HSCI 366 FINAL
1/110
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
What is the equation for thermoregulation and what does each letter stand for?
S= M + (W) ± Cv ± Cd ± R - E
M= metabolic heat simply at rest
W= work (always positive)
Cv= gain or loss of heat due to movement of air or water next to the body
Cool air= loses heat
Hot air= adds heat
Application: steam from hot water
Cd= heat gained or lost via direct contact with hotter or colder surface
Application: touching a hot pan
R= primarily involves environment
Hot environment= adding heat
Cool environment= losing heat
E= evaporation primarily involving sweat (always negative)
What are the two types of sweat glands?
Apocrine and Eccrine
What is the function of apocrine?
Primarily found in very distinct places
Scalp, armpits, and groin
Breakdown of waste products of bacteria= odor
Where are eccrine glands found?
Palms of hands and soles of feet
Helps with traction, that’s why there are sweat glands there
How are eccrine glands stimulated?
Activated by sympathetic activation= physical stress (Work/Exercise)
Application: under emotional stress, palms can get sweaty
Where does sweat come from?
Blood
What are the two portions of the eccrine gland?
Secretory (coiled) and Resorptive (straight)
What is the function of the secretory duct?
REMEMBER: water follows solutes
Neurotransmitter (acetylcholine) binds to muscarinic receptor → activating NKCC transporter (through the sodium potassium pump which allowed for concentration gradient) → chlorides exits cell into duct (FOCUS ON CHLORIDE → sodium follows chloride) → calcium channel opens → it enters duct → potassium leaves cell → enters duct → the movement of solutes to the duct allows for water to follow
ATTACH IMAGE
What is the function of the resorptive duct? What is the application (regarding potassium and exercise)
Myoepithelial cells
Straight portion of the eccrine
Pushes solutes and water to the surface of the skin
Reabsorbs sodium and chloride
APPLICATION: May lose some HCO3 in sweat
Metabolic acidosis
Must ventilate more to restore pH balance
APPLICATION: when potassium is lost via sweat, may cause muscle cramps → may eat banana to prevent potassium loss
What happens in heat exchange during exercise? What is the exception to this rule? What is the application (referring to dogs and how we get rid of heat)?
PRIMARY WAY TO LOSE HEAT BY HUMANS: Creating more metabolic heat to create more ATP so muscle can contract→ blood flowing through muscle is picking up the heat (Known as Conduction) → heated blood goes throughout body → secretory portion pushes solutes to duct → water goes to surface of skin (heat is released through the sweat) → as sweat evaporates on surface of skin, body is cooled down (E is ALWAYS NEGATIVE)
EXCEPTION: if someone exercises in hot and humid environment → heat is radiating heat to the body and humidity does not allow for evaporation of sweat → only way to get rid of the heat is to sweat more to get rid of the heat
APPLICATION: heat could also get rid through ventilation (water is in expired gas)
Dogs do not sweat, they pant (ventilation) → heat is getting removed
What happens if you store more heat than you can lose? What happens in each “step” of heat exhaustion?
Heat Cramps
Loss of potassium
If muscles spasms and giving a cramp, but you continue → can lead to Heat Exhaustion
Heat Exhaustion
Muscle weakness
Dizziness
Nausea/Vomiting
Headache
Heat Stroke
Significant loss of water/sweat → losing blood
Osmoreceptors are activated by the hypothalamus → hypothalamus turns off sweet response → only way to get rid of heat is through evaporation/sweat → body temperature significantly increases → causes fainting/unconsciousness to force the body to stop working and also to preserve blood volume
May lead to coma and death
What are the oropharyngeal receptors? What is the problem with the oropharyngeal receptors when you exercise?
Stimulates thirst response: air gets in and out of lungs through mouth → oropharyngeal receptors start drying out → stimulates thirst sensation
Problem: drink water → rehydrate oropharyngeal receptors → turns off thirst sensation in hypothalamus → the thirst sensation turns off before you rehydrate all the water that was lost → you aren’t adequately replacing water that is lost → always drink a bit more water
What is the function of skeletal muscle?
support (sitting upright, standing, anything resisting gravitational pull…), provide protection (i.e.: sternum protecting heart)
Skeletal muscle generally connected to skeletons– allows for movement– provides lever system for mobility
What cells do bones produces?
Red blood cells and white blood cells
What minerals do bones store?
calcium (contraction) and phosphate (adenosine triphosphate– fuels Na+/K+ ATPase pump)
What is present in red marrow?
Stem cells (Hematopoietic Stem Cells)
Stem cell can differentiate into a different type of cell
Can differentiate into RBC, WBC, or Osteoclasts (degrading bone)
What happens if calcium levels are too low? (what will bone do? what cells are involved?)
If calcium levels are low and calcium is needed → your body will take calcium from the storage depots → osteoclasts will degrade bone to release calcium and phosphate so your body can have it for neurotransmissions, contractions, hormone secretions…
What is the function of yellow marrow?
