BIO 338 Exam 2
1/104
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
105 Terms
neuroendocrinology
endocrine system releases hormones into circulation (blood stream)
hormones limited in speed, by cardiac output
slower
can give an indication of how nervous system is functioning
nervous system uses neurotransmitters
hormones
several classes
amino acid derivatives
peptides
proteins
steroids
chemical structure impacts the way they are transported and the way their effects are exerted on a tissue
blood hormone control
effect exerted by a hormone on a tissue is proportional to the concentration of that hormone in the blood and the number of active receptors
concentration of hormone dependent on:
rate of secretion from the gland
rate of metabolism or excretion
quality of transport proteins (steroid in particular)
changes in plasma volume
hormone secretion
rate of secretion dependent on:
magnitude of input (what is the stimuli?)
whether the input is stimulatory or inhibitory
input is ALWAYS a chemical, but can be an ion, substance (ex. glucose), neurotransmitter or another hormone
hormone control of processes are redundant with many inhibitors of secretion (one pathway is blocked, the process will continue)
metabolism of hormones
plasma concentration influenced by rate of metabolism
inactivation can take place at or near the receptor or in the liver
kidneys also help in hormone secretion
slow down metabolism; increase concentration of hormone
transport protein
some hormones require transport in blood via binding/transport protein
steroid hormones require this
hormone must be unbound or active to exert an effect
Amount of free hormone dependent on
quality of transport protein and the capacity and affinity of the proteins to bind the hormone molecules
want a lot of transporters and want them to be able to release their neurotransmitter well
first adaptation to altitude
exercising; more RBC than plasma - increased concentration of hormones in blood; more at higher intensity, higher concentration of O2 (by lessening plasma)
hormone-receptor interactions
carried via the circulation to all tissues, but effect only exerted on those with specific receptors
receptors are not static fixtures
downregulation
decrease in receptor number in response to high concentration of hormone - diminishing response for some hormone concentration (less sensitive)
ex. type II diabetes
upregulation
increase in receptor number in response to low concentration of hormone - enhance sensitivity
saturation
all receptors in or on a cell are bound with a hormone - any additional increase in hormone concentration will have no net effect on the tissue
too much hormone
competition
receptors are specific to chemical shape so two hormones can have a similar chemical shape and thus ‘compete’ for binding (least amount of drug needed to stimulate hormone)
ex. pharmaceuticals
mechanisms of hormone action
several ways by which a hormone can exert a response/effect
mechanism of hormone action 1
altering the activity of DNA in the nucleus to initiate or suppress the synthesis of a specific protein
steroids
mechanism of hormone action 2
activation of special proteins called “second messengers”
lipophobic
mechanism of hormone action 3
alerting membrane transport mechanisms
insulin
altering activity of DNA in the nucleus
lipophilic; steroid, easily diffuses into cell
steroid hormone binds to a receptor protein in the cytoplasm or nucleus
if bound, then complex enters the nucleus
in nucleus, hormone or hormone receptor complex bind to hormone - responsive elements on DNA
directly w/ DNA
activates or could suppress genes that lead to mRNA synthesis that carry codes from nucleus to cytoplasm where protein in synthesized
