Male Reproductive System
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
Sexual differentiation timepoints
5-6 weeks embryogenesis
7 weeks
7-12 weeks
7-8 months
5-6 weeks embryogenesis
Sexually indifferent
Gonad
2 immature duct systems (wolffian → male. and Müllerian ducts → female)
7 weeks
SRY protein
Transcription factor
Promotes the development of gonad into teste
Testosterone: development of male sexual organs (reproductive tract from Wolffian ducts)
Müllerian inhibiting substance (MIS): inhibits development of female sexual organs
7-12 weeks
Ovaries: begin oogenesis
Genitalia develop
7-8 months
Testes: descend into scrotum
Ovaries: all primary oocytes (prophase I of meiosis) and primordial follicles
Primary sex organs
Gonads
Testes
Production of gametes
Synthesis of hormones
Secondary sex organs
Accessory sex organs
Internal reproductive organs:
Epididymis
Vas (ductus) deferens
Urethra
Seminal vesicles
Prostate gland
Bulbourethral glands
External reproductive organs
Scrotum
Penis
Scrotum
Thin layer of skin overlaying the darts muscle
Elevates the testes (wrinkling)
Raphe:
Raised thickening of skin; divides scrotum into two internal scrotal cavities
Cremaster muscle:
Deep layer
Internal and external fascia layers
Contraction elevates the testes
Sexual arousal, cold temperatures
Development of spermatozoa requires temperatures…
2 degrees (F) lower than normal body temperature
Testes
Tunica albuginea: outer fibrous capsule
Fibrous partitions (continus with TA), divides testis into lobules
Seminiferous tubules: sight of sperm production; highly coiled individual tubules (around 800) which empty into common duct system
Rete testis: channels that direct spermatozoa out of testis and into the channels of the epididymis
