6. Circulatory - Thrombosis, Infarction, and Embolism
1/45
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
46 Terms
______________ is the pathologic counterpart of normal hemostasis and a ________________ is the pathologic counterpart of a blood clot.
- Thrombosis
- Thrombus
Define a thrombus.
- A type of blood clot formed under abnormal conditions. It consists of aggregated platelets, fibrin, and other elements of blood formed on the wall of a vessel.
How could you tell the difference between a clot and a thrombus if you were performing a necropsy on an animal?
- Thrombus occurs in vivo and becomes adhered to the endothelium while clots form postmortem and are not adhered to the vessel wall.
- Thrombi are more friable while postmortem clots are more "rubbery" and "smooth"
- Clots appear as a "chicken fat clot" due to settling of RBCs while thrombi are more consistent and may have a "tail"
What are the three factors which predispose one to a thrombus? Indicate which is likely the most important according to Dr. T.
1) Endothelial injury (Most important)
2) Alterations in blood flow
3) Hypercoagulability
What are some causes of endothelial injury which can predispose one to a thrombus?
- Trauma, vasculitis from infectious agents or immunologic reactions, metabolic disorders (i.e. diabetes mellitus), neoplasia, and toxins
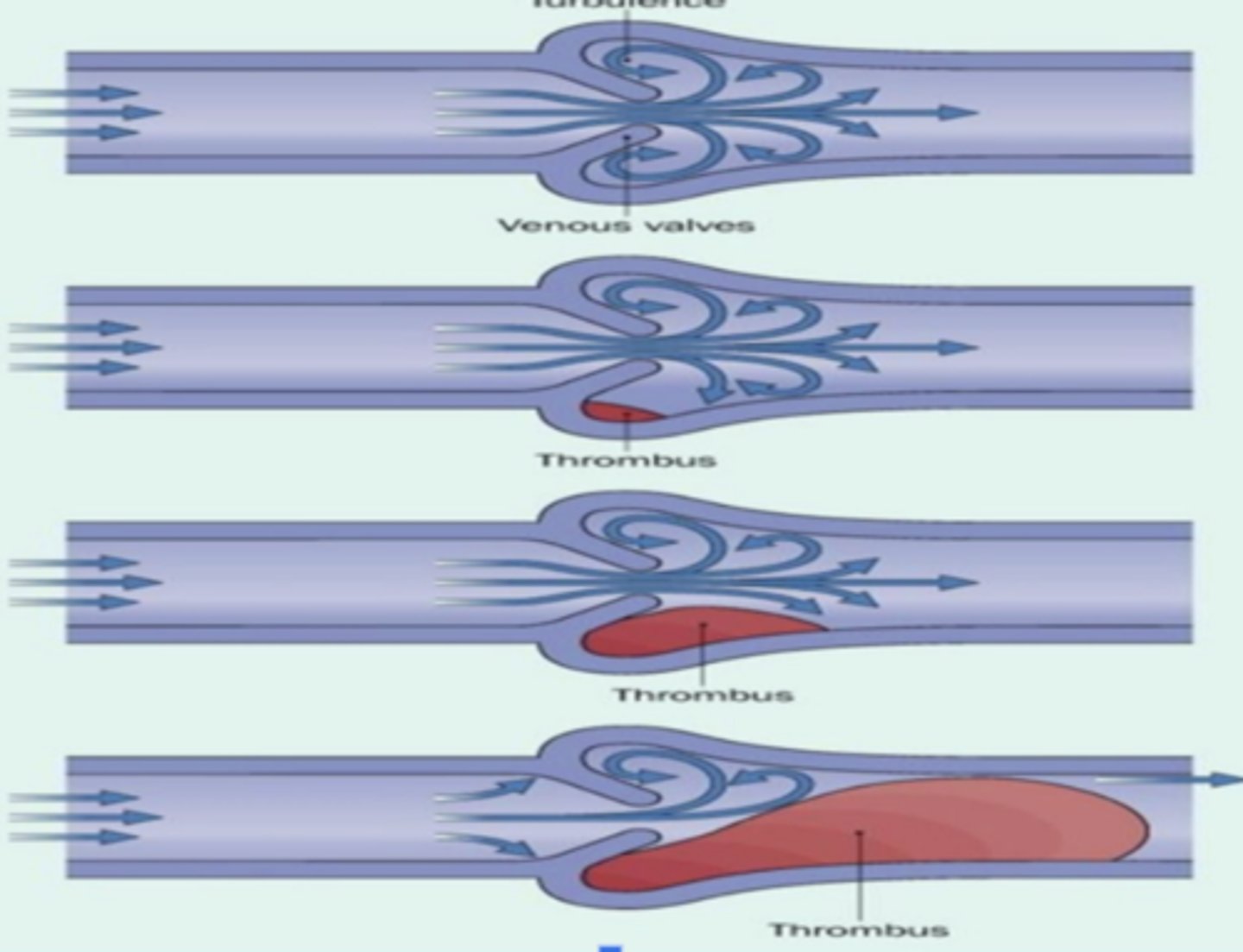
What are some causes of alterations to blood flow which can predispose one to a thrombus?