cyclic AMP second messenger mechanism
hormone binds to receptor on cell surface
activates G protein within cell membrane
link between inside of cell and hormone- receptor complex on surface
G protein activates adenylate cyclase which causes formation of cyclic AMP
increased cyclic AMP concentration activates protein kinase A
PKA activates response proteins to alter cellular activity
ion channel second messenger mechanism
hormone binds to receptor on cell surface
activates G protein located within cell membrane
link between inside of cell and hormone-receptor complex on surface
G protein activates phospholipase C
phospholipid on membrane is hydrolyzed into IP3; causing Ca++ release and DAG
Ca++ binds to an active calmodulin which activates proteins in the cell
work in concert with calmodulin effects
membrane transport
hormone binds to receptor on cell surface, which activates carrier molecules in or near near the membrane to facilitate the movement of substrates/ions into the cells
relevant for exercise physiology, determines how quickly you can get glucose into a cell
hormones: regulation and action
hormones are secreted from endocrine glands
hypothalamus and pituitary glands → release hormones to release other hormones; stimulate another endocrine organ to release their hormones
thyroid and parathyroid glands → T3 and T4
adrenal gland → norepinephrine and epinephrine
pancreas → insulin, glucagon
testes and ovaries → sex hormones
hypothalamus and pituitary gland
hypothalamus
controls secretions from pituitary gland
located at the base of the brain; attached to the pituitary
anterior pituitary gland
true endocrine gland
hormone release controlled via chemicals that originate in neurons in the anterior pituitary
these chemicals stimulate or inhibit the release of specific hormones from anterior pituitary
posterior pituitary
also controlled by hypothalamus - hormones move down the axon to blood vessels in pituitary where they discharge into circulation
anterior pituitary gland
adrenocorticotropic hormone (ACTH)
follicle-stimulated hormone (FSH)
luteinizing hormone (LH)
melanocyte-stimulating hormone (MSH)
thyroid-stimulating hormone (TSH)
growth hormone (GH) most relevant for exercise
prolactin
posterior pituitary gland
oxytocin
antidiuretic hormone (ADH)
reduces water loss (via urine output) to maintain plasma volume
results in increased water reabsorption from the renal tubules to capillaries
released stimulated by high plasma osmolarity and low plasma volume
due to sweat loss without water replacement
released during exercise
osmoreceptors in the hypothalamus sense water concentration in the interstitial fluid
osmolality high - release of ADH
osmolality normal; plasma volume low - stretch receptors in left atria initiate ADH release
growth hormone
secretion stimulated by exercise (resistant; most potent), sleep, stress, and low plasma glucose
stimulates growth of all tissue through actions of insulin-like growth factors (IGFs)
stimulates uptake of amino acids. the synthesis of new proteins, and long-bone growth
spares glucose; goes into circulation
GH release is controlled via negative feedback where GH and IGF concentration inhibit further GH release
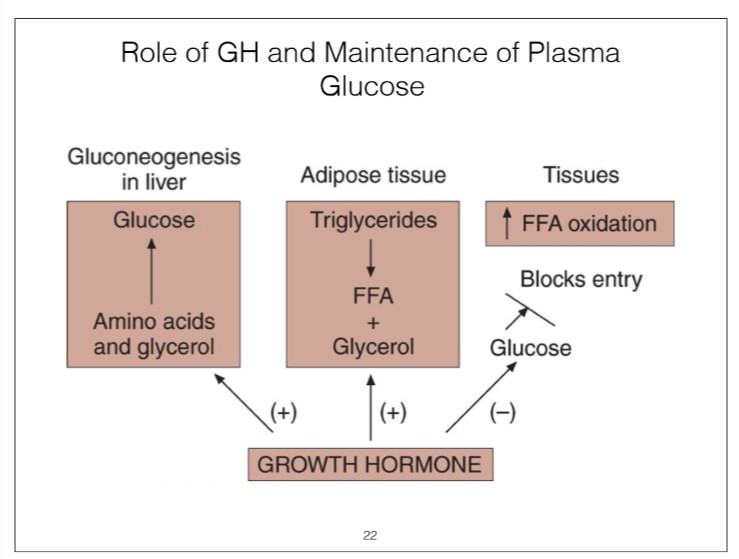
role of GH and maintenance of plasma glucose
increases blood glucose
use fatty acids instead of glucose
GH and exercise
very responsive to exercise
increases about by 2000% at max
greater in trained; mobilizing fat
GH and performance
increase protein synthesis and long-bone growth
used to treat childhood dwarfism, used by elderly, and by most athletes
athletes
definite history of use
effects more adverse than beneficial
not with micro dosing
