Old medsurge Final
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
65 Terms
Increased Intracranial Pressure ICP
pressure exerted by the volume of the intracranial contents within the cranial vault
Core principles:
The cranial vault is comprised of brain tissue, blood, and CSF, which are typically in equilibrium and produce stable ICP.
Monroe-Kellie hypothesis – there is only so much space for each component. An increase in one will result in a change in the volume of the others to stabilize ICP.
Etiologies:
Head injury/ trauma
Skull fracture
Hematoma
Brain tumors
meningitis complications
Subarachnoid hemorrhage
Toxic and viral encephalopathies
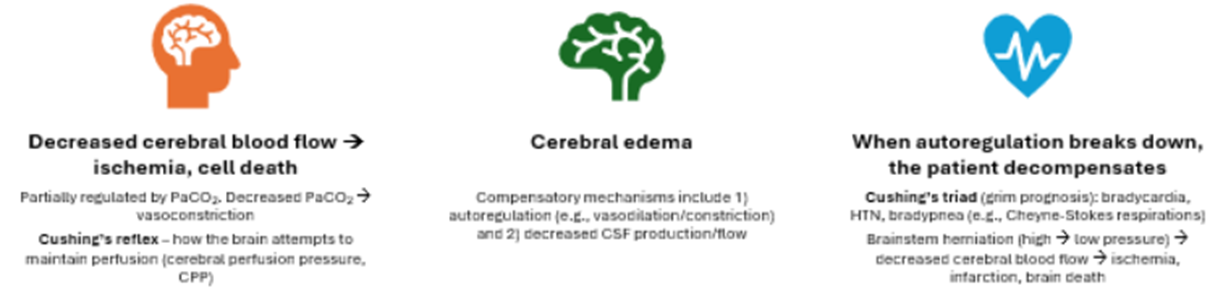
Decreased cerebral perfusion → cerebral edema → shifting of brain tissue → herniation → death
NEVER DO A LUMBAR PUNCTURE
ICP parameters
Normal ICP
0-10mm Hg
15 id high-normal
Increased ICP
16-20mm Hg]
Danger zone
25mm Ha
Movement can cause a transient increase in ICP, which should be momentary and self-regulate
Cushing’s triad
Wide BP, Low Pulse, Irratic respirations
ex) BP 168/58, P 58, RR 10
Cushing’s response (also called Cushing’s reflex) is seen when cerebral blood flow decreases significantly.
ICP Clinical manifestations
Early
Altered mentation
Confusion
irritability
visual changes
Pupillary changes (sluggish), impaired EOM (CN II, III, IV, VI)
Focal weakness, hemiparesis
Headache
Constant
Increasing in intensity
Aggravated by movement or straining
Late
LOC → comatose (GCS 8 or less)
FEVER
VS changes
Decreased or erratic HR, RR
Increased SBP, pulse pressure (SBP-DBP)
Irregular respiratory patterns
Cheyne-Stokes – long, labored, shallow, apnea
Projectile vomiting 2/2 medullar depression
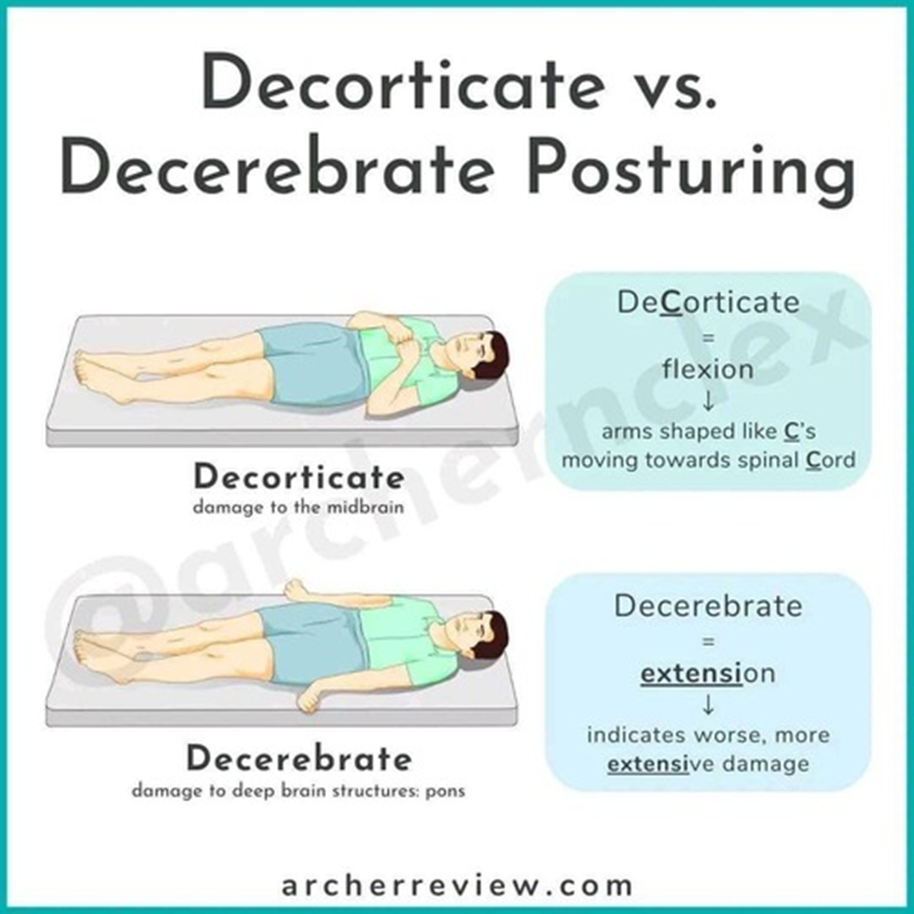
Pressure on brainstem → hemiplegia, decorticate or decerebrate posturing, bilateral flaccidity
Loss of brainstem reflexes – pupillary, corneal, gag, swallowing
ICP diagnostics
Neuroimaging – CT, MRI most commonly
Transcranial doppler – measures cerebral blood flow
NEVER ATTEMPT LUMBAR PUNCTURE IN A PATIENT WITH SUSPECTED OR CONFIRMED INCREASED ICP

ICP complications
Neuroendocrine derangements
Neurogenic diabetes insipidus → decreased ADH → volume depletion
Vasopressin
SIADH → increased ADH → volume overload
Urine output > 200 mL/hr for 2 consecutive hours
Herniation → decreased cerebral blood flow → ischemia → infarction → brain death
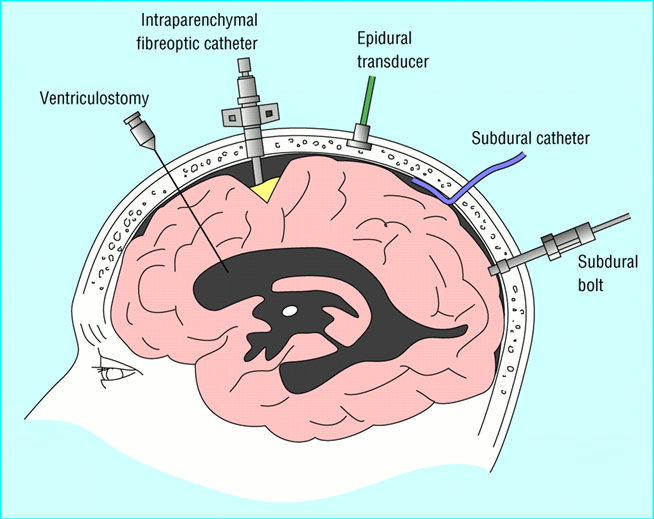
ICP Monitoring
Invasive
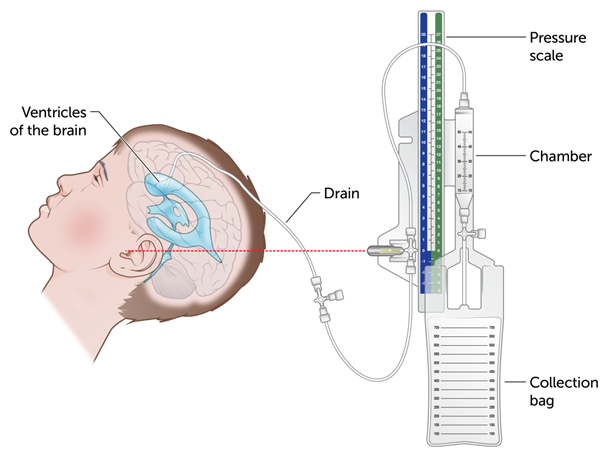
Intraventricular catheter/extra-ventricular drain (EVD)
Complications include infection, meningitis, ventricular collapse, catheter occlusion, problems with monitoring system
Aseptic technique
Continuous drainage of CSF under pressure control is an effective method of treating intracranial hypertension.
Subarachnoid screw/bolt
Complications include infection, screw occlusion by clot or brain tissue