- Reduced blood flow can happen due to systemic factors like heart failure (less efficient venous drainage and the "pump" is not working as efficiently - stasis) or more locally as in vascular obstruction or dilation.
Reduced blood flow is more commonly seen in veins, arteries, or capillaries?
- Veins
Where does turbulence most often occur?
- Turbulence occurs most often in areas where vessels branch (blood "turning" requires it to slow), where there is narrowing of the vessel lumen or at the site of valves (as in veins or lymphatic vessels)
What two mechanisms can lead to hypercoagulability?
1) Increased coagulation factors: Can occur in conditions such as inflammation, stress, surgery, neoplasia, pregnancy, and renal disease. Inflammation is probably the most common.
2) Increased platelet activity, occurring occasionally in conditions including diabetes mellitus, nephrotic syndrome, neoplasia, heartworm disease and uremia.
Thrombi can lead to significant problems by which two mechanisms?
1) A thrombus can obstruct blood flow to the local tissue, leading to ischemic injury
2) A thrombus can break off, float to a different site and cause problems there also, a process called embolism.
Different sites are associated with some differences in how thrombi form. Explain how "white" arterial thrombi form.
- These form under high blood flow rate conditions, so they usually don’t occlude the vessel right away, though many of them grow and eventually become occlusive. Because the rapidly flowing blood sweeps away many of the blood elements (e.g. the RBCs) arterial thrombi usually contain mostly platelets and fibrin so they are white or gray and friable. As they sit in a vessel and propagate, they may accumulate RBCs over time and thus appear to have a white/gray “head”, attached to the endothelial wall, and a red, floating “tail” downstream.
What is equine verminous arteritis? How do patients with this condition present?
- Thrombus in the cranial mesenteric artery
- Colicky
Different sites are associated with some differences in how thrombi form. Explain how venous thrombi form.
- Blood flow is much slower in veins, so thrombi that occur there tend to accumulate all the elements of a normal blood clot and will, in fact, often look like the blood clot that forms when you draw blood into a red-top tube. They also tend to be occlusive, but not very well attached to vessel walls.
What types of thrombi are more difficult to distinguish from post-mortem clots during necropsy?
- Venous thrombi
What is an important clinical conseqeunce of venous thrombi not being strongly adhered to the vessel wall?
- Can lead to embolism
The clinical significant of a thrombus depends on several factors including what?
- Size (small thrombi are more easily dsisolved)
- Location
- Rate of formation (slowly developing thrombi allow for collateral blood flow to develop)
- Amount of collateral circulation to the tissue supplied by the thrombosed vessel
If a thrombus doesn't cause fatal organ hypoxia at the onset, what are the four possible fates of a thrombus?
1) Propagation
2) Embolization
3) Dissolution or thrombolysis
4) Organization
Explain "propagation" as a fate of thrombi.
- The thrombus can continue to enlarge progressively, usually in the direction of the heart.
Explain "embolization" as a fate of thrombi.
- A piece of the thrombus can break off and move downstream until it reaches a vessel of smaller size where it will occlude the vessel.
Explain how dissolution of a thrombus occurs.
- Plasmin is the primary enzyme responsible for breaking down fibrin in clots or thrombi, as well as fibrin which may be formed during the healing process.
When is fibrinolytic removal of thrombi most successful?