minimal empirical evidence of performance improvement
can accelerate recovery; won’t directly improve performance but could improve training → negative outcomes
thyroid gland
thyroid stimulated by TSH to synthesize two iodine-containing hormones:
triiodothytonin (T3)
thyroxine (T4)
T4 is released from thyroid in greater amounts compared to T3, but most of T4 is converted to T3 which is the more potent of the two
thyroid hormones
central to establishing overall metabolic rate
related weight control
long latent period between T3 and T4 release and when their effects are observed
T3 6-12 hours
T4 2-3 days
controlled via negative feedback
during exercise “free exercise” concentration of hormone increase due to changes in binding characteristics of transport protein, which accelerates uptake by tissues
calcitonin - hormone released from thyroid gland that plays a minor role in Ca ++ regulation
critical for muscle contraction, bone growth, and bone decay
parathyroid gland/hormone
primary hormone involved in calcium regulation
adrenal gland
relevant for exercise
adrenal medulla
catecholamine
epinephrine and norepinephrine
adrenal cortex
mineralocorticoids
aldosterone - involved in maintenance of plasma Na+ and K+ concentration
glucocorticoids
cortisol - involved in plasma glucose regulation
sex steroids
androgens\ support prepubescent growth; androgens associated with post-pubescent sex drive in women
estrogens/
adrenal medulla
part of SNS
spikes fast; comes down quickly
secretes catecholamines (80% EPI, 20% NE)
fast-acting hormones
part of the “fight or flight” response
have wide acting effects on many different tissues and organs
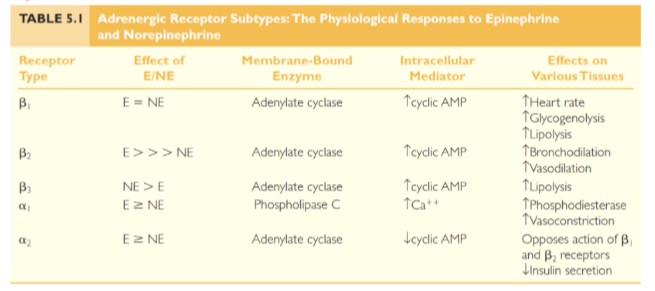
bind to adrenergic receptors on target tissues
alpha (a)
beta (B)
both can influence blood pressure
effect is dependent upon hormone and receptor type
epinephrine and norepinephrine
fast-acting hormones; appear quickly and disappear quickly
maintain blood glucose during exercise
plasma EPI and NE increase during exercise ( up to 1000 fold increase)
adaptions to training”
decreased plasma EPI and NE following training
things most important for survival have multiple pathways - REDUNDANT
effect of EPI and NE
different subunits of a and B stimulated by NE and EPI but lead to different effects
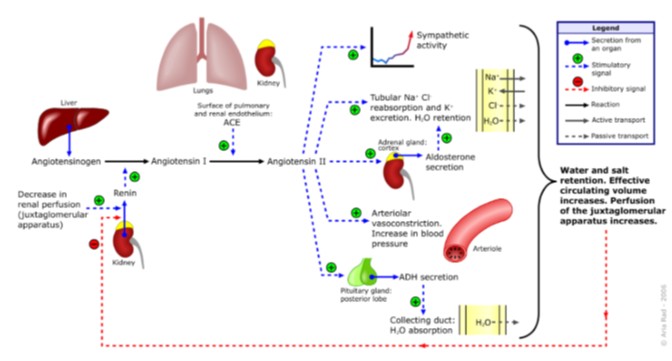
aldosterone
similar effects like vasopressin
controls blood volume
important regulator of Na+ and K+ and thus plays an important part in blood volume and bp regulation
chronically tend to increase over time; less negative consequences from higher blood pressure (temporary) than lower blood pressure
renin-angiotensin-aldosterone system
ACE inhibitors bring blood volume down
B blockers - reason why some need to try many medications
cortisol
mineralocorticoid
controls blood glucose during long-term fasting and exercise
promotes breakdown of tissue protein to form amino acids
more in circulation; keep it from entering cells
increases lipolysis
simulates liver enzymes involved in metabolic pathways leading to glucose synthesis
pancreas
blood glucose control
protects brain
insulin - secreted from B (beta) cells of the pancreas
facilitates movement of glucose from circulation to inside of cells
stimulated by plasma amino acid concentration, plasma glucose concentration, parasympathetic tone
inhibited by sympathetic outflow, EPI low plasma glucose
glucagon - secreted from a (alpha) cells of pancreas
opposite effect of insulin
stimulated by low plasma glucose, EPI
hormonal control of substrates during exercise
type of substrate and rate of utilization is the dependent upon the intensity and duration of exercise
intense = more carbohydrates
prolonged = more fats
control of muscle glycogen utilization