output is recorded on an oscilloscope not requiring a ventricular puncture
ICP Medical Management
Goal is to immediately 1) decrease cerebral edema, 2) decrease the volume of CSF or 3) decrease cerebral blood volume while maintaining cerebral perfusion
Osmotic diuretics
mannitol
3% NS
Corticosteroids if 2/2 tumor
Fluid restriction
Draining CSF – via EVD, NOT LP
Reducing metabolic demands
fever management
hypothermia?
reduce O2 needed
Decompressive hemicraniectomy
last result
Maintain hemodynamic stability, cerebral perfusion
Ionotropes (dobutamine, norepinephrine) → increased cardiac output
Monitor fluids and electrolytes
Foley
Serum osmolality, electrolytes
ICP Nursing process
Assessment
Pertinent PMHx – may be obtained from family/friends
Initial neurologic exam must be as comprehensive as possible
Subsequent exams care more focused – pupil checks, specific CNs, GCS
Monitoring of VS and ICP
Diagnoses
Impaired breathing
Risk for ineffective tissue perfusion
Hypovolemia 2/2 fluid restriction
Risk for infection associated with ICP monitoring
Beware of activities or interventions that may increase ICP, minimize intraabdominal/thoracic pressure
Be mindful of patient positioning, movement, turning
Avoid Valsalva – YES to stool softeners, NO to enemas; exhale with movement
Space out nursing interventions, promote calm environment
ICP should not increase beyond 25 mm Hg, and should normalize within ~ 5 min
Otherwise, may need sedation
Planning
Maintaining patent airway (A)
Suction with caution (up to 15s)
Pre-oxygenate with 100% O2 if on mechanical ventilator
Coughing discouraged bc increases ICP
Normalizing respiratory pattern (B)
Optimizing cerebral tissue perfusion (C)
HOB @ 30-45º; keep head in neutral, midline position
Hyperventilation → decreased PaCO2 → cerebral vasoconstriction?
Monitor ABGs
Maintain negative fluid balance
3% saline
Osmotic and loop diuretics
Fluid restriction – assess VS, skin turgor, mucous membranes, urine output (Foley), serum/urine osmolality; oral hygiene, perioral care
*Fluid replacement – slow to moderate rate
Mannitol, hypertonic saline - fluid shifts from intracellular → intravascular
Increased cardiac workload – monitor for pulmonary edema, heart failure
monitor urine osmolality, obtain I/O, accurately record ICP readings
urine output is monitored hourly.
Preventing infection
Aseptic technique when managing EVD system
Always examine CSF
usually clear
Monitor for meningitis
Monitor for other signs of local, systemic infection
Monitoring and managing potential complications
Assess, document, notify
Monitor for sustained increased ICP
STROKE
AKA CVA(cerebrovascular accident)
Sudden Impairment of cerebral circulation in 1 or more BV supplying the brain
Tissues fail to receive O2→necrosis
Third leading cause of death
Leading cause of long-term disability
Symptoms and signs depend on the vascular territory affected in brain.
