Pediatric Nutrition
1/12
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
“Normal” Nutritional Requirements…
Differ based on age, developmental stage, weight, and activity level.
Infants (0 to 12 months)
Toddlers (1 to 3 years)
Preschoolers (3 to 6 years)
School-Age Children (6 to 12 years)
Adolescents (11 to 20 years)
Adequate nutrition is essential for growth and development.
Infant Nutrition
Encourage breastfeeding until 6 months of age.
Formula Feeding:
Most formulas are 20 kcal/oz but can go up to 30 kcal/oz.
Types of Formula:
Standard Cow Milk Formula
Partially Hydrolyzed
Fully Hydrolyzed
Amino Acid-Based
Soy (also Lactose-Free)
Introduction of Solid Foods:
At 6 months of age, assess readiness for solid foods.
After 6 months, finger foods can be introduced.
New foods should be introduced every 4 to 7 days to monitor for allergies.
Foods should be introduced in this order: fruits → vegetables → meat → eggs → citrus.
Rice cereal, baby foods, and finger foods can be introduced at this time.
Transition to Whole Milk & Cup:
At 1 year of age, whole milk can be introduced.
Introduce a sippy cup at age 1 and phase it out by 18 months.

Nutrition: Breastfeeding
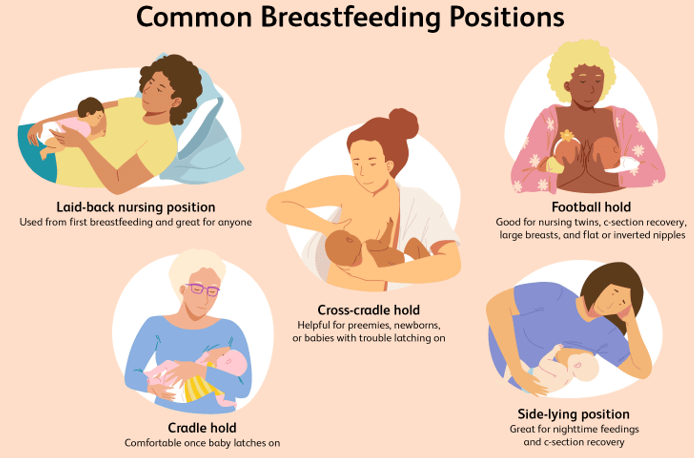
Breastfeeding or feeding of expressed human milk is recommended for all infants, including sick or premature infants.
Breastfeeding Statistics (2019):
83.2% of infants started out receiving some breast milk.
78.6% were receiving breast milk at 1 month.
At 6 months, 55% of infants received any breast milk, and 24.9% received breast milk exclusively.
Composition of Breast Milk:
Includes lactose, lipids, polyunsaturated fatty acids, and amino acids.
The concentration of iron in breast milk is lower than that of formula but has increased bioavailability, usually meeting the infant’s needs for the first 4 to 6 months.
Monitoring Input & Output:
Input is estimated based on feeding time, weight, and wet diapers.
Adequate output is approximately 1 mL/kg.
Toddler Nutrition
Establish healthy eating habits early.
Weaning from breastfeeding is an individualized decision.
Wean from the bottle around 12 to 15 months while ensuring adequate calcium intake.
Toddlers are picky eaters—avoid substituting unhealthy foods just to get them to eat.
Serve foods at room temperature in bite-sized pieces.
Encourage self-feeding and promote water intake.
Transition from whole milk to 2% if the child is tracking appropriately on the growth curve.

Preschooler Nutrition
Quality of food consumed is more important than quantity—primary teeth are present at this stage.
Continue to build and reinforce healthy eating habits.
Parents should maintain positivity, patience, and offer choices to encourage healthy eating.
Avoid substituting unhealthy foods if the child is not eating as much as expected.
Obesity is a concern in this age group—according to the National Health and Nutrition Examination Survey, 13.9% of 2- to 5-year-olds are obese.

School-Aged Child Nutrition
Children should consume fewer calories as their growth rate slows.
Common influences on eating habits include family, friends, and media.
Obesity is more prevalent in this age group.
Limit fat and processed sugar intake.
Avoid using food as a reward.
Encourage children to be involved in making healthy food choices.

Adolescent Nutrition
Desire for independence influences food choices.
Educational support on nutrition is essential.
Increased need for zinc, calcium, and iron.
Higher calorie intake is required for growth and sexual maturation.
Nutritional support is important for managing disorders at this age.

Eating Disorders
Anorexia Nervosa: Body image disturbance leading to extreme weight loss.
Bulimia Nervosa: Cycle of normal food intake followed by purging.
Complications:
Fluid and electrolyte imbalance
Decreased blood volume
Cardiac arrhythmia
Esophagitis
Rupture of the esophagus or stomach
Tooth loss
Menstrual problems
Nursing Considerations:
Restoration of fluid and electrolyte balance
Encourage family involvement
Prevent complications
Provide referrals to resources and support

Failure to Thrive
Inadequate growth resulting from the inability to obtain and/or use calories for growth.
Can be organic (e.g., GERD, malabsorption, cardiac conditions, increased metabolic needs) or inorganic (e.g., lack of education or resources).
Little to no weight gain.
Weight/age falls below the 5th percentile.
Nursing Management:
Provide education to caregivers.
Conduct a thorough assessment of nutritional intake and growth patterns.
Serve as a role model for healthy feeding practices.
Increase caloric intake for catch-up growth.
Implement multidisciplinary care (e.g., nutritionists, social workers, therapists).
Document progression and response to interventions.
Note: The patient may or may not appear malnourished.

Common Food Allergies
Cow’s Milk
Peanuts
Wheat
Eggs
Fish
Shellfish
Obesity in Children and Adolescents
For children and adolescents aged 2-19 years in 2017-2020, the prevalence of obesity was 19.7%, affecting about 14.7 million individuals (CDC, 2024).
Overweight: BMI at or above the 85th percentile
Obese: BMI at or above the 95th percentile
Two-part issue:
Diet
Exercise
Providing Nutritional Support: Enteral Nutrition
Routes: NG, NJ, OG, G-Tube
Functioning GI tract but cannot ingest nutrients orally.
Cost-effective, safer than parenteral nutrition.
Bolus or continuous feeds.
Special Considerations:
Correct measurement
Placement verification

Providing Nutritional Support: Parenteral Nutrition
TPN (Total Parenteral Nutrition)
Highly concentrated solution of carbohydrates, electrolytes, vitamins, and minerals.
TPN is given centrally, not peripherally.
Long-term use is not typical.
Complications include:
Air embolism
Electrolyte imbalance
Infection
