Week 6: Upper GIT
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
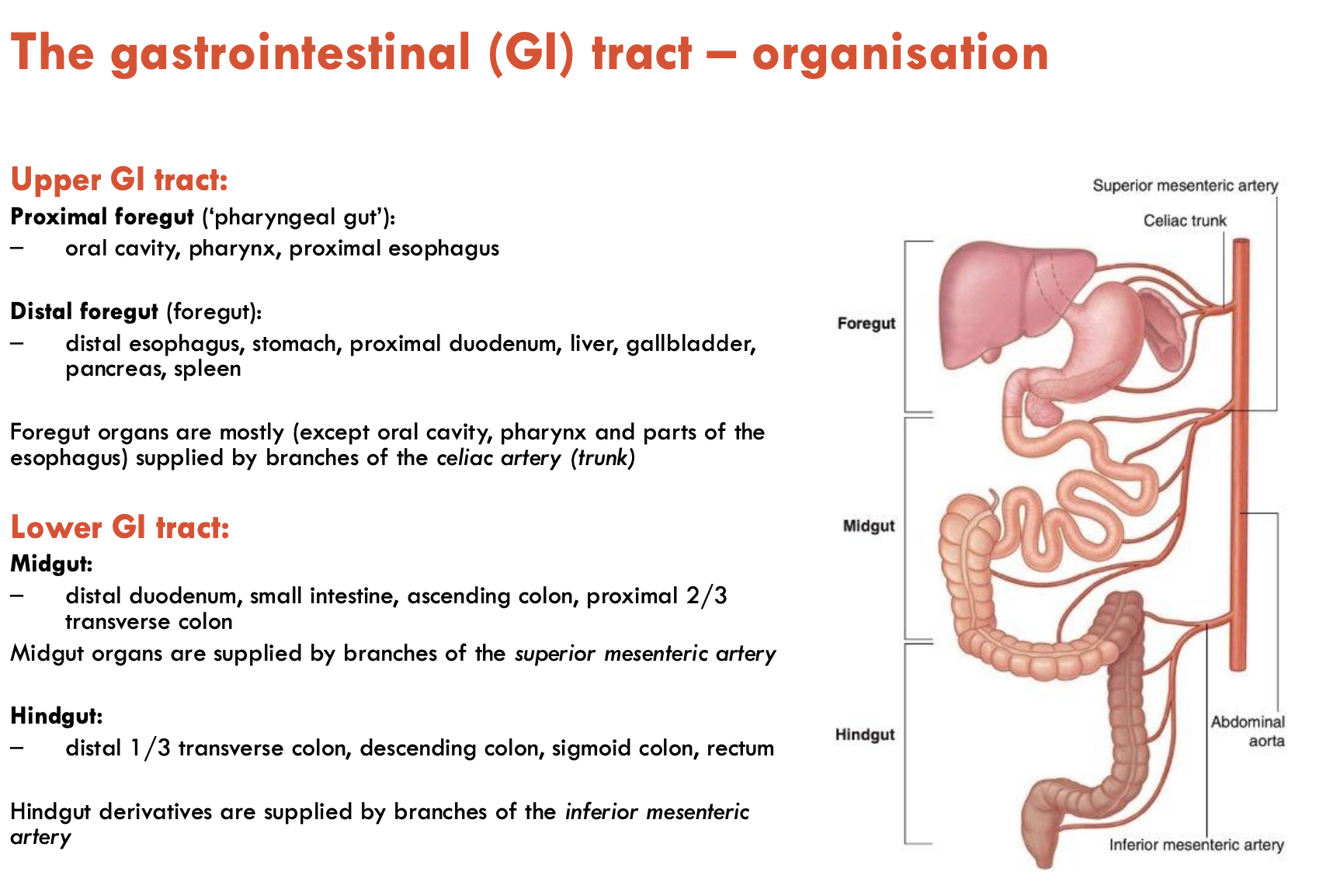
Describe the organisation of the GIT (4)
Upper GIT
Proximal foregut (‘pharyngeal gut’):
oral cavity, pharynx, proximal oesophagus
Distal foregut (‘foregut’)
distal oesophagus, stomach, proximal duodenum, liver, gallbladder, pancreas, spleen
Foregut organs are mostly supplied by branches of the coeliac artery (except oral cavity, pharynx, and parts of the oesophagus)
Lower GIT
Midgut:
distal duodenum, small intestine, ascending colon, proximal 2/3 transverse colon
supplied by branches of sup. mesenteric artery
Hindgut:
distal 1/3 transverse colon, descending colon, sigmoid colon, rectum
supplied by branches of inf. mesenteric artery
List the 3 stages of swallowing
Oral stage
Pharyngeal stage
Oesophagal stage
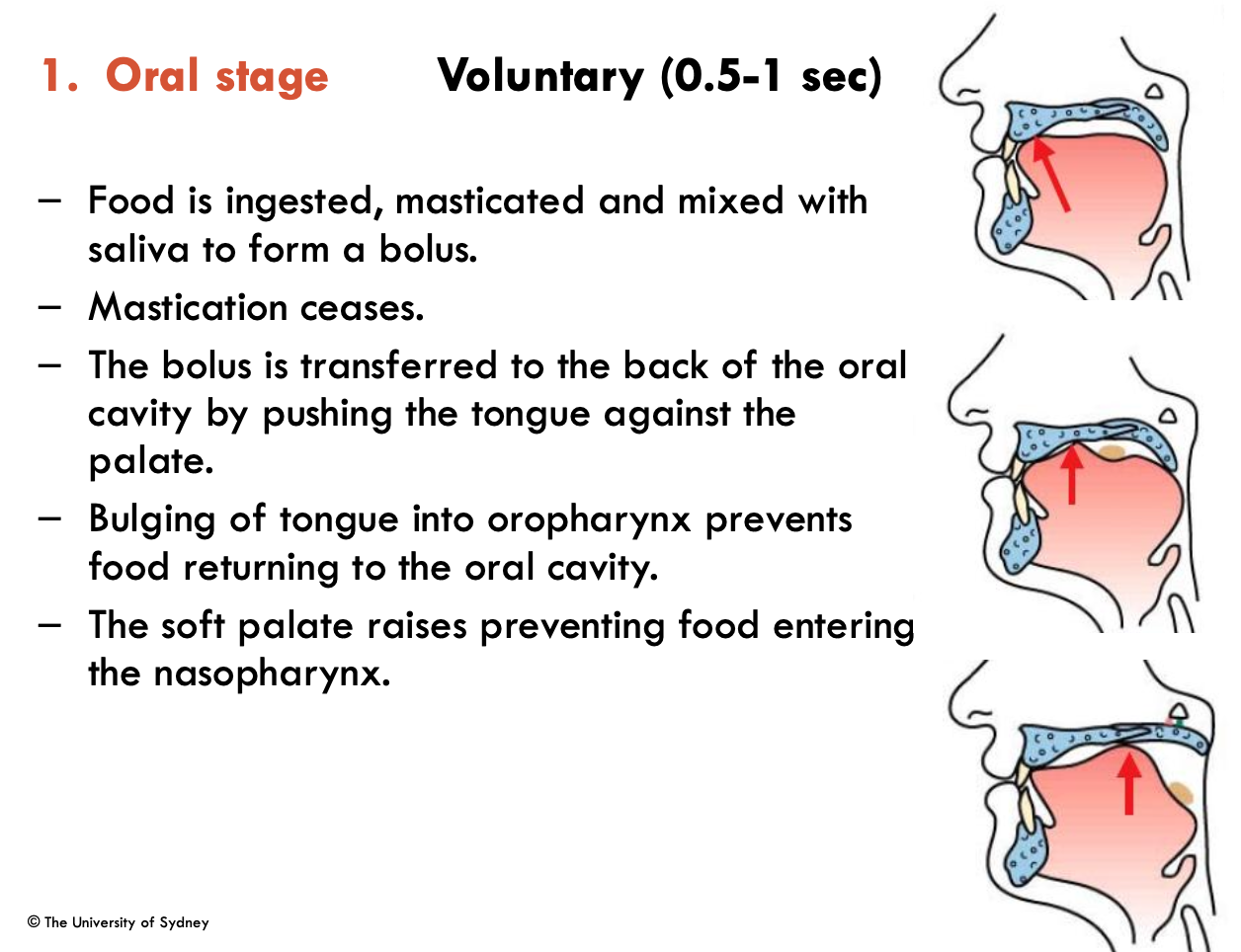
Describe the oral stage of swallowing (5)
Voluntary (0.5-1 sec)
Food is ingested, masticated, and mixed with saliva to form a bolus
Mastication ceases
Bolus is transferred to back of oral cavity by pushing tongue against the palate
Bulging of tongue into oropharynx prevents food returning to oral cavity
Raising of soft palate prevents food from entering nasopharynx
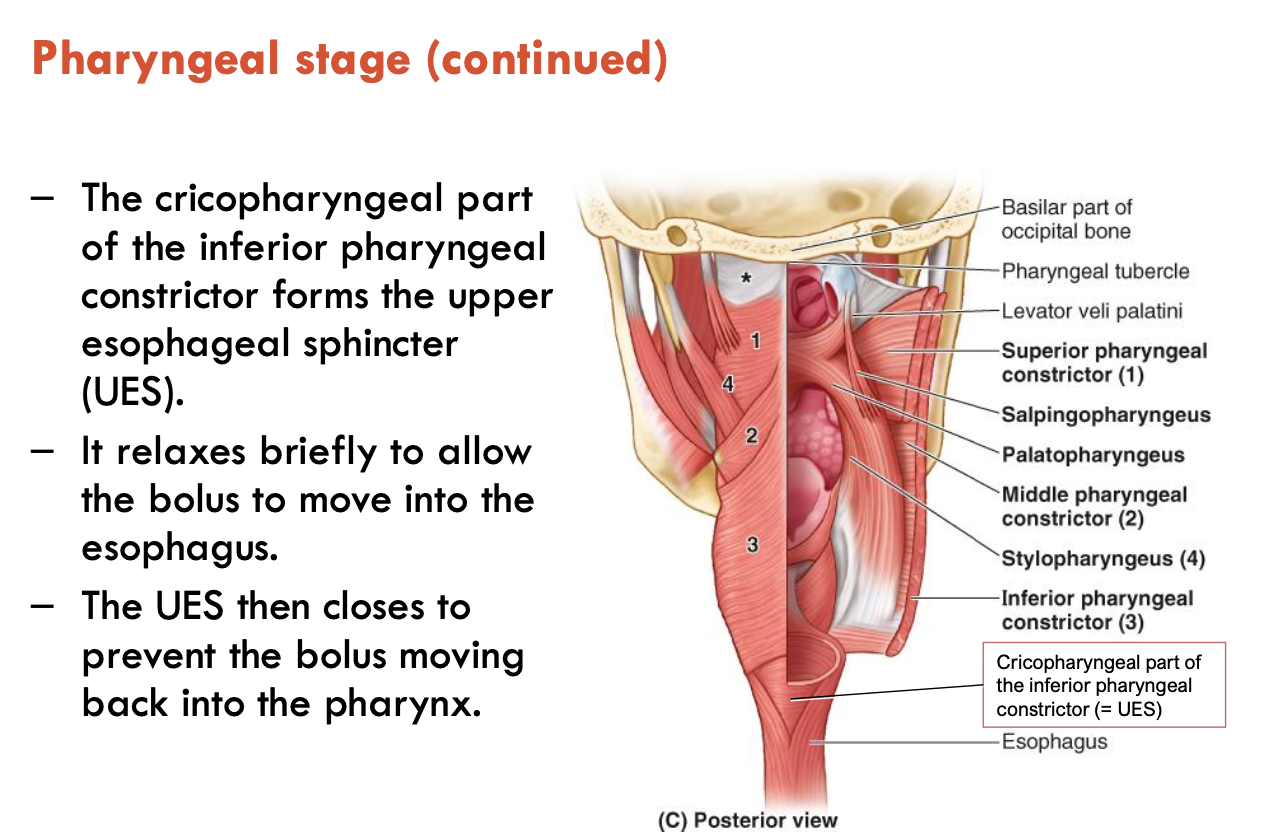
Describe the pharyngeal stage of swallowing (6)
Involuntary (1 sec)
Swallowing reflex is triggered by the bolus, stimulating tactile receptors on the faeces and uvula
