Micro Final Exam
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
179 Terms
Carbon Cycle
-Carbon enters a common pool of organic matter that can be oxidized back to CO2
-Cycle begins with carbon fixation
-1/2 of earth’s carbon is fixed aerobically and anaerobically by microbes
Mircoorganisms that do carbon fixation
-cyanobacteria, which are photosynthetic bacteria
-certain types of archaea found in extreme environments such as hot springs
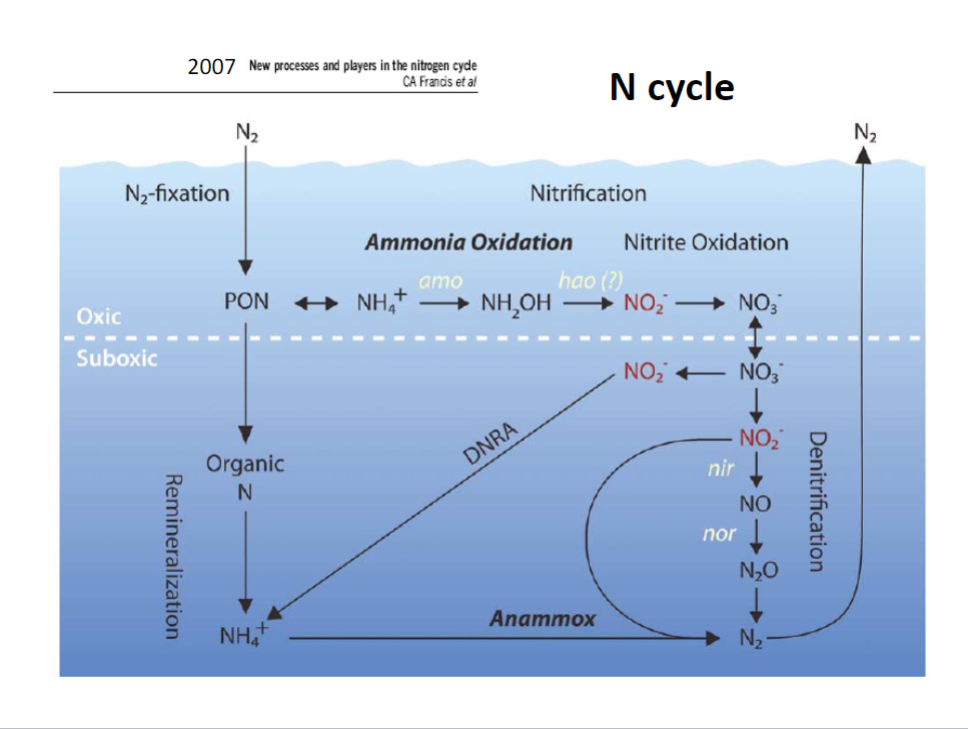
Nitrogen Cycle
-N2 fixation
-Nitrification: ammonia and nitrate oxidation
-Denitrification
-DNRA
-Anammox
Nitrogen Fixation (Diazotrophy)
-N2→NH4+→Organic N
-Energy-demanding process
-Catalyzed by the enzyme nitrogenase (sensitive to O2)
-Widespread in Bacteria and Archaea
-EX: cyanobacteria heterocyst
-EX: Alphaproteobacteria, Rhizobiales: motile rods, grow symbiotically as nitrogen-fixing bacteria within root nodule cells of legumes, most successful plant family on earth.