- The most successful fibrinolytic removal of thromboses usually occurs within the first several days of thrombus development, before the thrombus becomes more resistant to fibrinolysis. There are a number of steps to the degradation of fibrin, and they result in different-sized fragments which are collectively called fibrin degradation products (FDP’s). Cross-linked fibrin polymers are broken down into d-dimers by plasmin.
What are FDPs and D-Dimers? Which is more representative of fibrinolysis and why?
- They are both breakdown products of fibrinolysis (breakdown of fibrin clots).
- D-dimers are more representative of increased fibrinolysis because they indicate the activity of both thrombin and plasmin and are specific for fibrinolysis.
What are increased levels of FDPs and D-dimers consistent with?
- With disseminated intravascular coagulation (DIC) with the assay for D-Dimers being the more sensitive and specific test
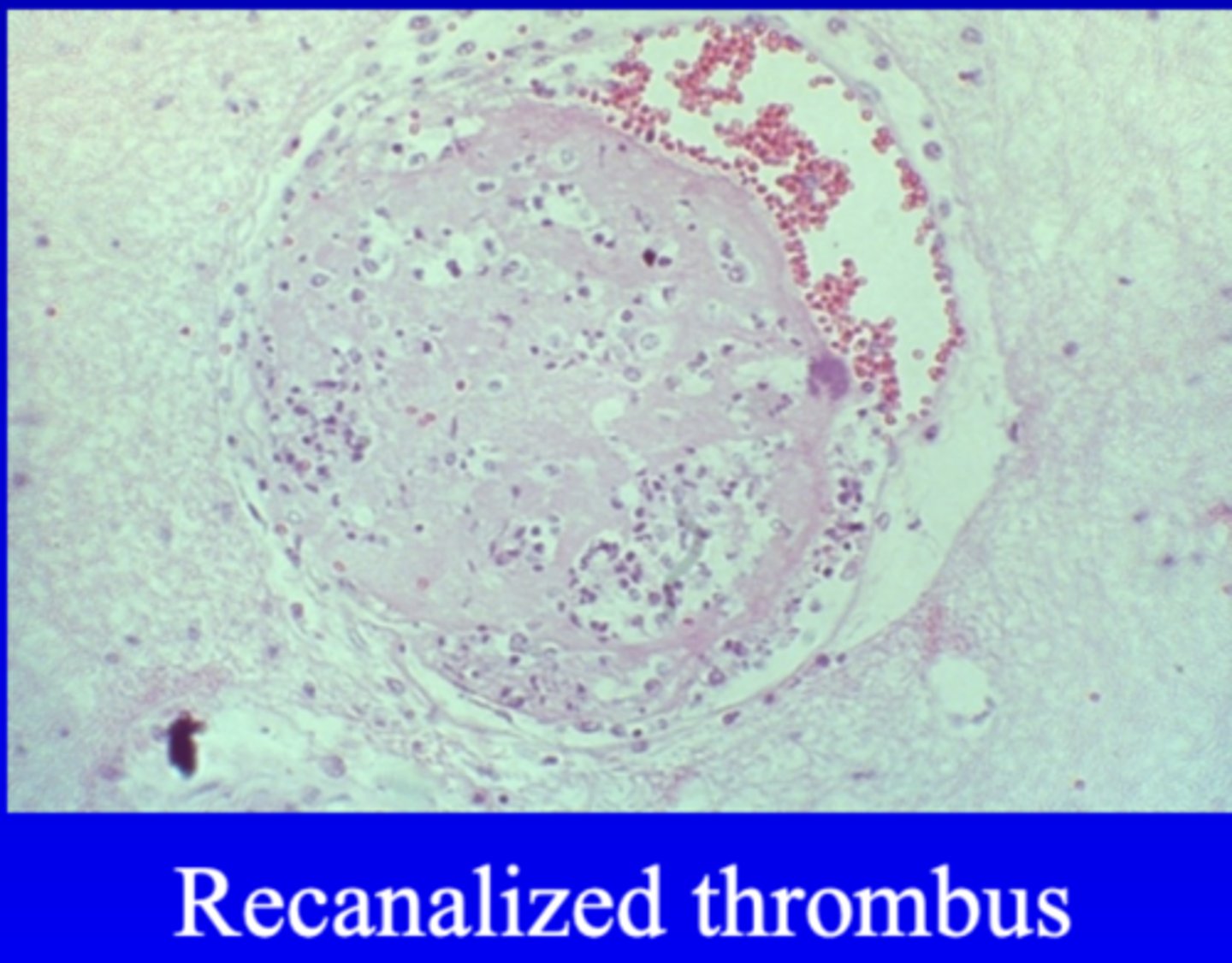
What does organization of a thrombus result in?