Most common: middle cerebral artery
TYPES:
Ischemic (87%)
Thrombotic (45%)
LVO’s/Large vessel occlusions
Small penetrating artery thrombosis/lacunar
Cryptogenic (30%)
unknown etiology
Cardioembolic (20%)
Afib
Valvular heart disease
Other (5%)
Hemorrhagic
Intracerebral hemorrhage
Subarachnoid hemorrhage
Cerebral aneurysm
AVMs
TIA
Transient Ischemic Attack (TIA)
Temporary neurologic deficit(s) typically lasting < 1 hr with complete resolution within 24 hr
Temporary interruption of BF
Warning stroke/mini stroke
Symptoms disappear in 10-20 minutes
No evidence of ischemia on neuroimaging
Increased risk of subsequent CVA

Ischemic Stroke
Disruption of blood flow → decreased cerebral perfusion/ischemia → cell death/infarction → loss of function
Caused by thrombosis or Embolis
Thrombosis (blood clot) of cerebral arteries or intracranial vessels that occludes BF
Causes congestion and edema in vessel which leads to ischemia
Embolism from a thrombus outside of brain (aorta, heart, common carotid artery)
Curs off circulation causes necrosis and edema
Embolism (sudden obstruction of bv by debris, which can be blood clots, plaque, bacteria, or air bubbles)
Ischemic Stroke Risk Factors
Nonmodifiable
Genetic pre-disposition
Age > 55
Female sex
Race/ethnicity – AA, Hispanic/Latino
Modifiable (table 62-1. p. 2035)
Carotid stenosis
Afib
HTN, DM, HLD
Hypercoagulable states
Sedentary lifestyle
OSA
Smoking
Chronic conditions
SCD
Migraine with aura, vasospasm
Patent foramen ovale – clots can bypass lungs and enter brain
Ischemic Stroke Clinical manifestations
Depend on location of stroke (i.e., what blood vessels are obstructed), size of the area of inadequate perfusion (penumbra), and amount of collateral blood flow
Deficits typically opposite side of stroke
Refer to NIHSS
Altered mentation, cognition
Dysarthria
A disturbance of speech due to emotional stress, to brain injury, or to paralysis, incoordination, or spasticity of the muscles used for speaking.
Dysphagia
Aphasia (receptive, expressive, global)
Impaired or absent comprehension or production of, or communication by, speech, reading, writing, or signs, caused by an acquired lesion of the dominant cerebral hemisphere
Visual disturbances (e.g., homonymous hemianopsia)
Heminumbness; hemiparesis (weakness), hemiplegia (paralysis)
Hemineglect
Changes in gait and/or coordination (ataxia)
Ischemic Stroke Nursing Considerations
For every deficit, there is a nursing diagnosis (p. 2041-2048)
Maintain patent airway
Frequent neuro checks
Serial NIHSS
Things can turn on a dime – hemorrhagic conversion
Continuous hemodynamic monitoring per unit protocol
Neuroendovascular stroke teams will often provide BP goals
Monitor ICP – refer to earlier slides
Monitor blood glucose
Seizure precautions
It’s not just about survivorship; it’s about recovery
Family may become caregivers overnight
Nursing diagnosis
Impaired breathing associated with neurologic dysfunction (brain stem compression, structural displacement)
Risk for ineffective tissue perfusion associated with the effects of increased ICP
Hypovolemia associated with fluid restriction
Risk for infection associated with ICP monitoring system (fiberoptic or intraventricular catheter)
Potential complications
Brainstem herniation
Diabetes insipidus
SIADH
Hemorrhagic Clinical Manifestations
Similar to ischemic stroke
Poor prognosis depending on extent of bleed
“Thunderclap” HA
worst headache they have ever had in life
Nuchal rigidity
Early changes in LOC
N/V
Seizures
AVM – visual disturbances (visual loss, diplopia, ptosis), tinnitus, photophobia
Hemorrhagic Assessment and Diagnosis
Similar to ischemic stroke
CT, CTA (especially if suspected AVM, aneurysm)
Toxicology screen when appropriate for patients < 40 years old
Hemorrhagic Complications and Management Goals
Rebleeding or hematoma expansion
FFP, idarucizumab (DOAC reversal)
Cerebral vasospasm ischemia, seizures
Acute hydrocephalus
Increased ICP
Others
Pain, fever
DVT
Hyper/hypoglycemia
Surgery if indicated
Endovascular AVM, aneurysm repair (coiling, stenting, glue embolization)
Refer to nursing considerations regarding ischemic stroke (minus the t-PA, thrombectomy)
Hemorrhagic Stroke Risk Factors
Non-modifiable
Older age
Male sex
Race/ethnicity – Latino, AA, Japanese
Modifiable
Uncontrolled HTN
Hemorrhagic Stroke