Nitrification: N-Oxidizing Bacteria
-Nitrifying bacteria
-Oxygen as electron acceptor
-Convert NH3→NO2- ; nitrosomonas of betaproteobacteria
-Convert NO2- → NO3- ; nitrobater of alphaproteobacteria
Denitrification
-multiple steps of reduction of N species from nitrate to dinitrogen gas
-several gas intermediates are involved
-NO3- → NO2- → NO → N2O → N2
-Anaerobic respiration: N as electron accepter
-Chemoorganoheterotrophs: widely distributed among bacterial phyla
-most facultative anaerobes
Anammox
-Anaerobic Ammonia Oxidation
-also produces N2, loss of N from the system
-NH4+ +NO3- →N2 + 2H2O
-phylum planctomycetes: gram -, cell walls lack peptidoglycan, having compartmentalized cells
-chemolithoautotrophs: may contribute 70% of nitrogen cycling in oceans
-Role of N2: Catabolic: NO2- + NH4+ → N2 + 2H2O Anabolic: 2NO2 +CO2 +H2O → CH2O +2NO3-
The Microbial Loop
-transfer of nutrients between trophic levels
-autotrophs are primary producers
-heterotrophic microbes consume dissolved organic matter (DOM)
-particulate organic matter (POM)
-Algae→Small Fish→Large Fish
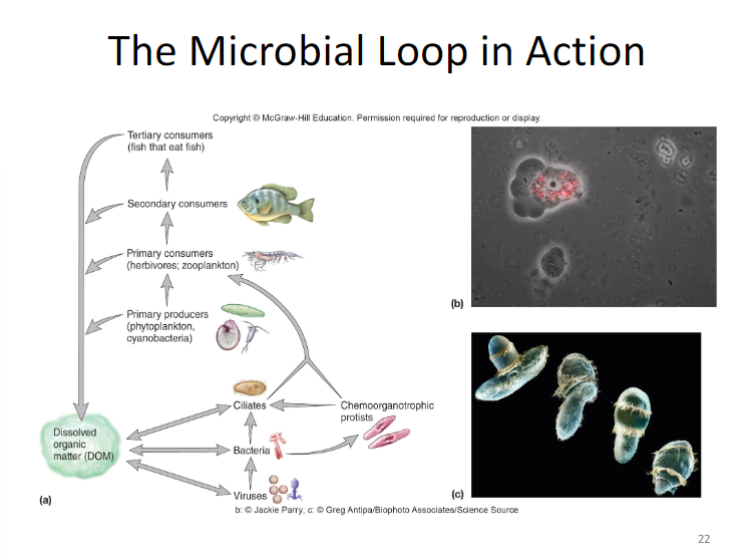
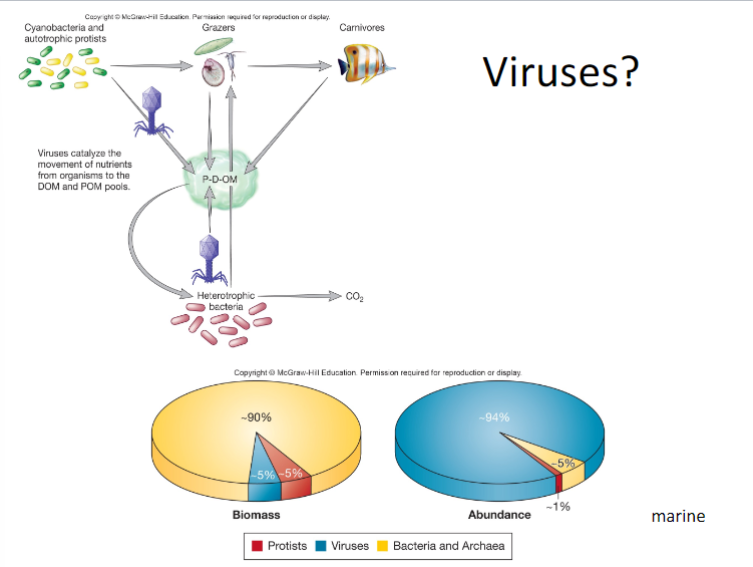
Viruses in Microbial Loop
Types of Microbial Interactions
-Symbiosis: Mutualism, Commensalism/Cooperation, Parasites, Amamensalism
-Predator-prey/parasitism
-Ammensalism
-Competition
Symbiosis
-a physical association of two or more different species of organisms
Ectosymbiont
organism located on surface of another organism, usually larger
Endosymbiont
organism located within another organism
Consortium
-hosts have more than one associated symbionts
-relationships can be intermittent and cyclic or permanent
Mutualism
-reciprocal benefit to both partners
-relationship with some degree of obligation
-often partners cannot live separately
-mutualist and host are dependent on each other
Zooxanthellae
-marine invertebrates harbor them
-dinoflagellates
-provide organic C to host
-coral has pigments that protect algae from UV radiation
-provide N compounds, phosphates, and CO2 to endosymbionts
-Coral bleaching: caused by temp increase, results from loss of photosynthetic pigments or expulsion of the zooxanthellae
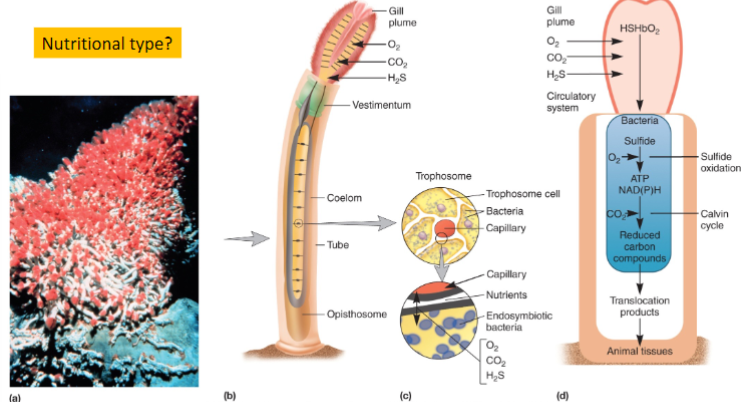
Tube Worm-Bacterial Relationship
Cooperation
-along with commensalism is a positive but NOT OBLIGATE form of symbiosis which involves syntrophic (cross-feeding) relationships
-beneficial to both organisms
-differs from mutualism because cooperative relationship is not obligatory

Commensalism
-one organism benefits and the other is neither harmed nor helped
-commensal: organism that benefits
