Comprehensive Study on Fat Soluble Vitamins: Deficiencies, Toxicities, and Populations at Risk
1/75
Earn XP
Description and Tags
Caleb Halleran
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
76 Terms
Retinol, Retinal, Retinoic acid = Vitamin ____
Vitamin A (Preform)
Beta-carotene & Alph-carotene = Vitamin ____
Vitamin A (Proform)
Calciferol = Vitamin ____
Vitamin D
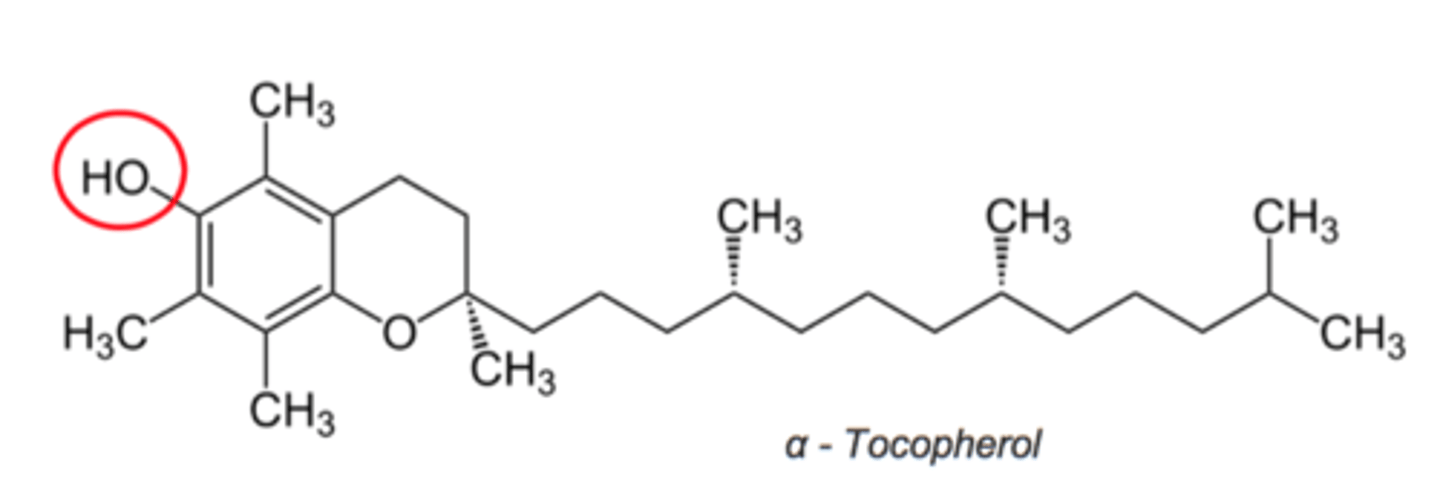
Alpha-Tocopherol = Vitamin ____
Vitamin E; alpha-tocopherol is the only structure recognized to meet human requirements
Tocotrienol = Vitamin ____
Vitamin E
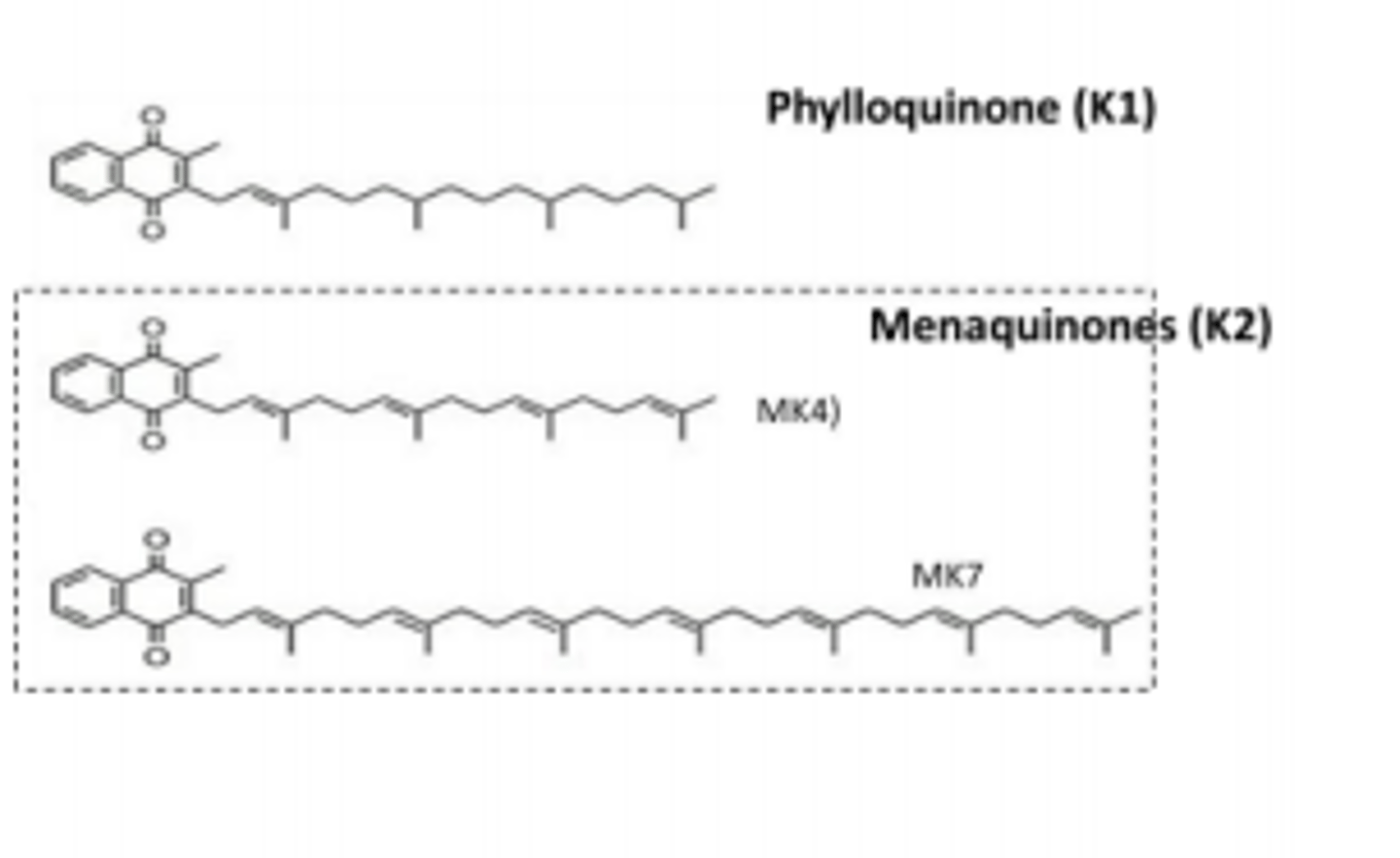
Phylloquinone = Vitamin ____
Vitamin K - plant
Menaquinone = Vitamin ____
Vitamin K - animal & LI
(T/F): Vitamins are organic compounds that are essential and provide us energy.
False; Vitamins do not provide us energy! They are required for normal physiologic function (biochemical reactions)
(T/F): All fat soluble vitamins are absorbed via passive diffusion.
True
(T/F): Men are at a higher risk of reaching toxic levels of Vit. K, A, E, and D than women.
False; women have more adipose tissue than men making women more at risk of storing too much fat soluble vitamins

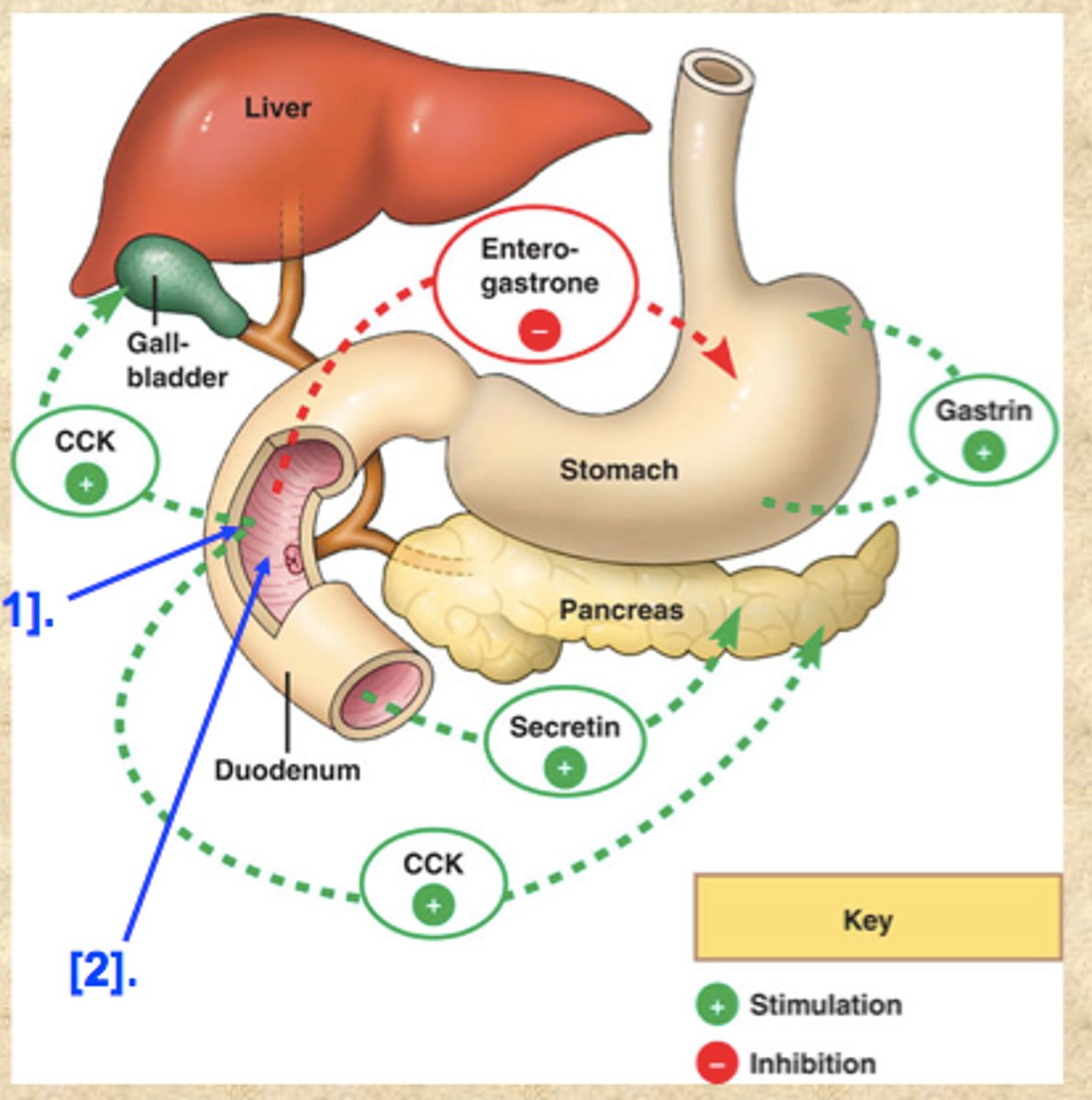
To best absorb fat soluble vitamins ____g of fat must be consumed to trigger ___________ to be released which helps with absorption.