- Results in the thrombus being reduced in size and eventually becoming a thickened, fibrous part of the vessel wall
How does organization of a thrombus occur?
- Organization occurs by granulation tissue, endothelial cells, and macrophages invading the thrombus and breaking down fibrin and cells while building up fibrous connective tissue. Capillaries which form in the thrombus often coalesce to create a new opening for blood flow through the thrombus, a process called recanalization.
In what case can an old thrombus be found at necropsy as an incidental finding?
- If the thrombus undergoes organization and the process of recanalization is successful
Generally, explain DIC (disseminated intravascular coagulation).
- DIC is the formation of numerous small fibrin thrombi in vessels all over the body. While they can cause some ischemia of tissues, the larger problem is the activation of the hemostatic system and the simultaneous activation of the fibrinolytic system, using up platelets and ciagulation factors. This can lead to bleeding disorders as normal coagulation can no longer occur.
What are typical laboratory findings associated with DIC?
- Thrombocytopenia
- Increased levels of D-dimers
- Prolonged coagulation times
What are potential catastrophic results of DIC?
- Widespread hemorrhage
- Widespread thromboses
- Multiple organ failure secondary to ischemia
What are some treatment options for DIC?
- Complicated: Treat the underlying cause first (usually the result of a systemic inflammatory disorder)
- Heparin (Stop the formation of thrombi)
- Fluid therapy
What is an infarct?
- A focal area of ischemic necrosis in a tissue or an organ
Generally, what are causes of an infarct?
- Nearly all infarcts are caused by occlusion of vessels by thromboses or emboli (arterial obstruction is most common cause)