Etiology:
Primary ICH
Spontaneous rupture of small vessels 2/2 uncontrolled HTN (80%)
Cerebral amyloid angiopathy (CAA) in older adults
Secondary ICH
AVM
Trauma
Tumors
Drugs (e.g., anticoagulants, cocaine, amphetamines)
SAH
Cerebral aneurysm
AVM
Hyponatremia
Loss of sodium
<135 meq/L
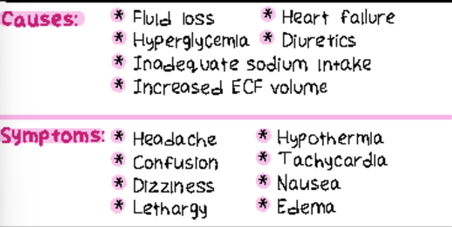
Causes
Excessive diuresis
GI fluid loss
Adrenocorticoid insufficiency
V/D
Diuretics
excess oral fluids
excess parenteral administration of dextrose and water
excessive IV administration
weakness, apprehension, coma, peronality changes, lethargy, confusion, muscle cramps and twitching, seizures
Treatment:
Restict fluid intake
Hypertonic 3% NaCl slowly with caution

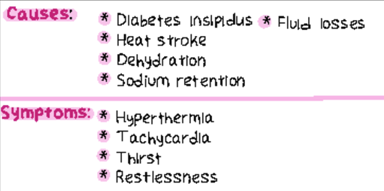
Hypernatremia
>145
water loss
Causes
rapid infusion of hypertonic saline, sodium bicarbonate or isotonic saline
drinking salt water
ingestions a lot of salt without increasing water intake
Excessive H2o loss
diarrhea
increase sensible loss
diabetes insipidus
decreased water intake
withholding water'
impaired thirst center
thirst, dry mouth, sticky mucous membrane, weak pulse, oliguria, anuria, Seizures, decreased reflexes, hallucinations, increased urine specific gravity, if severe: hallucinations, irritability, seizures
> 145 mEg/L
Treatment:
Administer hypotonic solution, 0.45 NaCl or 0.3% NaCl
If caused by diabetes insipidus give desopressin or vasopressin
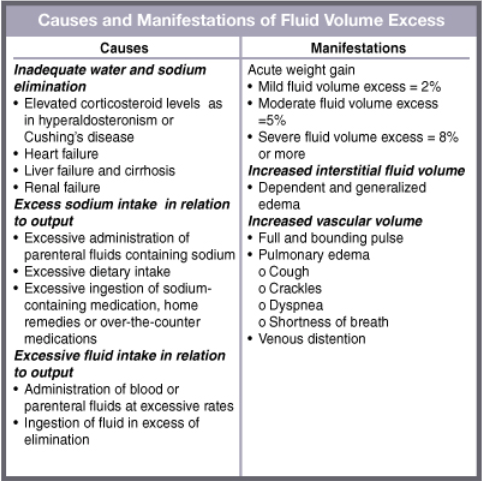
fluid volume excess
Hypervolemia: increased volume in blood
Edema: excessive fluid in cells or intercellular tissues
local or generalized
Third spacing: loss of extracellular fluid from vascular to other body components. Fluid trapped in space unable to be used
ascites
pleural effusion
Causes:
inadequate water and sodium elimination
excessive sodium intake in relation to output
Excessive fluid intake in relation to output
Manifestations:
tachycardia, bounding pulse, hypertension, tachypnea, acute weight gain, peripheral edema/ascites, crackles heard in lungs, SOB, decreased hemoglobin and hot, decreased urine specific gravity, distended neck veins, increased GI motility, altered LOC
Sodium
regulate fluid volume, interact with calcium to maintain muscle contraction, stimulates conduction of nerve impulse.
Cation
combines with Cl
Normal serum rate: 135-145 mEq/L
Regulated through:
Dietary intake
Excretion
Kidneys
Hormonal regulation
Aldosterone
ADH
Imbalance
Hyponatremia
Serum sodium lvl: 115-139 mEq/L
Hypernatremia
Serum sodium lvl: 148-154 mEq/L
Nursing interventions Hyponatremia
Treat underlying conditions
sodium replacement
Water restrictions
monitor I&O, labs, CNS changes, vital signs
Initiate seizure precautions
Nursing interventions hypernatremia
Gradual lowering of sodium via IV fluids
Encourage water intake
decrease sodium intake
monitor I&O, labs, CNS changes, vital signs
Initiate seizure precautions
Hypervolemia
ef:
Cause:
kidney failure
HF
cirrhosis
nephrotic syndrome
Clinical Manifestations
Dyspnea
Crackles
Tachypnea
Bounding rapid pulse
Edema
HTN
Edema
Ventricular gallop
Clammy skin
Treatment
Identify and treat underlying cause
restrict sodium and fluid water intake
id severe O2 therapy, morphine, IV diuretics, mechanical ventilation
Fluid volume excess Nursing interventions
Position in semifolwers
Obtain daily weight same time q day
Assess lung sounds
Monitor intake/output (I&O)
Implement fluid & sodium restrictions per orders
Administer O2 as prescribed and as needed
Administer diuretics
Irritable Bowel syndrome Patho, risk factors, clinical manifestation
Pathophysiology
recurrent abdominal pain associated with disordered bowel movements, which may include diarrhea, constipation, or both, without an identifiable cause
Genetics+envrionment
Risk factors/complications
<45yrs
Women>Men
Air pollutant
Tobacco
Notern climate
Ashkenazi Jewish
Chronic stress
Sleep deprivation
Bacterial overgrowth
Genetics
Surgery infections (Giardia)
Inflammation
Food intolerance
Clinical manifestations
Constipation
Diarrhea
Pain
Bloating
Abdominal distention
Irritable Bowel syndrome Assessment, diagnosis, Treatment
Focused assessment
Critea to Define IBS 2 or more:
Abdominal pain related to defecation;
Abdominal pain associated with a change in frequency of stool;
Abdominal pain associated with a change in form/appearance of stool.