5-10g of fat
CCK - Cholecystokinin causes the gallbladder to contract & stimulates pancreatic enzyme secretion
Forms of Vitamin A
1. Preformed - Retinol, Retinal, Retinoic acid
2. Proformed - Carotenoids
Active form of Vitamin A =
In-active form of Vitamin A =
Active = Performed Vit. A - Animal products (absorb 75-100%)
Passive = Proformed Vit. A - Plant products (absorb 3-90%)
(Functions) Preformed Vitamin A
1) Reproduction & Growth (Retinol)
2) Vision (Retinal)
3) Gene expression (Retinoic acid)
3a) Retinoic acid receptors (RAR) or Retinoic X receptors (RXR)*
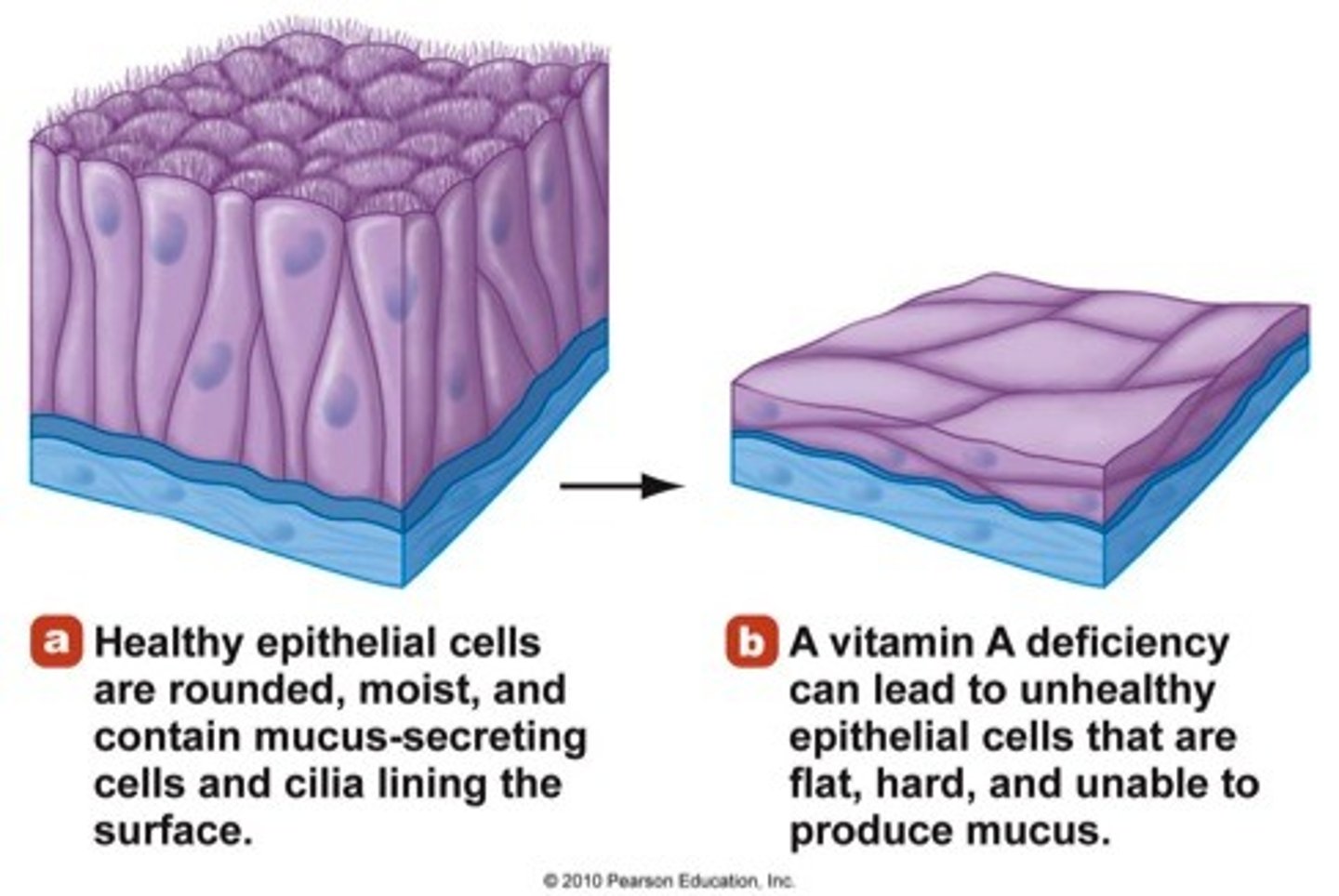
4) Mucus production (Retinoic acid)
4a) Hyperkeratinization (Keratinizing cells --> Mucus-secreting cells)
5) Immune cell fxn / Inflammation (Retinoic acid)
NISS - Nuclear-initiated steroid signaling (genes contain retinoic acid receptors)
MISS - Membrane-initiated steroid signaling (JAK/STAT)
(Deficiency Name) Preformed Vitamin A
Hypovitaminosis A
Most common cause for Hypovitaminosis A in U.S.:
Primary = Indecent intake (world wide)
Secondary = Fatty malabsorption
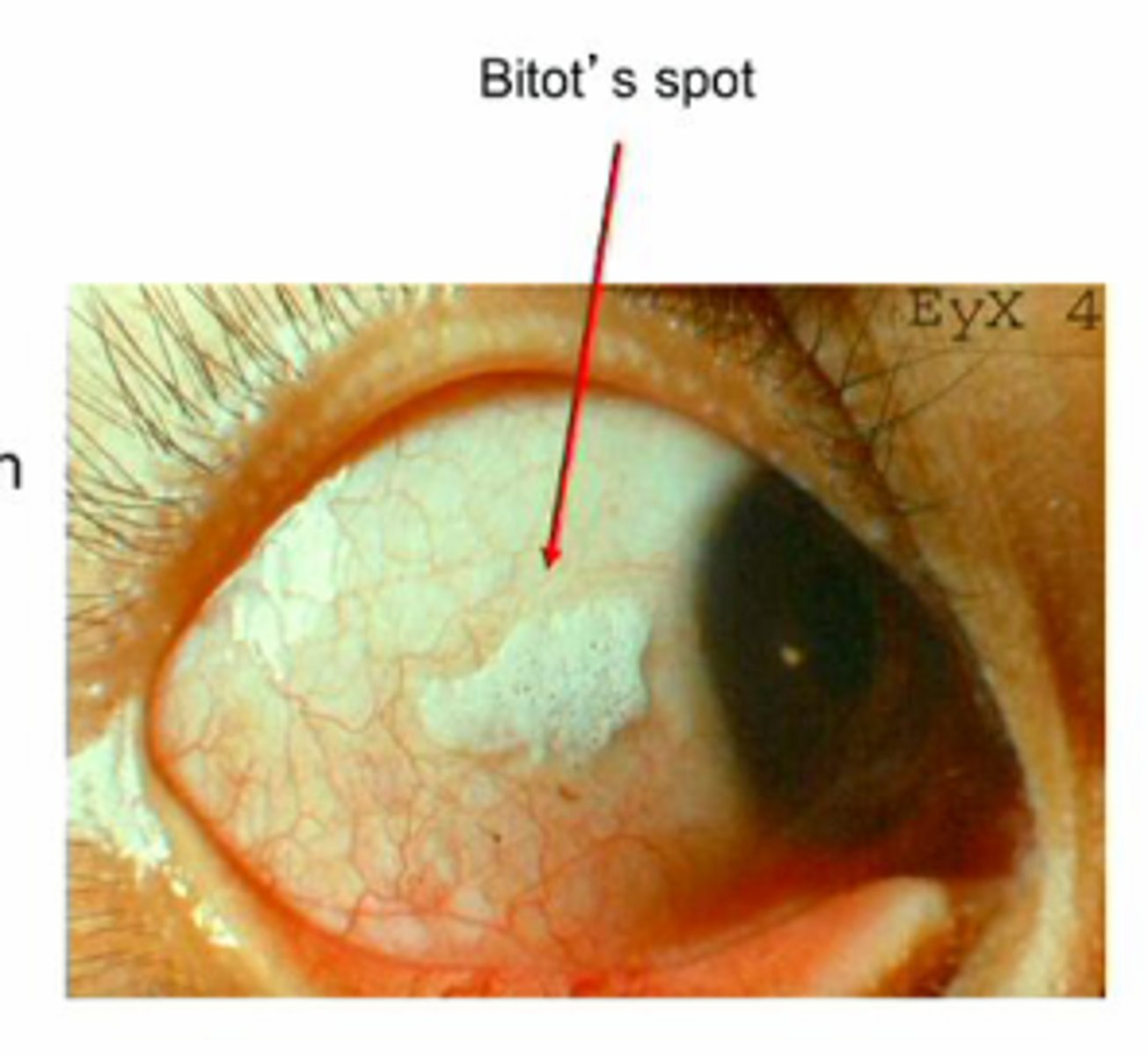