Epiglottis is deflected by the food bolus passing over it and by the larynx raising
This closes the larynx, preventing aspiration of food into the airways
The superior, middle, and inferior pharyngeal sphincters contract sequentially
The upper oesophageal sphincter (UES - formed by the cricopharyngeal part of the inf. pharyngeal constrictor) relaxes briefly to allow the bolus to move to the oesophagus
The UES then closes to prevent the bolus from moving back into the pharynx
Describe the oesphageal stage of swallowing (5)
Involuntary (8-20 sec)
Bolus is moved down the oesophagus by peristaltic contractions - involuntary waves of sequential contraction and relaxation of smooth muscle
Epiglottis returns to normal position
The lower oesophageal sphincter (LES) is tonically contracted
LES relaxes briefly during swallowing to allow the bolus to enter the stomach
The LES closes to prevent reflux/regurgitation back into the oesophagus
What is dysphagia?
Dysphagia is a subjective awareness of difficulty or obstruction during swallowing
caused by functional or structural abnormalities of the oral cavity, pharynx, oesophagus, and/or gastric cardia
relatively common (esp. with aging and in women)
fluoroscopy barium swallow study is the main imaging assessment
endoscopy may be used to examine oesophageal mucosa
cross-sectional imaging for further evaluation of masses/humans
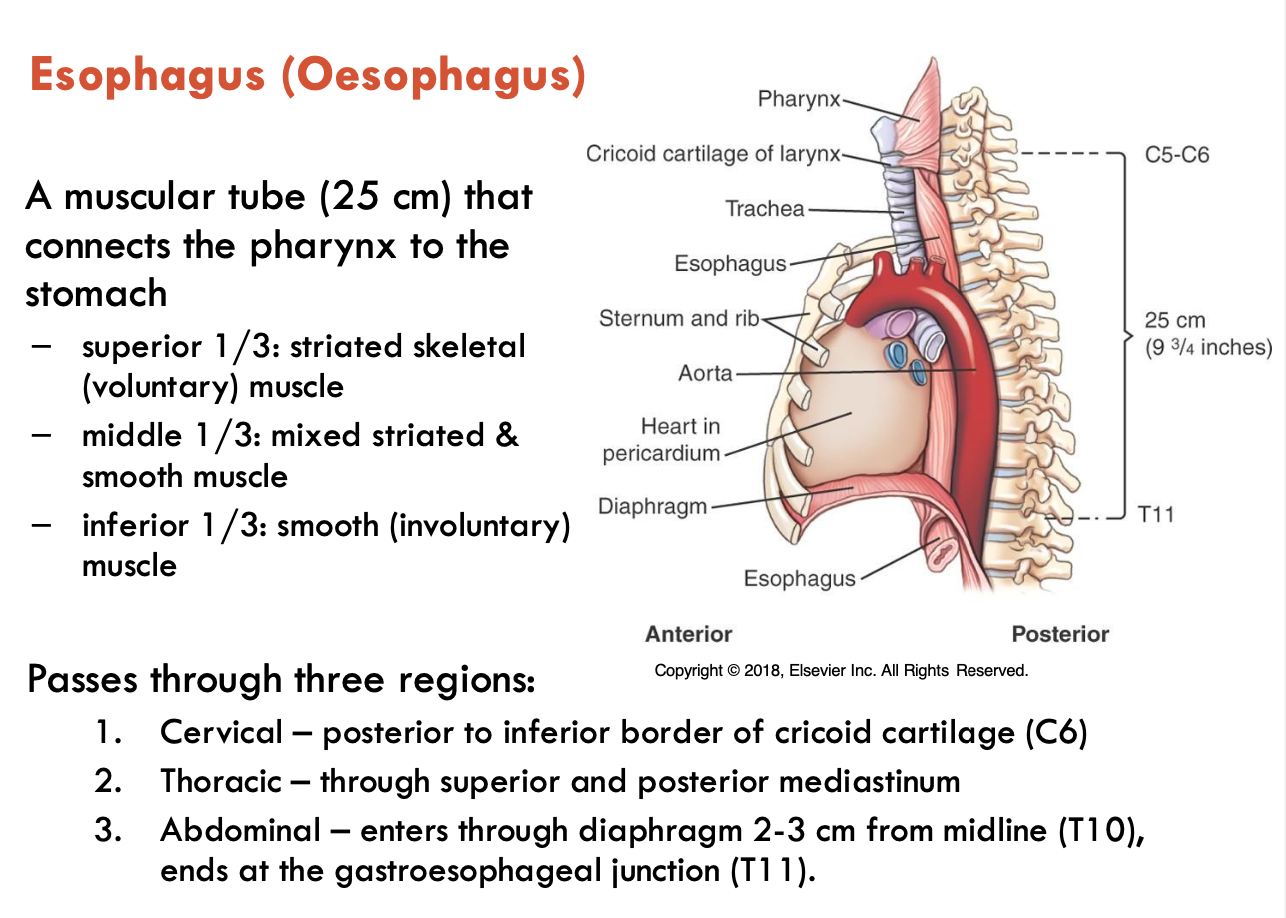
What are the features of the oesophagus?
