Final Revision Sheet
1/93
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
Immune tolerance
Ability to prevent immune response against host’s cells/tissues.
Central tolerance
Eliminates self-reactive lymphocytes in primary lymphoid organs
Peripheral tolerance
Eliminates self-reactive lymphocytes in secondary lymphoid organs/peripheral tissues
Commponents of peripheral tolerance
Tregs, clonal anergy, peripheral detection
Anergy
Functional inactivation of lymphocyte due to lack of co-stimulation (needed for complete activation and differentiation)
True or false: Self antigens induce the expression of co-stimulatory proteins
False
Molecular mimicry
Foreign substance with similar proteins to host causes cross-reaction
Neoantigens
Novel antigens found on cancer cells from genetic mutations, unique to tumour
Sequestered antigens
Hidden from immune system to prevent response against them, often in immunologically privileged areas
Epitope spreading
Immune response expands to include other epitopes released from tissue damage
Autoimmunity
Failure of immune mechanisms to eliminate self-reactive cells
Acute inflammation is an immediate __ response aiming to __, and mainly consists of _. It’s usually resolved when the _ is removed, leading to tissue _ and ___.
Chronic inflammation is a __ response that can be due to persistence of _ or failure of ___, and mainly consists of _, lymphocytes, and __. Chronic inflammation often results in tissue _ and ___.
short-term, clear stimulus, neutrophils, stimulus, repair, restoration of function, long-term, stimulus, acute inflammatory response, macrophages, plasma cells, damage, loss of function
Components of acute inflammation
Vasodilation, increased vascular permeability, migration of leukocytes/recruitment of cells
Cardinal signs of acute inflammation
Rubor, calor, tumor, dolor, functio laesa
What causes rubor and calor?
Vasodilation
What causes tumor?
Increased vessel permeability and fluid leakage
What causes dolor?
Chemical mediators stimulating nerve endings e.g. prostaglandins
Functio laesa is a consequence of…
Tumor and dolor
Immune response
Body’s defence mechanism to harmful substances/those not recognised as host’s own constituent
The primary antibody response is the initial reaction to a new antigen and is _ and _, with a longer _ period and lower peak _ levels and _. It is initated by _ and mainly produces _ antibodies.
The secondary antibody response is a _, _, more _ reaction upon _ to the antigen. It has a __ period and higher peak __ and _. It is _ initiated by ___ and mainly produces _ antibodies due to the presence of these.
slow, weaker, latent, antibody, affinity, naive B cells, IgM, faster, stronger, prolonged, re-exposure, shorter latent, antibody levels, affinity, memory B cells, IgG
Serology
In-vitro study of blood serum and its components to detect antigens or antibodies
Uses of serological tests
Diagnosis of disease, treatment evaluation, prognosis, quantitation of antigen and antibody
Polyclonal antibody production for lab use
Generated in animals by different B cell clones, produced as defence mechanism by plasma B cells when exposed to antigen
Monoclonal antibody production for lab use
Produced by a single clone of plasma B cells using hybridoma cell technology and mouse myeloma cell lines
Monoclonal antibody production steps
B cell and myeloma cell fusion, HAT medium selection, screening, antibody production
Hybridoma
Antibody-producing tumour cells; produce many copies of same antibody and grow easily in the lab
Hybridoma role
Large-scale monoclonal antibody production
Ouchterlony technique
Qualitative technique demonstrating double diffusion in two dimensions
Total identity
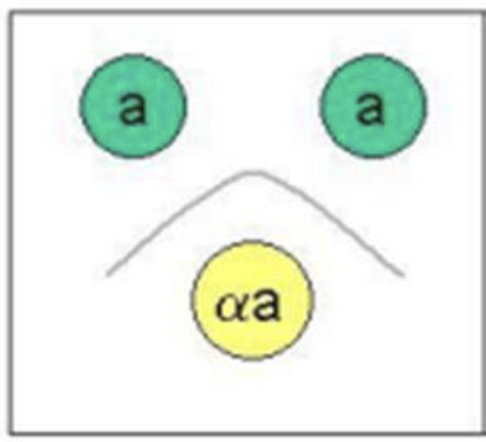
Partial identity

Non-identity

Single diffusion, one dimension
Oudin Procedure
Single diffusion, two dimensions
Radial immunodiffusion (Mancini technique)
Double diffusion, one dimension
Oakley-Fulthrope procedure
Direct Coomb’s test
Detects antibodies/complements already bound to RBCs
Direct Coomb’s test steps
RBCs washed to remove unbound antibodies, tested with anti-human globulin reagent, agglutination observed
Direct Coomb’s test use
Diagnosing autoimmune conditions, haemolytic disease, transfusion reactions
Indirect Coomb’s test
Detects antibodies free in serum, unattached to RBCs
Indirect Coomb’s test steps
Serum mixed with RBCs of known antigen type, agglutination observed
Indirect Coomb’s test use
Checks for antibodies that could cause reaction with RBCs; cross-matching for transfusions, prenatal screening
The complement fixation test detects the presence of ___ by observing whether a _ amount of complement is _ to an antigen-antibody _
specific antigens or antibodies, known, bound, complexes
Complement fixation test: Fixation phase
Serum + specific antigen, complement added
In the complement fixation test, the complement will only be fixed if…
both antigen and antibody are present
Complement fixation test: Detection phase
Sensitised sRBCs added, if complements unbound haemolysis occurs
Monoclonal antibodies are a _ population of antibodies, produced by ___ of plasma B cells.
