Unit 4 - Health psychology (psych)
1/60
Earn XP
Description and Tags
FINAL TOPIC! you got this, not long now - push through and achieve what i know you can :)
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms
Stress
The non-specific response of the body to any demand
Demands can be psychological or physiological
To experience stress = stressor must be present
Two types of stress (Selye, 1936)
Distress
Eustress
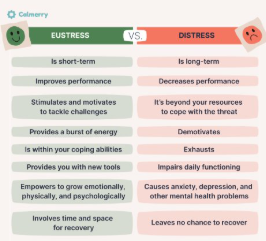
Distress (Two types of stress (Selye, 1936))
The negative psychological response to a stressor, indicated by the presence of negative psychological states (e.g. fear, anger)
Impedes ability to perform at an optimal level
Can lead to health risks
Experiences that can trigger include death of a loved one, financial difficulties, conflict
Eustress (Two types of stress (Selye, 1936))
The positive psychological response to a stressor, indicated by the presence of positive psychological states
Improves performance/motivation
Increases alertness and energy levels → optimum performance when facing challenging situation
Experiences that can trigger include exam, graduating, driving test, starting a new job, interview, skydiving, etc
Stressor
Any person, object or event that challenges or threatens an individual, thus causing feelings of stress
*they are sources of stress
4 types of stressors (Selye, 1936) (define each as well)
Environmental stressors: stems from conditions + physical surroundings of an individual e.g. noise, temp, smell, pollution, etc
Psychological stressors: stems from emotional and cognitive factors e.g. graduating, new job, buying house
Social stressors: stems from relationships and interactions with society e.g. peer pressure + conflict with friends/family
Cultural stressors: stems from cultural identity, values and cultural norms e.g. discrimination or loss of cultural practices
3 characteristics of stressors
Nature: can be categorised as environmental, psychological, social or cultural
Duration: can be short term (acute) or long term (chronic)
Strength: the severity/intensity of the stressor can range from mild to severe
Stress as a response
General Adaptation Syndrome (GAS) model (Selye, 1936)
Describes the physiological changes that the body automatically goes through when it responds to stress
2 physiological changes when exposed to a stressor and experience stress (Selye, 1936)
Heart rate increases
Breathing rate increases
3 stages of the GAS model (Selye, 1936)
Alarm
Resistance
Exhaustion
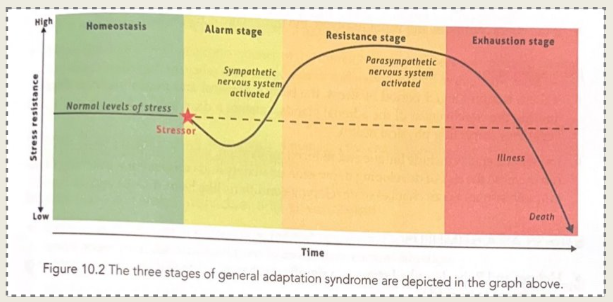
Alarm - GAS model stage (Selye, 1936)
The initial response to a stressor (one of the 4 types). Has 2 substages:
Shock: when we first perceive threat, body’s resistance drops below normal - responds as if it has been injured, physical effects makes person feel momentarily helpless
Countershock: after shock stage, body rebounds and sympathetic NS activates to prepare for fight or flight
The amygdala detects threat and signals the hypothalamus to initiate the SNS
When signal reaches adrenal glands, it triggers the release of adrenaline, noradrenaline and cortisol (stress hormones)
*countershock occurs 6-48 hours after initial stressor is detected
Hormones in alarm stage (GAS model, Selye 1936)
THEY ARE ALL SECRETED FROM ADRENAL GLANDS
Cortisol:
When body experiences stress, it increases pain tolerance but reduces performance of immune system and cognitive abilities
Adrenaline:
Increases heart rate and supports conversion of glycogen into glucose
Noradrenaline:
Causes blood vessels to constrict and blood pressure to increase
Resistance - GAS model stage (Selye, 1936)
If stressor remains = body enters this stage → attempts to restabilise its internal systems and fight stressor