Mesenchymal Stem Cells
Can differentiate into osteoblasts, osteocytes, chondrocytes, adipocytes (adipose/fat)
What are the two layers that bone has?
compact bone and spongy bone
What is the function of compact bone?
Goes around all the bone → lots of mineralized crystal (hydroxyapatite crystal) → gives bone lots of compressive strength and tensile strength
Compressive strength= bone will resist compression
Tensile strength= bone will resist stretching
What is the function of spongy bone?
Can withstand DEFORMATION STRENGTH (will allow twisting without breaking of the bone) → more pores in the spongy bone allows for twisting → that is why it tends to appear at the ENDS of the bone
What is the long bone comprised of?
End of long bone is epiphysis and middle of long bone is diaphysis
Describe modeling of the bone
When the baby is first bone, the bones are primarily made of cartilage (advantage: cartilage is bendy which allows for pushing of birth canal) → long bone begins to mineralize and grow after birth (grows in both directions to make it longer) → Chondrocytes are responsible for making more cartilage (in both directions) → chondrocytes eventually die, but leave behind cartilage (framework) → after chondrocytes, osteoblasts follow (osteoblasts are responsible for BUILDING more bone) → osteoblasts make osteoids (organic matrix of collagen, proteins..) → osteoid attaches to cartilage AND THEN IT MAKES hydroxyapatite crystals (helps in storing minerals like calcium and phosphate) → once osteoblasts finish making those two structures, osteoblasts differentiate into osteocytes (bone cells)
How are the cells for modeling of bone stimulated? (what is the application regarding height)
Hypothalamus releases GHRH (growth hormone releasing hormone) → Stimulates pituitary gland to release growth hormone → Mesenchymal stem cells are stimulated to make more chondrocytes and osteoblasts to stimulate more growth → bone begins to mineralize since no more growth takes place (due to growth plate/epiphyseal closure)
APPLICATION: height can be influenced by genetics AND diet (you need nutrients in order to grow → growth is stunted)
What is the simple definition of remodeling? What part of the bone does it focus on?
osteoblasts turn into osteocytes
Focus on compact bone (lots of compressive and tensile strength)
Bone is highly mineralized (lots of calcium and phosphate)
Describe the anatomy of compact bone
Concentric circles within compact bone= Osteon
Concentric circles within the osteon is a lamellae > within lamellae is lacuna > inside lacuna is an osteocyte > central canal/haversian canal holds blood vessels which carries nutrients (canaliculi is what helps carry nutrients from blood vessel to further cells within the osteon)
Compare osteoclast and osteoblast activity/size/amount in compact bone
There are more osteoblasts than osteoclasts surrounding osteon
Osteoclasts are also larger than osteoblasts
Osteoclasts are multinucleated and osteoblasts are mono-nucleated
Osteoclasts can release protease to break down the organic portion of the osteoid and an acid to break down the hydroxyapatite cartilage
Usually osteoclast activity = osteoblast activity
Describe how osteoclast and osteoblast activity changes
The release of sclerostin by osteocytes promotes an imbalance between the osteoclast and osteoblast activity, which makes osteoclast activity GREATER than the osteoblast activity= bone is degraded
If osteocytes decrease sclerostin activity, then the osteoclast activity is less than the osteoblast activity which means more bone is deposited/more hydroxyapatite
What is osteoporosis?
Pores within bone makes it extremely brittle since osteoclast activity is much greater than osteoblast activity
Osteoporatic fracture= hundreds of pieces/shattered bone
Crack= easier to repair than fracture
Who is more susceptible to osteoporosis and why?
Women more susceptible to disease than men
3:1 ratio from women to men
Why?
Men start to lose bone around age of 40-45 with 1% every year and women start losing bones around 30-35 with 1% every year
Rate of loss elevates to 3-5% a year once menopause starts at around 50-55 years old since there is a lack of estrogen secretion
Estrogen normally inhibits osteocytes from releasing sclerostin
Rate of loss continues for around 5-6 years until it returns to 1% loss every year
APPLICATION: estrogen replacement therapy for women on menopause
Men are bigger in stature → they have more bone mass to begin with to hold a bigger frame
What are the risk factors to osteoporosis and describe why (to the ones we’ve learned)?
Heredity
Race/Ethnicity
Asians are more susceptible to osteoporosis
Black people are less susceptible to osteoporosis
Smoking
Can inhibit appetite (if women chronically smokes) → earlier onset of menopause → rate of bone loss accelerates
Alcohol consumption
Enhances urination → calcium is usually absorbed paracellularly in proximal tubule → if rate of loss increases, there is no time to reabsorb calcium
Decline in milk consumption
Vitamin D helps absorb calcium from milk
They found that in college-aged individuals, milk consumption is replaced with alcohol, caffeinated products, and soft drinks
How can you prevent osteoporosis? And why?