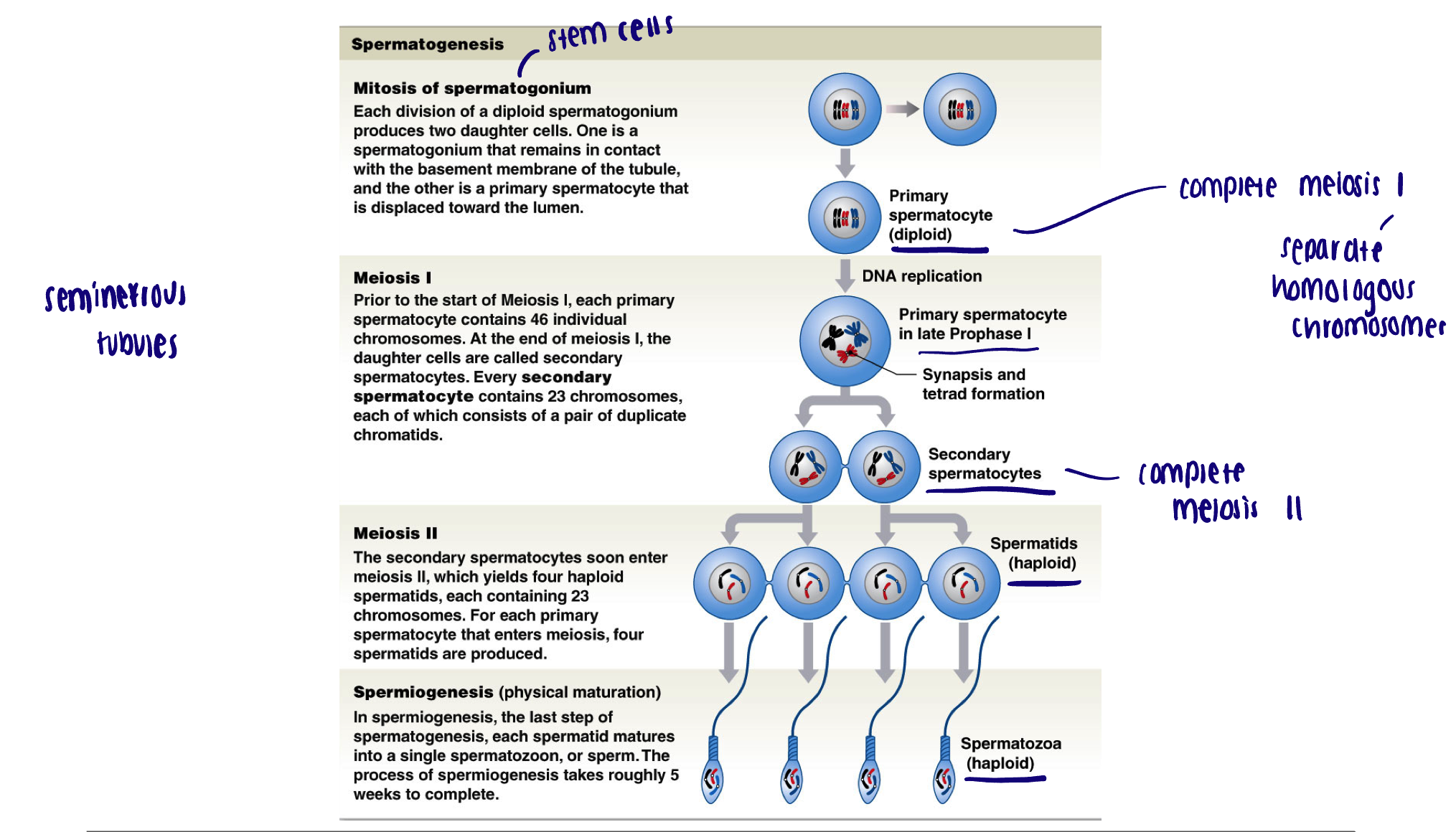
Cell types of the testes
Sertoli cells (nurse cells): form wall of the tubules
Key role: support spermatogenesis
Leydig cells: surround seminiferous tubules
Key role: androgen production (mostly testosterone small amount of DHT)
Gametes at various stages of development → key role: propagation of the species
Spermatogonia (stem cell)
Spermatocytes
Spermatids
Spermatozoa (sperm)
Hypothalamic-Pituitary-Gonadal Axis
Testosterone production by Leydig cells is under regulation of the hypothalamic-pituitary axis
The hypothalamic- pituitary axis also regulates the process of spermatogenesis
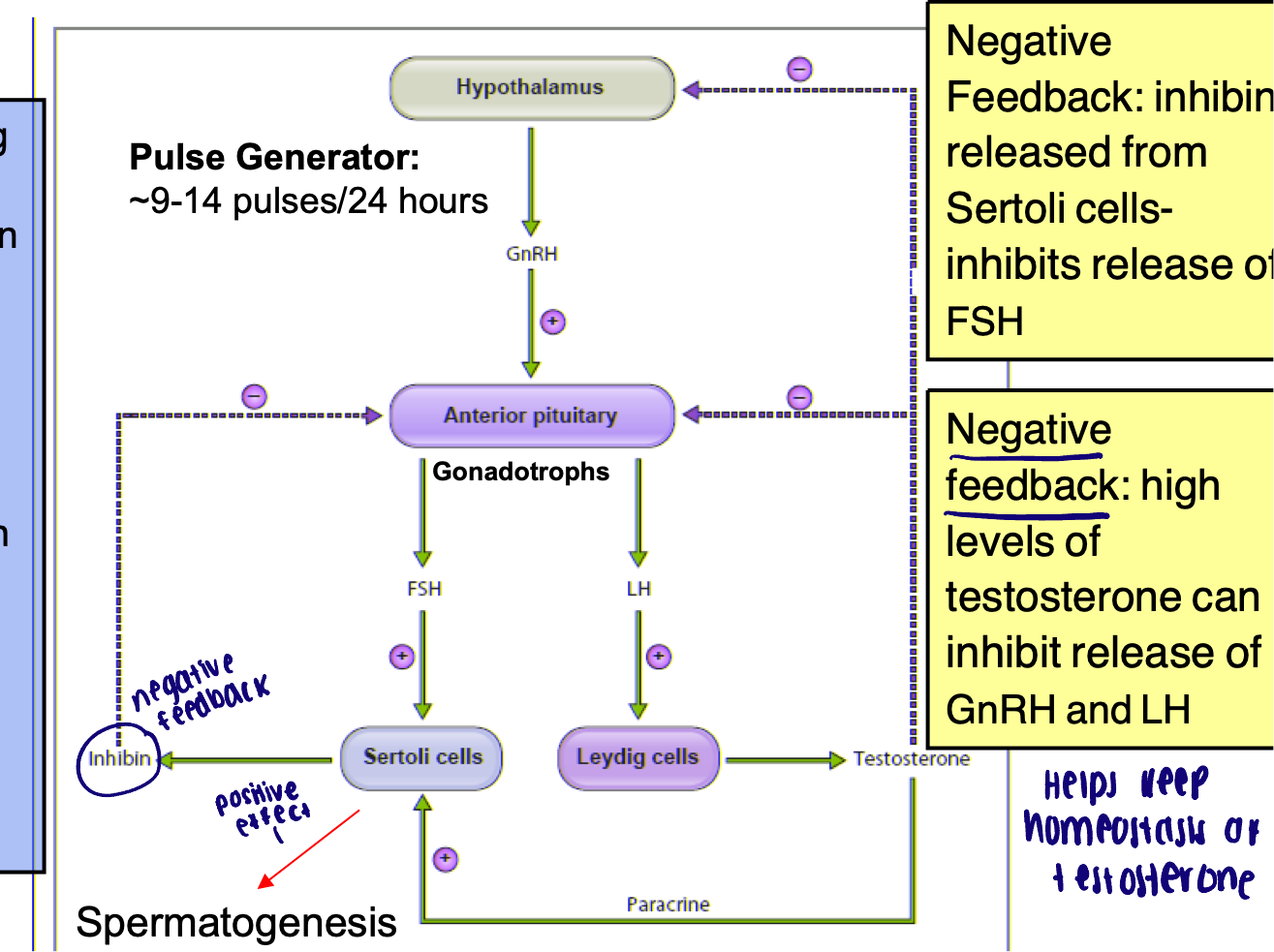
HPG axis → GnRH
Gonadotropin releasing hormone
Released in pulsatile fashion at onset of puberty
HPG axis → FSH
Follicle stimulating hormone
Receptors on Sertoli cells
Alter Sertoli cells to assist in spermatogenesis
HPG axis → LH
Luteinizing hormone
Receptors on Leydig cells
Stimulate testosterone production
HPG axis → negative feedback
Inhibin released from Sertoli cells - inhibits release of FSH
High levels of testosterone can inhibit release of GnRH and LH
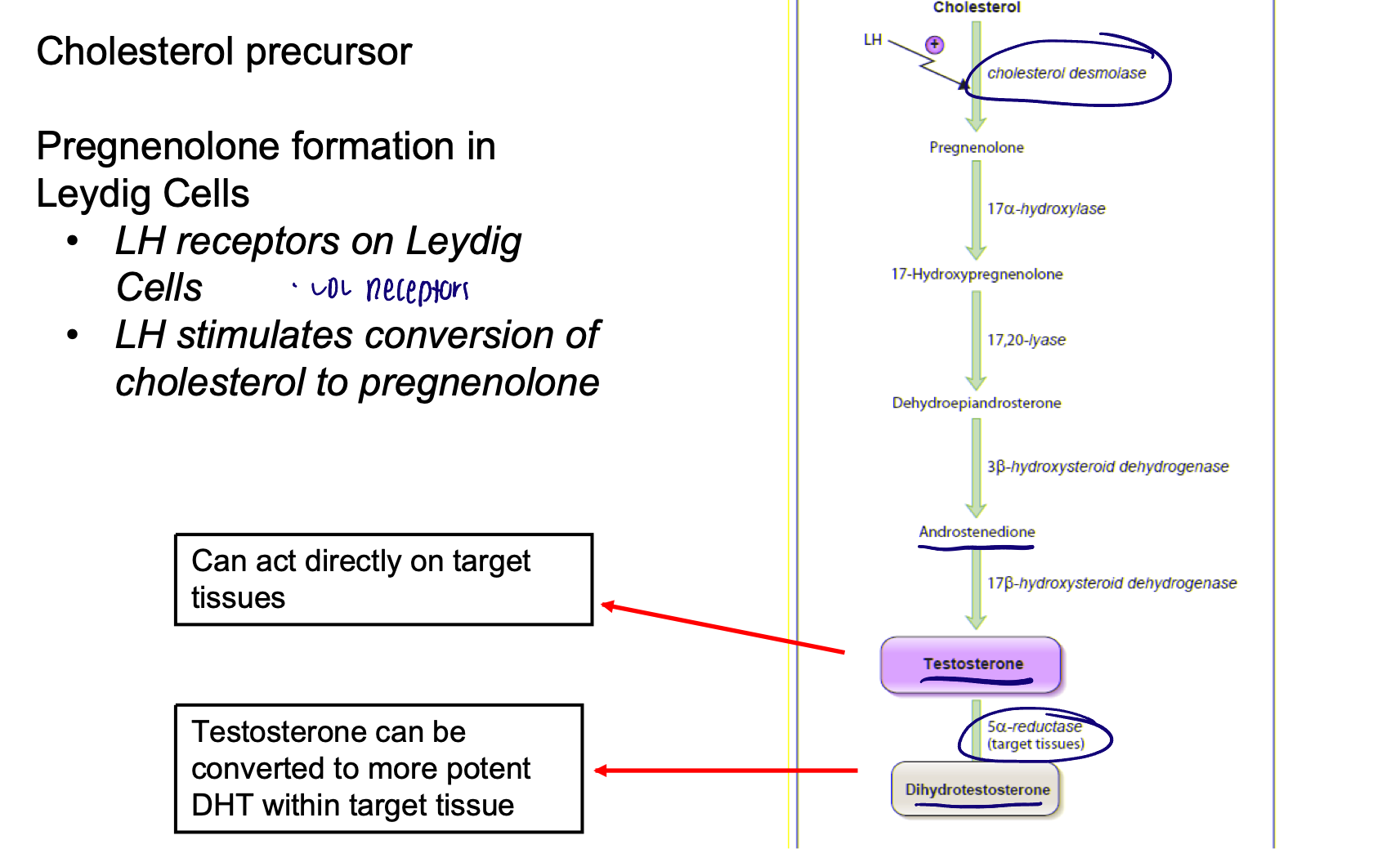
Biosynthesis of testosterone
Cholesterol precursor
Pregnenolone formation in Leydig cells
LH receptors on Leydig cells
LH stimulates conversion of cholesterol to pregnenolone
Both testosterone and DHT exert androgenic effects via androgen receptor (AR)
DHT binds the androgen receptor with much greater affinity than testosterone and is there 50X more potent
Target tissues of androgens
Androgenic: effects of development of internal and external male genitalia spermatogenesis, and libido