(Deficiency Symptoms) Preformed Vitamin A
1) Xerophthalmia (dry eye from inadequate mucus production)
2) Bitot's Spots (leading cause of preventable blindness in children)
3) Night Blindness (nyctalopia)
4) Xerosis (itching, burning of eyelid)
5) Decreased immune system (increased risk for infections)
6) Follicular hyperkeratosis (replace mucus-secreting cells in respiratory, gastrointestinal & urinary tracts with keratinizing cells)
(Toxicity Name) Preformed Vitamin A
Hypervitaminosis A
(Toxicity Symptoms) Preformed Vitamin A
1) Bone fracture
2) Liver damage
3) Blurred vision
4) Teratogenic

(Sources) Preformed Vitamin A
Animal products
1. Liver - close to toxic levels though
2. Dairy products
3. Fatty fish
4. Eggs

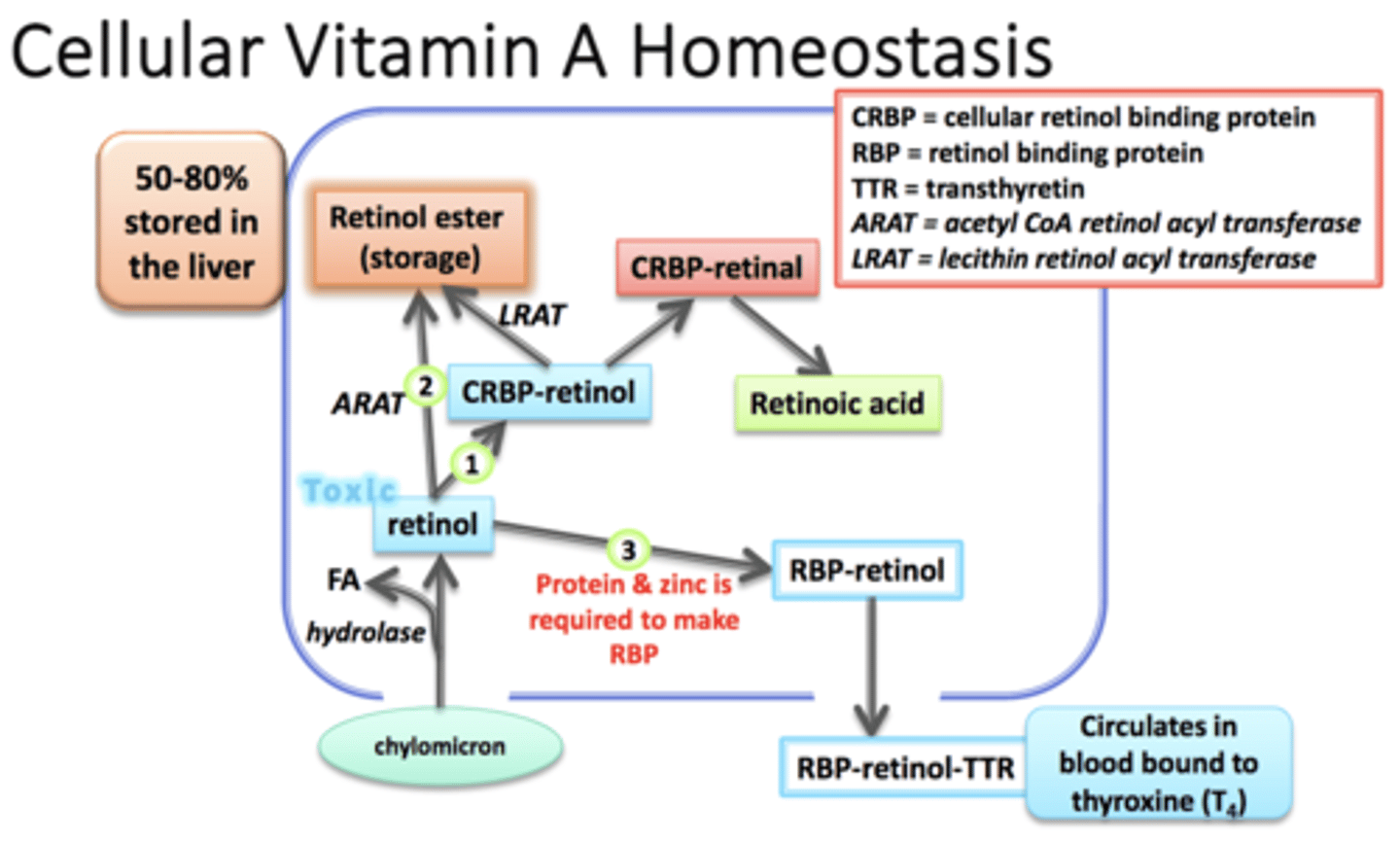
Pathway for Vitamin A storage =
1) Chylomicron brings Retinol into cell
2) Hydrolase removes FA from Retinol (free Retinol = toxic)
3) CRBP binds to Retinol (no longer toxic)
4) CRBP breaks off an LRAT adds FA making Retinol Ester
50-80% stored in the liver (stellate cells)
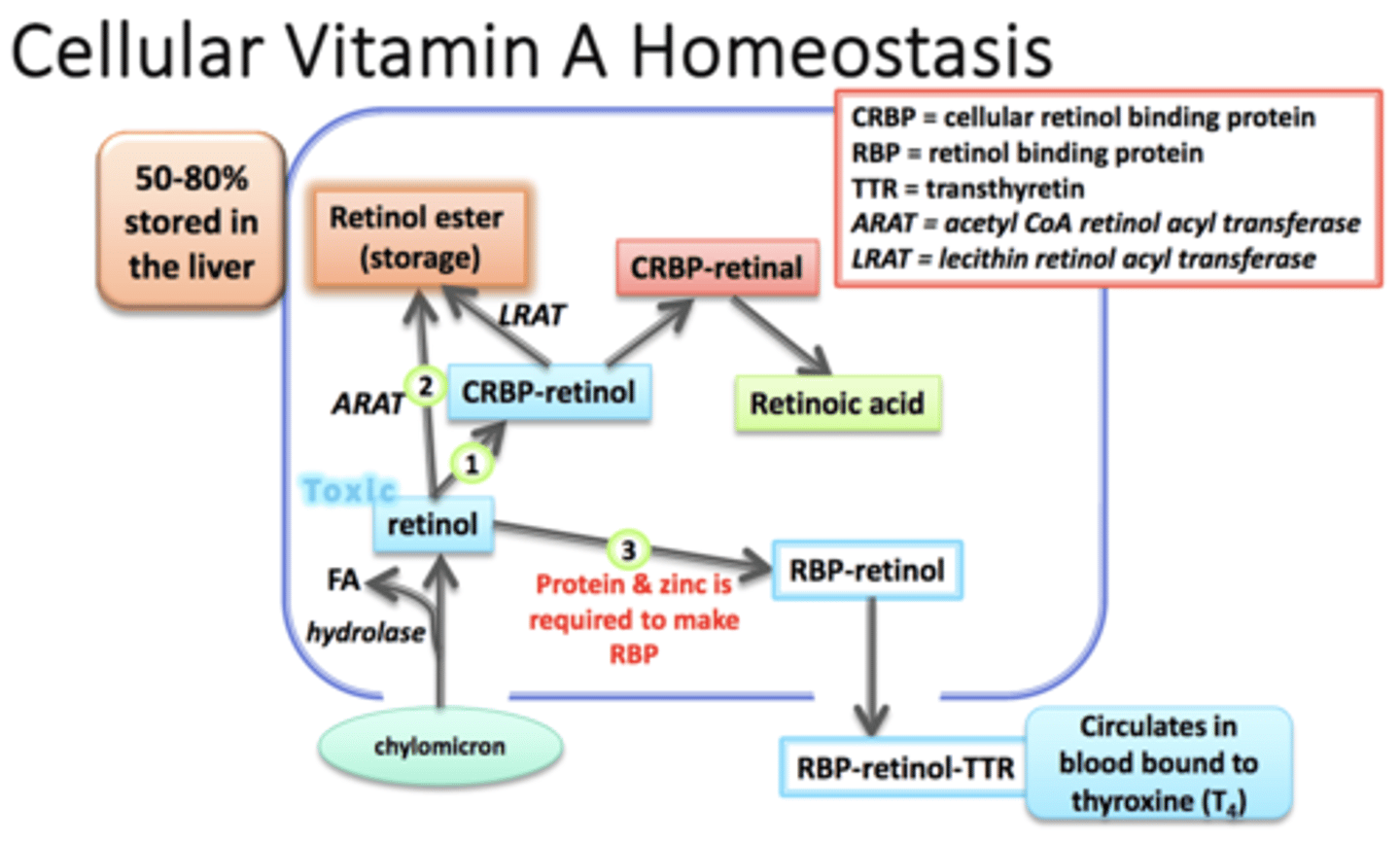
Pathway to use Vitamin A =
1) Chylomicron brings Retinol into cell