Engaging in strength training
Strength training= muscle gets stronger → bones are lever system for those muscles → lever arms get stronger to accommodate heavy lifting → bones get stronger
Osteocytes have mechanical sensing abilities → as you strength train and muscle is stimulated, osteocytes are also stimulated → osteocytes will lower the secretion of sclerostin → osteoblast activity is more than osteoclast activity → more hydroxyapatite is deposited to make the bone stronger
In animal studies, it was seen that bone marrow density increased by 3% when strength training → the force it took for bone to break is about 25-60% increase → use DXA to measure how much bone marrow density increased
Women should be strength-training and men should be doing cardio
What happens in skeletal system if calcium is too high?
Thyroid gland is stimulated → calcitonin is released → calcitonin lowers synthesis of vitamin D
When kidneys are stimulated by calcitonin → Ca2+ reabsorption decreases, excretion increases
Decrease in vitamin D synthesis → small intestines will decrease Ca2+ absorption
Reabsorption= physically part of the body and if your body does not want to keep it, it could be excreted
Absorption= liken digestive system as a “donut” where the hole in the middle is the esophagus empties into the stomach which empties into small intestines → large intestine; therefore, not “physically part of body” → if you want to keep certain solutes, it is absorbed, if not, it just flows through as feces
Collectively, calcitonin and decline in vitamin D → bones will increase osteoblast activity → some calcium is now stored in the bones
What happens in skeletal system if calcium is too low?
Parathyroid gland is stimulated → PTH (parathyroid hormone) is released → vitamin D is increased
When PTH is released, kidneys will increase Ca2+ reabsorption
Calcium is usually reabsorbed paracellularly in the proximal tubule → PTH opens calcium channels in the distal convoluted tubule → Ca2+ is now reabsorbed TRANScellularly since cells are very packed in the distal tubule
When Vitamin D is increased, small intestine will increase Ca2+ absorption
APPLICATION: milk is a great source of calcium and “fortified” with vitamin D → when it hits small intestine, you enhance the ability to increase calcium absorption → that’s why milk is fortified with vitamin D
Both PTH and Vitamin D will increase osteoclast activity in the bones
Osteoclast breaks down bone to make calcium more available
What is the lifespan of RBC/erythrocytes?
120 days
What is the process called of making new RBC?
erythropoiesis
Describe the process of making more RBC
Kidneys have many functions, one of which is releasing a hormone called erythropoietin (EPO) → EPO stimulates bone to make more RBC → a stem cell (hematopoietic) in the bone can differentiate into RBC
RBC differentiation starts with a nucleus, then the nucleus is lost (since RBC’s have no nucleus → meaning no regeneration is possible)
RBC also has no mitochondria → meaning no ATP/Na+/K+ ATPase Pump → the only way to make ATP in RBC is through glycolysis → only glucose can enter the RBC to make ATP
Within the erythrocyte differentiation, there is an iron dependent hemoglobin that is made → oxygen binds to hemoglobin/iron
Explain some applications to RBC formation
APPLICATION: increasing EPO/taking EPO means more RBC is made → more oxygen can be carried to muscles that need it
APPLICATION: “blood doping” → blood is taken out of athlete, kidneys make more blood from the blood loss → once the RBC is remade → blood is rethawed and inserted back into the body → an increase in RBC → more oxygen is able to enter muscles
APPLICATION: altitude training → air is thinner → body will make more RBC → when back to sea level, the body has increased amount of RBC/oxygen
APPLICATION: masks can be worn at sea level that mimic altitude training
What is RBC death called?
eryptosis
Why is the lifespan for RBC so short?
Lifespan is only around 120 days because they have to squeeze through very tiny blood vessels → this damages cell membrane of RBC → after the damage, the body recognizes it as “old” → subsequent death
Which organs are responsible for RBC death?
liver and spleen
Describe the process of RBC death
Macrophages will induce phagocytosis of the RBC
The liver recycles the important parts of the RBC → specifically, hemoglobin
The liver will dismantle the hemoglobin into the heme, globin, and iron
Heme = makes bilirubin → can either make bile or urochrome (only liver makes bile) → urochrome is a waste product and is filtered by the kidneys (urochrome is yellow which is why urine is yellow)
Globin= alpha and beta subunits are released → transported back to the bone → hemoglobin is restored
Iron= liver either stores iron (storage form of iron in liver is called Ferritin) OR liver can carry it to transport protein called Transferrin to transport it back to the bone so RBC can be reformed
What are the 6 nutrients that the body needs?
Carbohydrates
Fats
Proteins
Other three: water, vitamins, and minerals
What is the definition of digestion? Absorption?
Digestion: only way for absorption is to get the nutrient to its simplest form, only then will it be absorbed → that’s why digestion comes before absorption
Absorption
The actual act of uptaking the nutrients
What is the simplest form of carbohydrates?
Most simplest form= C6H12O6
There are three monosaccharides with this chemical formula, but structure is slightly different:
Glucose
Fructose
Galactose
Describe where digestion takes place in order
mouth, stomach, small intestine/pancreas, large intestine
What happens to carbohydrates in the mouth?