Anabolic: growth promotion of somatic tissues
Androgens are important for…
Sexual differentiation
Development/maintenance of male phenotype
Androgens play a role in libido in both men and women
Androgens → increase at puberty
Secondary sexual characteristic
Linear growth
Onset of spermatogenesis
Anabolic steroids
Exogenous androgens
Increased skeletal muscle mass
Decreased adipose
Decreased sperm production and testicular volume (inhibit HPG)
Acne
Liver tumors
Depression
Hypertension
Spermatogenesis
A continual process from the onset of puberty and throughout lifespan of the male
It takes approximately 64 days for one full cycle of spermatogenesis to complete
Around 2 million spermatogonia begin process each day
Anatomy of spermatozoa
Head
Location of nucleus
Acrosome: packet of enzymes necessary for fertilization of ova
Midpiece → mitochondria arranged in spiral around microtubules
ATP for tail movement
Tail → flagellum
Whip like motion to propel sperm
Maturation of spermatozoa
Immature spermatozoa (lack locomotion and ability to fertilize) detach from nurse cells and move along lumen (via villa) of seminiferous tables to epididymis
Epididymis
Includes head, body, and tail (23 ft long)
Storage and maturation of sperm (3 weeks)
Peristaltic smooth muscle movements and cilia
Recycle function for damaged/unused sperm
Capacitation
Develop mobility and ability to fertilize
Requires mixing with seminal fluid secretions and secretions from the female uterus
Spermatic cord
Extends from the abdominopelvic cavity to the testes (inguinal canal)
Layers of fascia and muscle surrounding: blood vessels, nerves, lymphatics, ductus deferens
Vas deferens (ductus deferens)