-can also involve modification of environment by one organism, making it more suited for another organism
-skin or surface microbes on plants or animals
-host plant/animal releases volatile, soluble, and particulate organic compounds, which are used by commensals
-nitrification: carried out by two different bacteria together (nitrosomonas and then nitrobacter)
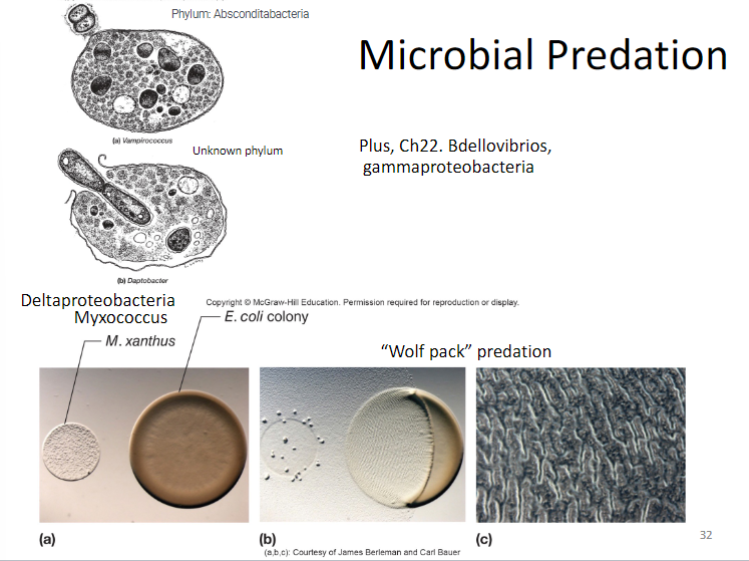
Microbial Predation
-Bdellovibrios
-gammaproteobacteria
-”wolf pack” predation
Parasitism
-one host organism gains (parasite) and the other is harmed (host)
-outcome of long-term parasitic relationship: genome reduction, parasite loses unused genomic information
-successful parasites have evolved to co-exist in equilibrium with their hosts
-Lichen: green bacteria and fungi
Ammensalism
-negative impact of one organism on another based on release of a specific compound
-EX: antibiotic production by fungi and bacteria; use of antibiotic-producing streptomycin by ants to control fungal parasites
Human-Microbe Interactions
-the human body is a diverse environment; specific niches at different parts of the body; dynamic conditions
-microbiome: all the genes of the host and microbiota
-superorganisms: host genes become integrated with those of the symbionts; co-metabolize various substrates, resulting in unique products
-pathogen/pathogenicity
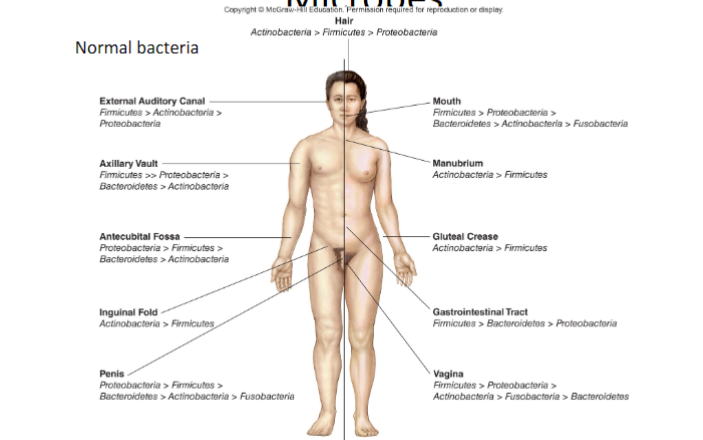
Normal microbiota for the human body
-microbes regularly found at an anatomical site, different at different regions
-relationship begins at birth; humans are born without any microorganisms; varies with environment and food source
-Bifidobacteria: found in breastfed babies; prototrophic: can synthesize all amino acids and growth factors from simple carbs
-microbes found on surface tissues of human skin and mucous membrane
The human microbial metagenome
-colonization of skin, oral/respiratory tract, genitourinary system and gastrointestinal tract begins immediately at birth
-our adult bodies contain 10 times more microbial cells than human cells
-human colon contains 100 trillion bacteria
-comparative metagenomic studies have suggested that shifts in the populations of microbial communities may be associated with a number of important acute and chronic diseases: IBD, obesity, heart disease, eczema, vaginal infections
Adaption of microbiota to human body
-Skin: transient or resident; dry, moist, oily
-Mouth, oral cavity: nutrient rich but subjected to mechanical forces
-Stomach: low pH
-Small/large intestine: nutrient rich, suitable pH
-Urinary track: frequent flush
What organ hosts the largest amount of normal microbiota in humans?