In the mouth, there are teeth which breaks down food to smaller pieces, called mechanical digestion
In the mouth, there is also chemical digestion with an enzyme called salivary amylase
In the mouth, the food is lubricated with saliva → allows for easy movement to the esophagus
What happens to carbohydrates in the stomach?
In the stomach, there is a lot of HCl acid → that acidity denatures the amylase enzyme (no more chemical digestion takes place in the stomach)
The HCl acid is there because it protects you from pathogens that you might have inadvertently consumed AND also for protein digestion (it denatures proteins)
E.Coli or Salmonella can survive through the acid
Describe the parts of the small intestine
The diameter is smaller in the small intestine, but it is very long
Initial part of small intestine is called duodenum → to jejunum → to ileum
What does the small intestine secrete to break down carbohydrates?
The pancreas secretes an enzyme called pancreatic amylase to restart chemical digestion again → it releases this enzyme at the duodenum
Amylase breaks bonds to separate carbs into sucrose, maltose, or lactose → THEN, the enzymes in the brush borders further breaks down the sugars
What specific enzymes are present in the small intestine to break down specific molecules of sugar?
There are “waves” in the small intestine which increases surface area
Within the “waves” are brush borders which will increase surface area even more
On the brush borders, there are three important enzymes: sucrase, maltase, lactase
—> Sucrase breaks down sucrose into glucose and fructose
—> Maltase breaks down maltose into glucose and glucose
—> Lactase breaks down lactose into glucose and galactose
Allows plenty of surface area and plenty of time to digest and absorb nutrients
What cells are present in the small intestine?
epithelial/enterocytes
Once the small intestine absorbs glucose, what happens?
Once the cells in the small intestine (epithelial/enterocyte cells) absorb glucose, it releases GIP from the duodenum → GIP stimulates the pancreas to secrete insulin → insulin-dependent tissues (mainly in skeletal muscle)
What does insulin do in respect to carbohydrate digestion?
In skeletal muscles there are glucose transporters located inside the cell → you want the transporter to be located on the membrane to absorb glucose → to change the location of the transporter, insulin is needed (similar to how aquaporins needed ADH to translocate them from inside the cell to the cell membrane) → glucose can now be absorbed inside the cell
What other stimulation does glucose receptors respond to? What is the application (referring to diabetics)?
There is another set of glucose transporters in the cell which DON’T respond to insulin, but rather they respond to MUSCLE CONTRACTIONS → therefore, if you exercise you will not need insulin in order to absorb glucose since the muscle contractions allows glucose transporters to be on the membrane to absorb more glucose → therefore, when you exercise, insulin secretion decreases
APPLICATION: People who are diabetic, need a readily form of glucose so by chance, when insulin is injected and they exercise (insulin + muscle contractions) → muscle will suck up all the glucose, leaving very little for the brain → can lead to hypoglycemia
What are insulin-independent tissues?
They don’t depend upon insulin (like RBC in the brain) because the glucose transporters are already on the membrane
What does the ileum release in response to carbohydrate digestion?
Ileum releases GLP-1
Ozempic is a GLP-1 agonist which mimics GLP-1
GLP-1 can also stimulate the pancreas to secrete insulin → this GLP-1 induces another sensation of satiety → it makes you feel full which leads to weight loss
Very effective for Type II diabetes, since many Type II diabetics are also obese
What is the glucose paradox briefly?
The first organ to be exposed to glucose consumed is the liver → the liver wants to retain/expected to keep that glucose → HOWEVER, most of the glucose you consume ends up leaving the liver anyway
How does glucose leave the liver and go to other cells?
If you want glucose to stay in a cell, a phosphate is needed on the 6th carbon of glucose → the enzyme in the liver that does this is glucokinase and in the skeletal muscle is hexokinase
Although they both do the same thing, the Km of glucokinase is 10 mM while the Km of hexokinase is 0.1 mM → this means that hexokinase works much faster than glucokinase (it only takes 0.1mM of hexokinase to get to half of Vmax)
Which organs have gluconeogenic properties?
kidneys and the liver
What does the large intestine do briefly?
The large intestine packages any undigested food for secretion (feces)
Almost 98% of carbohydrates are digested and absorbed, the exception is someone who is lactose intolerant
What happens to those who are lactose intolerant who consume dairy?
There is not enough/no lactase to break down lactose → leads to gastrointestinal distress/diarrhea since there are lots of solutes that are not absorbed → water follows solutes
How are artificial sweeteners digested and absorbed?
there are artificial sweeteners, because the body doesn’t recognize it → it is not digested → it is not absorbed → that’s why artificial sweeteners have 0 calories → there is no gastrointestinal distress even though it is not absorbed because artificial sweeteners are hundreds of times sweeter than sugar → therefore, you don’t need much artificial sweetener to trick your taste buds → therefore, there is not enough to cause distress
How is fiber digested and absorbed?
you can consume fiber (also is glucose) → but the fiber/glucose is structured differently → in fiber, glucose is structured differently in a way which your body can not break it down → the solute ends up in the large intestine → attracts water → helps with constipation
What is fat (what is it comprised of)?