2) Hydrolase removes FA from Retinol (free Retinol = toxic)
3) CRBP binds to Retinol (no longer toxic)
4) CRBP-retinol --> CRBP-retinal ---> CRABP-Retinoid Acid
CRABP-Retinoid Acid travels to nucleus to alter gene expression
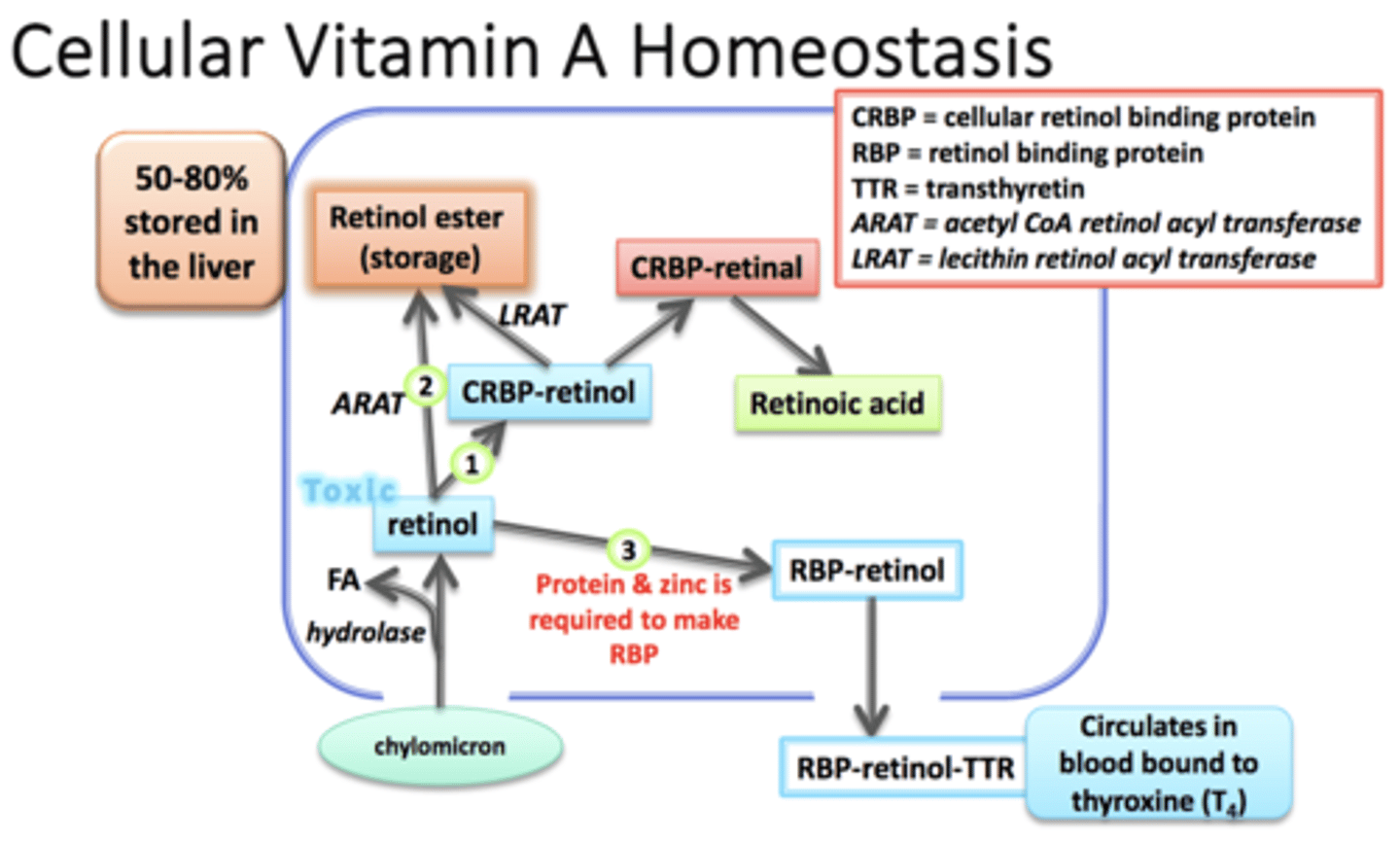
Pathway to mobilize Vitamin A =
1) Chylomicron brings Retinol into cell
2) Hydrolase removes FA from Retinol (free Retinol = toxic)
3) RBP-retinol + Protein + Zinc
binds to Thyroxine (RBP-retinol-TTR) and circulates blood
(Functions) Proformed Vitamin A
1) Antioxidant
2) Cell growth & differentiation
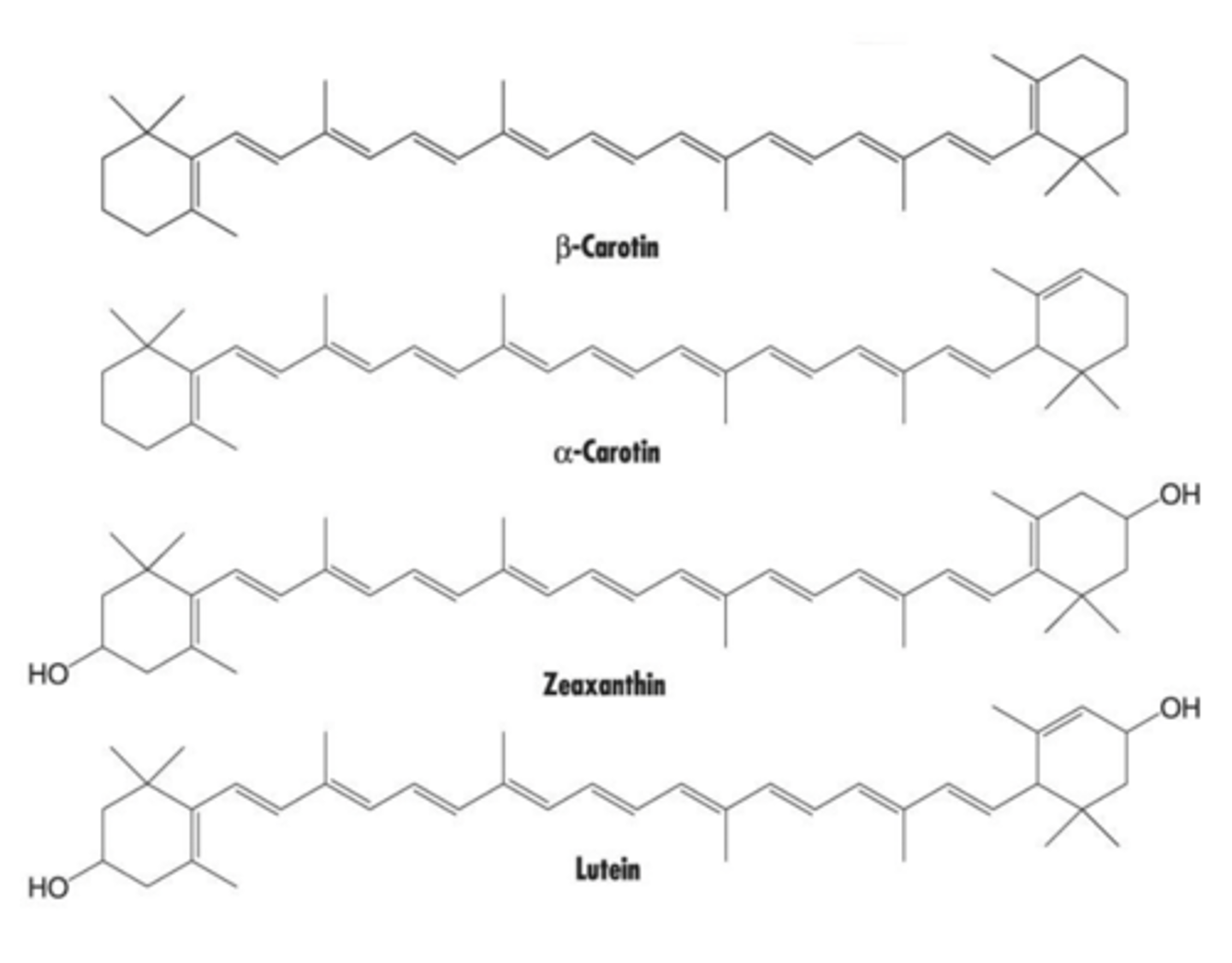
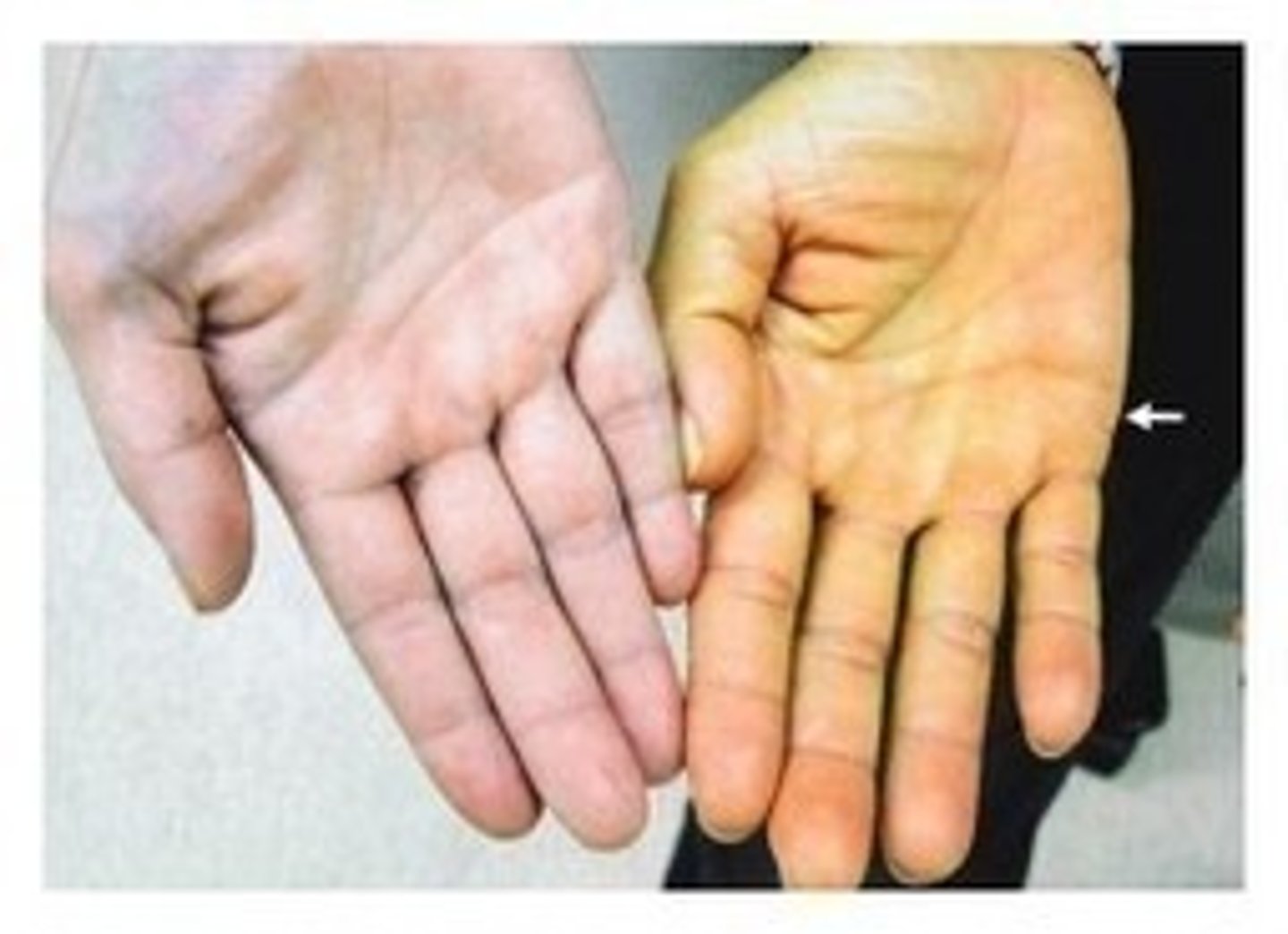
(Toxicity Symptoms) Proformed Vitamin A
NONE from dietary carotenoids; chronic consumption can lead to yellow/orange skin (hypercarotenosis)
Higher does supplements may increase cancer risk
(Sources) Proformed Vitamin A
Red, orange, yellow plants
1) Dark leafy veggies
2) Carrots
3) Pumpkin
4) Spinach

What population(s) are at risk for Vitamin A deficiency?
1) Chron's Disease (Fatty malabsorption)
2) Cystic Fibrosis (Fatty malabsorption)
3) Premature infants / Infants & young children