In general, which tissues can least tolerate ischemia without total loss of function (i.e. are most susceptible to tissue damage secondary to an infarct)?
- The heart and the brain
What types of tissues are least susceptible to infarction? What is an exception to this rule?
- Tissues that have dual blood supplies (lung, liver, intestines)
- Colonic infarction in horses due to embolism in the cranial mesenteric artery (even though there is dual blood supply to the intestines, it almost entirely stems from one common artery).
What are the two general types of infarcts?
1) White or anemic infarcts
2) Red or hemorrhagic infarcts
Where do white or anemic infarcts occur? How long does it take for the appearance of the organ to change?
- Occur with arterial occlusion in solid organs (i.e. kidney and heart)
- The pale appearance of the organ due to the infarct occurs within 24 to 48 hours as any blood cells which seeped out into the tissue are lysed and the hemoglobin is broken down.

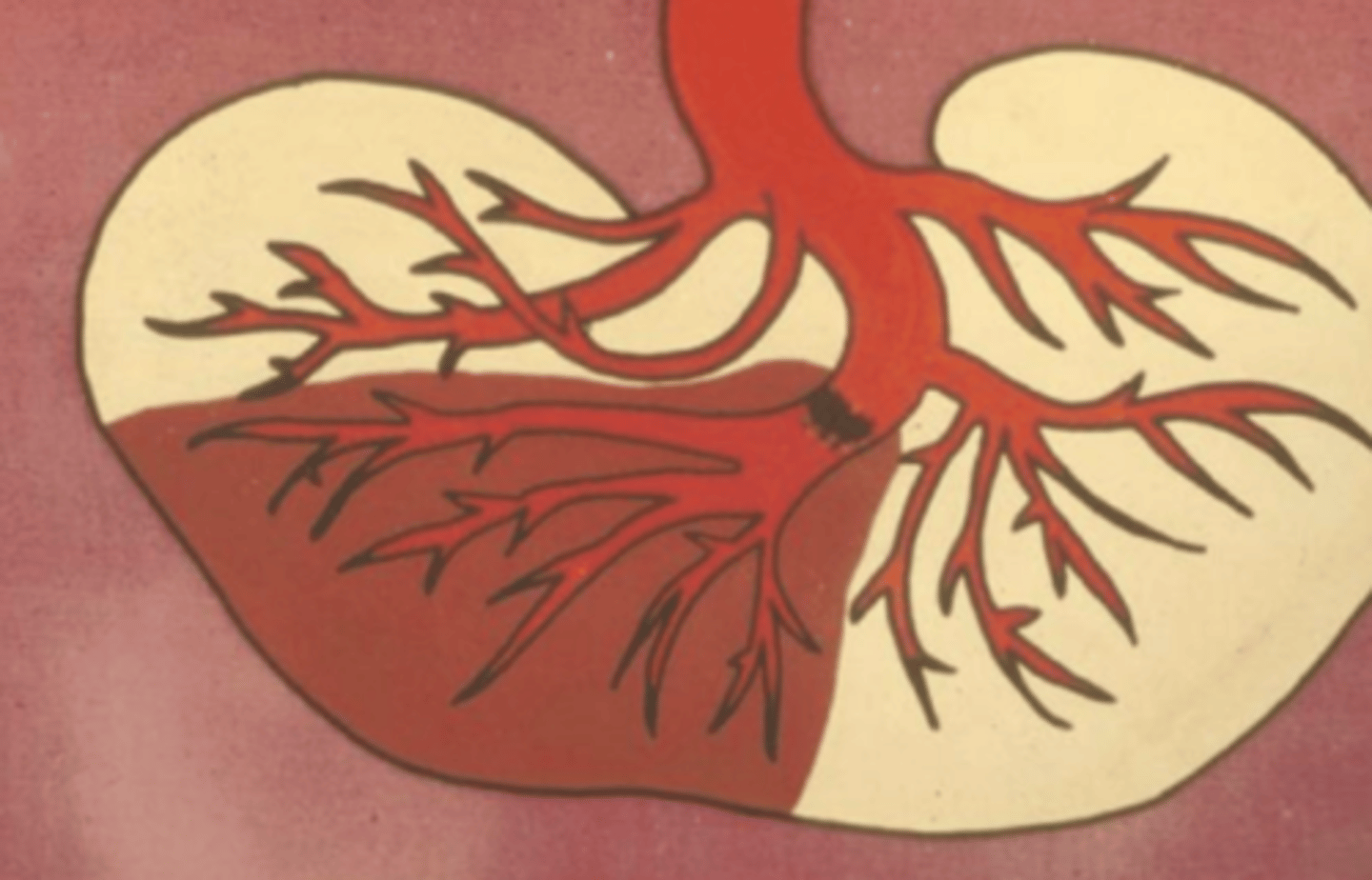
Where do red or hemorrhagic infarcts occur? Why do these infarcts appear hemorrhagic?
- These occur with venous occlusion, in loose tissues such as the spleen and lung, and in tissues which have double circulation (i.e. lung (see image) and intestine)
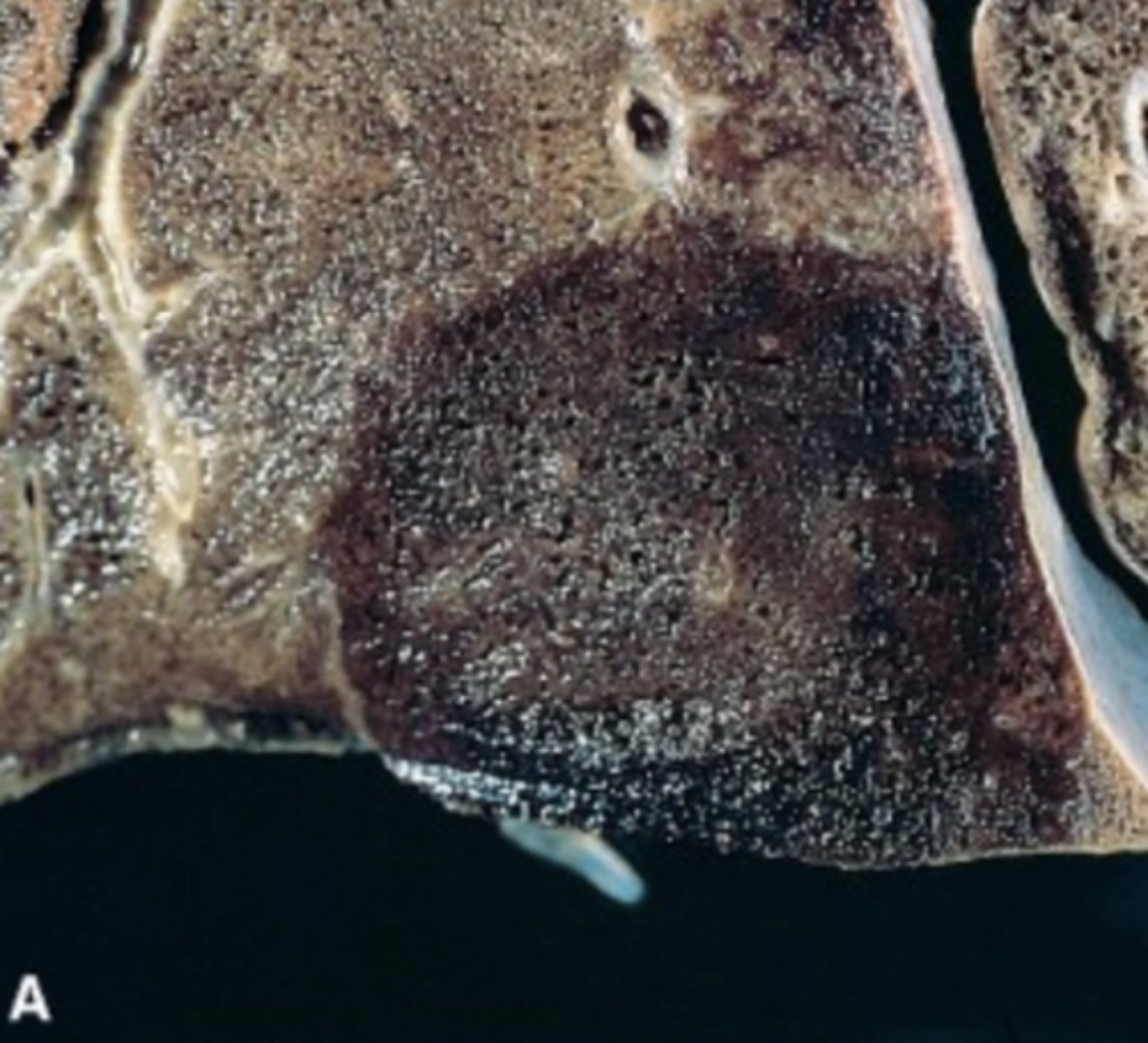
Describe the typical appearance of infarcts, including color, shape, margins.
- Infarcts usually appear dark red right after they occur. Most infarcted areas are wedge-shaped, with the apex pointed towards the occluded vessel. Grossly, the margins become fairly well-defined within 24 hours; white infarcts typically go on to become very well-demarcated and paler over the next several days.