Diagnosis
CBC
C-reactive protein
Fecal calprotectin
Serotoloci tests
Stool studies
colonoscopy
Treatments/nursing interventions
LOW FODMAP diets
Fermentable Oligosaccharides (e.g., wheat, rye, asparagus, legumes, garlic, onions),
Disaccharides (lactose-containing foods such as milk, yogurt),
Monosaccharides (fructose-containing foods such as honey, agave nectar, figs, mangoes), And
Polyols (e.g., blackberries, lychee, and low-calorie sweeteners)
Antidiarrheal agents
Lomotil
Antidepressants
dicyclomine
Smooth muscle antispasmodic agents
Abx for diarrhea
Nurising interventions
Avoid fatigue
Reduce anxiety
Increase knowledge
Prevention of FV deficiet
Avoid complications
Restore bowel elimination
Educate
Releave Pain
Indications
Crohn’s disease: SBO, abscess, perforation, hemorrhage,
fistula formation, stricturesUlcerative colitis: colon cancer/colonic dysplasia, megacolon
hemorrhage, perforation, strictures
Proctocolectomy (surgical excision of the colon and rectum)
and
total colectomy (surgical excision of the entire colon) with
ileostomy (surgical opening into the ileum via stoma to allow
drainage of bowel contents)Curative for ulcerative colitis but not for Crohn’s
99
Inflammatory Bowel disease
Ulcerative colitis
Crohns disease
Crohn’s disease
Pathology:
Subacute and chronic inflamation of GI tract
skip lesions, cobblestome 1/1 ulcerations, fistulas, fissures, abscesses
Relapsing progressive
Clinical manifestations:
Anorexia, wt loss, malnutrition
Steatorrhea
Dehydration
Location: Ileum, ascending colon (usually)
Crampy RUQ pain
Bleeding: Usually not, but if it occurs, it tends to be mild
Perianal: Common
Fistulas: Common
Diarrhea: Less severe
Abdominal Mass: Common
Diagnostic Findings
Imaging- Abdomincal CT, MRI, US
Procedures: colonscopy+biopsy
Lab studies
CBC
Elevated ESR, CRP
B12 deficiency
Low serum albumin, protien
Therapeutic management:
Corticosteroids, aminosalicylates (sulfasalazine)
Immunomodulators (e.g., azathioprine) or monoclonal antibodies (e.g., infliximab, adalimumab) may be tried if refractory to corticosteroids and aminosalicylates
Antibiotics
Parenteral nutrition
Partial or complete colectomy, with ileostomy or anastomosis
Rectum can be preserved in some patients
Recurrence common
Ulcerative colitis
Patho:
Inflammatory disease of the
mucosal and submucosal layers of the colon and rectumMucosal ilceration→ exposure of capillaries→ bleeding
Relapsing and remitting (flares and heels)
S&S
Bleeding: Common-severe
Fever, anorexia, wt loss, Vomitting
LLQ cramping releaved by poopining
Perianal: Rare
Fistulas: Rare
Diarrhea: severe
Abdominal Mass: rare
Diagnostic Findings
Imaging- abdominal XR, CT, MRI, US
Procedures-colonoscopy+biospy
Lab studies
CBC: anemia, leukocytosis
CMP: electrolyte abnormalities
Elevated ERS
Stool sample
r/o parasites
+ blood
Hypoalbumenia
Complications
Perforation
Bleeding
Osterporotic fractures
Colon cancer
Toxic megacolon
Therapeutic management:
Corticosteroids, aminosalicylates (sulfasalazine) useful in preventing recurrence
Immunomodulators (e.g., azathioprine) or monoclonal antibodies (e.g., infliximab, adalimumab) may be tried if refractory to corticosteroids and aminosalicylates
Bulk hydrophilic agents
Antibiotics
Proctocolectomy, with ileostomy
Rectum can be preserved in only a few patients “cured” by colectomy
Hepatitis
Pathophysiology
5 types
Hepatitis A -avoid causative agent, No treatment
Hepatitis B – Interferon-education
Hepatitis C – Interferon & Ribavirin
Hepatitis D – No treatment
Hepatitis E – No treatment
Avoid ETOH
GOOD HANDWASHING
Reportable, communicable disease
Clinical manifestations
Fatigue
Jaundice (yellowing of skin/eyes)
Anorexia, nausea, vomiting
RUQ abdominal pain
Dark urine, pale stools
Fever (in acute cases)
Hepatomegaly (enlarged liver)
Joint pain (arthralgia), especially in HBV and HCV
Risk factors/complications
V drug use
Unprotected sex (especially HBV, HCV)
Healthcare exposure (needlesticks)
Travel to endemic areas (HAV, HEV)
Blood transfusions before 1992 (HCV risk)
Poor sanitation (HAV, HEV)
Chronic hepatitis → cirrhosis → liver failure → liver cancer (especially HBV and HCV)
Hepatitis focused assessment and Treatments
Focused assessment
Assess for jaundice, fatigue, RUQ tenderness
Monitor liver function tests (AST, ALT, bilirubin)
Assess for bleeding/bruising (decreased clotting factors in liver disease)
Monitor for neurological changes (hepatic encephalopathy)
Ask about risk factors (travel, drug use, sex, needle sharing)
Treatments/nursing interventions
Promote rest and balanced nutrition (small frequent meals)
Avoid alcohol and hepatotoxic drugs (e.g., acetaminophen)
Educate on infection control (handwashing, safe sex, no sharing razors/needles)
Administer medications as prescribed (e.g., Interferon, Ribavirin)
Monitor labs (LFTs, CBC, coagulation panel)
Encourage vaccination for Hep A & B (prevention)
Prepare for possible liver biopsy or transplant evaluation in chronic cases
Report to public health as required
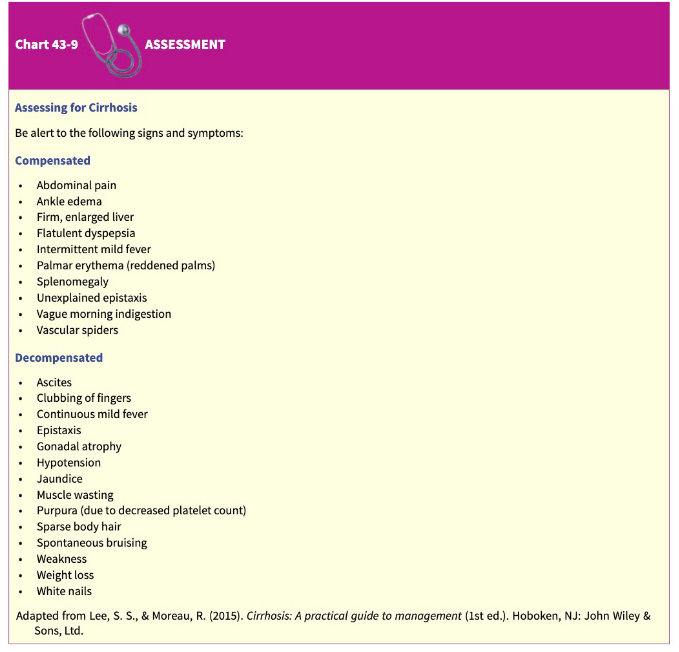
Cirrhosis
Compensated and decompensated
Compensated
Liver can still perform essential functions, often without noticeable symptoms
Decompensated
noticeable symptoms, can’t function
Pathophysiology
Extensive, irreversible scarring of the liver->impairments in BF and lymph flow
Cause: chronic reaction to hepatic inflammation or necrosis
Laennec: Alcohol induced
Post necrotic: viral hepatitis/drugs
Biliary: chronic biliary obstruction and infection
Cardiac: chronic Rt side HF causing elevated venous pressure & liver congestion
Clinical manifestations
Compensated: no obvious symptoms
Decompensated: ascites, jaundice, hepatic, encephalopathy or variceal bleeding
Liver enlargement
Portal obstruction & asities
dullness or fluid wave on percussion
Infection & peritonitis
dx by paracentesis
spontanious bacteriola peritonitis
GI varices
Edema extremities
Vitamin deficiency ACK, anemia
Mental deterioration
Risk factors/complications
Fatal without transplan
Renal Gerontologic Considerations
GFR decreases between ages 35 to 40yrs
1 mL/min continues thereafter each year
Older adults susceptible to acute and chronic kidney injury
Older adults are more prone to develop hypernatremia and fluid volume deficit, because increasing age is also associated with diminished osmotic stimulation of thirst
Slow response to sudden physiologic changes
Diminished osmotic stimulation of thirst
Urinary incontinence is present in 15% to 30% of community-dwelling older adults, 50% of older adults who are institutionalized, and 30% of older adults who are hospitalized
Incomplete emptying of the bladder
A fluid balance deficit in older adults can lead to falls, medication toxicity, constipation, urinary tract and respiratory tract infections, delirium, seizures, electrolyte imbalances, hyperthermia, and delayed wound healing.