Body tries to repair itself from initial shock by reducing SNS, initiating Parasympathetic NS to counteract SNS’s heightened arousal
Stress hormones continue to be secreted to help the body cope
Energy is directed to managing the stress
Exhaustion - GAS model stage (Selye, 1936)
Occurs if stressor continues for a prolonged period
Adrenal glands lose effectiveness, blood sugar drops and physical health declines
The body’s resources become depleted, leading to…
fatigue, low motivation, impaired immunity, and increased risk of mental illness and physical illness
Stress as a stimulus
Holmes and Rahe (1967)
Describes stress as a significant change in life that requires an adjustment to be made
Assumes:
Life changes are stressful events that will cause the development of physical/mental illness if change exceeds a general limit of adjustment
Levels of adjustment are similar among everyone
According to the theory, personality, life experiences and social support do not affect the impact of stress or adjustments
Social Readjustment Scale (SRS) - Holmes and Rahe, 1967
*also referred to as the Holmes and Rahe Stress Scale
Assesses amount of stress experienced by an individual in the past year
Comprises of 43 life events that are allocated a score between 1-100
These scores = life change unit (LCU) = estimates amount of readjustment required if event is experienced
Individual indicates events experienced in past year + their LCU’s are added to equal their final score of total stress readjustment
Likeliness of developing a physical/mental illness can be calculated through this
Strength and limitations of the Social Readjustment Scale (SRS) (Holmes and Rahe, 1967)
Strength:
Quantitative data is collected, easy to statistically analyse
Limitations:
Checklist = subjective measure, can allow for exaggerated responses
No reasoning for responses, limiting richness of the data
Stress as a transaction
Lazarus and Folkman, 1984
Suggests individuals utilise their perception of a stressful situation + their subjective past experiences to help them cope
Stress response depends on emotions and psychological factors unique to the individual
Emphasises relationship between person and characteristics of event that took place
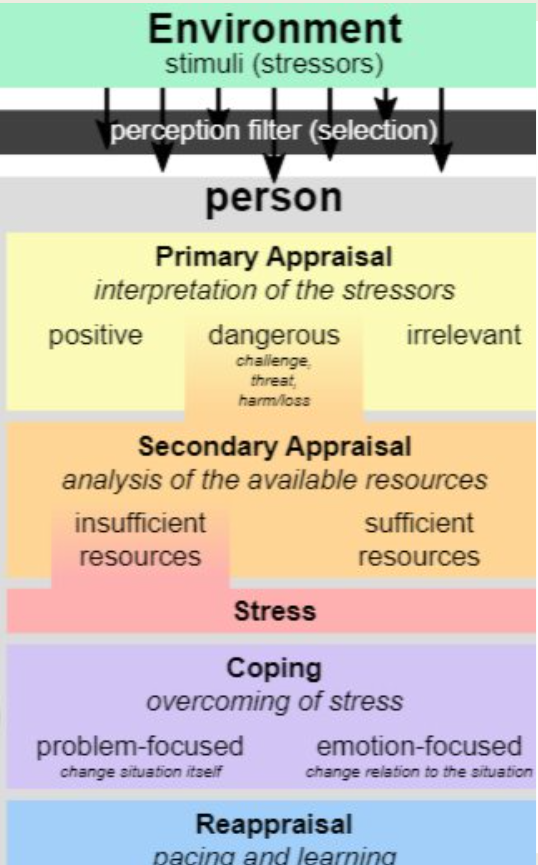
Role of cognitive appraisal (Lazarus and Folkman, 1984)
Refers to cognitive abilities used to assess situations
Stress is present when an individual cognitively appraises an event as stressful
Stages within the transactional model of stress (Lazarus and Folkman, 1984)
Primary appraisal: notice a stressor in the environment, decide how important the event is to ones wellbeing. Can be:
Irrelevant
Positive
A challenge or threat/loss risk = STRESSFUL CATEGORY - if it is either of these, proceed to secondary appraisal
Secondary appraisal: assesses both the internal and the external resources that are available, and evaluate whether they can meet the demands of the stressor
if they believe they have resources to cope = positive secondary appraisal = no stress/eustress
if they feel demands of stressor exceeds ability to cope = negative secondary appraisal = distress
*secondary appraisal does not necessarily happen after primary appraisal
Two methods of coping
Emotion focused coping:
Goal = manage emotional reactions to stress. Used when individual perceives that they don’t have the resources to deal with the stressor
e.g. meditation, relaxation techniques, talk therapy, systemic desensitisation, etc
Problem focused coping:
Goal = address the root cause of the stress. Used when an individual perceives that they do have the resources to deal with the stressor
e.g. pitch at work, quitting a job, etc
Two types of coping strategies for stress
Maladaptive coping: involve harmful and unhealthy stress management that worsens negative effects of stress.