Large intestine
What organ hosts the smallest amount of normal microbiota in humans?
Lungs
Immunity
-host’s ability to resist infectious diseases
Nonspecific (innate, natural)
-first line of defense
-no specificity, no immunological memory
Specific (acquired, adaptive)
-resistance to a particular foreign agent
-has “memory”
Level 1: Barriers
-microbial (commensal organisms)
-physical (epithelium, mucous membrane)
-chemical (AMPs, APRs, cytokines)
1.1: Microbial
-the relationship between normal/commensal microbiota and the host
-can offer mutual benefits: normal microbiota often prevent colonization by pathogens; bacterial produces e.g. vitamins B and K are beneficial to the host
-opportunistic pathogens: members of normal microbiota that produce disease under certain circumstances
-compromised host: debilitated host with lowered resistance to infection
1.2: Physical Barriers
-interface between human and microorganisms are guarded
-skin & mucous membranes: mouth, resp. system, gastrointestinal tract, genitourinary tract
Skin
-inhospitable environment for microbes
-shedding of outer skin cells
-high NaCl
-periodic drying
-strong mechanical barrier to microbial invasion: keratin produced by keratinocytes in outer layer; hard to penetrate
Mucous Membrane
-mucous: slippery, flushing, acidic, special structure (ciliated epithelial cells), antimicrobial chemicals (lysozyme, degrade peptidoglycan)
-lungs don’t have normal microbiota
-cells are alveolar sponges
Mucous Membranes by Part
-mouth: biofilm on teeth, transitional (flush away)
-stomach: unfriendly env., gastric acid pH 2-3
-small/large intestine: microbe number increases from small to large, fluid like pancreatic enzymes and bile, pH becomes more alkaline, most bacteria at the end
-genitourinary tract: urine flushing and kill bacteria (low pH and toxic compounds), normal microbiota
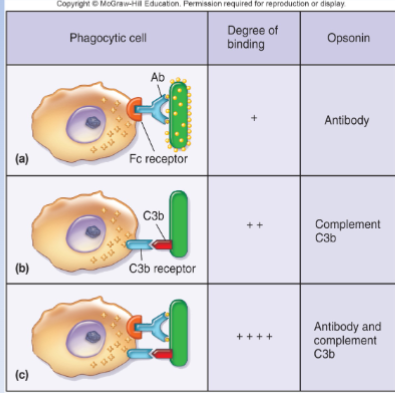
Opsonization-Enhanced Phagocytosis
-microbes are coated by opsonins in preparation for recognition/ingestion by phagocytic cells
-opson: to prepare victims for…
Chemical Mediators: Cytokines
-cytokines: cell movement; works in both innate and adaptive immunity
-chemical messages between cells
-soluble proteins or glycoproteins act as intercellular mediators (signaling molecules)
-synthesis is inducible from nonspecific stimuli
-3 functional groups as regulators of: innate resistance, adaptive immunity, and hematopoiesis
Level 2: Cells of the Immune System
-Leukocytes: white blood cells, involved in both specific and nonspecific immunity, granulocytes vs agranulocytes
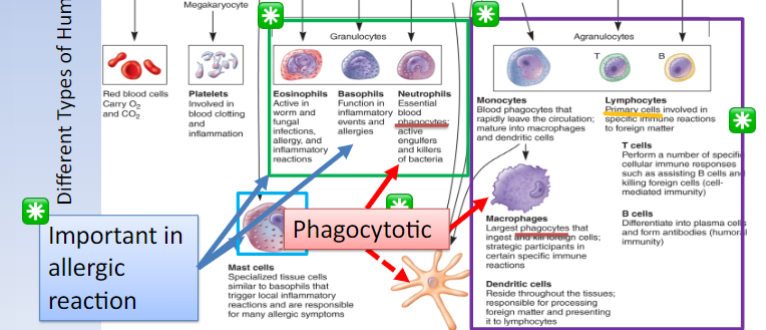
Granulocytes
-Eosinophils: active in worm and fungal infections, allergy and inflammatory reactions
-Basophils: function in inflammatory events and allergies
-Neutrophils: essential blood phagocytes; active engulfers and killers of bacteria
Arganulocytes
-ALL are phagocytotic plus Neutrophils
-Monocytes: blood phagocytes that rapidly leave the circulation; mature into macrophages and dendritic cells
