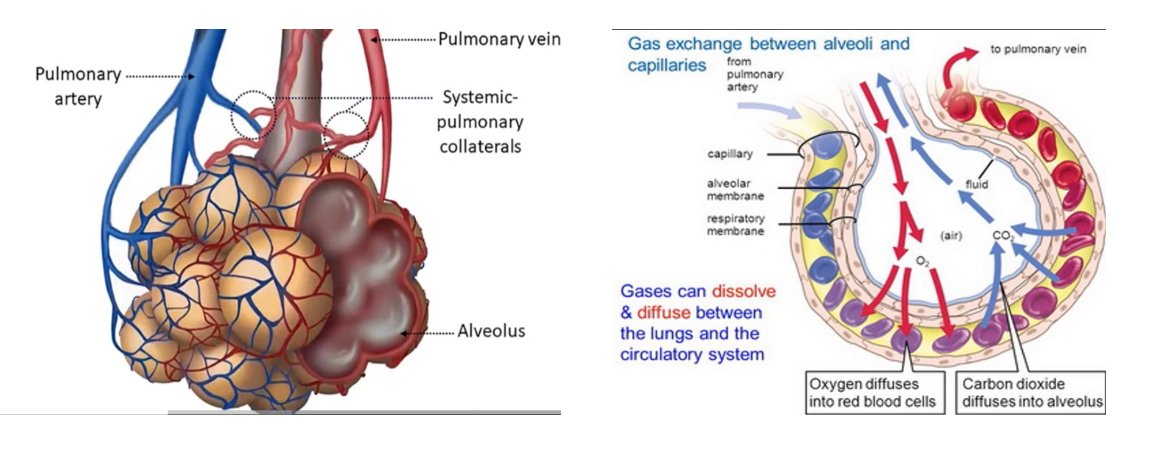
Pulmonary trunk to L and R pulmonary arteries, to smaller pulmonary arterioles, and finally to capillaries where
gas exchange (discharging CO2 and picking up O2).
In the lungs, gas exchange happens in the
alveoli
Pressure in capillary bed in pulmonary circulation
the artery behaves like a vein because they have a thinner wall and less smooth muscle
Main function of pulmonary circulation is
Gas exchange
Filtering blood: remove micro emboli
Metabolic regulation of hormones
Endothelium keeps homeostasis
Inflammation/infection damages this endothelium results in
extravasation of proteins, cells, and fluid
Pulmonary Circulation and Lymphatic System
keep alveolar membrane dry and helps drain pleural fluid
With venous drainage, it helps create negative pleural pressure (-4 to -7 mmHg) helping alveoli to tether to visceral pleura, avoiding collapse
Bronchial vasculature (blood supply for the lungs) is part of ________ circulation.
systemic
Bronchial vasculature supplies blood to the
tracheobronchial tree and terminal bronchioles
What are the two pathways for the bronchial veins?
Deep bronchial veins
Superficial veins
Deep bronchial
veins partially drain into pulmonary venous system then to LA (~0.5% total return).
Superficial bronchial
veins drain into azygos veins on the right, and hemiazygos vein on the left, part of systemic venous system.
ABG is
Arterial Blood Gas
Normal pH for blood is
7.35 - 7.45
Alkalosis
too much bicarbonate in the blood
a condition in which the body fluids have excess base
pH 7.45 or higher
Acidosis
caused by an overproduction of acid that builds up in the blood, an excessive loss of bicarbonate from the blood, or by a buildup of carbon dioxide in the blood that results from poor lung function or depressed breathing
pH 7.35 or lower
What HC03?
bicarbonate
What is bicarbonate and why is it important?
Bicarbonate is also known as HCO3. It's a byproduct of your body's metabolism. Your blood brings bicarbonate to your lungs, and then it is exhaled as carbon dioxide. Your kidneys also help regulate bicarbonate. Bicarbonate is excreted and reabsorbed by your kidneys.
Hydration and Dehydration process
Cells release CO2, brought to lungs by blood as Bicarb (HC03) and again exhaled as CO2.
Describe the buffering system of the blood.
Buffering system in the blood keeps the balance between Carbonic acid (H2CO3), and Bicarbonate (HCO3-) so the body maintains homeostasis.
Pulmonary Vascular Resistance (PVR)
Resistance against blood flow from 4 pulmonary veins to the LA
Low pressure. It is 1/10 of the systemic vascular resistance (SVR)
PVR Formula is
PVR = (Mean PAP - LAP / CO) x 80
Normal measurement for PVR is
Normal is .25-1.6mmHg.min/L
Pulmonary resistance (and blood flow distribution) is highest in
the capillaries unlike systemic circulation
Normal artery pressure (PAP) is
25/10 mean is 15mmHg.
PVR is influenced by
Pulmonary intravascular pressure
Lung volumes
Gravity (highest in PVR zone 1 from higher alveolar pressure)
Alveolar hypoxia
Smooth muscle tonicity, less smooth muscle
Pulmonary vascular pressure (CO=Cardiac output)
When CO increases, PVR decreases, increasing flow to alveoli, facilitating gas exchange such as in exercise. This happens by capillary distention and recruitment.
Alveolar hypoxia
(sensed by chemoreceptors) induces vasoconstriction, shunting blood to better areas
Smooth Muscle Tonicity; lower vascular tone, less smooth msucle
Increasing PVR: serotonin, epi, norepi, thromboxane A. Pulmonary. Endothelial cells cause vasodilation by producing nitric oxide (NO).
Why is nitric oxide important?
Allows for vasodilation
Gas Exchange
Gases can dissolve and diffuse between the lungs and the circulatory system. Oxygen diffuses into red blood cells. Co2 diffuses into alveolus. This is why we breath.
Pick up oxygen and discharge C02.
Additional Controls: Baroreceptors
Stretch-sensitive baroreceptors are present throughout the vasculature playing a role in BP regulation
Low pressure baroreceptors
cardiopulmonary baroreceptors
Sympathetic stimulation via ____ _____ increases vascular resistance.
Alpha receptors
Parasympathetic _______ ______ vasorelaxation of pulmonary arteries
cholinergic-mediated
Parasympathetic ______ arteries
relaxes, dilates
Hormones involved in pulmonary circulation control
thyroid, serotonin, estrogen, progesterone
Peripheral circulation
Blood vessels provide channels of delivering O2 and nutrients to body tissues
Elastic vessels
large artery, especially aorta, low resistance
Resistance in vessels
Resistance (< 1mm, small arteries and arterioles) ~90% of SVR.
Normal SVR = 700-1500 dynes/sec/cm- 5
SVR = (MAP – RA or CVP/CO) x 80
Major resistance vessels in systemic circulation is
arterioles
Capacitance
large veins that can store and mobilize large amounts and regulate venous return
Vessels can
shunt or clamp down and send blood back to vital organs
Local arteriole is modulated by
ANS (primarily sympathetic) and cause blood vessel constriction and in the heart vasodilation
ANS predominates in ____
skin, splanchnic, and resting skeletal muscles
Increased O2 consumption and release of CO2 results in ________, increased blood flow.
vasodilatation
Vasconstriction
decreases vessel diameter, increasing resistance
Vasodilation
increases vessel diameter – reducing resistance
Microcirculation
Arterioles + Capillaries+ Venules
How does sympathetic nervous system affect systemic blood vessels?
In blood vessels, sympathetic activation constricts arteries and arterioles (resistance vessels), which increases vascular resistance and decreases distal blood flow.