Avoids dealing with stressors that are causing problems.
e.g. negative self-talk, denial, substance abuse, withdrawing from society, rumination (repetitive thoughts), self blame, procrastination
Adaptive coping: involve beneficial and productive stress management that decreases the negative effects of stress
e.g. meditation, exercise, positive reframing, planning, acceptance, humour, emotional support by talking to others
Sleep
Refers to periods of altered/loss of consciousness
Sleep latency
The length of time it takes to fall asleep
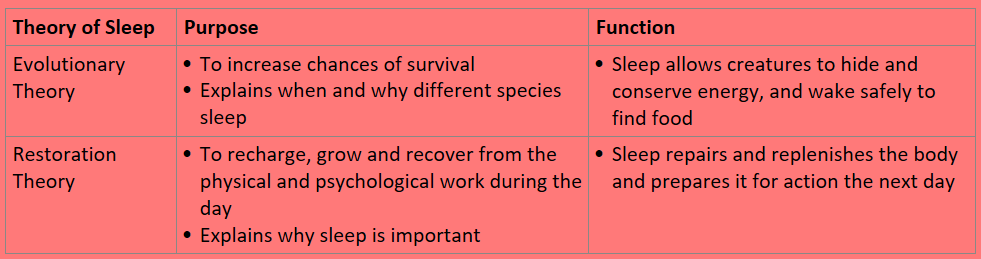
Evolutionary purpose of sleep
States sleep serves as a means to increase an animals or humans chance of survival in its environment
Early humans used daytime instead of night to eat, drink and reproduce as there was greater risk of injury/predators in the dark that could threaten survival
Sleep depends on animals vulnerability to predators + the animals need to find food
Sleeping at night allowed for energy to be conserved
Restorative purpose of sleep
States sleep allows us to recharge, grow and recover from physical and psychological work during the day
Claims homeostasis of the body is disrupted when humans are awake → sleep acts to restore it
Sleeping allows energy levels that decline during wakefulness to be restored:
Repairs and replenishes body
Increases alertness
Increases immunity to disease
Comparison of purposes of sleep
Sleep wake cycle
The recurring pattern of wakefulness and sleep that individuals undergo on a daily basis
Measured by recording times of regular events e.g. eating and sleeping
Regulated by the circadian rhythm, body temperature, metabolic rate, and release of hormones
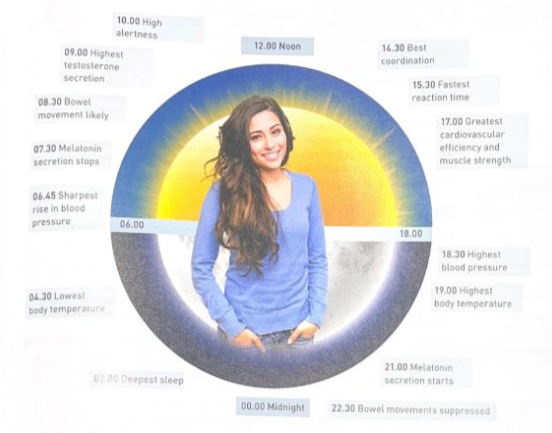
Circadian rhythm
The biological cycle that lasts around 24 hours and controls the nocturnal release of hormones including melatonin
For humans, dominant circadian rhythm = sleep wake cycle
This is largely controlled by suprachiasmatic nucleus = the internal body clock located in the hypothalamus
Melatonin
The hormone that regulates the sleep wake cycle
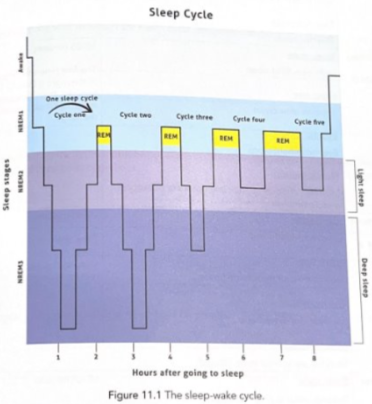
4 distinct stages of the sleep cycle
There are 3 non-REM stages and one REM
REM = rapid eye movement
NREM = non-rapid eye movement
Non Rapid Eye Movement (4 distinct stages of the sleep cycle)
Sleep state: transitional period between wakefulness and sleep
Heart rate decreases
Eye movements are a slow rolling movement (once asleep they stop moving)
Muscles relax
Length of stage: 1-7 minutes
If uninterrupted, individuals quickly move into NREM 2 and minimal time spent in this stage
Non Rapid Eye Movement (4 distinct stages of the sleep cycle)
Sleep state: light NREM sleep
Heart rate slows down
Eye movements stop
Muscles continue to relax + there are occasional muscle twitches
Length of stage: 10-25 minutes
First time stage occurs = lasts 10-25 minutes, then increases in length with each repetition
Non Rapid Eye Movement (4 distinct stages of the sleep cycle)
Sleep state: deep NREM sleep
Heart rate continues slowing down
Minimal eye movement
Muscles are at most relaxed state
Length of stage: 20-40 minutes
First few stages = lasts 20-40 minutes, then reduces in length