-Macrophages: largest phagocytes that ingest and kill foreign cells; strategic participants in certain specific immune reactions
-Dendritic cells: reside in the tissues; responsible for processing foreign matter and presenting it to lymphocytes
-Lymphocytes: primary cells involved in specific immune reactions to foreign matter
-T-cells: lymphocyte, perform a number of specific cellular immune responses like assisting B cells and killing foreign body cells (cell-mediated immunity)
-B-cells: lymphocyte, differentiate into plasma cells and form antibodies (humoral immunity)
Lymphocytes
-natural killer cells-innate
-no phagocytic granular lymphocytes
-important role in innate immunity
-kill malignant cells and cells infected with pathogens by releasing cytotoxic enzymes
-NK cells DO NOT kill foreign particles, but neutrophils and macrophages do
B-cell: Adaptive Immune System
-bone marrow
-circulate in blood and can settle in lymphoid organs
-plasma cells and produce antibodies
-humoral immunity: antibody-mediated immunity

T-cell: Adaptive Immune System
-thymus
-circulate in blood or reside in lymphoid tissue
-differentiated tissue helper (TH) and cytotoxic lymphocytes (CTLs)
-major role in B-cell activation
- cellular immunity: cell-mediated immunity

Primary B and T cell location
-bone marrow
-thymus
Secondary B and T cells locations
-axillary lymph node
-spleen
-MALT (mucosal-associated lymphoid tissue)
-afferent lymphatic vessels
-involved in skin and mucous membrane immunity
Level 3: Processes-Phagocytosis
-the process of cell eating
-the lysosomes fuse with the phagosomes containing the ingested microbes and the microbes are destroyed
-recognize: pattern recognition molecules (PRM)
-ingest
-digest
-microbe-associated molecular patterns (MAMPs): LPS for G -, peptidoglycan for G +
-intracellular digestions and exocytosis: secretory vesicles expel out or build membrane
Level 3: Processes-Inflammation
-innate immune defense reaction but also combined with adaptive defense
-bring all the host defense together in response to injury or infection
-localized to tissue infection/injury: can be used by pathogen or physical trauma, acute inflammation is the immediate response of body to injury or cell death
-cardinal signs: redness, warmth, pain, swelling, altered function
-acute or chronic inflammation
Specific (Adaptive) Immunity
-recognize nonself
-respond to nonself
-remember nonself
Acquired Immunity
-Natural immunity: is acquired though normal life experiences and is not induced through medical means
-Artificial immunity: is produced purposefully through medical procedures (immunization)
Natural Immunity
-active immunity: the consequence of a person developing his or her own immune response to a microbe (ex: infection)
-passive immunity: the consequence of one person receiving preformed immunity made by another person (ex: maternal antibody)
Artificial Immunity
-active immunity: the consequence of a person developing his or her own immune response to a microbe (ex: vaccination)
-passive immunity: the consequence of one person receiving preformed immunity made by another person (ex: immune globulin therapy)