Oesophagus = muscular tube (25 cm) that connects the pharynx to the stomach
superior 1/3: striated skeletal muscle
middle 1/3: mixed striated & smooth muscle
inferior 1/3: smooth muscle
Passes through 3 regions:
Cervical - posterior to inf. border of cricoid cartilage (C6)
Thoracic - through superior and posterior mediastinum
Abdominal - enters through diaphragm 2-3 cm from the midline (T10), ends at the gastroesophageal junction (T11)
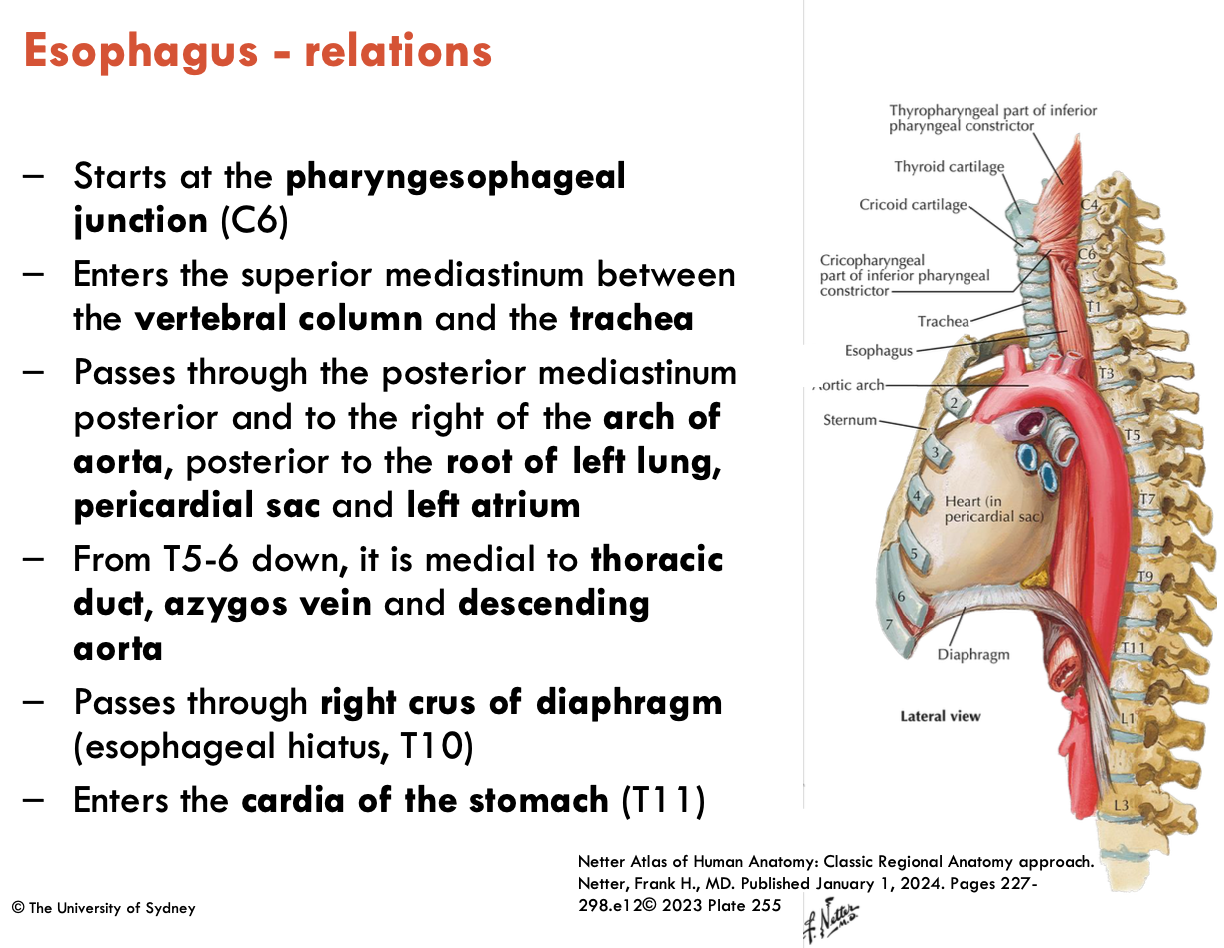
Describe the relations of the oesophagus
starts at the pharyngoesophageal junction (C6)
enters the sup. mediastinum between the vertebral column and the trachea
passes through the post. mediastinum posterior to the right of the aortic arch, posterior to the root of the left lung, pericardial sac, and left atrium
From T5-6 down, it is medial to the thoracic duct, azygos vein, and descending aorta