Rapid Eye Movement (4 distinct stages of the sleep cycle)
Sleep state: dreams occur during this stage
Heart rate increases to match the rate when awake (varies based on dream content)
Rapid eye movement, visual information is not transmitted to the brain
Muscles are temporarily paralysed (except for breathing and eye movement)
Involves a high level of brain activity
Length of stage: 10-60 minutes
Stage increases in duration over the night ranging from a few minutes to one hour
Order of stages within each sleep cycle
Sleeper enters stage 1 NREM sleep (usually happens only once per night)
Then sleeper progresses through stages 2 + 3, reaching deeper sleep
They then reverse back to stage 2 before entering REM sleep
e.g. NREM stage 1→ stage 2 → stage 3 → stage 2 → REM
After first cycle, sequence typically becomes: stage 2 → stage 3 → stage 2 → REM
Sleep cycles throughout the night and purpose of NREM/REM sleep
Each night of sleep is made up of 4-6 sleep cycles lasting approx 90-110 min (first cycle is 90 min)
From third cycle →, stage 2 NREM and REM lasts longer whilst stage 3 NREM becomes shorter
In fourth, fifth and sixth cycle, stage 3 NREM = rare, more time spent in REM
There is evidence that:
NREM sleep (stage 3) = involved with restoring the body and physical energy
REM sleep = important for restoring brain function e.g. memory and concentration
These cycles can be visualised as a hypnogram
Sleep deprivation
The condition of not getting sufficient sleep
Causes for sleep deprivation
Shift work
Drugs
Sleep environment
Stressors
Shift work (causes of sleep deprivation)
Involves altering sleep wake cycle and consequently reducing the amount and quality of sleep
Trouble sleeping is caused by the disruption of hormones that regulate the sleep wake cycle + circadian rhythm, and the lack of zeitgebers (person is no longer given signals when to wake up/fall asleep)
Drugs (causes of sleep deprivation)
Some drugs impact sleep stage progression/quality, reducing NREM sleep + affecting REM sleep
Caffeine is a stimulant drug, it speeds up the CNS
Alcohol is a depressant, it slows down the CNS - when it wears off it causes people to wake up
Alcohol and caffeine both negatively impact sleep
Sleep environment (causes of sleep deprivation)
A bright environment (reduces melatonin) and/or loud environment (wakes people up) can disrupt the sleep wake cycle
Stressors (causes of sleep deprivation)
Stressors cause anxiety which can cause issues falling and staying asleep
e.g. test/exam, headache (illness), school, etc
2 types of sleep deprivation
Partial sleep deprivation
Chronic sleep deprivation
Partial/acute sleep derivation (2 types of sleep deprivation)
The severe reduction or complete lack of sleep over a short period.
No exact number constitutes this - generally less than 5 hours of sleep over 24 hours
Can be due to disruptions to the normal progression/sequence of sleep stages → fragmented sleep and decreased quality
Immediate effects can typically be reversed with adequate sleep
Common causes: staying up to finish an assignment, illness/sickness, jet lag, pulling an all nighter, stress
Chronic sleep deprivation (2 types of sleep deprivation)
The persistent reduction of sleep over a long period of time.