Antigens
-self and nonself substances that elicit an immune response and react with products of that responses
-antigenic determinant sites (epitopes)
-antibody affinity: strength with which antibody binds to its antigen at a given antigen-binding site
-most are large, complex molecules
Haptens
-small organic molecules
-not antigenic, but may become antigenic when bound to larger carrier molecules
-ex: penicillin, may elicit hapten-specific and carrier-specific responses
Recognize non-self (antigens)
-major histocompatibility complex (MHC): collection of genes that code for self/nonself recognition potential of a vertebrate
-present antigens to activate T-cells
T-cell Development
-antigen-presenting cells (APC)-dendritic cell
-T-cell receptors (TCR) complexes: bind to MHC
-endocytosis
-degrade by lysosomal process
-bind with MHC receptor
-presentation on the cell surface
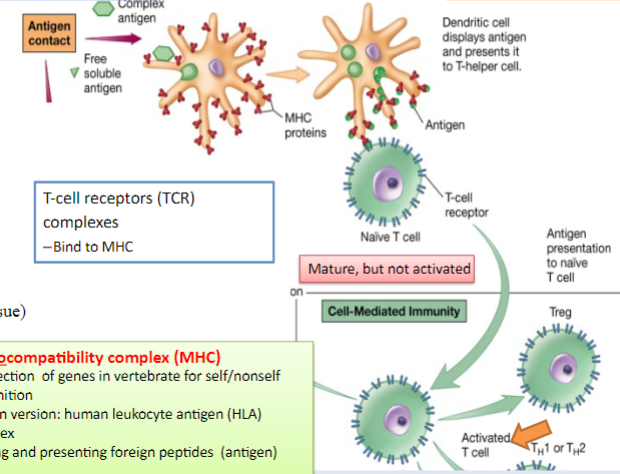
Major Histocompatibility Complex (MHC)
-a collection of genes in vertebrates for self/nonself recognition
-human version: human leukocyte antigen (HLA) complex
-binding and presenting foreign peptides (antigen)
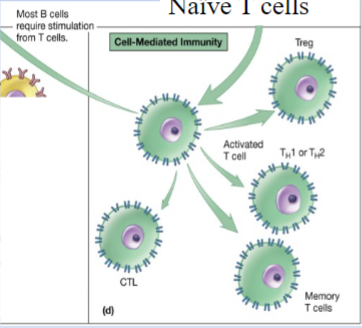
Mature T-cells
-mature T-cells are naive until they are activated by antigen presentation
-once activated, they proliferate into effector cells and memory cells
-effector cells carry out specific functions to protect host
-regulatory (Treg) cells
-T-helper (TH) cells: help with activation CTL
-cytotoxic lymphocyte (CTL): matured from cytotoxic t-cells, destroy infected host cells
-memory T-cells
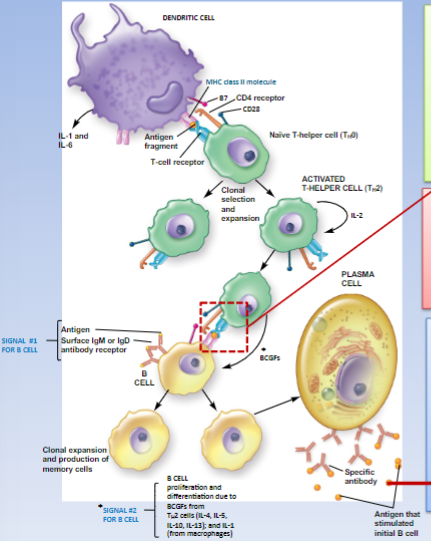
B-cell Activation/Functioning
-B-cells must be activated before functioning
-2 mechanisms for antigen-specific activation: T-dependent where B-cell binds with T-helper cell, or T-independent (minor)
-activation leads to proliferation and differentiation into plasma cells (secrete antibodies)
-antibodies neutralize or recognize antigens
-also called immunoglobulin (Ig)
-in blood serum, tissue fluids, and mucosal surfaces of vertebrate animals; an antibody can recognize and bind antigen that caused its production
Ig Structure
-Y-shape
-stalk: crystallizable fragment (Fc) and constant region (C)
-top: binding fragments (Fab) and both constant and variable regions (V)
-four polypeptide chains: two identical heavy chains (H) and two identical light chains (L) connected by disulfide bonds

Ig classes: gamma and mu
-IgG: heavy chain gamma, 9 mg/ml mean serum concentration, 80-85% of total serum antibody, most abundant in body fluids, neutralizes toxins, opsonizes bacteria
-IgM: heavy chain mu, 1.5 mg/ml mean serum concentration, 5-10% of total serum antibody, first to appear after antigen stimulation, very effective agglutinator, expressed as membrane-bound antibody on B-cells
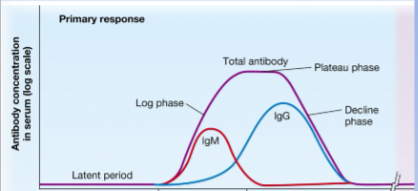
Ig Primary Response
-latent (lag) period: several days to weeks after initial exposure to antigen; no antibody detectable in blood
-IgM appears first, followed by IgG