exercise intensity is inversely related to duration
higher intensity = shorter duration; quicker depletion
plasma EPI is powerful stimulator of glycogen breakdown
blood glucose homeostasis during exercise
all pathways in place to keep blood glucose in range
exercise provides a significant challenge to blood glucose control
plasma glucose maintained through 4 processes:
mobilize glucose from hepatic glycogen stores
mobilize FFA from adipose tissue and spare plasma glucose
synthesize new glucose via hepatic gluconeogenesis from amino acids, lactate, and glycerol
block glucose entry into cells to force the use of FFA as fuel
obviously goal is to maintain plasma glucose AND sustain work
permissive/slow acting hormones
thyroxine
thyroid hormones
T3 and T4 responsible for establishing basal metabolic rate and allow other hormones to have their full effect (permissive)
impacting number of receptors at the cell surface or altering the affinity of the receptor for a hormone
EPI has a minimal effect on FFA mobilization from adipose tissue in the absence of T3
cortisol
stimulates FFA mobilization from adipose tissue
slows uptake of glucose
GH
decreases glucose uptake by tissues
increases FFA mobilization
enhances hepatic gluconeogenesis
increases substantially during exercise and to a greater extent in trained vs. untrained
direct slow effect on blood glucose during exercise
fast acting
EPI and NE
mobilization of glucose from liver
mobilization of FFA from adipose tissue
interference with the uptake of glucose by tissues
NE taken to reflect SNS activity
EPI viewed as primary catecholamine in the mobilization of glucose
responsive to endurance training
plasma glucose still maintained; less needed at given workload
at maximal exercise is greater following training
insulin and glucagon
same sensed variable but opposite effect
insulin - increases glucose storage; lowers blood glucose concentration
involved in glucose uptake in ALL tissue
concentration decreases during graded exercise
glucagon - increases glycogen breakdown; increases blood glucose concentration
increases during exercise and favors FFA mobilization and hepatic glycogen breakdown
type 2 diabetes improves with exercise
SNS modifies the secretion of insulin and glucagon
skeletal muscle
human body contains over 600 skeletal muscles
40-50% body mass (change w/ phenotype)
functions
force production for locomotion and breathing
force production for postural support
heat production during cold stress
support of blood and lymphatic system
connective tissue covering skeletal muscle
epimysium - outer layer
perimysium - connective tissue that surrounds bundles of muscle fibers (fascicles)
endomysium - connective tissue that surrounds each muscle fiber within the fascicles
basement membrane - protective tissue around every fiber under the endomysium
sarcolemma - cell membrane of muscle cells
satellite cells
*precursor cells
undifferentiated cells, flexible fate contribute nuclei to muscle fibers
located above the sarcolemma but below the basement membrane
play a key role in muscle growth and repair
addition of nuclei increases capacity for protein synthesis
important adaption to strength training
myonuclear domain - volume of cytoplasm to nucleus; more nuclei, more capacity for growth
need nuclei for growth (hypertrophy)
microstructure of skeletal muscle
multi-nucleated
thick filament - myosin
thin filament- actin
striated appearance
sarcomere - functional component, separated by z line
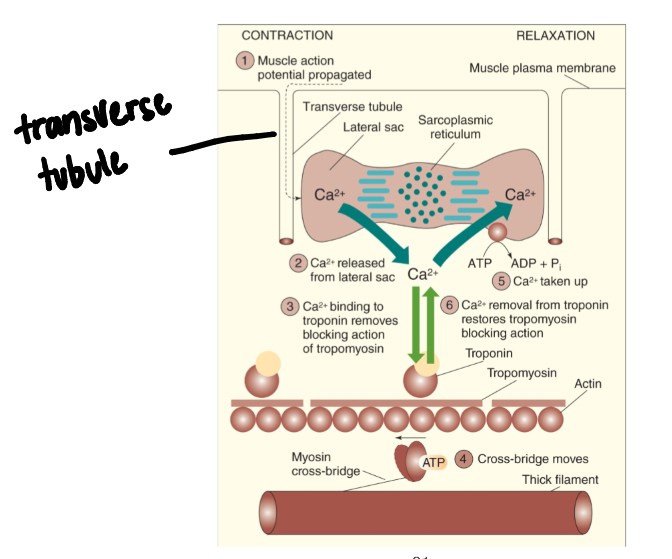
sarcoplasmic reticulum and transverse tubules
SR is membrane channel surrounding myosin fibril
storage of Ca++
transverse tubules pass through fiber -sandwiched between terminal cisternae of SR