Inadequate sleep for more than a few weeks at a time, sometimes lasting years
The consequences are more detrimental than those caused by partial sleep deprivation
Common causes: insomnia, sleep disturbances, work hours, life style choices
Effects of partial sleep deprivation
Attention: lapses in attention increase when sleep deprived
Mood: can decrease mood and cause irritability
Reflex speed: reaction times tend to become higher which means it takes longer to react to stimuli
Vision: can become blurry, eye twitches (spasms) may occur and eyes become more sensitive to light
*reversible once adequate sleep is achieved
Effects of chronic sleep deprivation
Heart disease: increased blood pressure + high cholesterol are effects, both possibly leading to heart disease
Obesity: individuals increasing intake of high energy foods as well as amount of food they eat
Insomnia: a sleep disorder involving difficulties falling asleep or staying asleep (low sleep latency). Also common to wake up not feeling well rested
Anxiety: emotional regulation is negatively affected by this, possibly worsening symptoms of anxiety
Sleep hygiene
The behaviour and sleep environment that results in a healthy sleep
Zeitgebers
Cues in the environment that provide signals to our brains to do things at certain times. Sleep wake can be improved by exposure to correct zeitgebers at appropriate times
e.g. light → when brain receives lower levels of light, SCN signals the release of melatonin, making us feel drowsy and promoting sleep
e.g. if you brush you teeth, put on pjs and read a book prior to sleep every night, this routine will signal your brain that its time to sleep
3 techniques to improve sleep hygiene
Management of electronic devices
Consistent sleep patterns
Sleep environment
Management of electronic devices (3 techniques to improve sleep hygiene)
It is recommended that electronic device use is ceased one hour prior to bedtime
They emit blue light that prevents melatonin production - disrupting circadian rhythm which makes it difficult to fall asleep
Results in brain simulation that reduces both sleep quality and duration, due to heightened cognitive arousal
Consistent sleep patterns (3 techniques to improve sleep hygiene)
Critical for good sleep = regulates the circadian rhythm. This increases amount of sleep.
Consistent bed time and wake time can help prevent sleep deprivation, can achieve this by getting recommended sleep hours based on age
Sleep environment (3 techniques to improve sleep hygiene)
Circadian rhythm can change due to uncomfortable sleeping space
Bedroom should be free of distractions like electronic devices
Bed should be used for sleeping and intimacy only - creates a cognitive link between bed and sleep
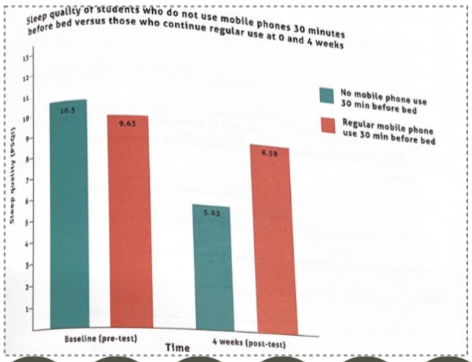
Aim (Restricting Bedtime Mobile Phone Use, He et al 2020)
To determine how limiting the use of mobile phones before bedtime affects mood, working memory, pre-sleep arousal, sleep quality and sleep habits.
Method (Restricting Bedtime Mobile Phone Use, He et al 2020)
Participants: 38 University students with habit of using their mobile phone before bed AND experience poor sleep quality.
Materials: Positive and Negative Affect Schedule (PANSAS), n-back task, Pre-Sleep Arousal Scale (PSAS), Pittsburgh Sleep Quality Index (PSQI) and an online sleep diary.
Design:
IV = use of mobile phones during bedtime vs no mobile phone use for 30 minutes before bedtime.
DV = mood, working memory, pre-sleep arousal, sleep quality and sleep habits
Procedure (Restricting Bedtime Mobile Phone Use, He et al 2020)
Researchers obtained ethics approval from the Ethics Committee. Participants volunteered (via social media) and signed online informed consent sheets
Participants completed all tests to gain a baseline of results
Participants were randomly assigned to experimental group with restricted mobile phone use or control group with no restrictions (19 in each)
For the next 4 weeks, participants in experimental group did not use mobile phones for 30 minutes prior to bedtime. Participants in control group continued with normal mobile phone use.
At the four week mark, participants completed the same tests as sat during pretesting and these were compared.
Tools for measuring sleep used in He et al study
Positive and Negative Affect Scale (PANSAS) = subjective quantitative (likert)
n-Back Task = objective quantitative
Pre-sleep Arousal Scale (PSAS) = subjective quantitative (likert)
Pittsburgh Sleep Quality Index (PSQI) = subjective quantitative
Online sleep diary = qualitative (survey)
Key findings (Restricting Bedtime Mobile Phone Use, He et al 2020)
Participants who had restricted mobile phone use had positive benefits (1 mark, if more, list the benefits shown below):
Improved positive affect and reduced negative affect
Improvement in their working memory
Reduced pre-sleep arousal
Improved quality of sleep
Take less time to fall asleep and stayed asleep for longer
Contributions to psychology (Restricting Bedtime Mobile Phone Use, He et al 2020)
Recent study that uses well established measures, allowing it to be replicated by other researchers
With replication comes the ability to assess reliability
Criticisms/limitations (Restricting Bedtime Mobile Phone Use, He et al 2020)
Sample characteristics: small sample size limits the ability to generalise results to the population
Self report measures: as all measures except for the n-back task were self reports, the data was subjective and open to bias