Tube (18 inches long) carries sperm and mixes it with seminal secretions
Begins at the tail of the epididymis
Thick layers of smooth muscle control movement via peristaltic waves
Travels the spermatic cord
Branches posterior to bladder and curves inferiorly behind bladder
Ampulla: enlargement of the lumen that occurs prior to prostate (sperm can be stored here)
The two ductus deferens converge (with the duct of the seminal gland) to form the short ejaculatory duct
This duct penetrates the prostate and empties into the (prostatic) urethra
Accessory glands
Seminal vesicles
Prostate
Bulbourethral gland (Cowper’s gland)
Seminal vesicles
Paired glands at posterior surface of bladder
Alkaline secretions contain:
Fructose → used to generate ATP
Prostaglandins → influence smooth muscle contractions
Clotting factors → fibrinogen/activators
Prostate
Glandular tissue surrounded by smooth muscle
Secretions include:
Antibiotics
Anti-coagulates → break down fibrin
Bulbourethral glands (Cowper’s gland)
Paired glands at base of penis
Thick alkaline, mucus secretion (buffer)
Lubricate glans of penis
What makes up semen
Spermatozoa + secretions from accessory glands (spermatozoa is less than 5% of total volume of semen)
General functions of accessory gland secretions
Capacitation
Provide nutrients
Provide a medium for movement
Buffers to counteract acidity of urethra/vagina
Parts of the penis
The root
The body
The glans
Erectile tissue
Dorsal vein, dorsal artery and dorsal nerve runs along the dorsal side of penis
The root of the penis
Internal
Fixed end of the penis which attaches it to the body wall
The body of the penis
Mobile tubular portion
Skin and darts muscle continuation of scrotum