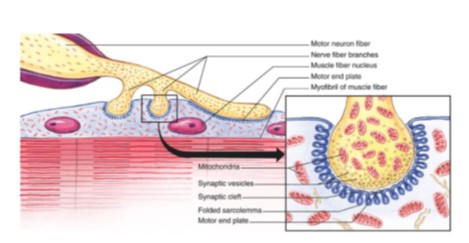
neuromuscular junction
junction between motor neuron and muscle fiber (where motor neuron meets muscle cell)
motor neuron - where nerve meets contractile component
motor unit = motor neuron and all fibers it innervates
motor end plate = pocket formed around motor neuron by sarcolemma
neuromuscular cleft = short gap between neuron and muscle fiber
acetylcholine is released from the motor neuron
causes end-plate potential (EPP)
results in depolarizing of muscle fiber
muscular contraction
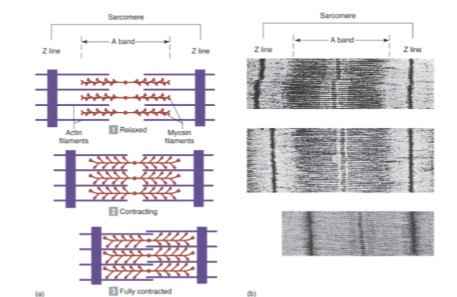
end result is actin ‘sliding’ over myosin which causes the muscle to shorten (contract) and develop tension
crossing of thick and thin filaments
process of muscular contraction is explained by sliding filament theory
sliding filament theory
muscle fibers contract by a shortening of their myofibrils due to actin sliding over the myosin
results in a reduction in the distance between Z lines
formation of cross-bridges between actin and myosin
rigor mortis - no ATP (dead), muscles stay contracted
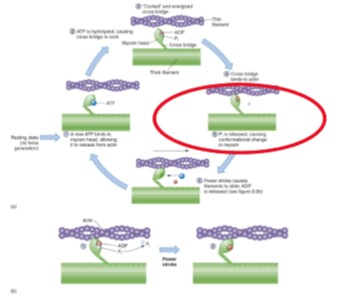
energy for contraction
energy required at several steps
breakdown of ATP is done via ATPase (present at myosin head)
this release of energy serves to energize the myosin cross-bridge which results in the pulling of actin towards the center, shortening the fiber
power stroke -single contraction, of all the cross bridges in a muscle would only shorten the muscle ~1% and some can shorten up to 60%, must be done many times
excitation
process begins when a nerve impulse arrives the the neuromuscular junction
depolarization is conducted down the transverse tubules deep into the muscle fiber
end result - release of Ca++ from SR
contraction
released Ca++ diffuses into the muscle and binds to troponin
troponin is directly on tropomyosin which lies in the grooves of the double strand of actin
in relaxed muscle there is no cross-bridge formation because tropomyosin is in the way of the binding sites
attachment of a fresh ATP breaks the actin-myosin cross-bridge
ATPase again hydrolyzes ATP and provides energy for a new ’cocking’ of the myosin head and reattachment of the cross-bridge to a new site and generation of another power stroke
lack of Ca++ or accumulation of H+ and Pi, impair cross bridge movement and ability to generate force
relaxation
signal to stop contraction is the absence of impulse
triggers an energy-requiring Ca++ pump within the SR to requestor Ca++ back to the SR
this will remove Ca++ from troponin causing tropomyosin to roll back and cover binding sites on actin
important to get into relaxed state
steps of skeletal muscle contraction
excitation
nerve impulses reaches the neuromuscular junction
depolarization sweeps through the transverse (T) tubules
Ca++ is released from SR
contraction
Ca++ binds to troponin
tropomyosin rolls and reveals site of cross-bridge formation
ATP binds to myosin, energy is released, and myosin is cocked and energized
without tropomyosin in the way, myosin binds to actin
Pi is released, myosin rotates toward midline and shortening occurs
ADP is released and myosin remains bound to actin until another ATP binds to myosin - once new ATP binds to myosin the bridge is broken
ATP is broken down my myosin ATPase and myosin is re-cocked and shortening occurs
Relaxation
nerve impulse is gone triggering the re-sequestration of Ca++ into the SR
once Ca++ is pulled back into the SR the contraction is over and myosin can’t bind anymore because tropomyosin is in the way
muscle function
motor unit - one motor nerve and all the muscle cells it innervates
ratios from 1:1 to 1:2,000 or more
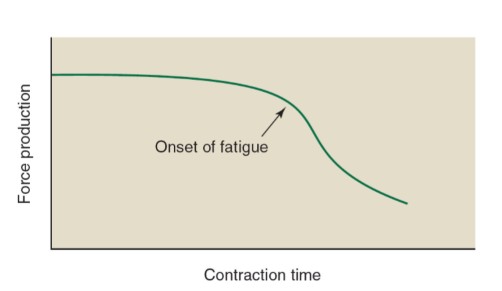
muscle fatigue