Cells in infarcted areas undergo what? Over time, they may be replaced by what?
- Ischemic coagulative necrosis
- Replaced with scar tissue
There is usually some ____________ or ___________ at the margin of infarcts.
- Hyperemia
- Inflammation
If bacteria are present, infarcts may be ______________. Alternatively, they can be _______________.
- Septic
- Bland
What is an embolus?
- A detached intravascular mass carried by the blood from its site of origin to a distant site; a process called embolism
What are the types of emboli and which is most common?
- The most common type arises from a thrombus
- Fat
- Bone marrow
- Neoplastic cells
- Clumps of bacteria or fungi
- Parasites
- Amniotic fluid
- Catheters
What is the most common fate of emboli? How does this relate to the word thromboembolism?
- Emboli usually end up lodging in small vessels where they totally or partially occlude the vessel. At this point, many emboli attach to the vessel, become thrombi and go on to do the things that thrombi do (e.g. propagate, dissolve, organize, etc).
- The term thromboembolism is used to describe these entities which have uncertain origins as thrombi or emboli.
What are common examples of how emboli can develop in animal patients?
- Left atrial thrombi which arise in cats with hypertrophic cardiomyopathy often embolize to the iliac bifurcation and extend into both right and left branches and are called saddle emboli.
- Another example is liver abscesses (initiated by hardware disease) in cattle that erode through the vena cava and release septic emboli into the circulation, often ending up in the lungs.
What would be physical exam findings in a cat with a saddle thrombus?
- Cold hind limbs
- Paraparesis to paraplegia of the hindlimbs
- Yowling
- Weak to absent femoral pulses