homogeneous, a single clone
Monoclonal antibody specificity
Highly specific for a single epitope on an antigen
Monoclonal antibody production is…
consistent across batches(high reproducibility), expensive
Monoclonal vs polyclonal antibody sensitivity
Monoclonal: moderate
Polyclonal: high
Polyclonal antibodies are a __ of antibodies, produced by ___.
heterogeneous mixture, different B cell clones
Polyclonal antibody specificity
Lower specificity, bind to same antigen but possibly different eptitopes
Polyclonal antibody production is…
cheap, varies across batches (low reproducibility)
Control
Benchmark with known value or property, processed alongside patient samples
Controls ensure _ and _ of results and provide a ___. They can detect issues that could lead to __.
accuracy, reliability, point of comparison, false results
Precipitation is…
2 soluble reactants join to make 1 insoluble product
Formation of lattices
Soluble antigen type (proteins, toxins)
Agglutination is…
Development of ag-ab complexes in the form of particle clumps
Lattices of polyvalent antigens
Particulate antigen type (cells, beads)
Which immunoglobulin is a particularly good agglutanin? Why?
IgM, pentamer shape = high avidity
Factors affecting rate of diffusion in a precipitation reaction
Temperature, molecular size, gradient, viscosity of medium, distance and surface area
Factors affecting rate of diffusion in a precipitation reaction:
Temperature
Higher = faster
Lower = slower
Factors affecting rate of diffusion in a precipitation reaction:
Molecular size
Larger = slower
Slower = faster
Factors affecting rate of diffusion in a precipitation reaction:
Viscosity of medium
Higher = slower
Lower = faster
Zone of antibody excess
Prozone
Initial, insufficient antigen for visible lattice formation
Zone of equivalence
Optimal ag-ab itneraction, maximal precipitation
Zone of antigen excess
Postzone
Precipitation declines
Precipitin curve: To achieve the optimal ratio…
antigen is slowly added to antibody solution
Components of complement fixation test
Patient serum, known antigen, complement source, indicator system
ELISA principle
Binding target analyte to labelled particle, producing measurable visible signal
Direct ELISA
Enzyme-labelled primary monoclonal antibody binds to antigen
Enzyme reacts with substrate to produce signal
Indirect ELISA (compared to direct)
Labelled secondary antibody binds to unlabelled primary antibody
Sandwich ELISA
Antigen bonded between capture antibody on well floor and labelled detection antibody
Competitive ELISA
Antigen competes with labelled antigen for antibody binding
Labelled secondary antibodies produce inverse signal
Fluorescent Immunoassay (FIA)
Fluorescent-labelled antibodies used for detection
Radioimmunoassy (RIA)
Radioactive isotopes used for sensitive antigen detection
Neutralisation
Binding antibody to epitopes/soluble molecules to inhibit thier ability to bind to host cells
Cell flow cytometry
Fluorescent-labelled cells pass through laser in single stream
Physcial and chemical properties are measured
Nephelometry
Light passes through soln. with suspended particles
Light scatters upon contact
Intensity of scattered light is measured
Turbidimetry (compared to nephelometry)
Intensity of light that passes through (not scattered) is measured
What types of antigens can be used in neutralisation tests?
Viruses (whole or parts), bacterial toxins, viral proteins
Cell flow cytometry: Forward-scatter (FSC)
Light scattered in forward direction (very slight angle from laser beam)
Cell flow cytometry: Side-scatter (SSC)
Light scattered at 90º angle to laser beam
SSC light is influenced by…
granularity, internal complexity, structure of particle/cell
ELISA: Biotin
Molecular tag, binds to antibodies or other target molecules
ELISA: Streptavidin
Protein with extremely high affinity for biotin
ELISA: Streptavidin and biotin role
Signal amplification
Turbidimetry: Light absorbance
Light absorbed by sample
Turbidimetry: Light transmittance
Light passed through sample
Non-heritable influences affecting immunity
Exposure to microbes, diet, stress, sleep, environment
Heritable influences affecting immunity
WBC counts, cytokine concentration/profiles, variants within cytokine genes and immune-mediated disease
Circadian rhythm
Natural cycle regulating sleep-wake cycle patterns, other physical/mental/behavioural changes
Primary immunodeficiency
Usually genetic and congenital and apparent by 6 months of age when maternally-derived antibodies disappear
Primary immunodeficiency example
Severe Combined Immunodeficiency (SCID)
Secondary immunodeficiency
Usually caused by environment and may occur at any time in life
Secondary immunodeficiency possible causes
Infection, therapeutic treatments, cancer, malnutrition
Secondary immunodeficiency example
Acquired Immunodeficiency Syndrome (AIDS)
Most common clinical characteristics of immunodeficiency
Recurrent/chronic infections
Inability to clear infectious agents after standard antibiotic therapy
Unusual infectious agents