passes through the right crus of diaphragm (oesophageal hiatus: T10)
enters the cardia of the stomach (T11)
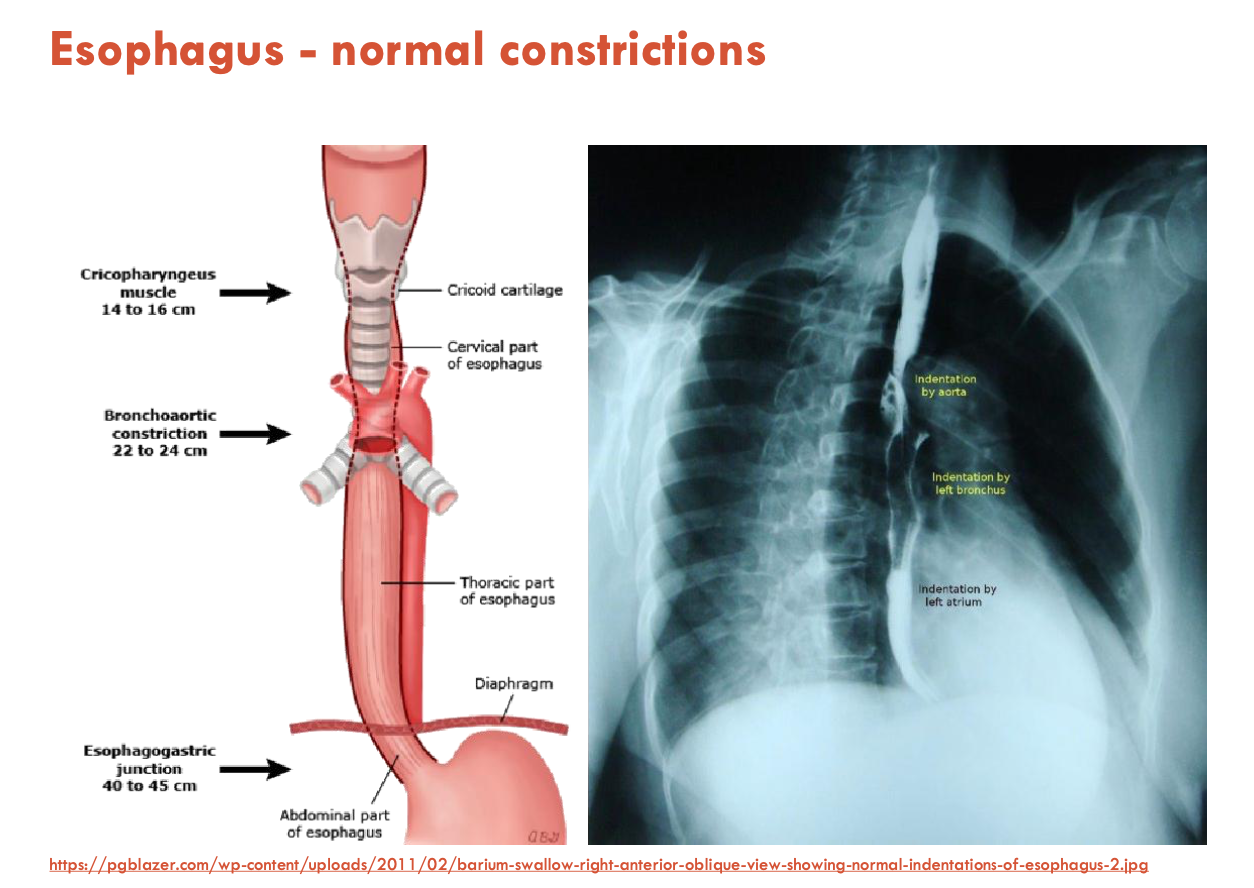
List the normal constrictions of the oesophagus (3)
UES (upper oesophageal constrictor - cricopharyngeal part of the inf. pharyngeal constrictor)
Bronchoaortic constriction
Oesophagogastric junction
Dysphagia can cause abnormality in these constrictions
Describe the blood supply to the oesophagus
Cervical 1/3:
Arterial: inf. thyroid artery
Venous: inf. thyroid veins → SVC
Thoracic 1/3:
Arterial: oesophageal branches of the abdominal aorta
Venous: oesophageal veins → azygos/hemiazygos
Abdominal 1/3:
Arterial: left gastric art. & left phrenic art.
Venous: left gastric v. → portal venous system
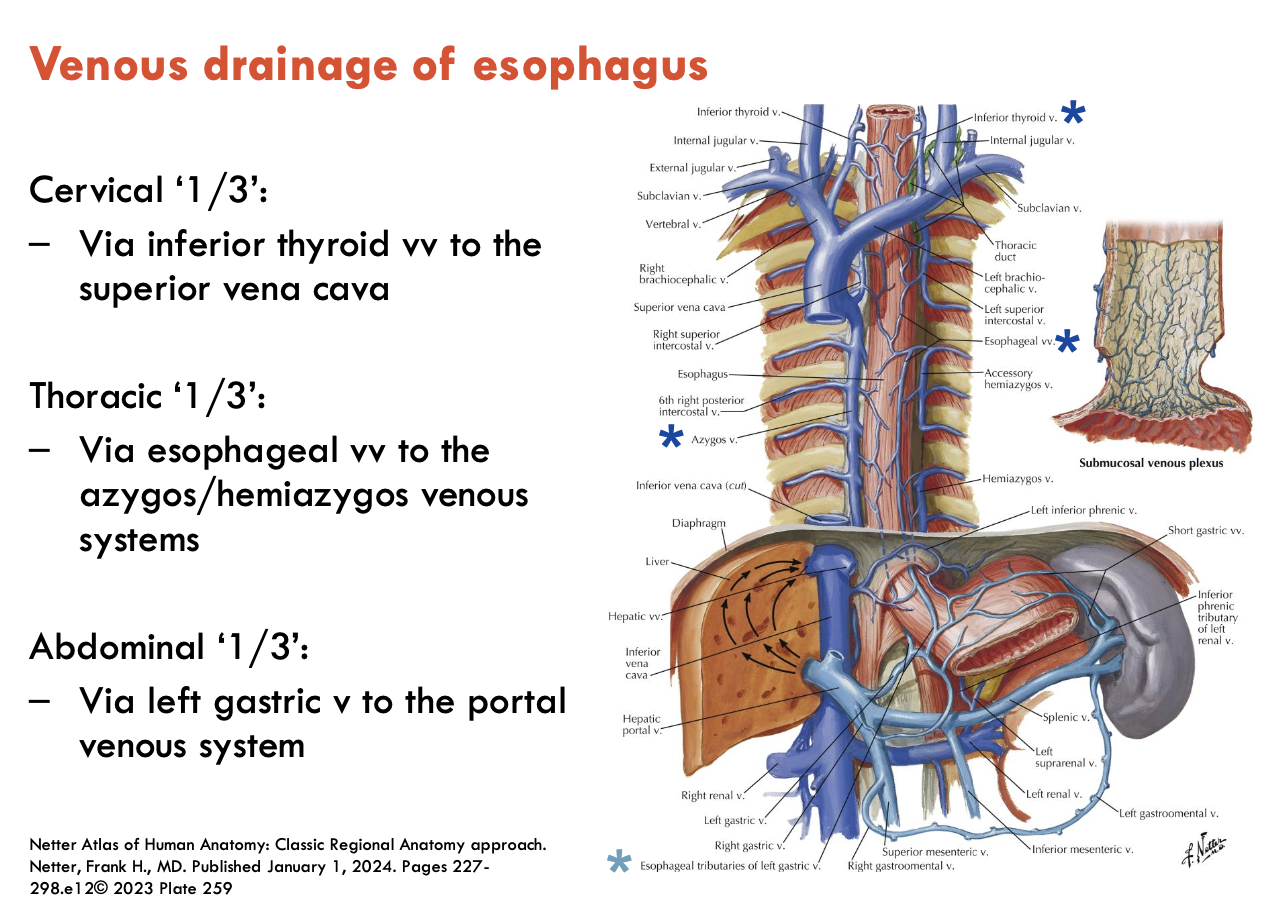
What are oesophageal varices?