-log phase: plasma cells/antibodies production
-plateau phase: antibody titer stabilize
-decline phase: antibody binds to antigen
Ig Secondary Antibody Response
-upon secondary exposure to same antigen, B-cells mounted a heightened memory response
-shorter lag
-rapid log phase
-longer persistence
-a higher IgG titer
-production of antibodies with a higher affinity for the antigen
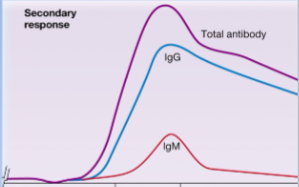
Comparing Phases 1 and 2
-antigen exposure: first vs. re-exposure
-lag phase: long vs. short
-log phase: antibody concentration low vs. high; production time of IgM and IgG: IgM earlier than IgG vs. similar time
-persistence of antibody: shorter vs. longer
-antigen affinity of produced antibodies: low to moderate vs. high
Specific Immune Response
-vaccine
-antibody diversity
-each human can synthesize antibodies that can bind to more than 10^13 antigens
Immune Disorders
-hypersensitivities
-autoimmune diseases
-transplantation (tissue) rejection
-immunodeficiencies
The Chain of Infection
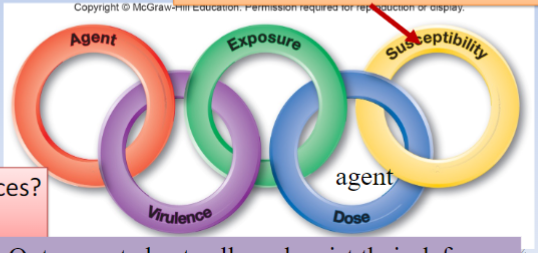
Agent: Pathogen
-any parasitic organism causing infectious disease
Pathogenicity
-ability of a parasite to cause disease
Primary (frank) Pathogen
-causes disease by direct interaction with healthy host
Opportunistic Pathogen
-may be part of normal flora and causes disease when it has gained access to other tissue sites or host is immunocompromised
Time Course of Infectious Disease
-Incubation period: no obvious signs and symptoms
-Prodromal stage: onset of signs and symptoms, not clear enough for diagnosis
-Period of illness: disease is most severe, signs and symptoms
-Convalescence: signs and symptoms begin to disappear
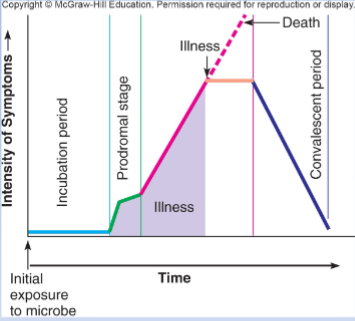
Signs
-objective changes in body that can be directly observed
Symptoms
-subjective changes experiences by the patient
Disease Syndrome
-signs + symptoms
Virulence
-degree or intensity of pathogenicity
-toxic to the host
-resist host defense
-largely determined by genes on pathogenicity islands: genes for toxin production, bacterial attachment, intracellular survival; HGT
Virulence Factors
-determine the degree to which the pathogen causes damage, invasion, infectivity
Virulence: Attachment and Colonization
-pili and fimbriae bind to complementary receptor sites on host cell surface

Virulence: Invasion
-invasiveness
-penetration
Invasiveness
-ability to spread to adjacent tissues
Peneetration
-active: occurs through lytic substances which disrupt host cell surface
-passive: skin lesions, insect bites, wounds; spread by body fluid/chemicals
Virulence: Exotoxins
-soluble
-heat liable
-proteins
-could be lethal
- highly immunogenic
-mostly produced by G -
-easily spread out
-various types: AB exotoxins - A subunit is responsible for toxic effect, B subunit binds to specific target cell
-botulinum toxin

Virulence: Endotoxins
-heat stable
-weakly immunogenic
-generally similar, despite source
-cause general system effects: fever, diarrhea, inflammation, intestinal hemorrhage
-bring about these effects indirectly