Lower Urinary Tract Infections
Causes: bacteria colonize the urinary tract, backward flow of urine from the bladder into the ureters, obstruction of free flowing urine
The most common cause of UTIs occur when fecal organisms ascend from the perineum to the urethra and bladder
Cystitis
(inflammation of the urinary bladder),
Prostatitis
(inflammation of the prostate gland), and bacterial
urethritis
inflammation of the urethra)
Females at greater risk due to short urethra
Assess patients for dysuria, frequency, urgency, nocturia, incontinence, suprapubic or pelvic pain, UA, Urine C&S
Bacteriuria increases with age (women > men)
UTI is the most common infection of elderly
Initiate ABT orders – decrease s/s, prevent complications
Encourage fluids to flush bacteria and promote renal blood flow
Patient education. Review “Nursing Process – The Patient with a Lower Urinary Tract Infection”
NURSING DIAGNOSIS
Acute pain associated with infection within the urinary tract
Lack of knowledge about factors predisposing the patient to infection and recurrence, detection and prevention of recurrence, and pharmacologic therapy
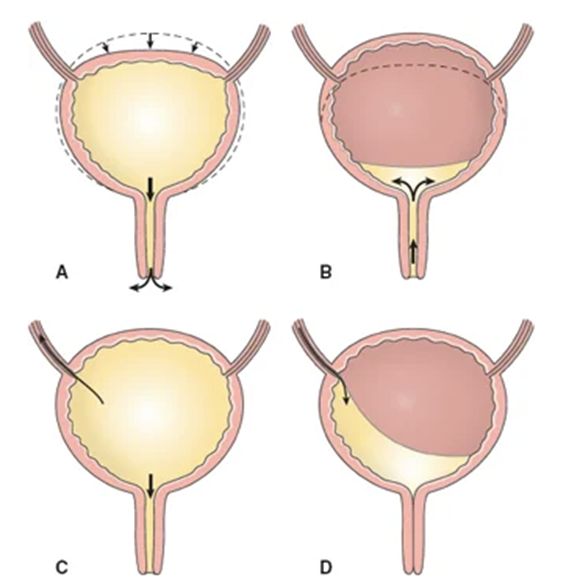
Neurogenic Bladder
Urinary incontinence resulting from a neurological disorder
Causes: spinal cord injuries, spinal tumors, congenital spinal disorders, infections, or complications of disease processes such as diabetes and multiple sclerosis
Types: Spastic bladder and flaccid bladder. Spastic bladder empties on reflex. Flaccid bladder empties by overflow incontinence
Assessment: UA, skin integrity, I&O, residual urine, assess for sensory awareness of bladder fullness
Complications: infection, kidney stones
Nursing management: prevent over-distention of the bladder, encourage low calcium diet, encourage fluid intake, bladder retraining
Upper Urinary Tract infections
Acute pyelonephritis
a bacterial infection causing inflammation of the kidents andis one of the most common diseases of the kidneys. It occurs as a complication of an ascending urinary tract infection which spreads from the bladder to the kidneys and their collecting systems.
Chronic pyelonephritis
unclear cause
can be caused by reflux nephropathy
kidneys are damaged by backward flow of urine back into kidney due to leaky valve
Renal Abscess
occurs within kidney tissue
Interstitial nephritis
Causing inflammation around tubules
lowers person ability to clean their body and produce urine
Perineal abscess
occurs around one or both kidneys
Human Papilloma Virus (HPV)
One of the most common STI
Commonly asymptomatic
Chronic condition
Virus stay in nerve cells
Sexual contact
Gardasil vaccine can prevent some types
Human Papilloma Virus (HPV) Transmission
Unprotected Vaginal, anal, oral sex
Mother to baby: pregnancy , labor, birth
Can lead to cancers
Female
Male
Both
Typically asymptomatic
Gardasil 9
indication: HPV
MOA: Recombinant vaccine inducing antibody production
AE: Injection site reactions, headache, fever, fainting (vasovagal), syncope
Nursing Considerations:
Give IM in deltoid
Monitor 15 mins post-injection (fainting risk)
Series of 2 or 3 doses depending on age
Chlamydia Trachomatis & Neisseria Gonorrhea
More prevalent in females 15-24
C. Trachomatis common with young women 15-24
Most commonly reported infectious diseases
Chlamydia Trachomatis & Neisseria Gonorrhea: Clinical Manifestations
General
Fever
Purulent drainage
Foul odor discharge
Typically painless
Visualization of site
Joint pain
Women
Both commonly don’t cause symptoms in women
Uterine tenderness
Mucopurulent cervicitis with exudates in endocervical canal
GONORRHEA: present with UTI or Vaginitis
Men
More likely to have symptoms
Can be asymptomatic with both
Inguinal lymph node swelling
Buring during voiding
Penile discharge
GONORRHEA: painful, swollen testicles
Chlamydia Trachomatis & Neisseria Gonorrhea: Complications
Women:
Pelvic Inflammatory disease PID
Ectopic pregnancy
infertility
Men:
Epididymitis
Can lead to infertility
Painful
GONORRHEA: Both sexes
Arthritis
Bloodstream infection
Chlamydia Trachomatis & Neisseria Gonorrhea: Assessment and Diagnostic Findings
Assess for fever, discharge, and signs of arthritis
Gram stain in lab
Culture
Male
Urethra
Anal canal
Pharynx cultures
Female
Urethra
Anal canal
Pharynx cultures
Nucleic acid amplification tests (NAAT)
Annual testing for women <25yrs who are sexually active, or > 25 with new or multiple sexual partners
Pregnant women =chlamydia testing bc 70% asymptomatic
Chlamydia Trachomatis & Neisseria Gonorrhea: Medical management
Dual therapy bc patients are often coninfected
dual therapy is recommended, even if only gonorrhea has been laboratory proven
Serologic testing
If the patient reports a new episode of symptoms or tests are positive for gonorrhea again, the most likely explanation is reinfection rather than treatment failure.