The glans of the penis
Extended distal end surrounding the urethral orifice
Prepuce: foreskin, surround and cover the glans
Sebaceous glands secrete smegma (oily mixture and collected dead cells)
Erectile tissue in the penis
Consists of interconnected vascular channels that have walls composed of smooth muscle and elastic fibers
Corpus cavernosa; two lateral columns of erectile tissue which each surround a central artery
Corpus spongiosum; column of article tissue that surrounds penile urethra
Flaccidity
(Non-erect state) is maintained through constriction of arteries to the penis and contraction of the muscular partitions of the erectile tissue
Smooth muscle is actively contracting
Relax smooth muscle for erection → remove Ca2+
Erection
Regulated by the parasympathetic nervous system
Parasympathetic postganglionic neurons of the penis contains the enzyme (neural) nitric oxide synthase (nNOS)
Activation of parasympathetic nerves - increased production and release of nitric oxide
Nitric oxide diffuses into smooth muscle of corpus cavernosa and corpus spongiosum
Initiates signaling cascade which decreases levels of intracellular calcium
Smooth muscle relaxes
Also diffuse into penile arteries - vasodilation (increase local blood flow to penis)
Emission
Movement of semen into prostatic urethra from the ejaculatory duct
Mediated by the sympathetic nervous system: smooth muscle contraction in response to norepinephrine release (alpha1 receptors)
Ampulla of ductus deferens: delivery of sperm
Seminal vesicles: addition of secretions
Prostate: addition of secretions
Internal urethra sphincter (prevent retrograde flow of sperm into bladder)
Ejaculation
Expulsion of semen into the urethra