decline in muscle power output; inability to maintain a specified power output
or perception of increased effort when maintaining power output (can be central fatigue)
decrease in force generation
decrease in shortening velocity
high intensity exercise ~60 sec
prolonged submaximal exercise ~2-4 hrs
CNS factors for fatigue
central fatigue
brain or spinal chord sends less signal to the muscle (less force generated)
more peripheral feedback, less central drive—very difficult to dissociate
fatigue neuromuscular junction
rapid, repeated contractions causes depletion of acetylcholine a neuromuscular junction
leads to less stimulus going to the muscle and thus a reduction in force generation
fatigue contractile apparatus
don’t want high acidity in muscle
something at the level of muscle inhibits contraction or development of energy
lactic acid accumulation; buildup of H+
inhibits Ca++ release from SR
negatively affects ca++ binding to troponin
H+ ions inhibit PFK
fatigue tries to prevent too high [H+]
ATP-PC depletion (ATP not depleted, but PC is)
glycogen depletion (longer duration exercise)
Pi causes fatigue
muscle cramps
spasmodic involuntary muscle contractions (don’t know exact reason why)
electrolyte depletion and dehydration theory
water and sodium loss via sweating causes spontaneous muscle contractions
Na+ accumulates in interstitial space resulting in excess Ach release into synapse
altered neuromuscular control theory
muscle fatigue causes abnormal activity in muscle spindle and golgi tendon organ
leads to increased firing of motor neurons
hypocapnia - (possible cause) low CO2 in body
clear effect of CO2 on cramps
stretching of a muscle activates
golgi tendon organ which inhibits motor neurons, allows muscle to relax and stops cramps temporarily
characteristics of muscle fiber types
biochemical properties
oxidative capacity
number of capillaries, mitochondria, and amount of myoglobin
type of myosin ATPase
speed of ATP degradation
contractile properties
maximal force production
speed of contraction (Vmax - velocity)
myosin ATPase activity
muscle fiber efficiency
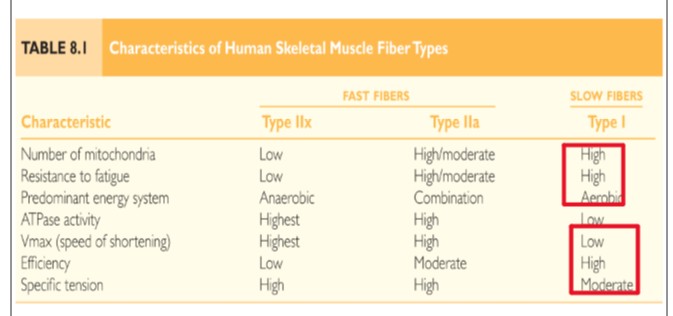
characteristics of individual fiber types
type I fibers (endurance athletes)
slow-twitch fibers
slow oxidative fibers
type IIa fibers (anaerobic and aerobic glycolysis)
intermediate fibers
fast-oxidative glycolytic fibers
type IIx fibers (fatigue a lot faster)
intermediate fibers
fast-glycolytic fibers
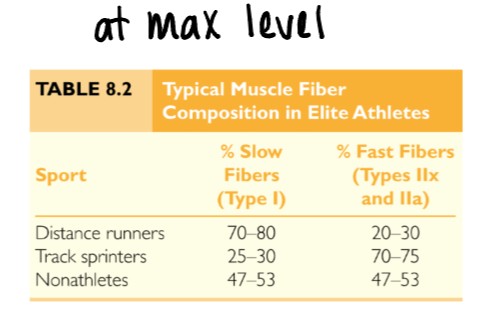
fiber types and performance
no sex difference in fiber type distribution
mostly genetic; some plasticity w/training
sedentary individuals posses approximately 50% slow twitch fibers
power athletes have a high percentage of type II fibers
endurance athletes have high percentage of type I fibers
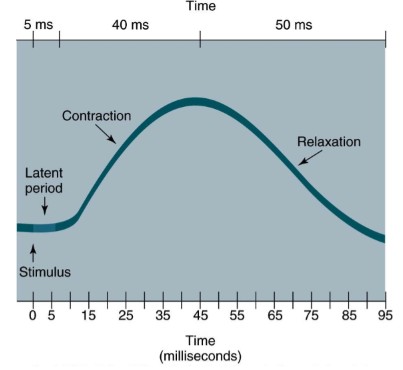
muscle twitch
if muscle given a single stimulus; responds with a simple twitch
twitch characteristics dependent of proportion of fiber types
latent period - immediately after stimulus; lasts a few milliseconds
contraction phase - muscle shortening; lasts ~40 milliseconds
relaxation phase - return to original length; lasts ~50 milliseconds
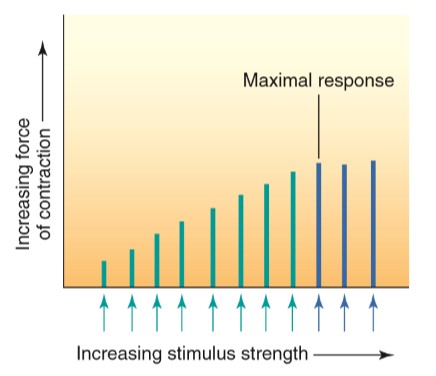
force regulation in muscle
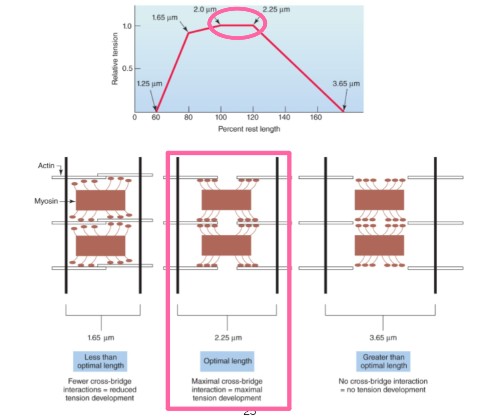
w/in single fiber, force related to actin-myosin contact
number and type of motor units required
initial muscle length overlap of actin and myosin)
ideal length for force generation
nature of neutral stimulation of motor units
frequency of stimulation
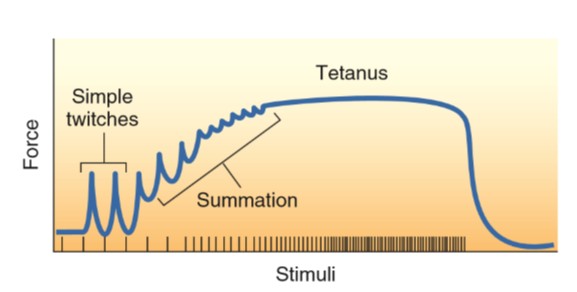
simple twitch
summation
tetanus
prior contractile activity
can help or hinder; ex. post-activation potential
relationship between stimulus strength and force of contraction