Fat = 3-carbon glycerol and has three fatty acids attached (each are 16-C long)
Fat is a really large molecule
Therefore, simplest molecule is the individual fatty acid
What breaks down fat?
lipase
What is the issue with breaking down fat?
fat is non-polar and lipase is polar
What happens at the mouth when digesting fat?
Mechanical digestion still takes place: you break down the clump of triglycerides
Chemical digestion= lingual lipase → breaks off some fatty acid chains on the outside of the clump of triglycerides since the ones on the inside of the clump are surrounded by the nonpolar triglycerides
What happens in the stomach when digesting fat?
In the stomach, HCl DOES NOT denature the lingual lipase
Instead, the stomach releases gastric lipase
What happens in the pancreas/small intestine when digesting fat?
The pancreas also releases pancreatic lipase
Enterocytes in the small intestine are epithelial cells which will release enteric lipase
What is released when fat is absorbed by the enterocytes?
CCK and enteric lipase
What is the main function of CCK?
CCK= stimulates the gallbladder to release bile (the liver makes the bile, gallbladder is where bile is stored) → bile emulsifies fat (emulsification– meaning it breaks off all the triglycerides and help the lipase to mix with the triglyceride)
What is the secondary function of CCK? What is the application?
CCK also stimulates the ventromedial hypothalamus → satiety
APPLICATION: eating slow and the meal has fat, it can stimulate CCK and create sensation of satiety → if you give your body time to stimulate CCK and reach the hypothalamus, then you may not eat as much → prevents overeating
APPLICATION: potential obesity if ventromedial hypothalamus is never stimulated → you never feel full → you keep eating
Lateral hypothalamus stimulated = hunger
When blood glucose is low, your lateral hypothalamus is stimulated to make you hungry
APPLICATION: overstimulation of lateral hypothalamus makes you overly hungry → leads to overeating
CCK is how the polar lipase mixes with the nonpolar triglycerides
Which organs can release lipase?
mouth, stomach, pancreas, and small intestine
How is fat transported?
Lipases break down the TG to fatty acids → the fatty acid chains will form a micelle (micelle= fatty acid chains that bind together) → enters enterocyte → the enterocytes will reform the micelle/fatty acid chains to reform a triglyceride → the TG is packaged into a protein coat called chylomicron (if you just leave the TG without packaging, the oil will find each other and glob up, so chylomicron decreases the likelihood of this happening and minimizes TG globbing) → chylomicron is then sent to the lymphatic system → into the heart → enters the circulatory system → the chylomicron is now dispersed throughout (heart, liver, stomach, skeletal muscle, adipose tissue…)
Adipose tissue: lining the blood vessels is the endothelial cells → endothelial cells have an enzyme called LPL which breaks down the fatty acid chains of TG/chylomicron → adipose tissue takes up fatty acid and forms a TG
The body does not absorb TG as it is because it is way too big to be transported into the phospholipid bilayer → that is why fatty acid chains need to be broken down
What is alcoholic fatty liver disease?
Individual who chronically consumes alcohol → liver is the main organ of detoxification of alcohol to fatty acid → fatty acid is stored in the liver → fatty liver → liver swells and starts damaging liver cells → scar tissue is placed in replacement of the damaged liver cells → causes cirrhosis → potential death
Why is the liver NOT the first organ that sees fat?
If the liver was the first organ that was exposed to fatty acid → the liver may store fatty acid as TG in the liver → liver is swollen and cells are damaged → scar tissue is placed down → cirrhosis → liver cancer → potential death
How does uncontrolled diabetes lead to fatty liver disease?
In order to make glycerol, glucose is needed → insulin-dependent cells → glucose transporters are inside the cell → insulin is needed to change the location of the glucose transporters →if you are a Type 1 Diabetic (no insulin is secreted at all) → no glucose is allowed inside the adipocytes → no glycerol is created → no TG is formed → fat can not be stored → absence of insulin secretion interprets the body that you are not eating enough → the body activates sympathetic nervous system to cleave off fatty acid chains in the TG that you already have stored in adipose tissue → fatty acid levels in the body increase → liver will take the fat and convert it to ketones → may cause ketosis → your body’s favorite nutrient is glucose → your body is interpreting that you’re not eating enough glucose → ketones are made to cross the BBB → the brain is using ketones to make ATP (seen in starvation as well)
Diabetics will eat, but they will lose weight → no fat is being stored AND the ketones in the blood will increase (ketones can get filtered by the kidneys → kidneys will try to reabsorb ketones and glucose → but if they can’t reabsorb fast enough → ketones and glucose end up in urine)
There is plenty of glucose, fat, and ketones in the blood
Atkins diet: avoid eating glucose → leads to ketosis → may lead to keto-acidosis → pH is changing in body → coma and death
What can the liver convert a fatty acid into?