Chlamydia Trachomatis & Neisseria Gonorrhea: Nursing management
Reportable communicable diseases
reported to the local public health department to ensure follow-up of the patient.
Prevention education: adolescence and young adult
Pregnancy: routine screening for chlamydia.
Teach abstinence, limiting sexual partners, using condoms, age of initial sexual exposure
Chlamydia Trachomatis & Neisseria Gonorrhea: Patient education
Medication adherence
Sexual adherence
5P’s
Partners
Prevention
Pregnancy
Protection
Past histories
Chlamydia Trachomatis & Neisseria Gonorrhea: Nursing Diagnoses
Knowledge deficit
Anxiety
Nonadherence
ceftriaxone
Indication: N. Gonorrhea, UTI, ROUTE: IV, IM
MOA: Inhibits bacterial cell wall synthesis (β-lactam antibiotic)
AE:
CNS: fever, taste disturbance, headache, dizziness.
CV: IV site phlebitis, flushing.
GI: diarrhea, nausea, vomiting.
GU: increased BUN level, increased creatinine level, moniliasis, vaginitis.
Hematologic: anemia, eosinophilia, thrombocytosis, leukopenia.
Hepatic: increased transaminase levels.
Skin: pain, induration, and tenderness at injection site, rash, diaphoresis.
Other: hypersensitivity reactions, chills.
Nursing Considerations:
IM injection can be painful (may mix with lidocaine)
Check allergy history (esp. penicillin cross-reaction)
Assess for cephalosporin allergy
Monitor PT and INR
Monitor Diarrhea
Venous Thromboembolism (DVT)
Risk factors
Endothelial damage
Venous stasis
Altered coagulation
Manifestations
Deep veins
Superficial veins
Complications of Venous Thrombosis
Chronic venous occlusion
Pulmonary emboli from dislodged thrombi
Valvular destruction:
Chronic venous insufficiency
Increased venous pressure
Varicosities
Venous ulcers
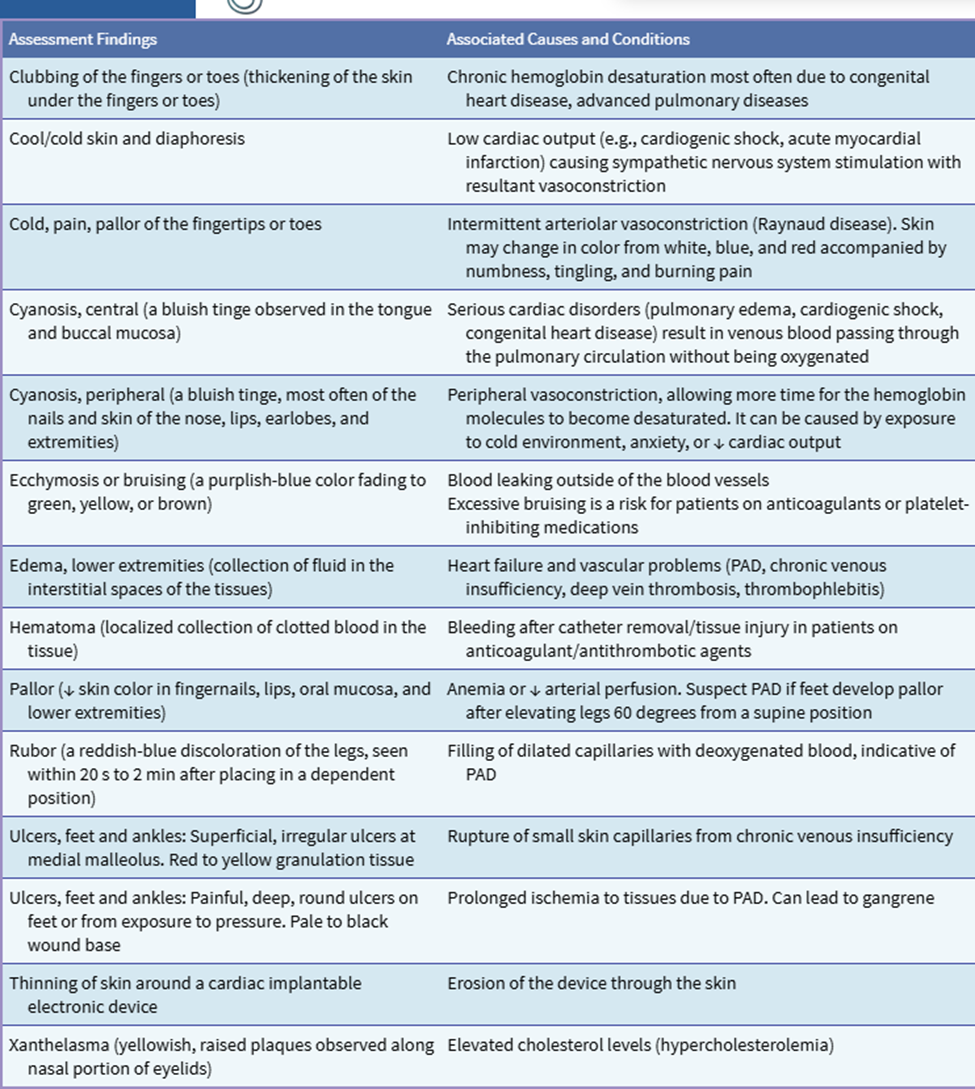
Physical Assessment of cardiovascular system: Skin
P’s=acute abduction of atrial BF in extremities
Pain
Pulselessness
Pallor
Paresthesia
Poikothermia
Paralysis
Major blood vessels of the arms and legs may be used for catheter insertion. During these procedures, systemic anticoagulation with heparin is necessary, and bruising or small hematomas may occur at the catheter access site.