Varicose (enlarged) veins around the lower part of the oesophagus
due to portal hypertension often associated w/ liver disease (e.g. cirrhosis)
only lower 1/3 of oesophagus because they contribute to portal vein
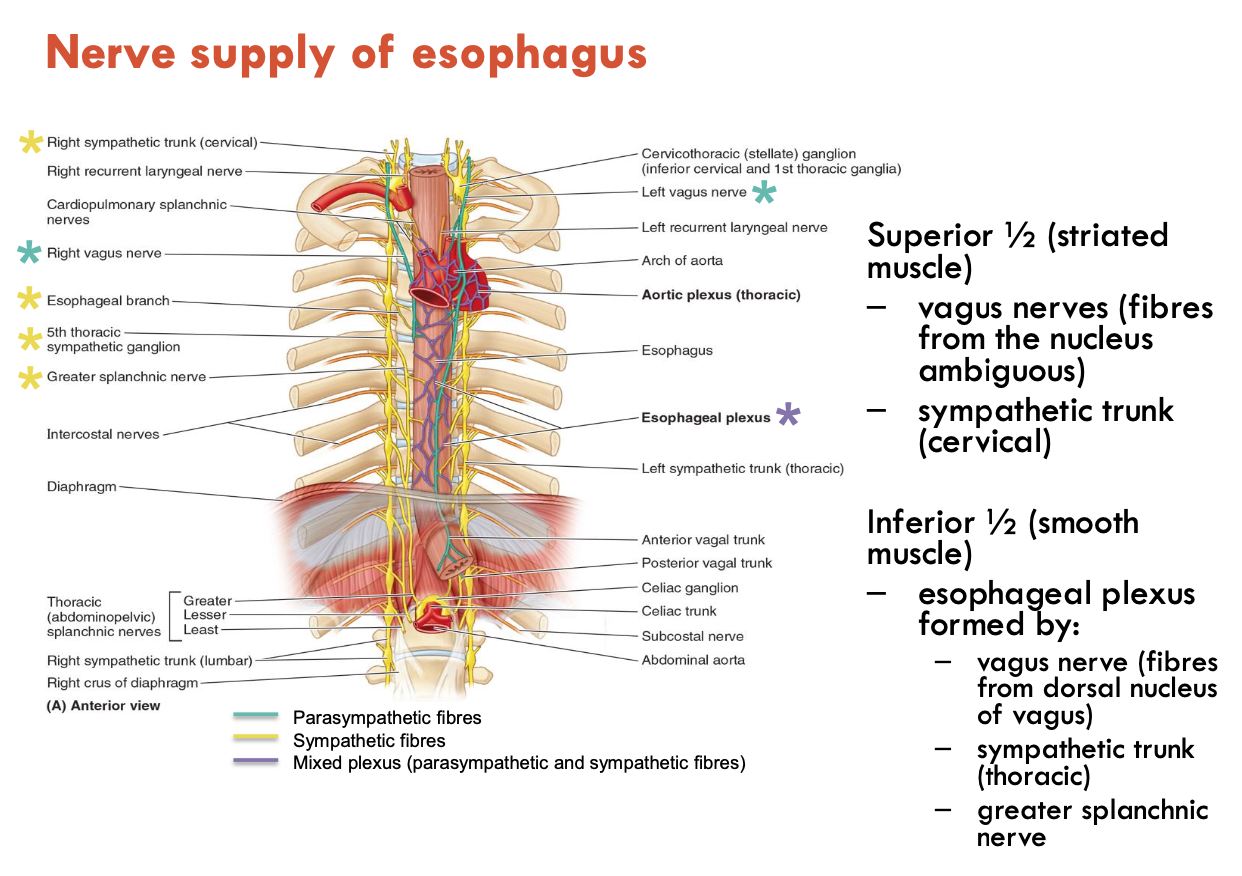
Describe the nerve supply of the oesophagus
Superior ½ (striated muscle):
vagus nerves (fibres from nucleus ambiguus)
sympathetic trunk (cervical)
Inferior ½ (smooth muscle):
oesophageal plexus formed by:
vagus nerve (fibres from dorsal nucleus of vagus)
sympathetic trunk (thoracic)
greater splanchnic n.
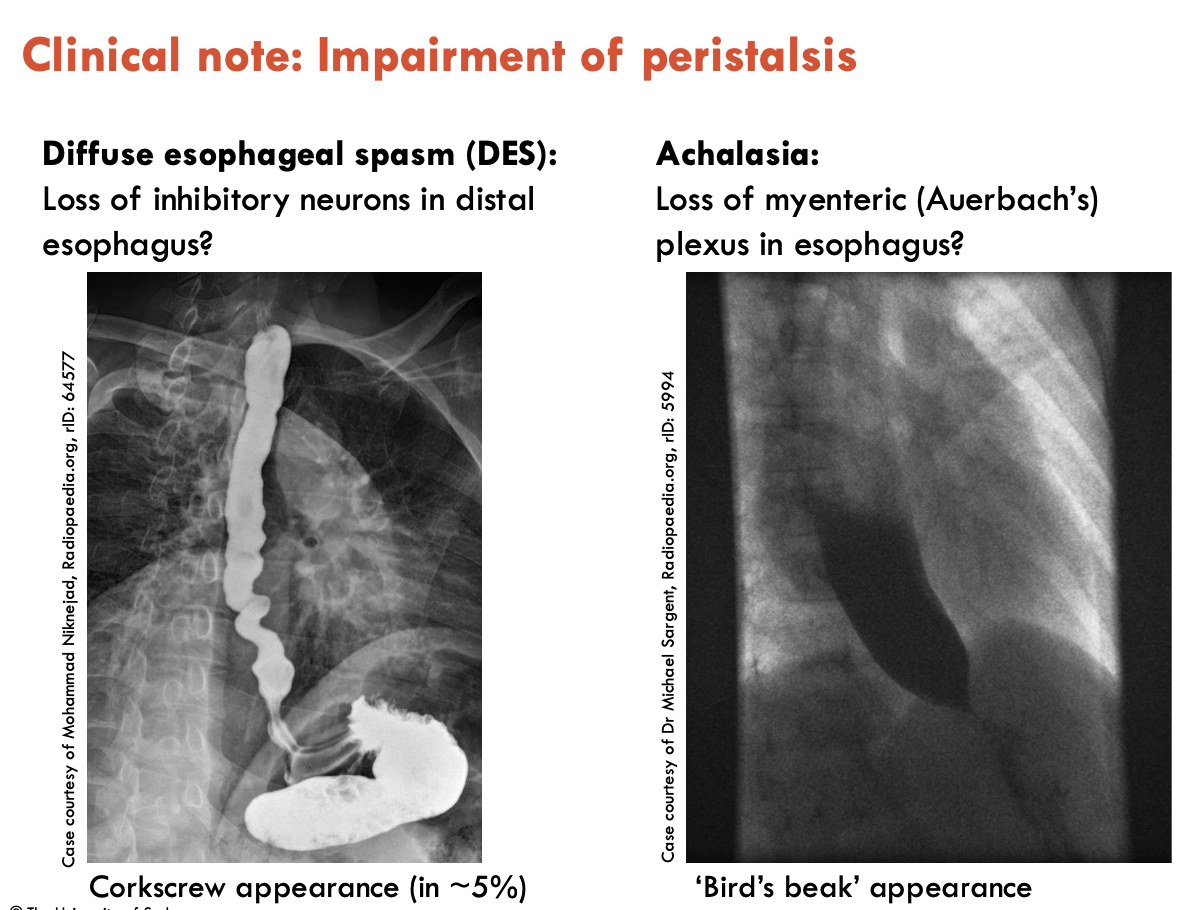
What conditions arise from peristalsis impairment?