-interacts with host molecules and cells, activating host systems; coagulation, complement, fibrinolytic, and kininogen system
-ex: LPS: G-bacteria (leads to septic shock)
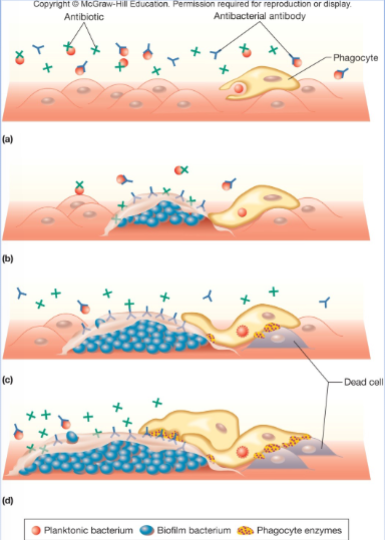
Virulence: Biofilm Development
-physiologically different from planktonic growth
-may cause chronic infection
-increases virulence
-becomes less sensitive to antibiotics
-make cells in biofilm more resistant to host defense (“frustrates” phagocytes)
Virulence: Resisting Host Defenses
-numerous mechanisms for both viral and bacterial pathogens
-infection of immune system cells, diminishing function
-fuse with adjacent cells to prevent exposure to antimicrobial proteins in host
-capsules prevent phagocytosis
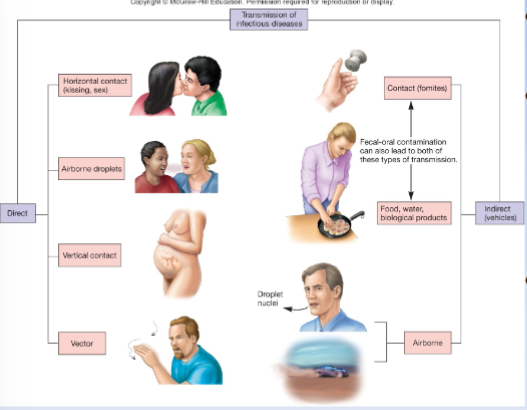
Pathogen Transmission
-direct contact → less virulent
-vector-borne → highly virulent in human host, relatively benign in vector
-greater ability to survive outside host → more virulent
Epidemiology
-science that evaluates occurrence, determinants, distribution, and control of health and disease in a defined human population
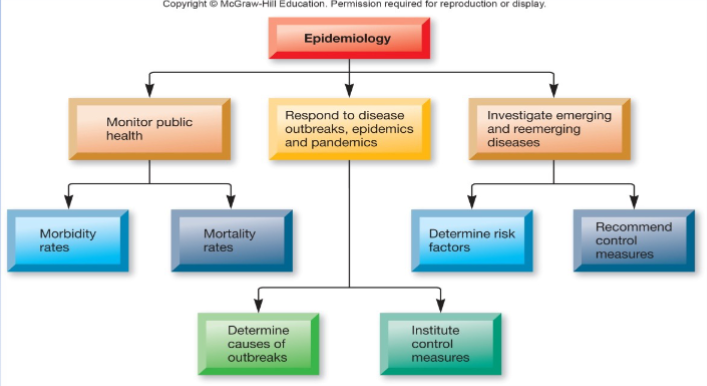
Sporadic Disease
-occurs occasionally and at irregular intervals
Endemic Disease
-maintains a relatively steady low-level frequency at a moderately regular interval
Hyperendemic Disease
-gradually increase in occurrence frequency above endemic level but not to epidemic level
Outbreak
-sudden, unexpected occurrence of disease
-usually focal or in a limited segment of population
Epidemic
-sudden increase in frequency above expected number
Index Case
-first case in an epidemic
Pandemic
-increase in disease occurrence within large population over a wide region (usually worldwide).
COVID-19
-disease name: Coronavirus disease
-transmission: primarily airborne (zoonotic origins)
-agent name: SARS-CoV-2 virus (severe acute respiratory syndrome coronavirus 2)
-agent structure: enveloped (spikes), ssRNA, huge for a virus
-virulence factors: multiple (ACE2-binding, FURIN, etc)
-signs and symptoms: fever, chills, cough, fatigue, difficulty breathing, cytokine storm (hyperactive innate immune response)
-treatment and prevention: antiviral drug, antibody treatment, mRNA vaccine
Treatment, Prevention, and Control of Viral Infection
-rapid immunologic tests
-antivirus drugs (target the replication cycle)
-symptomatic/supportive therapy
-major way: vaccine (inactivated virus vaccine)
Other Airborne Viral Diseases
-pathogen suspended in air and travels less than 1 meter
-droplet nuclei: small particles (1-4 micro m), can remain airborne for long time, can travel long distances, usually propelled from respiratory tract (source)
-dust particles
-ex: chicken pox, flu

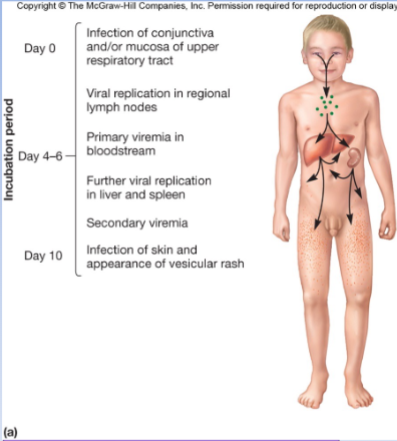
Chicken Pox
-varicella-zoster virus
-transmission: acquired by droplet inhalation into respiratory system
-susceptible population: children 2-7 yo
-signs and symptoms: 10 day incubation period, like a common cold (runny nose, couch, stomach ache), rash appears after 1-2 days
-become immune after recovery
-still a carrier, latent