LDL (using a saturated/trans fat)
The body needs cholesterol for two reasons:
1.) steroid hormone regulation (like aldosterone, testosterone, estrogen, progesterone…)
2.) cholesterol is in phospholipid bilayers
Why is cholesterol packaged into LDL?
it's a fat-soluble molecule that cannot dissolve in the blood's water-based plasma
If blood cholesterol is high, endothelial cells can be damaged → causing atherosclerosis
Saturated fat costs less which is why many people consume saturated fat
What’s the simplest unit of proteins?
Simplest unit= amino acid
Amino acid has an amino group and a carboxylic acid
Half of the amino acids are essential, meaning it is needed that you eat it because your body can not make it
Therefore, nonessential amino acids means your body can make it
Amino acids formed together can form different types of proteins
Peptide bond connects amino acids together
What happens to protein digestion at the mouth?
Mechanical digestion is present
THERE IS NO CHEMICAL DIGESTION
What happens to protein digestion at the stomach?
HCl acid DENATURES proteins
Denaturing= the protein structure is folded in a way where the peptide bonds are easier to break
Stomach also releases pepsinogen
Pepsinogen is inactive form and the presence of HCl → forms pepsin (the active form of pepsinogen) → breaks down protein to smaller peptides
What enzymes does the pancreas release for protein digestion?
Pancreas releases trypsinogen and chymotrypsinogen into the small intestine
What enzymes does the small intestine release for protein digestion?
On the brush borders of the small intestine, enterokinase converts trypsinogen into trypsin
Peptidase is also found on the brush borders and it breaks down the peptide bonds of the last 2-3 amino acids put together (similar to how there is sucrase, maltase, or lactase to break down two structure bonds)
Chymotrypsinogen is converted into chymotrypsin by TRYPSIN
Chymotrypsin is a lot more effective in breaking peptide bonds
Inactive enzymes are released and where the food is located, that’s where the enzymes are activated
This occurs so that the body doesn’t break down protein structures present in the cell that IS NOT food
What is the difference between afferent and efferent system?
Afferent system = soma receptors or special senses
Afferent system leads to the brain
Efferent system= somatic or autonomic
Autonomic= can be parasympathetic or sympathetic
This parasympathetic and sympathetic is the enteric system (aka digestive system)
Enteric system can function INDEPENDENTLY of the brain– that’s why it’s labeled as a “system”
Primary system we use to activate the enteric system is the parasympathetic (we want to absorb those nutrients since sympathetic focuses on breaking down the nutrients)
The nerve responsible for activating the enteric system is the vagus nerve
Efferent system is stemming from the brain towards the enteric system
What are the phases of digestion (explain each step)?
1.) Cephalic
Can be activated with the mere sight and smell of food
One of the things secreted is called gastrin (primarily secreted by the stomach)
May stimulate peristaltic motion (stomach is starting to move to prepare for consuming food)-- also stimulates HCl in the stomach
Explains why your stomach “growls” when you are hungry
2.) Gastric
You significantly increase gastrin since you are actively eating the food now
Stomach releases a lot of HCl in the stomach
3.) Intestinal
Increase the release of secretin
Secretin stimulates the secretion of enzymes from the pancreas
What is chyme?
Chyme is a semiliquid mass (mixed with HCl) of partially digested food that the stomach releases into the duodenum, the first part of the small intestine
Once chyme leaves the stomach, acid is neutralized to optimize enzyme activity from the bicarbonate ion to neutralize the acid that is mixed with the food
More water is added since it is easier to mix enzymes and food when in water
What is peristaltic rush?
You want a slow peristaltic motion to maximize digestion and absorption
HOWEVER, the exception is when you consume a pathogen
There are lymph nodes (detects pathogens) in digestive tract and respiratory tract
You want a lot of lymph nodes here since its the two primary entries for pathogens
In the digestive tract, if it detects a pathogen, it’s going to speed up peristaltic motion
—>This limits the ability to digest food → limits ability to absorb that pathogen → goes to large intestine → solutes attract water → causes diarrhea
How does your body release HCl?