Triggered by the movement of semen into the urethra at the base of the penis
(Most of the mechanics not well understood) increased firing of efferents from spinal cord stimulate involuntary rhythmic contractions of striated musculature of the perineum (from coccyx to pubic symphysis) to help forcefully expel semen from urethra
“Point of no return” - ejaculation is inevitable
Tightly linked to orgasm
Sexual response cycle
Similar events in both males and females
Excitement
Plateau
Orgasms
Resolution
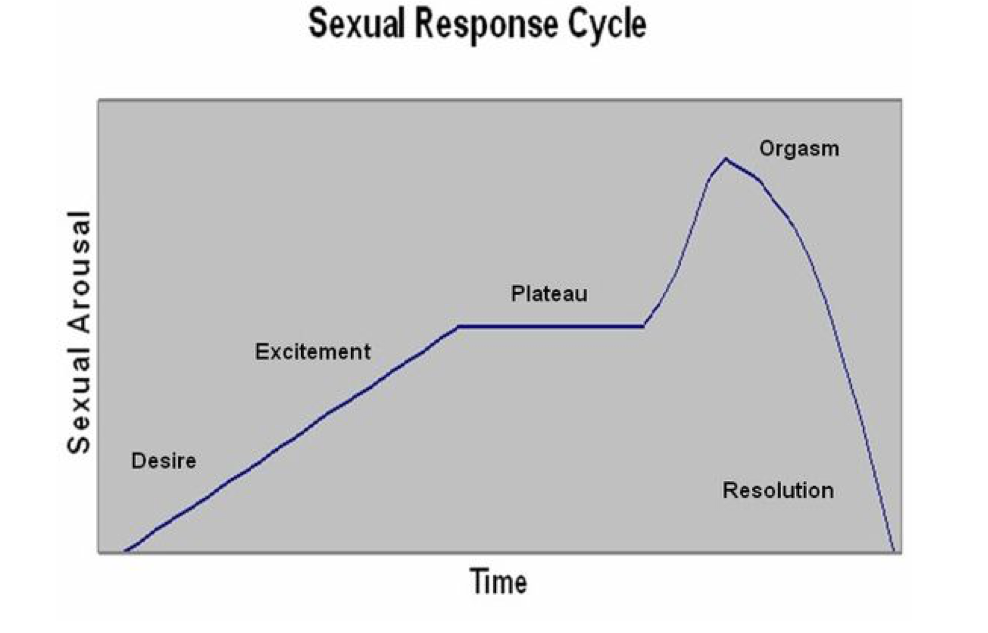
Excitement
Increased heart rate and muscle tension
Lubricating secretions
Increased blood flow: penile, clitoral, vestibular bulb erecetion
Plateau
Amplification of excitement phase and increases in blood flow
Muscle spasms
Emission in males
Orgasm
Involuntary muscle contraction
Vaginal contractions
Ejaculation in males
Forceful relaxation of sexual tension
Resolution
Fatigue and return to normal functioning
Male specific refractory period: time which another erection cannot be initiated
Fertilization
Fusion of a secondary oocyte and a sperm to create a zygote
At ovulation: oocyte surrounded by a layer of follicle cells known as the corona radiata (granulosa cells)
Enzymes in the acrosome of the sperm break down connections between cells of the corona radiata (requires enzymes with dozens of sperm)
A single sperm makes contact with sperm receptors on the plasma membrane of the oocyte
Membranes of sperm and oocyte fuse (directed by enzymes)
Activation of the oocyte
Fusion triggers Na+ influx: depolarization
Release of Ca2+ stores from the SER
Inactivation of sperm receptors
Completion of meiosis II
Creation and then fusion of male and female pronuclei