4) Pregnant & lactating women
It takes ____ times as much Proformed to equal Preformed activity. (Vitamin A)
12
Excessive dietary vitamin A decreases vitamin ______ absorption.
vitamin k
Vitamin A (RA) is required for _______ absorption, transportation and utilization.
iron absorption, transportation and utilization.
Vitamin A deficiency can manifest as iron deficiency anemia
Low ____________ and/or _________ prevents Vitamin A from mobilizing from the liver.
low protein and/or zinc
Where is Vitamin A stored?
50-80% stored in the liver (stellate cells)
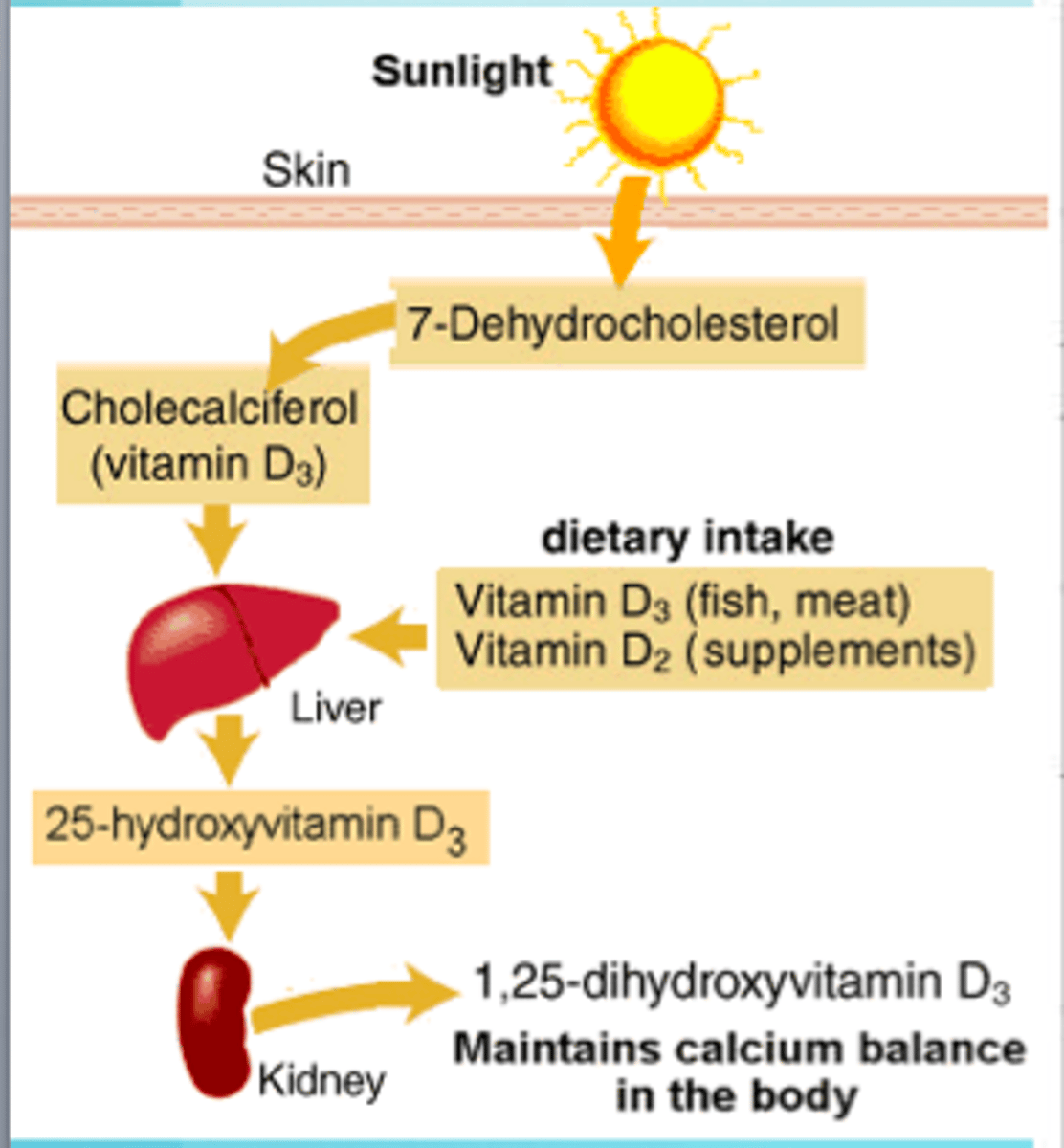
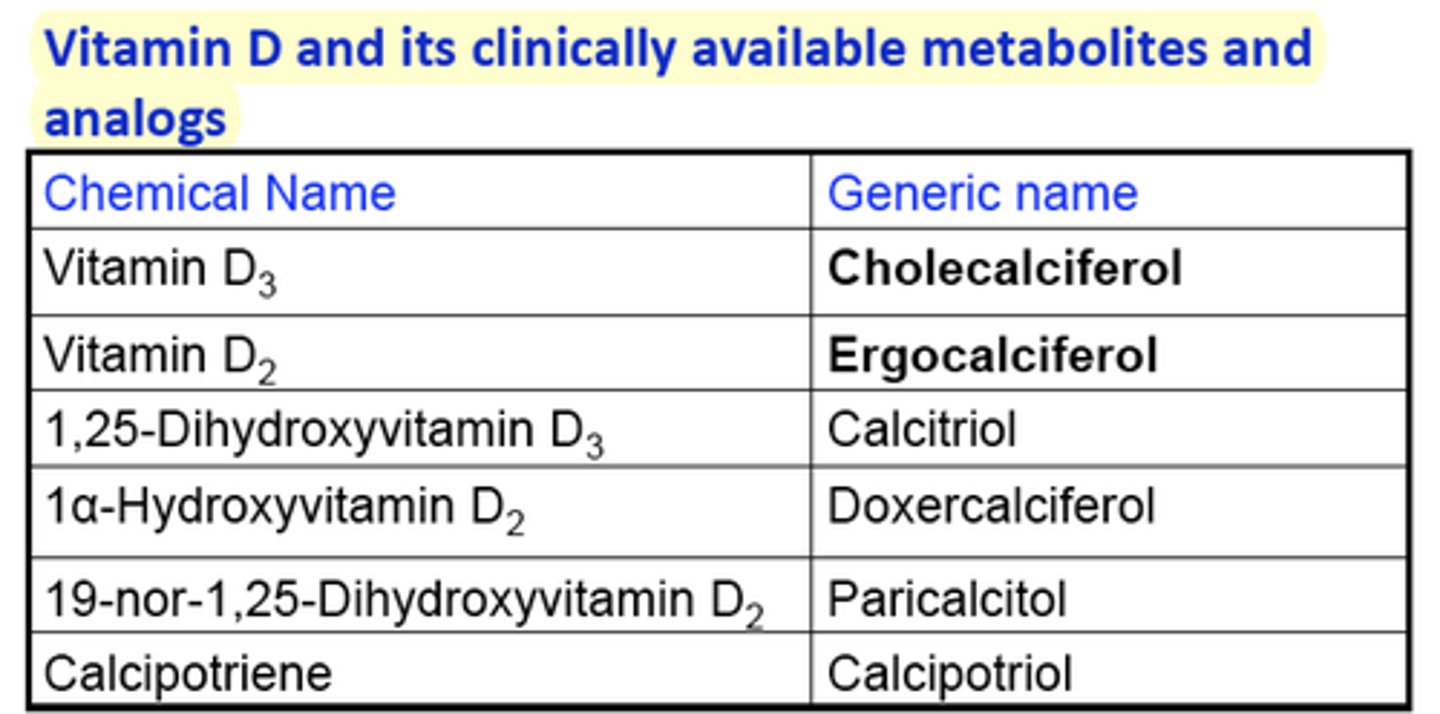
Forms of Vitamin D
1) Colecalciferol (D3) - Animals & Synthesis
2) Ergocalciferol (D2) - Plant
(Functions) Vitamin D
1) Homeostasis of Calcium and Phosphorus; acts like a steroid hormone and affects gene expression
2) Gene expression; vitamin D receptor on genes
3) Cell signaling - MISS
4) Cell growth, differentiation and proliferation (WBCs, stem cells)
5) Muscle function (Type II muscle)
6) Immune system (all immune cells contain vitamin D receptors)
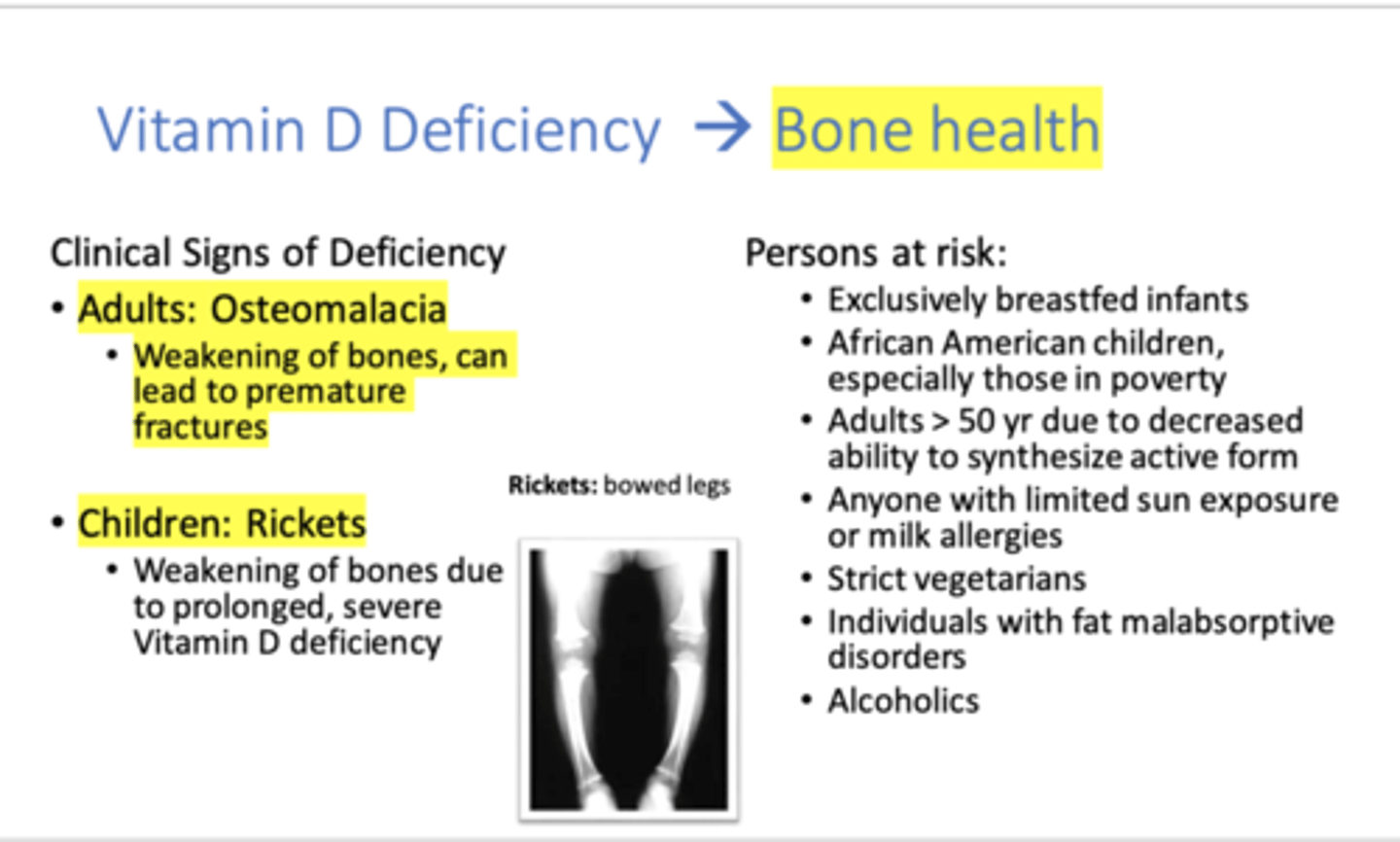