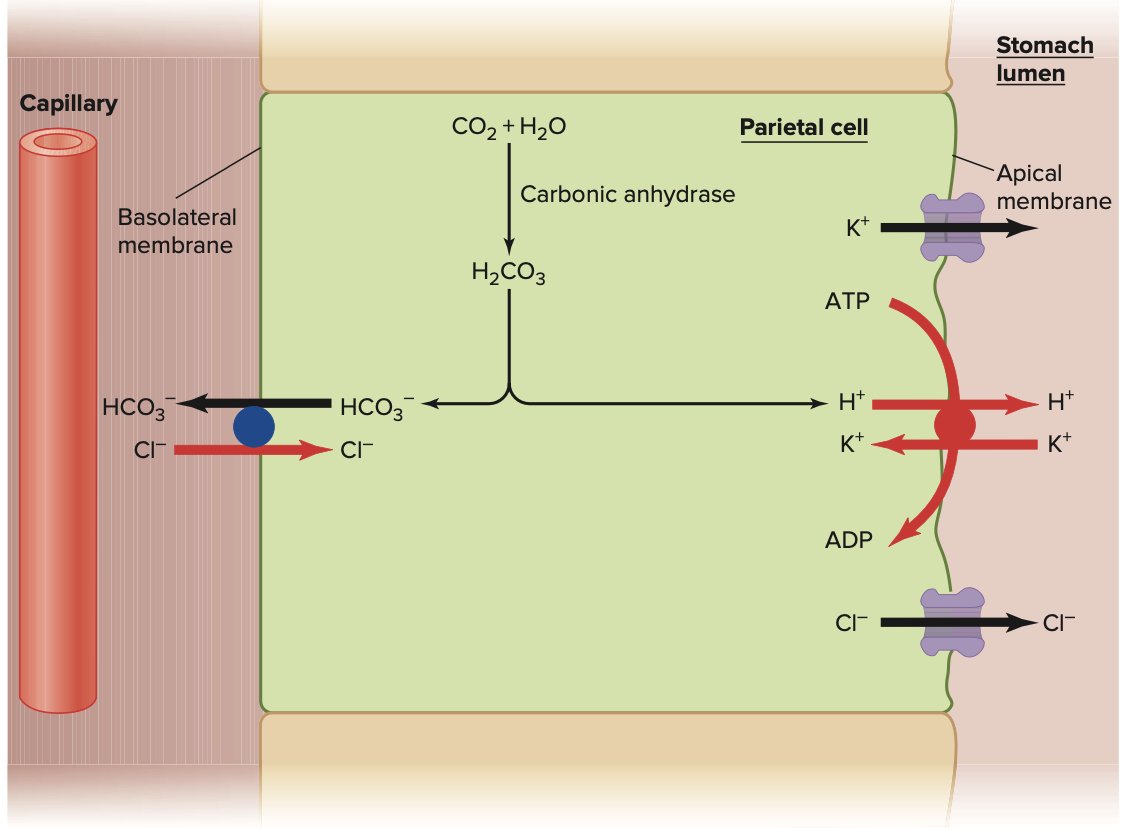
(REFER TO IMAGE)
When your body releases gastrin → different types of cells in the stomach respond to the gastrin named parietal cells (pushes more HCl to where the food is) → gastrin binds to receptor → stimulates Gs protein → converts ATP → cAMP → cAMP changes the location of H+/K+ pumps located in the cells to the membrane of the cell (translocation) → the H+/K+ pump exchanges potassium in for proton out → the proton/H+ came from CO2 + H2O → HCO3- + H+ → the bicarbonate ion is transported out in exchange for chloride in → the chloride exits to where the food is → the H+ and Cl- combine to form HCl → HCl converts pepsinogen to pepsin, kills bacteria, denatures protein
How do you buffer HCl?
Occurs in pancreas and duodenum
Chyme (mixed with HCl) leaves the stomach and now it enters the small intestine (duodenum) → the acid is neutralized/buffered so that you can optimize enzyme activity
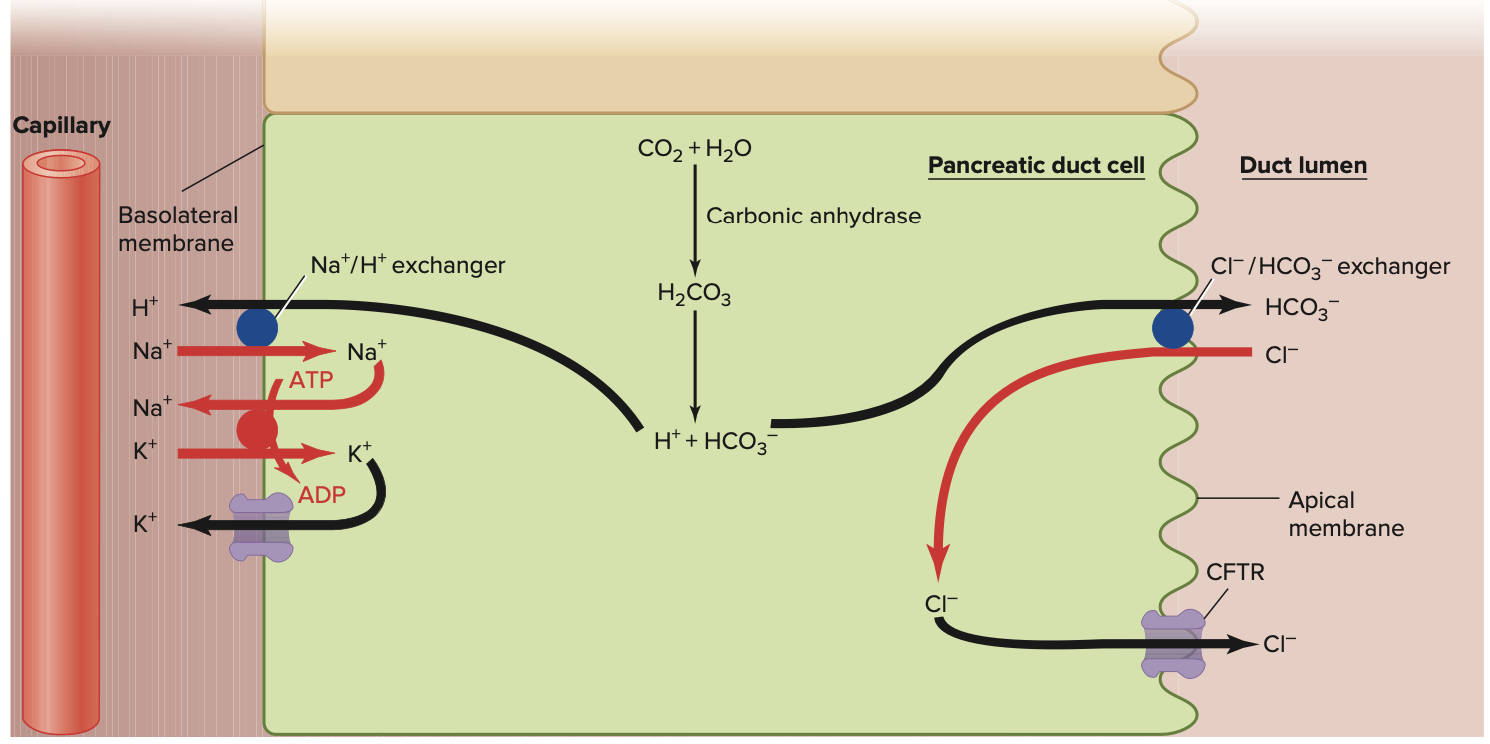
Secretin activates Na+/H+ proton exchange on the basolateral side → sodium goes in for proton out → proton combines with bicarbonate ion to form H2CO3 + CO2 +H2O → CO2 enters the cell and combines with water → it forms H2CO3 → the H2CO3 forms bicarbonate ion and leaves the cell in exchange for a Cl- in to buffer the chyme → the H+ removal from the H2CO3 will fuel the Na+ proton exchanger
HCl + HCO3- → H2CO3 → CO2 + H2O
How do you add more water to the chyme to mix the food with enzymes better and to easily pass the chyme through the small intestine?
(REFER TO IMAGE)
Gastrin also stimulates the crypts of lieberkuhn cells to form cAMP and activate the CFTR (cystic fibrosis transmembrane conductance regulator) → chloride channel opens allowing chloride to leave (since chloride came into the cell previously in exchange for bicarbonate ion and chloride also comes in through NKCC channel) → When chloride leaves, Na+ also follows chloride → water follows solutes
Difference: in the kidneys, sodium was main importance and transporter, in this case, CHLORIDE is main transporter
Describe peristalsis
There are smooth muscle cells lining small intestine
There is also cells of cajal (pacemaker cells) lining the small intestine
Cells of cajal stimulate the smooth muscle cells, but they DO NOT bring the smooth muscle cells to threshold