Nerve supply to the oesophagus controls peristalsis
Impairment to this can lead to:
Diffuse oesophageal spasm (DES): loss of inhibitory neurons in distal oesophagus (corkscrew appearance)
Achalasia: loss of myenteric (Auerbach’s) plexus in oesophagus (Bird’s beak appearance)
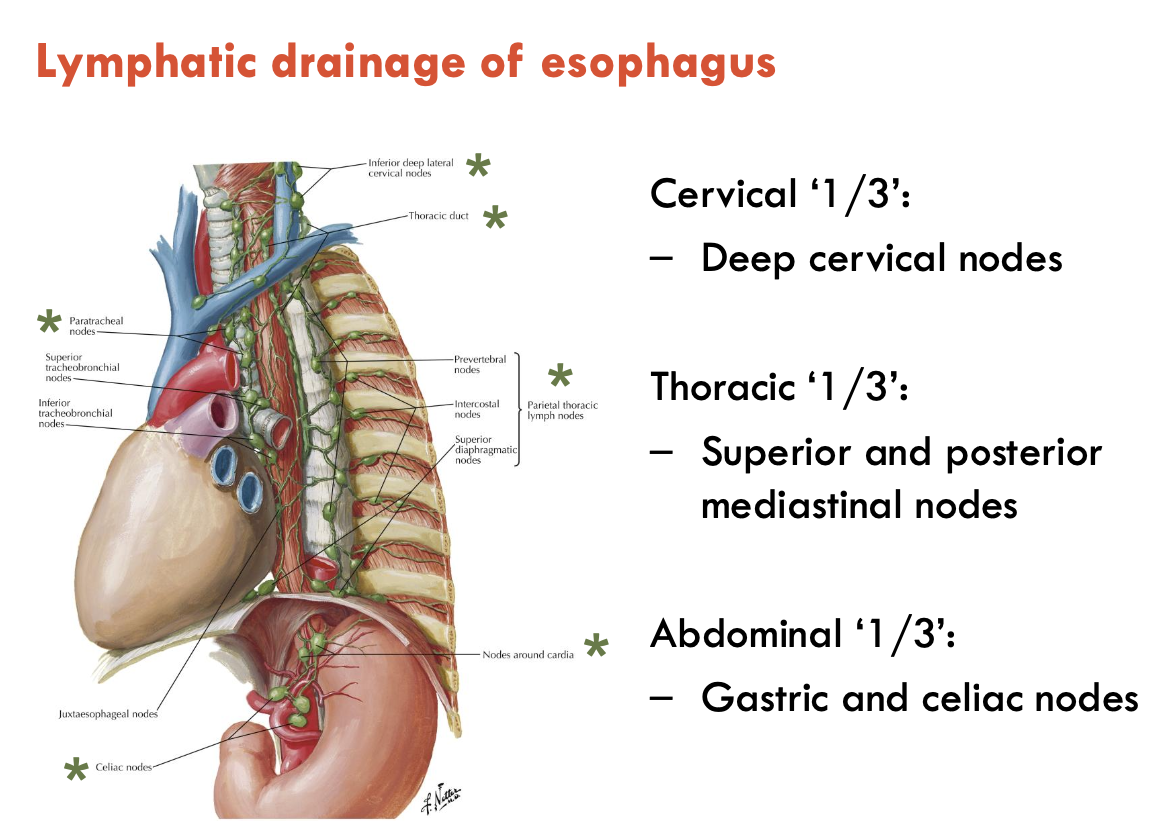
Describe the lymphatic drainage of the oesophagus
Cervical 1/3: deep cervical nodes
Thoracic 1/3: sup. and post. mediastinal nodes
Abdominal 1/3: gastric and coeliac nodes
List the 4 regions of the stomach
cardia
fundus
body
pyloric part: antrum, canal, sphincter/pylorus
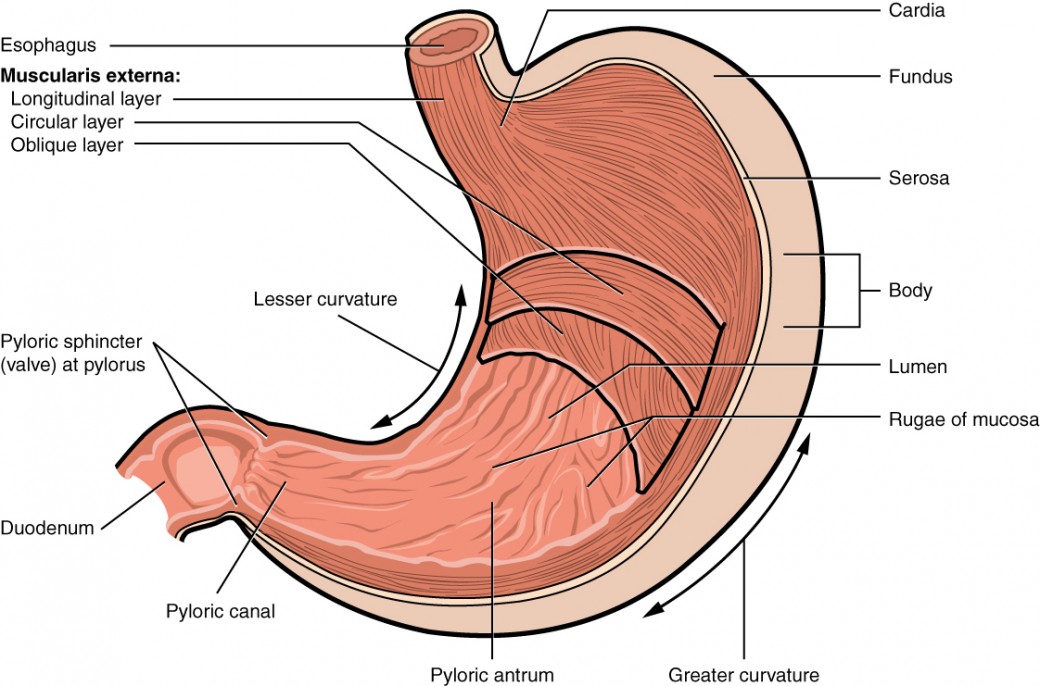
List the 2 curvatures and 2 sphincters of the stomach
Curvatures:
Lesser - shorter concave border
Greater - longer convex border
Sphincters:
Lower oesophageal sphincter (LES)
Pyloric sphincter
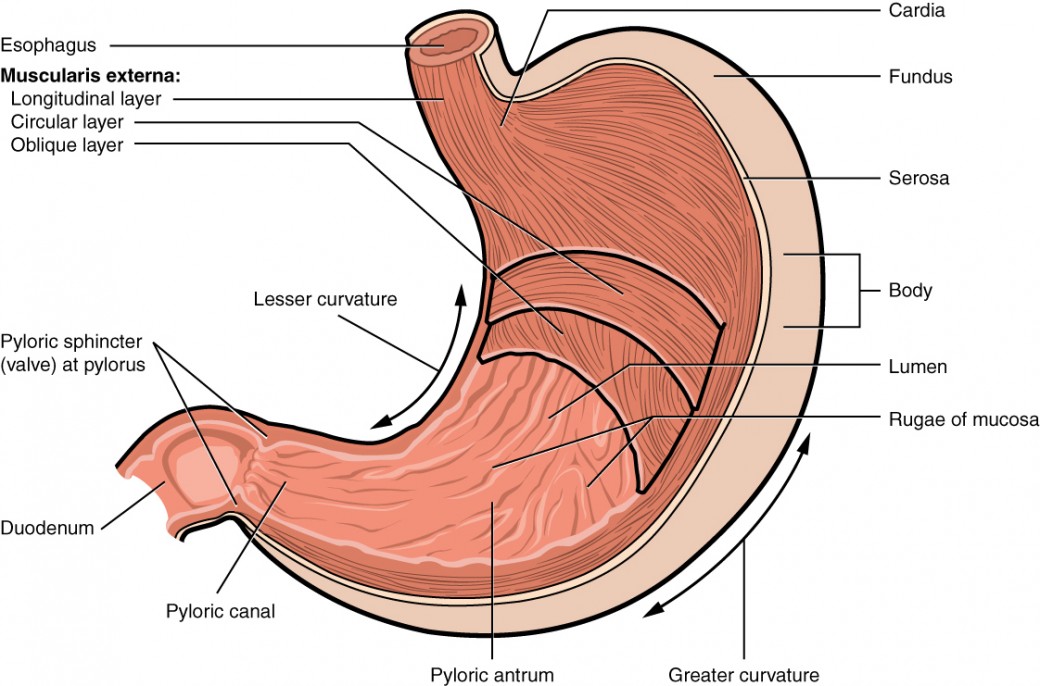
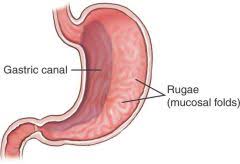
What are the internal features of the stomach (3).?