length-tension relationship on skeletal-muscle
optimal length
simple twitch, summation, and tetanus
prior contractile activity
if a muscle performs a fatiguing exercise, subsequent force production is decreased
short period of non-fatiguing exercise can enhance force production ex. warm-up
post-activation potential (PAP)
phosphorylation of myosin light chains increases sensitivity of Ca++ release
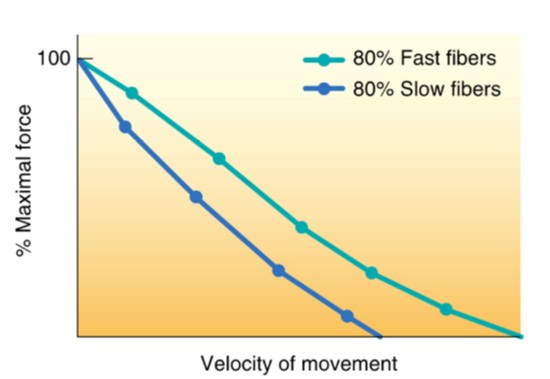
force-velocity relationship
ideal speed of contraction for force generation
at any absolute force, the speed of movement is greater in muscle with the higher percent of fast-twitch fibers
the maximum velocity of shortening is at the lowest force
true for both slow and fast-twitch fibers
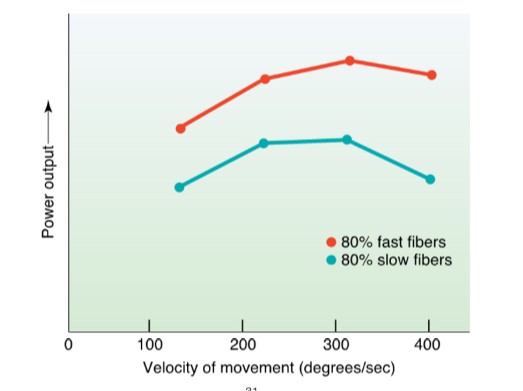
force-power relationship
at any given velocity of movement, the power generated is greater in a muscle with a higher percent of fast-twitch fibers
peak power increases with velocity up tp movement speed of 200-300 degrees/sec
power decreases beyond this velocity because force decreases with increasing movement speed
general nervous system functions
control of the internal environment w/ the endocrine system
voluntary control of movement
programming spinal cord reflexes
assimilation of experiences necessary for memory and learning
organization of the nervous system
central nervous system
brain and spinal cord
peripheral nervous
neurons outside of the CNS
sensory division
afferent fibers transmit impulses from receptors to CNS
afferent - arrives to brain and spinal chord
motor division
efferent fibers transmit impulses from CNS to effector organs
efferent - exits from brain and spinal chord
somatic - skeletal muscles, external
autonomic - smooth muscle, cardiac, glands, often not voluntary
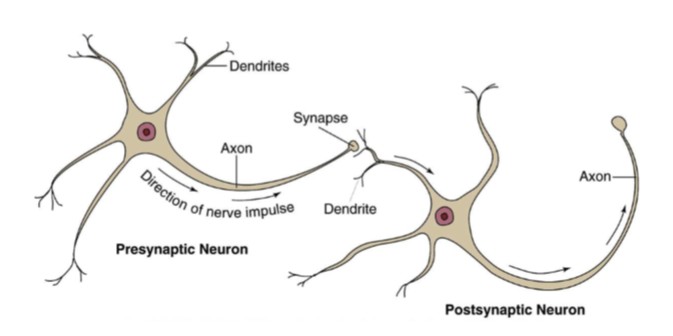
structure of the neuron
cell body - center of operation and contains nucleus
dendrites - narrow cytoplasmic connections; serve as receptive area that can conduct electrical impulses towards the cell body; receives information
axon - carries electrical message away from cell body towards another neuron or effector organ; axon transmitting action potential
synaptic connections lost as you age
schwann cells
insulating layer of cells covering axons (white matter of brain)
contain large amount of myelin (lipid protein structure)
nodes of ranvier
gaps between myelin segments
play an important role in neural transmission
larger the nerve fiber, the faster the transmission
saltatory transduction
impulse ‘jumps’, fast from node to node
electrical activity in neurons
neurons are an excitable tissue
irritability
ability to respond to a stimulus and convert it to a neural impulse
conductivity
transmission of the impulse along the axon
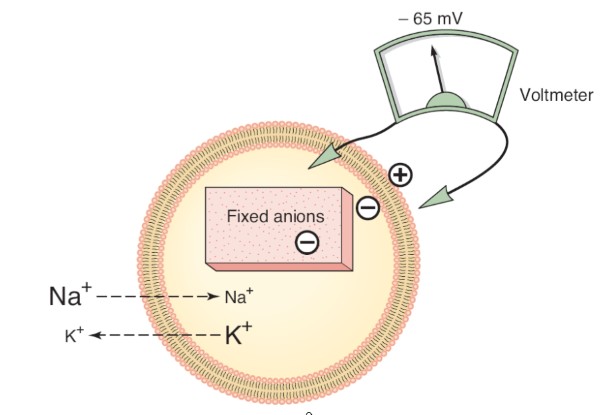
resting membrane potential
cells negatively charged
polarized
attracts positively charged cations on outside of neurons
-5 to -100 mv determined by
permeability of the cell membrane to different ions
differences in ion concentrations between the intracellular and extracellular fluids
many ions present, but Na+, K+, and Cl- exist in the highest concentrations and play the most important role
more negative - hyperpolarization
more positive - depolarization
concentrations of ions across a cell membrane
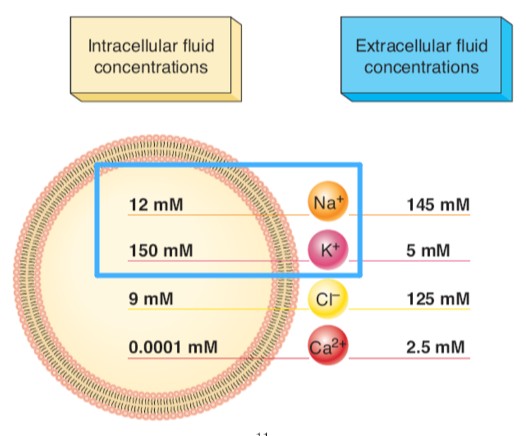
resting membrane potential specifics
permeability of a neuron membrane to K+, Na+, and other ions regulated via ion channels
can be opened or closed by gates within the channel
when open, ions move from high to low concentration (increase permeability)
at rest, almost all Na+ channels are closed (some K+ open)
negative resting membrane potential in neurons is maintained by:
