Homeostasis: control of blood water potential
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
17 Terms
Define osmoregulation
Control of blood water potential via homeostatic mechanisms
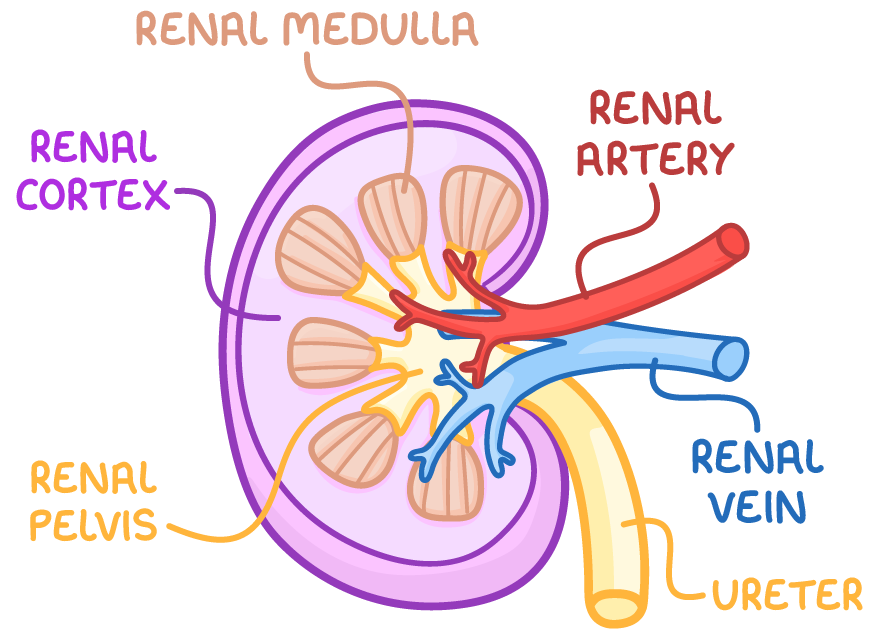
Describe the gross structure of a mammalian kidney
Fibrous capsule: An outer membrane that surrounds and protects the kidney
The renal cortex : outer region consists of Bowman’s capsules, convoluted tubules , blood vessels
The renal medulla : inner region consists of collecting ducts, loops of Henle , blood vessels
The renal pelvis: cavity collects urine into the ureters
Describe the structure of a nephron
Bowman's capsule (renal capsule) - This surrounds a capillary ball known as the glomerulus, from which filtrate is formed, and contains cells called podocytes in its inner layer.
Proximal convoluted tubule (PCT) - This section reabsorbs useful substances, including water, glucose, and salts, into surrounding capillaries and the epithelial cells in its wall have microvilli to increase their surface area.
Loop of Henle - This long, hairpin loop extends from the cortex into the medulla and then back into the cortex, and creates a high solute gradient in the medulla, helping with the reabsorption process.
Distal convoluted tubule (DCT) - This part fine-tunes the water balance by reabsorbing water into surrounding capillaries, influenced by antidiuretic hormone. It is surrounded by fewer capillaries than the PCT.
Collecting duct - This tube collects filtrate from multiple nephrons and further fine-tunes the water balance, before the urine formed is passed to the bladder.