Large hemaromas sus
Peripehral edema
Edema of feet, legs, and ankles
HF, PVD, DVT, chronic venous insufficiency
0, 1, 2, 3, 4
Prolonged capillary refill
Clubbing
Chronic hemoglobin desaturation=congenital HD
Chronically reduced O2
Hair loss
Brittle nails
Drys skin
Uclers
Skin color changes
Heart Failure
Chronic condition
Acute on chronic exacerbations
Types
Left sided
Right sided
Diagnostic Assessment
Imaging
CXR: enlarged heart (NOT DIAGNOTIC)
Vascular engorgement, cardiomegaly, or pleural effusions
Echocardiogram (best diagnostic tool):
EF
Valvular changes, chamber enlargement
Pericardial effusion
Blood clots
Cardiac wall motion
BNP: Brain natriuretic peptide
higher number= more intense the HF
norms: <100pg/mL
suggests HF: 100-299
Mild HF: 300-599
Moderate HF: 600-899
Severe HF: >900
ECG
Stress testing
Cardiac Catheterization
Heart Failure: Interventions
Pharmacologic
Diuretic
Beta blockers
Iv Infusion of Inotropic
Inotropic agents, or inotropes, are drugs that change the force of a heart's contractions. Inotropes can be positive or negative, depending on whether they strengthen or weaken the heartbeat
Positive inotropes
Used when the heart is too weak to pump enough blood, such as when the heart can't get enough blood to the body. Positive inotropes strengthen the heart's contractions, which increases cardiac output and the amount of blood the heart pumps.
Negative inotropes
Used when the heart is working too hard, such as when a patient has high blood pressure, chest pain, or an abnormal heart rhythm. Negative inotropes weaken the heart's contractions.
Examples of positive inotropic medications include digoxin, dobutamine, and milrinone.
Clonidine and Atenolol are examples of negative inotropic medications
Nutritional therapy
Dash diet
Low sodium
No canned food
No processed foods
Heart Failure: Nursing process & Patient education
Care
Focus
Effectiveness of therapy
Patient’s self-management
S&S if increased HF
Emotional or psychosocial response
Health history
PE
Mental status; lung sounds: crackles and wheezes; heart sounds: S3; fluid status or signs of fluid overload; daily weight and I&O; assess responses to medications
Patient education
Medications
Diet: low-sodium diet and fluid restriction
Monitoring for signs of excess fluid, hypotension, and symptoms of disease exacerbation, including daily weight
Exercise and activity program
Stress management
Prevention of infection
Know how and when to contact health care provider
Include family in education
Heart Failure: Nursing Diagnosis
Activity intolerance related to decreased CO
Excess fluid volume related to the HF syndrome
Anxiety-related symptoms related to complexity of the therapeutic regimen
Powerlessness related to chronic illness and hospitalizations
Ineffective family therapeutic regimen management
Pump Failure
Inadequate peripheral blood flow occurs when the heart’s pumping action becomes inefficient
Heart failure with reduced left ventricular ejection fraction (HFrEF; also called systolic HF) causes an accumulation of blood in the lungs and a reduction in forward flow or cardiac output, which results in inadequate arterial blood flow to the tissues.
Heart failure with preserved left ventricular ejection fraction (HFpEF; also called diastolic HF) causes systemic venous congestion and a reduction in forward flow
Coronary Vascular Disorders
Coronary Atherosclerosis
Angina Pectoris
Acute Myocardial Infarction
Coronary Atherosclerosis
Most common CAD disease
Abnormal accumulation of lipid, or fatty substances, and fibrous tissue in the lining fom arterial blood vessels blocks the coronary arteries and reduces blood to the myocardium
Coronary Atherosclerosis: Clinical Manifestations
Depends on location and degree of narrowing
Ischemia
Angina pectoris
Sudden cardiac death
Epigastric distress
Pain that radiates to the jaw or left arm
Older & diabetes SOB
Women atypical
Indigestion
Nausea
Palpations
Numbness
Coronary Atherosclerosis: Risk Factors
Elevated LDL
Diabetes
Peripheral arterial disease
Abdominal aortic aneyurism
Older
Large abdominal circumference
Hypertension
Reduced HDL
Angina Pectoris
Angina=chest pain
A Syndrome characterized by episodes or paroxysmal pain or pressure in the anterior chest caused by insufficient coronary blood flow
SOB, diaphoresis, palpitations, fatigue, N/V
Physical exertion or emotional stress increases myocardial oxygen demand, and the coronary vessels are unable to supply sufficient blood flow to meet the oxygen demand
Can radiate across chest to arms, jaw, shoulders, upper back or epigastrium
Radiation to arm and hands described as numbness and tingling
Stable angina: more O2 than heart can handle
Unstable: acute coronary syndrome. It is characterized by sudden and unexpected chest pain, typically while at rest, and it can persist longer than stable angina. This condition is a sign that your heart is not getting enough oxygen, and it requires immediate medical intervention.
Variant: random angina
Acronym: PQRST
P:
Q
R
S
T
Aggravating factors
Physical exertion, emotional upset, eating large meal, or exposure to extremes in temperature
Treatment
Rest, nitroglycerin, O2
MONA
Acute Myocardial Infarction
Emergency
AKA coronary occlusion, Heart attack
Acute Myocardial Infarction: Interventions
Pharmacologic
Nitrate
Beta-Adrenergic blockers
Antiplatelet
Calcium-Channel blocker
PCI
Cardiac catherterization
Percutaneus coronary intervention
Coronary artery stent
Surgical Intervention
Coronary artery bypass graft (CABG)