If you eat food, the parasympathetic nervous system is activated which is stimulated by the vagus cranial nerve → the vagus nerve sends impulses to the digestive tract through the mesenteric plexus → mesenteric plexus is responsible for bringing the smooth muscle cells to threshold → these smooth muscle cells are unitary → allows for peristalsis
Peristalsis= cells are not stimulated simultaneously, it creates a wave-like effect → splits up the food into smaller segments called segmentation → allows for more absorption
Where does digestion take place in the SI, how about absorption?
While enzymes are on the troughs of the SI, the absorption takes place on the peaks of the SI
Describe absorption of glucose, A.A, and galactose
Na+/K+ concentration gradient pump → Na+ is mixed with the food → concentration gradient allows Na+ to enter the cell → glucose is absorbed through secondary active transport → as Na+ goes in the cell, glucose follows
This happens same with galactose, and amino acids
Describe absorption of fat
Enters as a micelle and transported as a chylomicron
Describe absorption of fructose (what is the application)
Through facilitated diffusion → need a transporter to follow the concentration gradient
Secondary active transport is much faster than facilitated diffusion
APPLICATION: overconsumption of fructose → overwhelms the fructose transporters → fructose ends up in long intestine → solute attracts water → causes diarrhea
Describe absorption of calcium
Once again, there is always a Na+/K+ ATPase pump on the basolateral side
Calcium is absorbed via concentration gradient → sodium wants to come in the cell, for calcium out → therefore, calcium outside the cell will always want to come back in
Best source of calcium is milk since there is vitamin D → Vitamin D can get transported into the cell → activates the Calcium ATPase pump which means calcium is rapidly pumped out → creates even greater concentration gradient so calcium will want to enter the cell
Describe how you reabsorb water in the ileum of the small intestine
You want to reabsorb some of the water back
Na+/K+ ATPase pump always on the basolateral side → Na+ is motivated to enter the cell → Cl- is motivated to reenter the basolateral side by following the sodium → water follows solutes (PARACELLULARLY)
How does reabsorption of water occur in the colon?
Absorption of water is different
Now, water is absorbed transcellular (as long as there are not a lot of solutes on the food side)