(Deficiency Name) Vitamin D
Children = Rickets
Adults = Osteomalacia
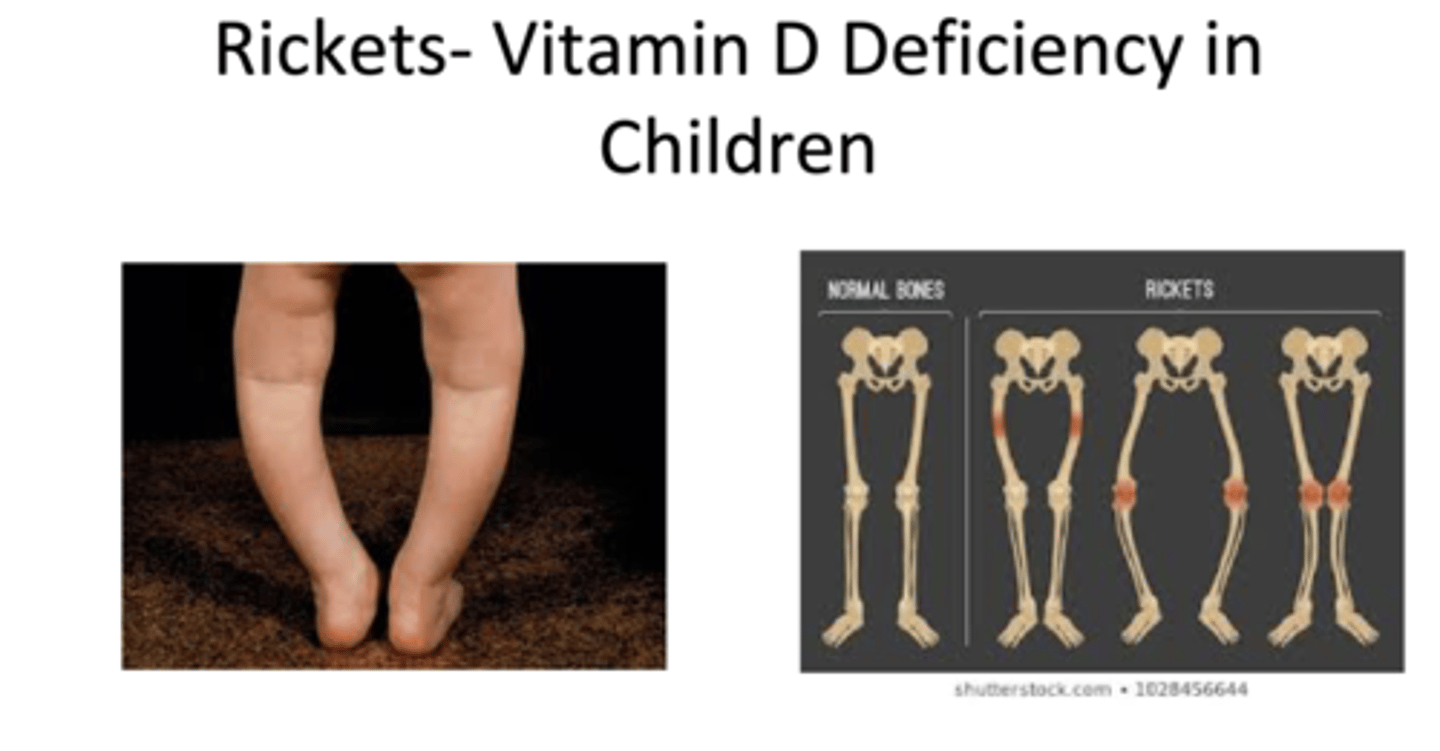
(Deficiency Symptoms) Vitamin D
Softening and weakening of bones
Rickets = Bowed legs, bilateral knee pain
Osteomalacia = Muscle weakness, bone pain
(Toxicity limit) Vitamin D
Tolerable upper limit 4,000 IU/day; issues arise with daily does of 10,000 IU or more for more than 6 months
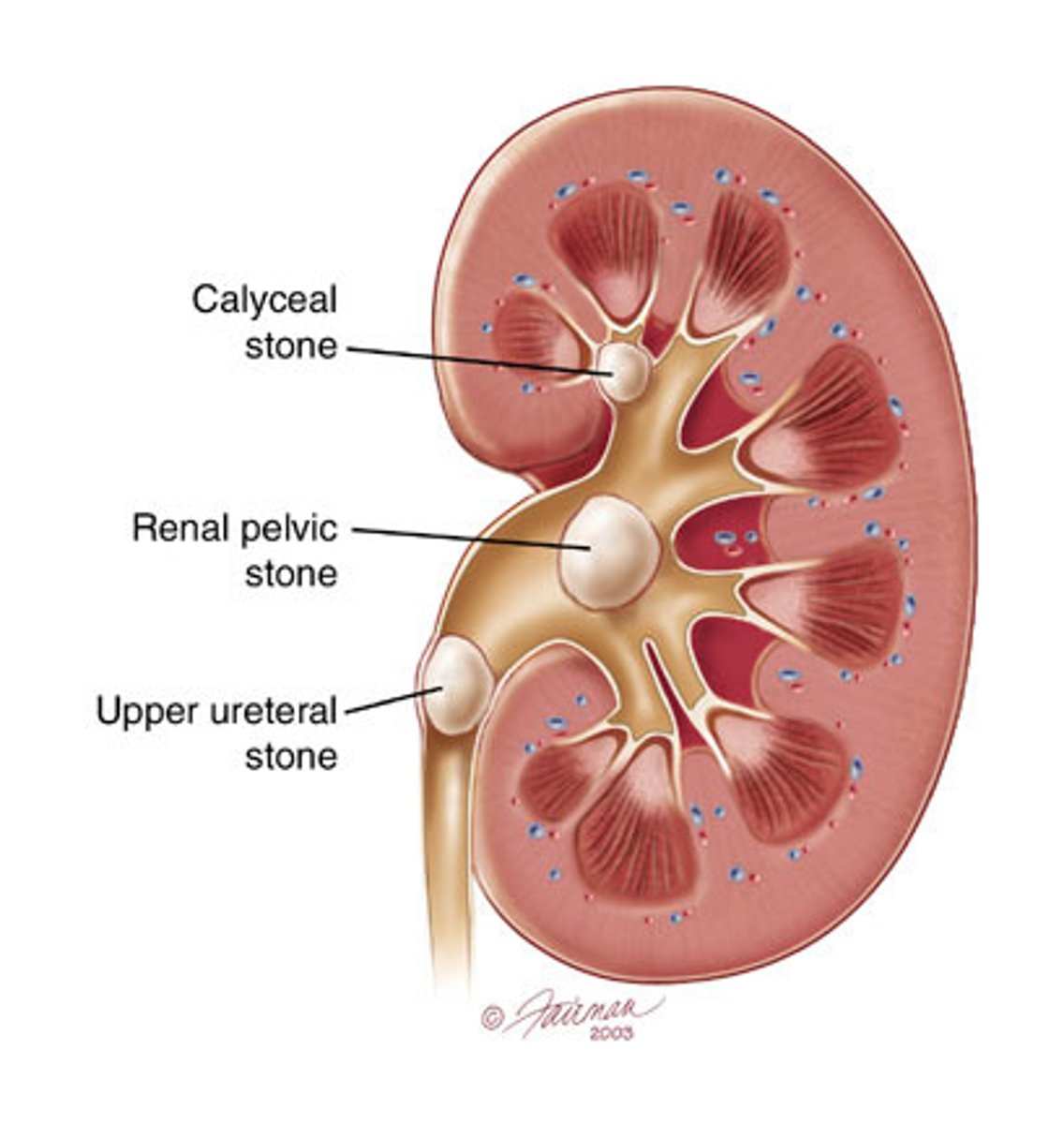
(Toxicity Symptoms) Vitamin D
Hypercalcemia and Hyperphosphatemia --> Kidney stones (calcification of soft tissues, kidney, lungs, heart, etc)
(Sources) Colecalciferol Vitamin D
Animal products
1) Sunlight
2) Fish
3) Cow's milk
(Sources) Ergocalciferol Vitamin D
Plants
1) Mushrooms

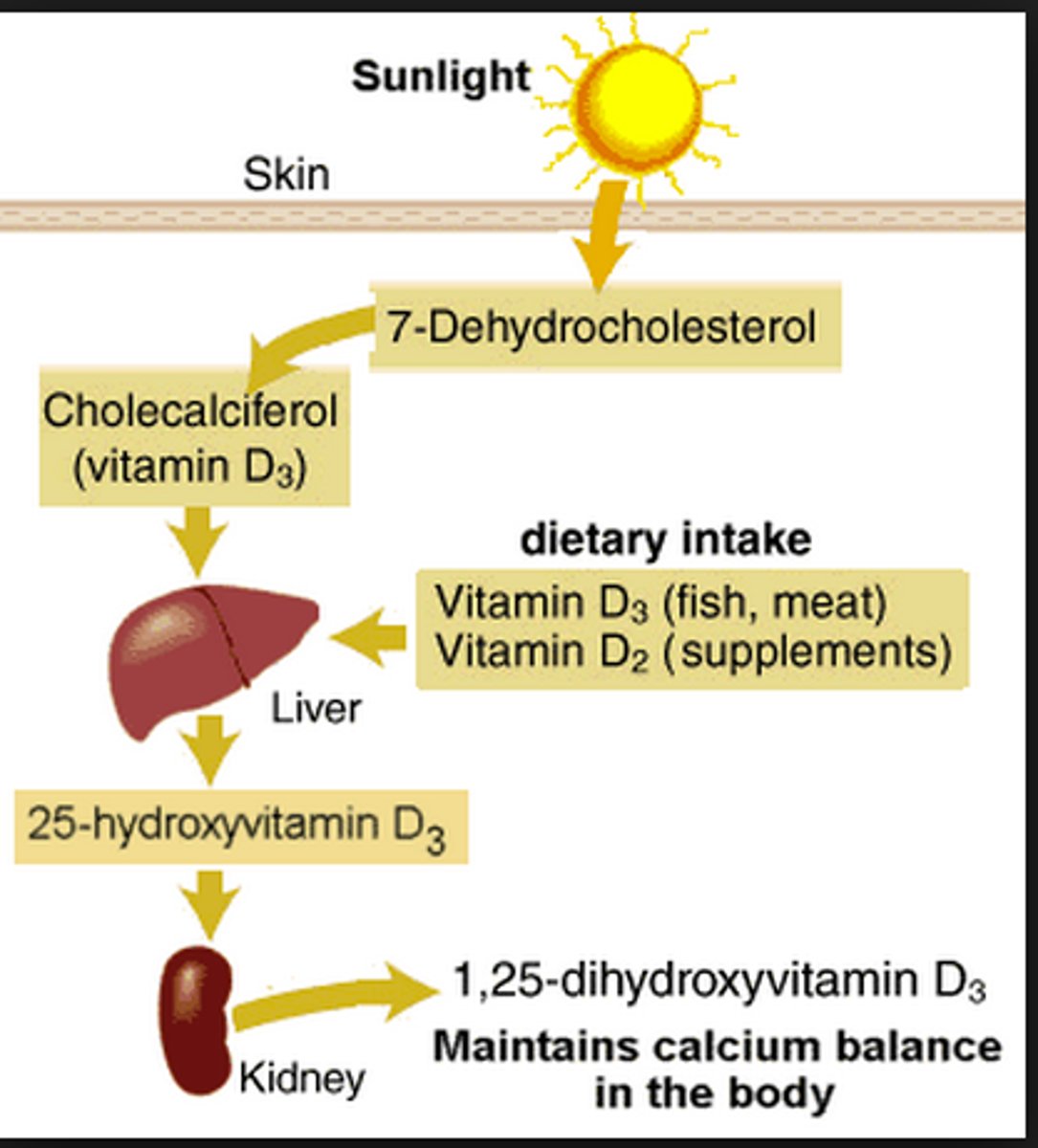
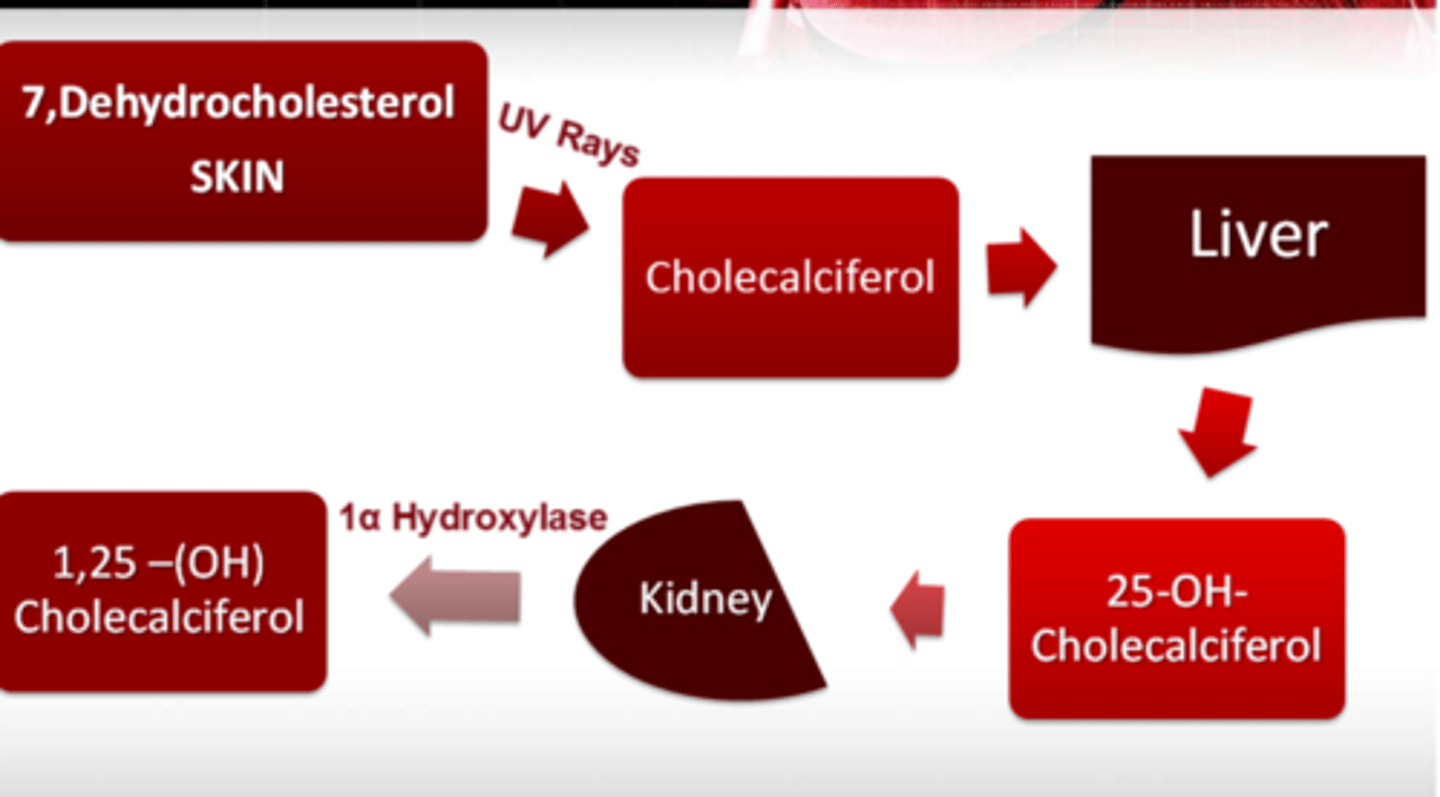
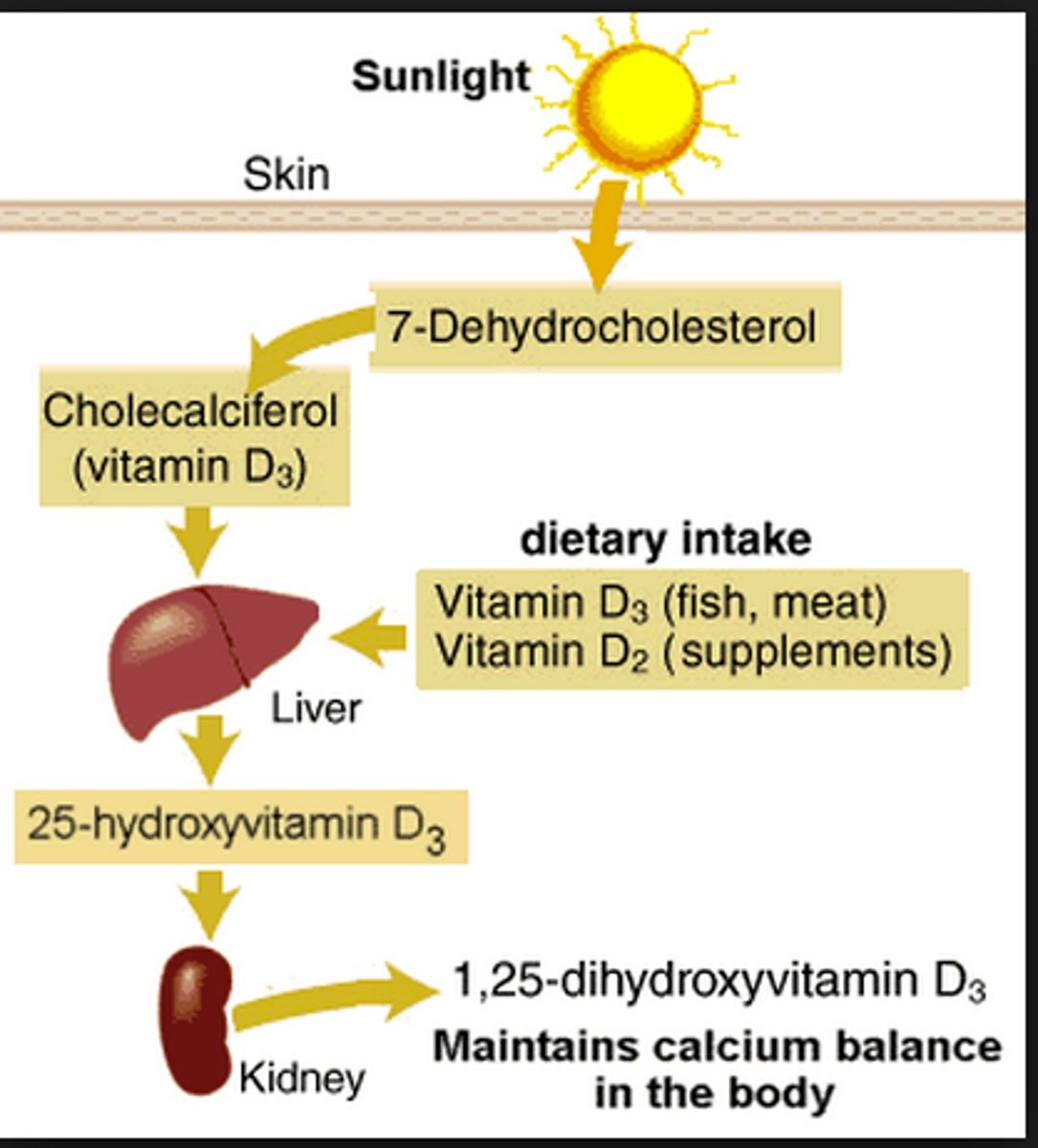
Type of vitamin D we can synthesis in the skin =
Type of vitamin D we eat in food =
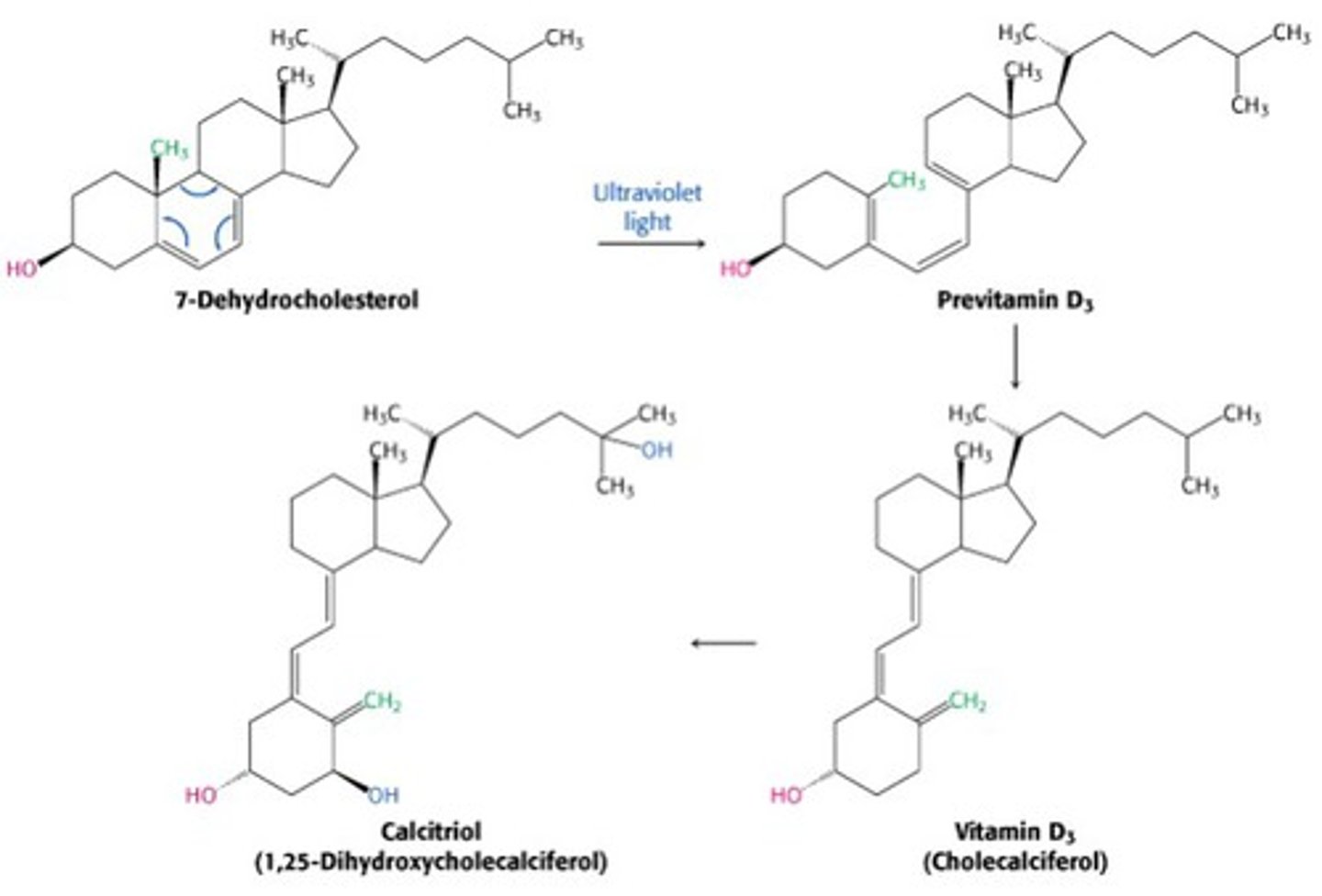
7-dehydrocholesterol --(UVB)--> previtamin D --> Calciferol
Eat = Colecalciferol (animal) or Ergocalciferol (plant)
What 7 factors affect synthesis of Vitamin D?