higher permeability of the membrane for K+ compared to Na+
concentration gradient for K+ promotes movement of K+ out of the cell
Na+ wants in; K+ wants out
cell membrane has a Na/K pump that uses ATP to maintain the intracellular/extracellular ion concentrations by pumping Na out and K in
energy consuming; against concentration gradient
3 Na+ for every 2K+
Na/K pump

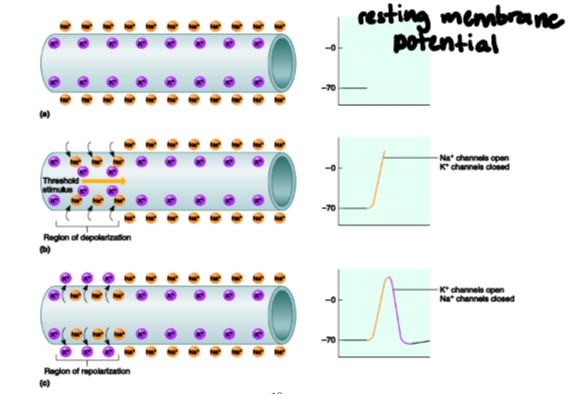
action potential
stimulus of sufficient strength depolarizes the cell; all or nothing
opens Na+ channels (reaches threshold) and Na+ moves in to the cell —> depolarization
when critical threshold is reached, more Na+ gates open; action potential occurs
ionic exchanges along axion occur to propagate the nerve impulse sequentially along nodes of ranvier
repolarization
return to resting membrane potential- occurs immediately after depolarization
K+ leaves cell rapidly (increased permeability)
Na+ channels close, few positive ions enter the cell
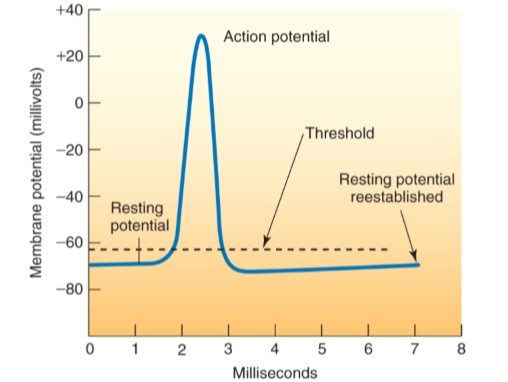
all or none law
if threshold is not reached; nothing happens
if impulse occurs; it will travel entire length of axon without a decrease in voltage; does not lose strength
depolarization/repolarization of a nerve fiber
neurotransmitters and synaptic transmission
neurons communicate using synaptic transmission
requires sufficient amount of neurotransmitter from synaptic vesicles into synapse
synapse - small gap between presynaptic neuron and postsynaptic neuron
neurotransmitter
acetylcholine (most common in muscle)
chemical messenger released from presynaptic membrane
binds to receptor on postsynaptic membrane
causes depolarization of postsynaptic membrane (excitatory neurotransmitters)
excitatory postsynaptic potentials (EPSP)
causes depolarization of entire cell body/neuron
can bring postsynaptic neuron to threshold by:
temporal summation - rapid, repetitive excitation from a single excitatory presynaptic neuron
spatial summation - sum EPSPs from several different presynaptic inputs/axons
inhibitory postsynaptic potential (IPSP)
cause hyperpolarization (more negative) making it more difficult for threshold to be reached
proprioceptors
receptors that provide CNS with information about body position
located in joints and muscles
kinesthesia
conscious recognition of the position of body parts
reason the brain has such a high metabolic rate
limb movement rates
joint proprioceptors
free nerve endings
most abundant
sensitive to touch and pressure
strongly stimulated at movement initiation, then adapt
golgi-type receptors
found in ligaments around joints (stress on ligaments)
similar to free nerve endings; not as abundant
pacinian corpuscles
in tissues around joints
detect rate of joint rotation
muscle proprioceptors
provide sensory feedback to nervous system; required for properly controlled movements
mechanoreceptors
tension development by muscle
account of muscle length
muscle spindle (stretch)
golgi tendon organ (tension)
muscle spindle
respond to changes in muscle length
primary endings (respond to dynamic changes)
secondary endings (provide information about static muscle length)
intrafusal fibers - run parallel to normal muscles (extrafusal fibers)
gamma motor neurons - stimulate intrafusal fibers to contract with extrafusal fibers by alpha motor neurons to tighten the spindle
stretch reflex - stretch on muscle causes reflex contraction
knee-jerk reflex
golgi tendon organ
monitors tension developed in muscle
prevents muscle damage during excessive force generation
stimulation results in reflex relaxation of muscle
inhibitory neurons send IPSPs to muscle fibers
ability to voluntarily oppose GTP inhibition may be related to gains in strength (muscle hypertrophy)