The stomach is highly distensible (can contain 45 - 1500 mL), and has the following internal features:
gastroesophageal junction marked by the ‘z-line’ - the transition between oesophageal (stratified squamous) and gastric (columnar) mucosa (more of a histological feature, hard to see on specimens)
longitudinal gastric folds (rugae) - most developed in the pyloric part and along the greater curvature
gastric canal - forms along the lesser curvature during swallowing
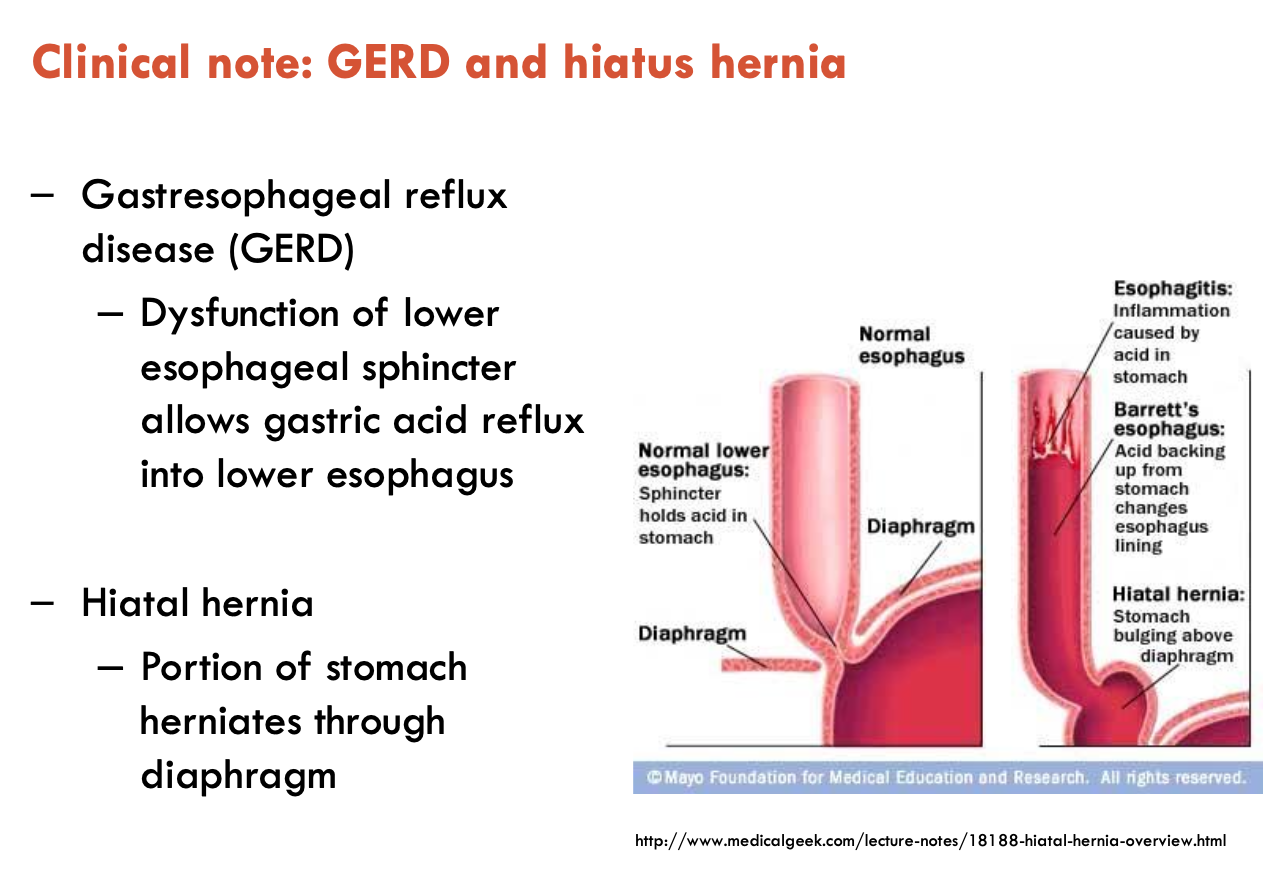
What is gastroesophageal reflux disease?
Gastroesophageal reflux disease (GERD)
dysfunction of lower oesophageal sphincter allows gastric acid reflux into lower oesophagus, can lead to hiatal hernia
Hiatal hernia: portion of stomach herniates through the diaphragm
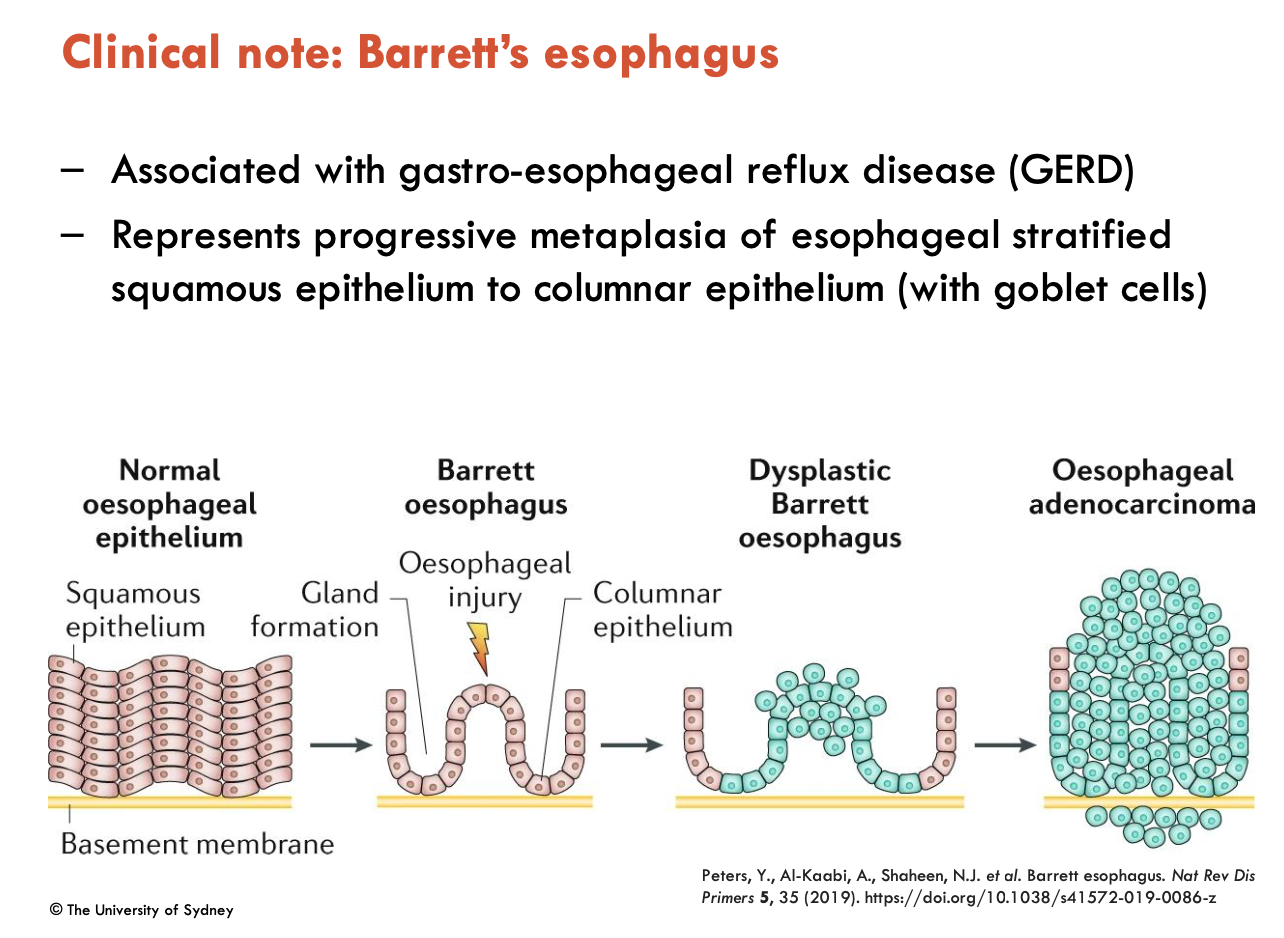
What is Barrett’s oesophagus?