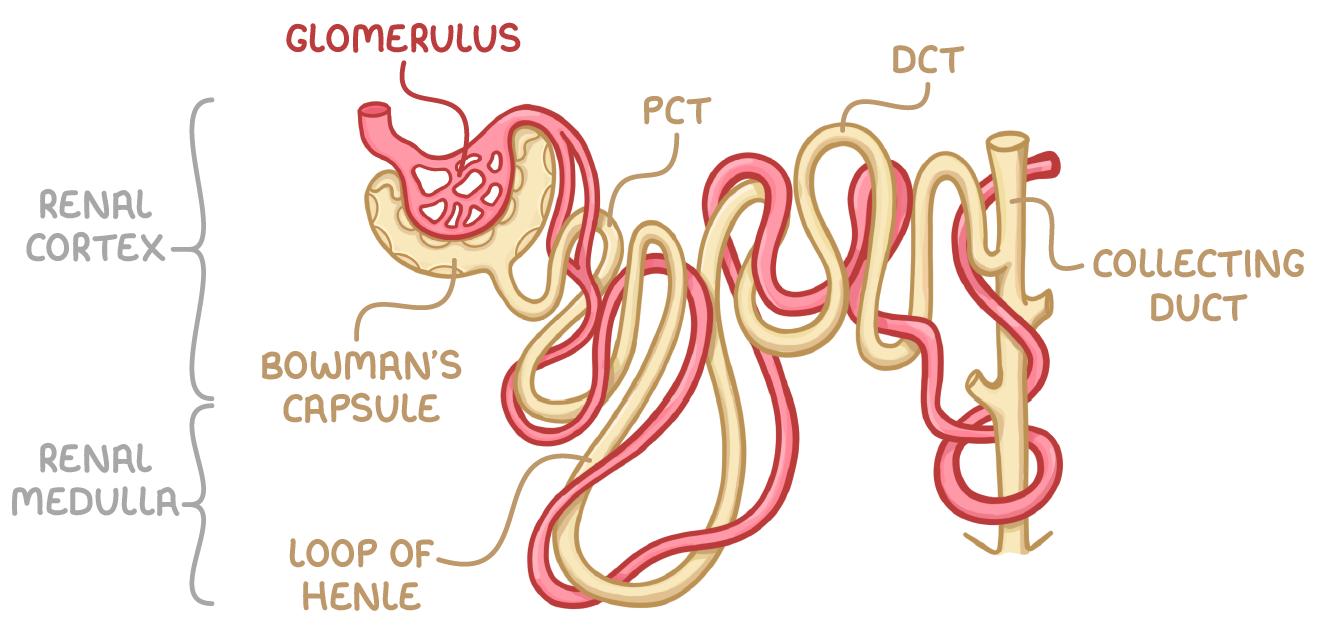
Describe the blood vessels associated with a nephron
Wide afferent arteriole from renal artery enters renal capsule and forms glomerulus: branched knot of capillaries which combine to form narrow efferent arteriole
Efferent arteriole branches to form capillary network that surrounds tubules
Explain how glomerular filtrate is formed
Ultrafiltration in Bowman’s capsule
High hydrostatic pressure in glomerulus forces small molecules (urea , water , glucose and mineral ions) out of the capillary fenestrations AGAINST osmotic gradient
Basement membrane acts as filter. Blood cells & large molecules e.g large proteins remain in capillary
How are cells of the Bowman’s capsule adapted for ultrafiltration
Fenestrations between epithelial cells of capillaries
Fluid can pass between and under folded membrane of podocytes
Stats what happens during selective reabsorption and where it occurs
Useful molecules from glomerular filtrate e.g glucose are reabsorbed into blood
Occurs in proximal convoluted tubule
Outline the transport processes involved in selective reabsorption
Sodium ions (Na+) are actively transported into blood capillaries, reducing the Na+ concentration in epithelial cells lining the PCT.
Na+ moves from the PCT lumen into the epithelial cells, down its concentration gradient.
Na+ is co-transported with substances like glucose and amino acids into the epithelial cells.
These reabsorbed molecules can then diffuse into blood capillaries.
How are cells in the proximal convoluted tubule adapted for selective reabsorption
Microvilli: large SA for co-transporter proteins
Many mitochondria: ATP for active transport of glutes into intercellular spaces
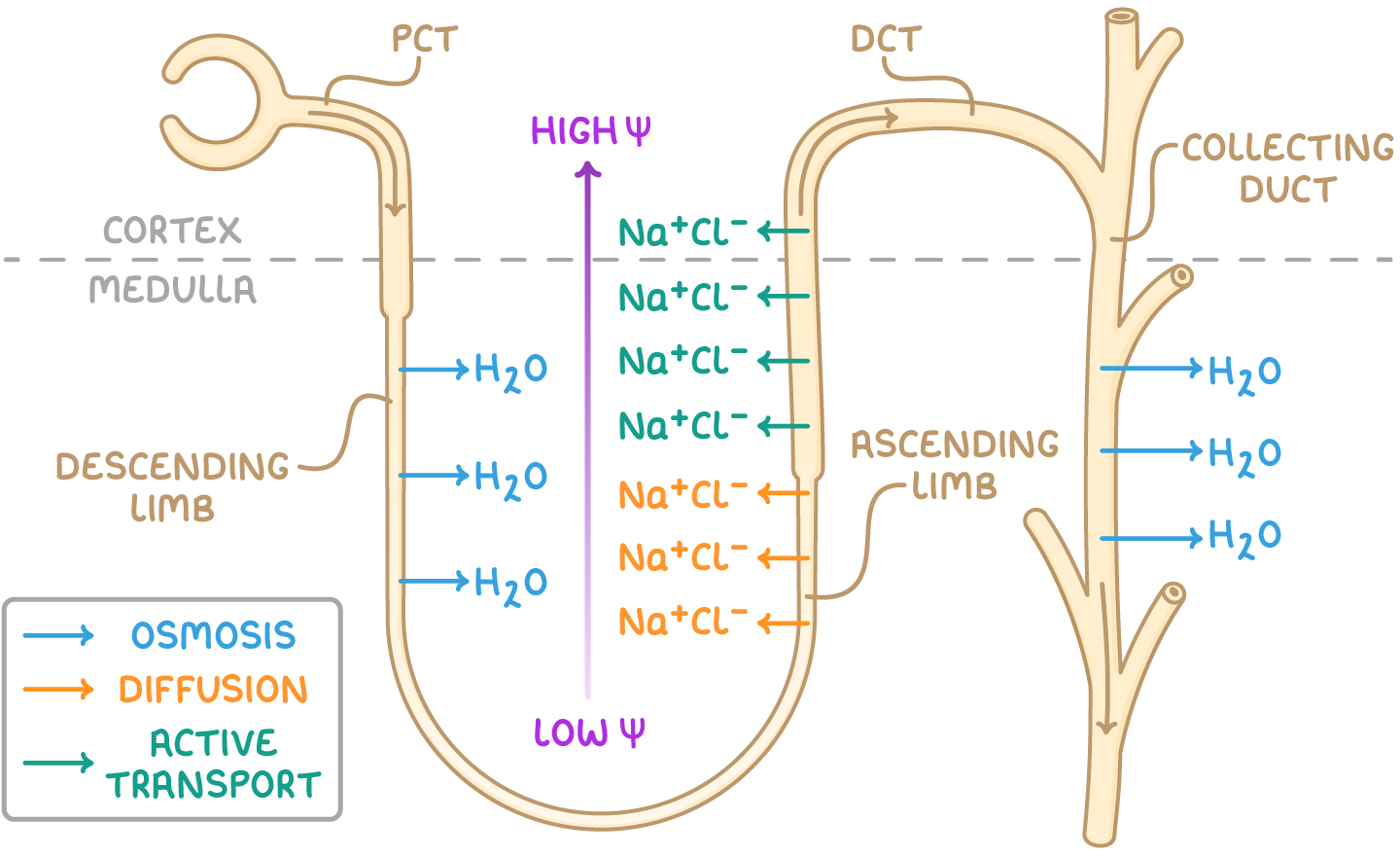