1) Season
2) Latitude
3) Cloud cover
4) Pigmentation
5) Age
6) Sunscreen
7) Obesity

What are the steps to make active vitamin D?
Calciferol (inactive) --(25-hydroxylase)--> 25-hydroxyvitamin D / Calcidiol (inactive)
25-hydroxyvitamin D / Calcidiol (inactive) --(1α-hydroxylase)--> 1,25-dihydroxyvitamin D / Calcitriol (active)
What is the main biomarker used to measure vitamin D levels?
a) 7-dehydrocholesterol
b) Calciferol
c) 25-hydroxyvitamin D (aka Calcidiol)
d) 1,25-dihydroxyvitamin D (aka Calcitriol)
c) 25-hydroxyvitamin D (aka Calcidiol) - inactive
has a longer 1/2 life (2-3 weeks)
Vitamin D + vitamin ______ work together to alter Gene Expression?
vitamin A
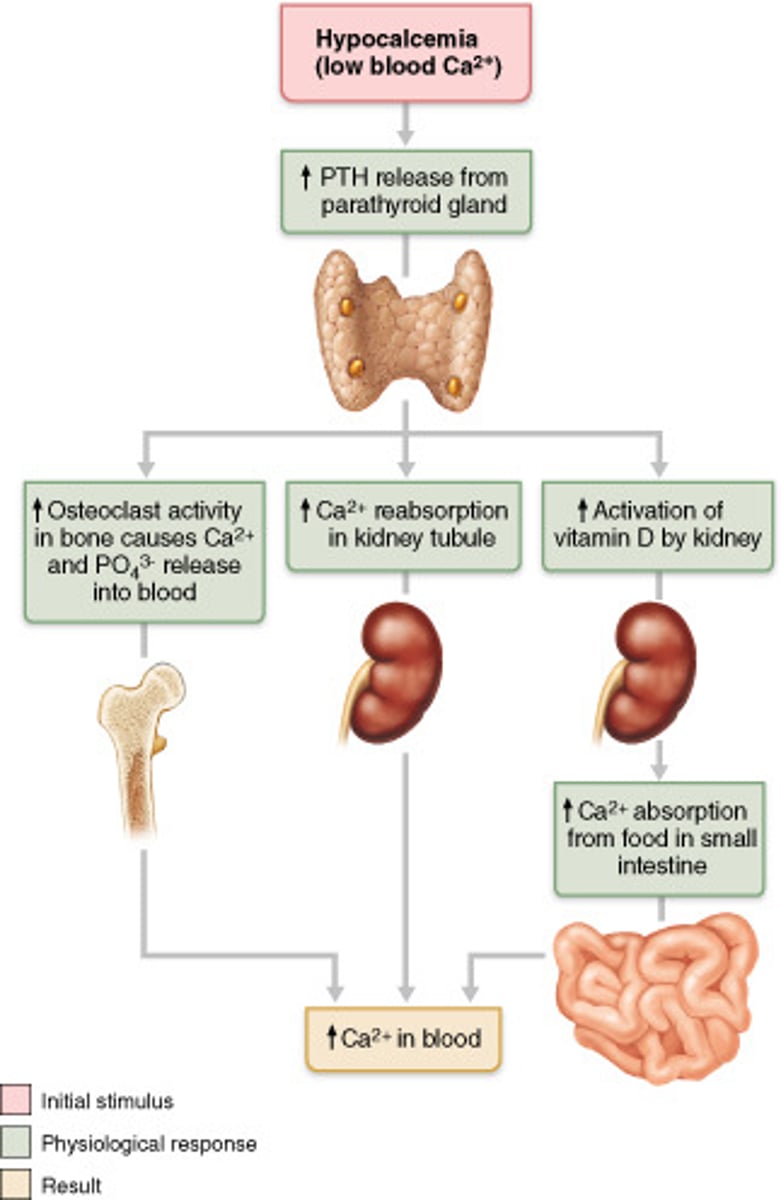
(Know this) How does vitamin D increase free blood calcium levels?
1. Free low blood calcium
2. Parathyroid hormone (PTH) secreted from parathyroid gland
3. PTH induces hydroxylase in kidneys
4. Hydroxylase activates calcitriol
5. Calcitriol stimulates synthesis of calcium-binding proteins
6. Calcium-binding proteins increase calcium absorption and decrease calcium excretion
(Know this) Current Vitamin D Recommendations
≤ 1 year = ____________IU (_____mcg)
1-70 years = ____________IU (_____mcg)
>70 years = ____________IU (_____mcg)
≤ 1 year = 400 IU (10 mcg)
1-70 years = 600 IU (15 mcg)
>70 years = 800 IU (20 mcg)
These are not optimal dose recommendations, these are doses that prevent deficiency in 97.5% of pop.
(T/F): Consumed Vitamin D requires no digestion to be absorbed.
True
(T/F): If an individual is outside in the sun too long they can can reach toxic levels of vitamin D.
False; there has been no documented cases of toxicity from excessive sunlight
Where is Vitamin D mainly stored in the body?
Adipose tissue

What populations are at risk for vitamin D deficiency?
1) Breastfed infants
2) Older adults (70-year olds have 75% less synthesis)
3) Fatty malabsorption (IBD, Cystic fibrosis, Celiac)
4) People with more skin pigmentation
5) Limited sun exposure (season, cloud cover, latitude)
6) Obese patients or those with gastric bypass
In what organ does the enzyme alpha-1-hydroxylase hydroxylate vitamin D3 to its fully active form?
Kidney
Does vitamin E need to be digested?
Yes it is toxic on it's own; esters are required for digestion using pancreatic esterase and duodenal mucosal esterase
Forms of Vitamin E
1) Tocopherols
2) Tocotrienols
(Functions) Vitamin E
1) Antioxidant; donates H to free radicals to protect PUFA in plasma membranes
2) Immune system
3) Inflammation & platelets
4) Decrease clotting / thin out blood
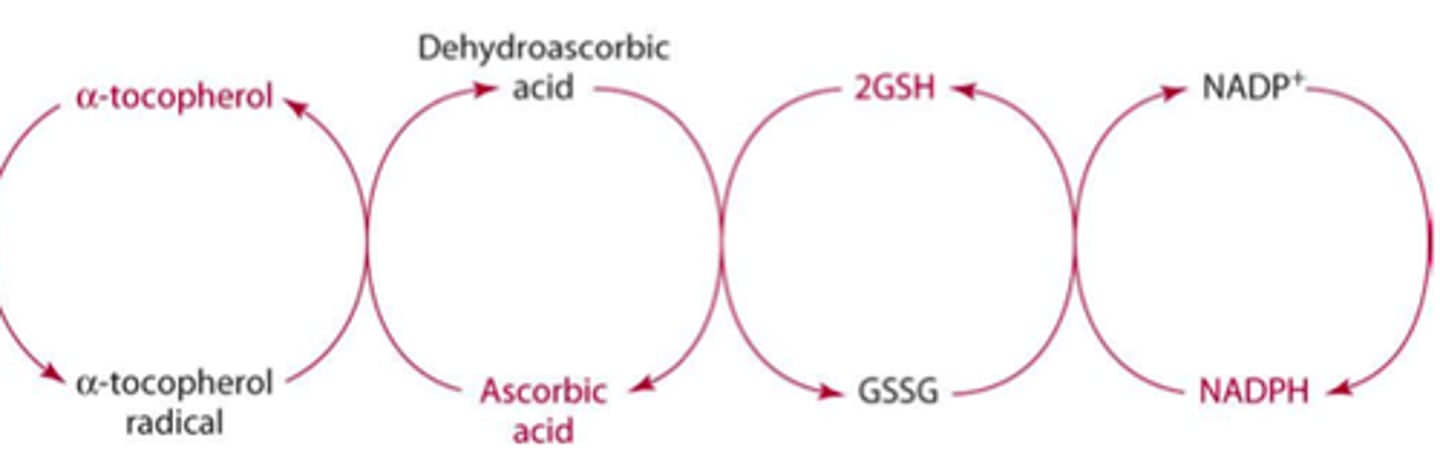
Vitamin _____ is required for the regeneration of vitamin E.
Vitamin C ("C is the Key to E")
(T/F): Natural and Synthetic forms of vitamin E are equally bio-available to us when consumed.
False; the natural form found in food is more bio-available

(Deficiency Name) Vitamin E
Hypovitaminosis E
(Deficiency Symptoms) Vitamin E
rare in adults; have to be low for >5 years
1) Hemolytic anemia (premature infants only)
2) Neuropathy; due to disturbances in myelin production
3) Retinopathy
4) Skeletal myopathy
5) Impaired immune response

(Toxicity limit) Vitamin E
Hypervitaminosis E
(Toxicity Symptoms) Vitamin E
1) Supplements inhibit vitamin K activity = Thrombocytopenia / Increased bleeding
2) Impaired bone mineralization
(T/F): The only way to have toxic levels of Vitamin E is through supplementation, eating it in food has no toxic level.
True
(Sources) Vitamin E
1) Wheat germ oil
2) Nuts & seeds / seed oils
3) Olive oil

What populations are at risk for vitamin E deficiency?