Associated with GERD, Barrett’s oesophagus represents progressive metaplasia of oesophageal stratified squamous epithelium to columnar epithelium (with goblet cells)
difficult to detect using radiographic (barium swallow) imahing
often detected incidentally when using upper endoscopy for assessment for GERD - confirmed on biopsy
if metaplasia continues, can lead to cancer
What are gastric ulcers?
Gastric ulcers are characterised by a decrease in mucosal barrier
one of the most common chronic GIT diseases
risk of perforation (hole)
major risk factors:
Helicobacter pylori infection
frequent, long-term use of NSAIDs
Image of Blood Supply of Stomach
Arteries
coeliac trunk
L & R gastric arteries
short gastric arteries
L & R gastro-omental arteries
Veins
portal vein
L & R gastric veins
short gastric vein
L & R gastro-omental veins
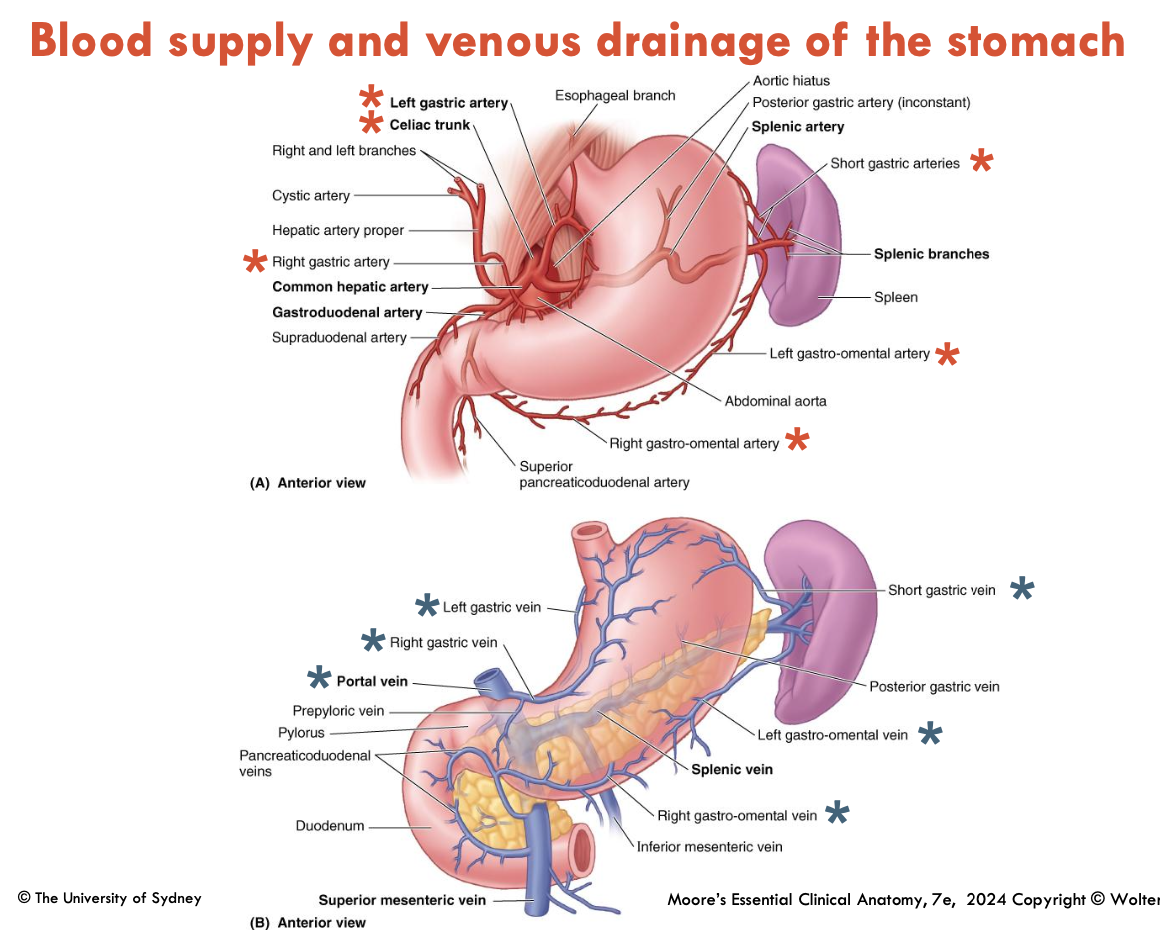
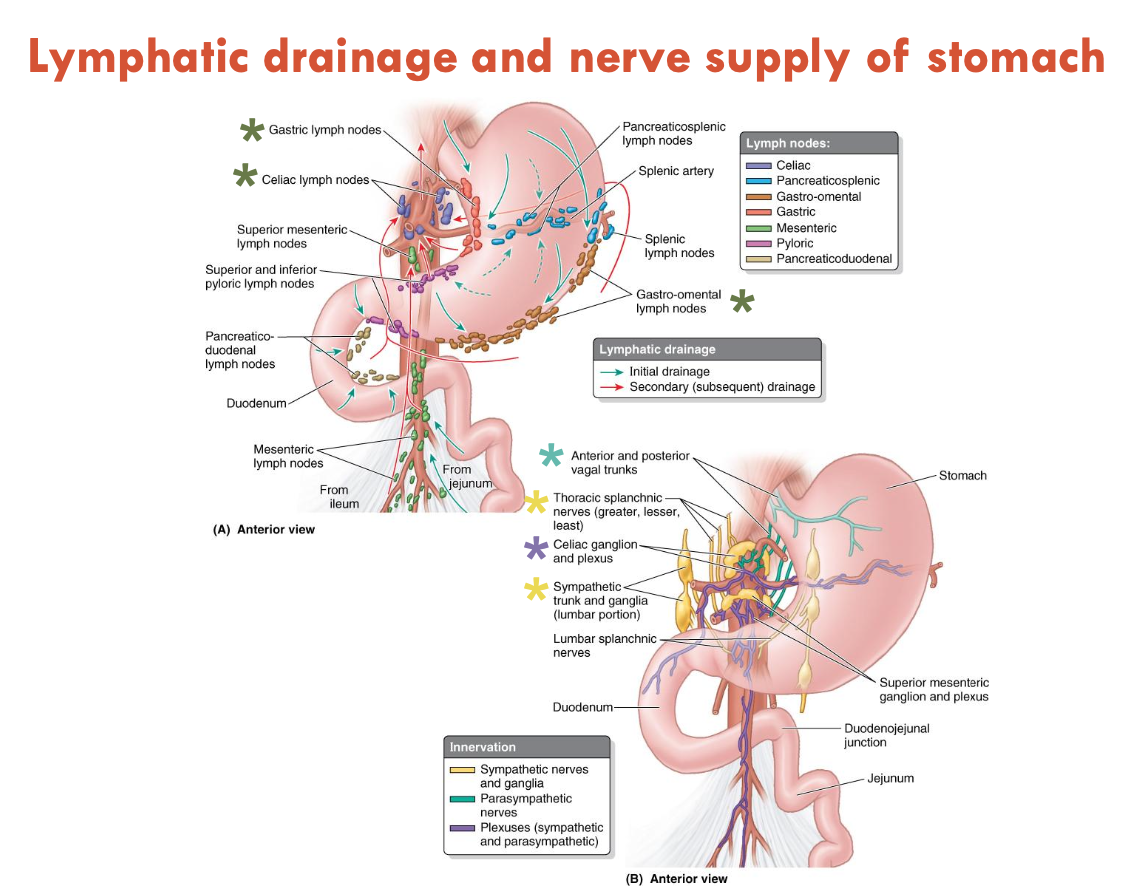
Image of Lymphatic Drainage and Nerve Supply of Stomach
Lymph Nodes
gastric lymph nodes
coeliac lymph nodes
gastro-omental lymph nodes
Nerves
Ant. & Post. vagal trunks
thoracic splanchnic nerves (greater, lesser, least)
coeliac ganglion and plexus
sympathetic trunk and ganglia (lumbar)