What happens in the loop of Henle
Active transport of Na+ and Cl- out of ascending limb.
Water potential of interstitial fluid decreases
Osmosis of water out of descending limb (ascending limb is impermeable to water)
Water potential of filtrate decreases going down descending limn: lowest in medullary region, highest at top of ascending limb
Explain the role of the distal convoluted tubule
Reabsorption of water via osmosis
Reabsorption of ions via active transport
Permeability of walls is determined by actions of hormones
Explain the role of the collecting duct
Reabsorption of water from filtrate into interstitial fluid via osmosis through aquaporins
Explain why it’s important to maintain an Na+ gradient
Countercurrent multiplier: filtrate in collecting ducts is always beside an area of interstitial fluid that has a lower water potential
Maintains water potential gradient for maximum reabsorption of water
What might cause blood water potential to change
Level of water intake
Level of ion intake in diet
Levels of ions used in metabolic processes or excreted
Sweating
Explain the role of the hypothalamus in osmoregulation
Osmosis of water out of osmoreceptors in hypothalamus causes them to shrink
This triggers hypothalamus to produce more antidiuretic hormone (ADH)
Explain the role of the posterior pituitary gland in osmoregulation
Stores and secretes the ADH produced by the hypothalamus
Explain the role of ADH in osmoregulation
Makes cells lining collecting duct more permeable to water: binds to receptor > activate phosphorylase > vesicles with aquaporins on membrane fuse with cell surface membrane
Makes cells lining collecting duct more permeable to urea: water potential in interstitial fluid decreases. More water re absorbed= more concentrated urine