1) Fatty malabsorption (Cystic fibrosis, pancreatic cancer, bile disorders)
2) Premature infants

Vitamin E and Selenium work together to form...
antioxidant enzyme Glutathione peroxides; antioxidant enzymes that protect organisms from oxidative damage
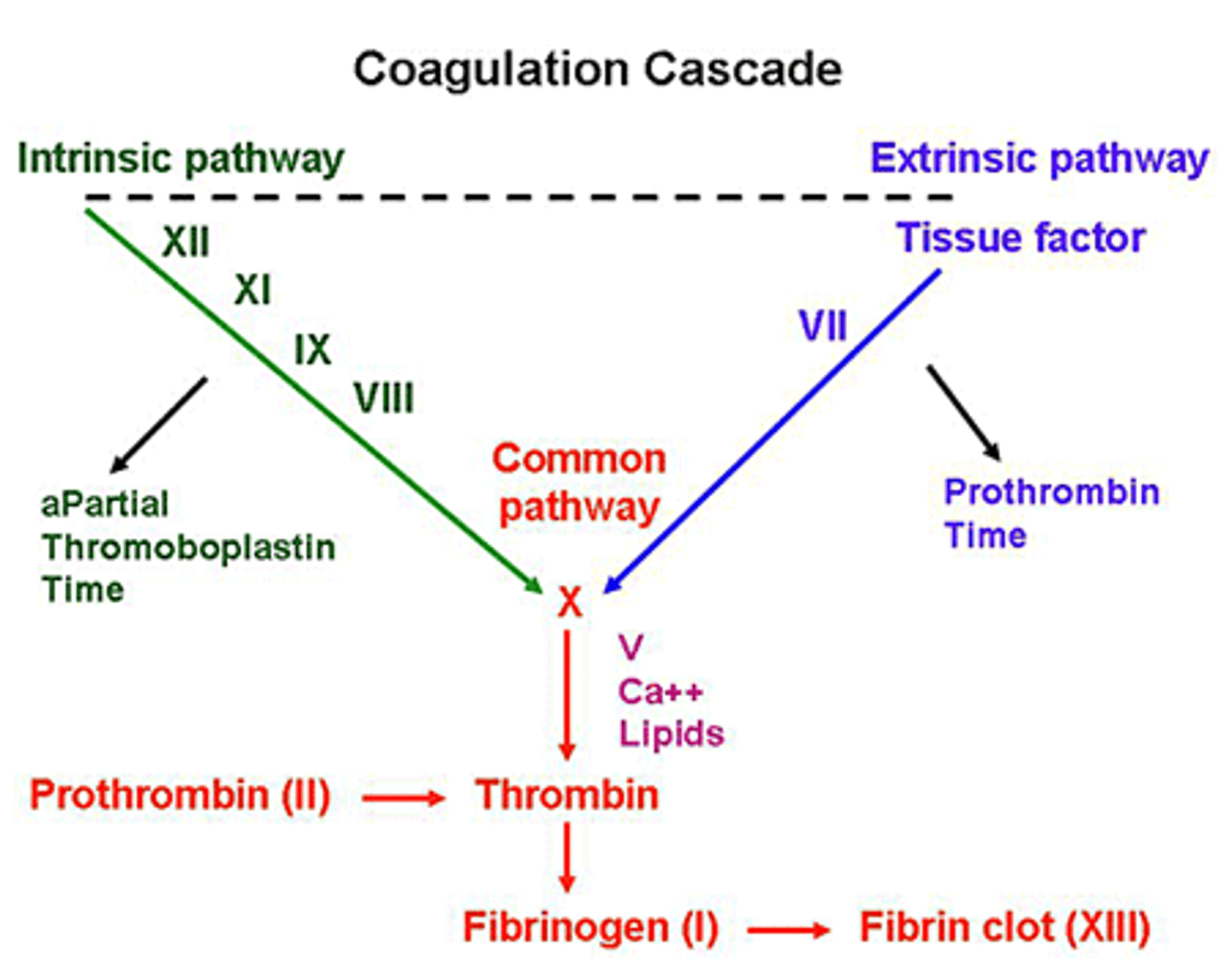
(Functions) Vitamin K
1) Coenzyme (Vitamin K-dependent carboxylase); adds a carboxylic acid group to glutamate residues in specific proteins to make carboxyglutamates
1a)prothrombin - clotting cascade
1b) calcium binding site
1c) osteocalcin for bone formation
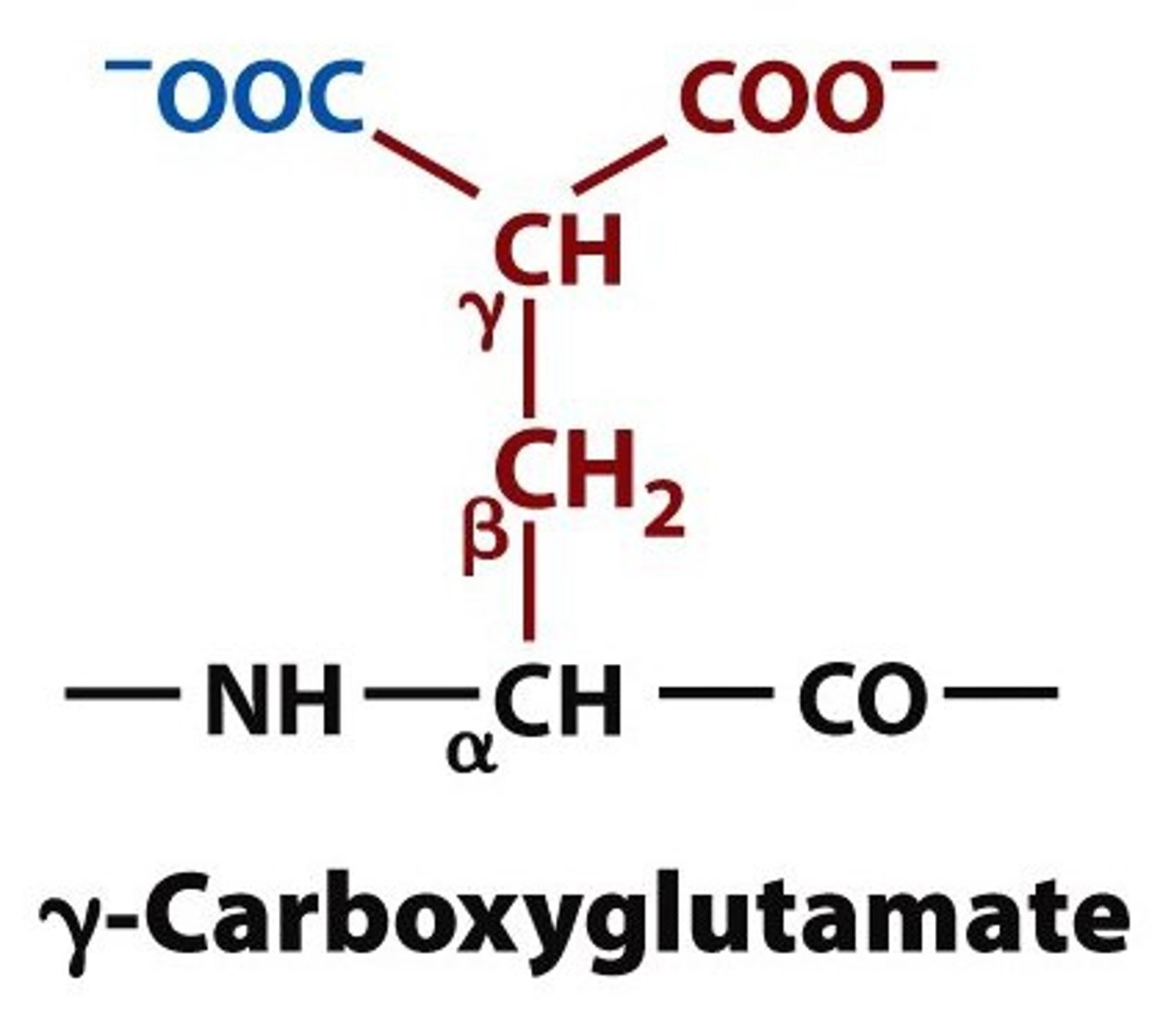
What is the function of carboxyglutamates?
Calcium-binding sites; found in clotting factors (VII, IX, & X), prothrombin and osteocalcin (secreted by osteoblasts) & bone formation
What are the two forms of Vitamin K?
Phylloquinone - Plant
Menaquinone - Animal & LI bacteria
(T/F): Consumed Vitamin K requires no digestion to be absorbed.
True
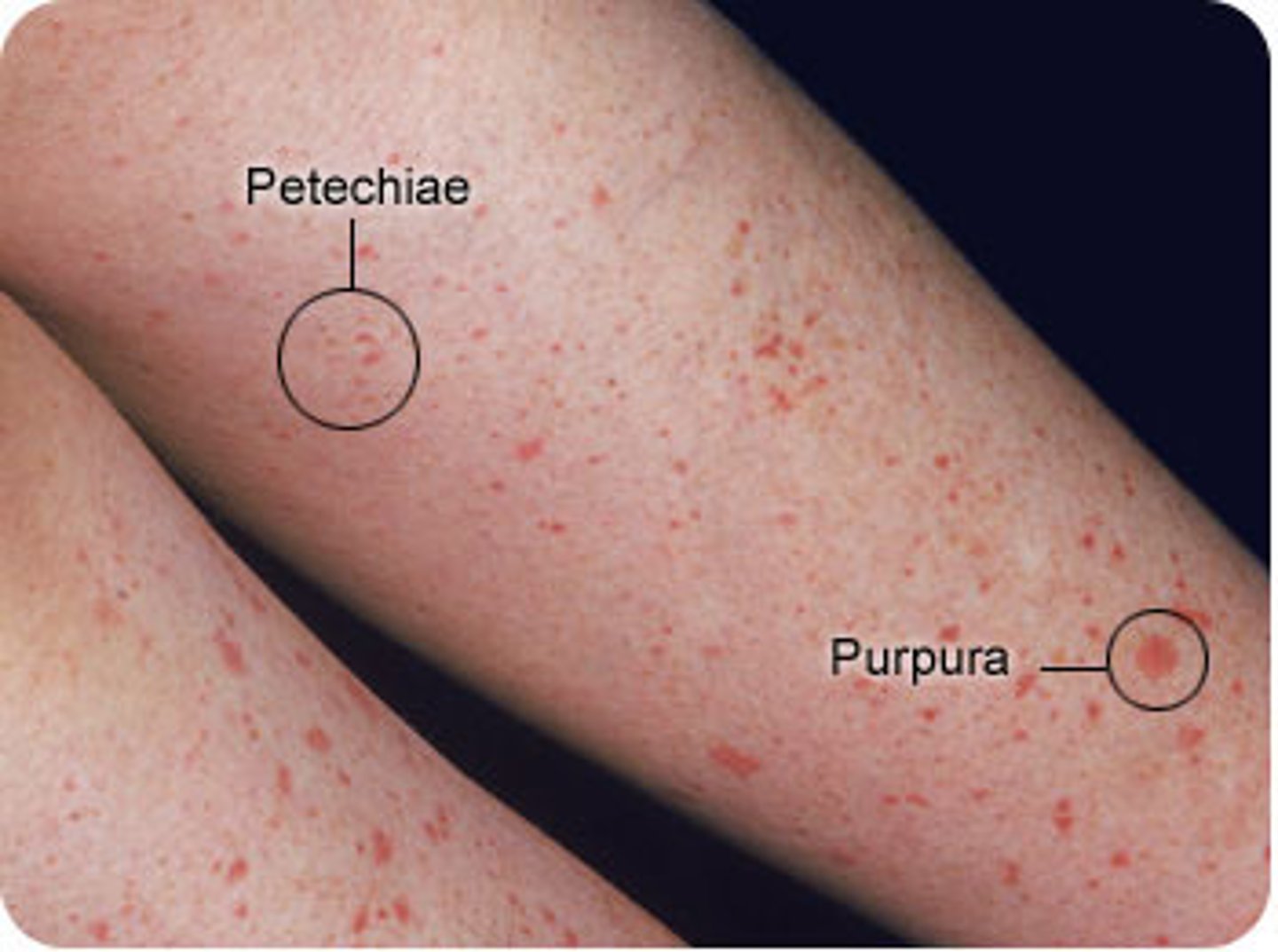
(Deficiency Symptoms) Vitamin K
1) Increased bleeding (common in malabsorptive patients and newborns)
2) Poor bone growth

(Toxicity limit) Vitamin K
None from food or current supplements
(Sources) Vitamin K
Phylloquinone = dark leafy veg.
1) Broccoli
2) Dark green leafy vegetables
3) Kiwi
Manaquinones = animal products
4) Meat, Dairy, Eggs
5) Natto (Fermented soybeans)
What populations are at risk for vitamin K deficiency?
1. Newborns (get vitamin K shot at birth to prevent bleeding in the brain)
2. Fatty malabsorption (Cystic fibrosis, pancreatic cancer, bile disorders)
3. Prolonged use of antibiotics (alters gut microbiome - Menaquinone)

What two fat soluble vitamins are toxic and need to be digested?
A & E
A =
1) Chylomicron brings Retinol into cell
2) Hydrolase removes FA from Retinol (free Retinol = toxic)
3) CRBP binds to Retinol (no longer toxic)
4) CRBP breaks off an LRAT adds FA making Retinol Ester
E =
esters are required for digestion using pancreatic esterase and duodenal mucosal esterase
Which vitamin is most likely to become toxic in large quantities?
Alpha-tocopherol (Vitamin E) or Preformed Vitamin A (Teratogenic)
Which does NOT have antioxidant functionality?
Alpha-tocopherol
Retinol
Ascorbic acid
Beta-Carotene
Retinol (Preform vitamin A)
Alpha-tocopherol - vitamin E
Ascorbic acid - vitamin C
Beta-Carotene - proform vitamin A