oral manifestations of systemic disease
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
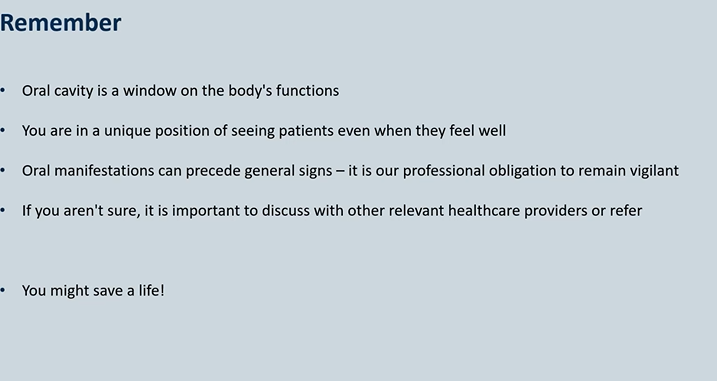
Dentistry – beyond teeth
skin, GI tract, musculoskeletal conditions
mouth is the gateway to the rest of your body
Thorough intraoral examination can reveal the first signs of an underlying systemic disease.
Be aware of the relationship between oral lesions and systemic diseases
Recognition of abnormal, review and refer when appropriate
Prompt discussion with other healthcare professionals, who may not understand oral presentations.
Can lead to an early diagnosis and treatment if recognised.
Be inquisitive

Example – Gingival Swelling
29 year old female Medically well, takes no regular medications Complaining of bleeding and gums
Dental clinic receptionist
Seen by one of the dentists, who notes significant generalised gingival swelling
Reasonably good plaque control
Pocket depths 3-4mm in all quadrants
Radiographs – no bone loss
ask questions - have you noticed anything? weight loss without trying? difficulty swallowing? fever?
New rash on her arms
Clinician suspected something systemic, as there did not appear to be a clear local cause

Example – Gingival Swelling - answers
Discussed with the GP who undertook screening bloods
FBC (full blood count)
Diagnosis of Leukemia – Referred to haematology urgently for treatment and successfully treated
But the outcome could have been very different
what to look for when patients ‘ walk through the door’ 4
are they looking pale
do they look well
are they short of breath walking a short distance
any signs of self neglect
extra-oral examination 7
Facial symmetry
Skin abnormalities - rashes, pale, jaundice
TMJ - sounds such as crepitus
Salivary glands - soft, full, firm
Lymph nodes: Submental, Submandibular, Cervical chain, Supraclavicular , Occipital , Posterior auricular , Anterior auricular → early clues for cancers and haematological malignancies , lymph adenopathies
Lips and peri-oral region - crusting - peri-oral erythema
Neck examination
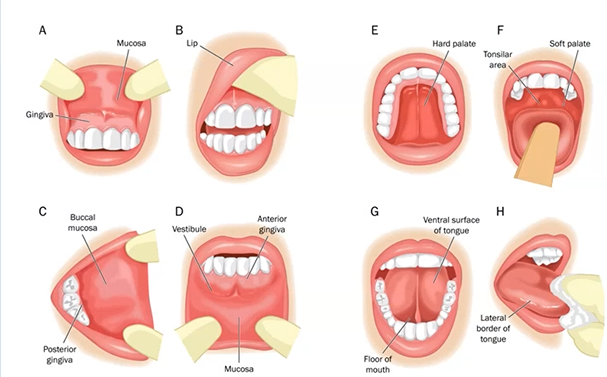
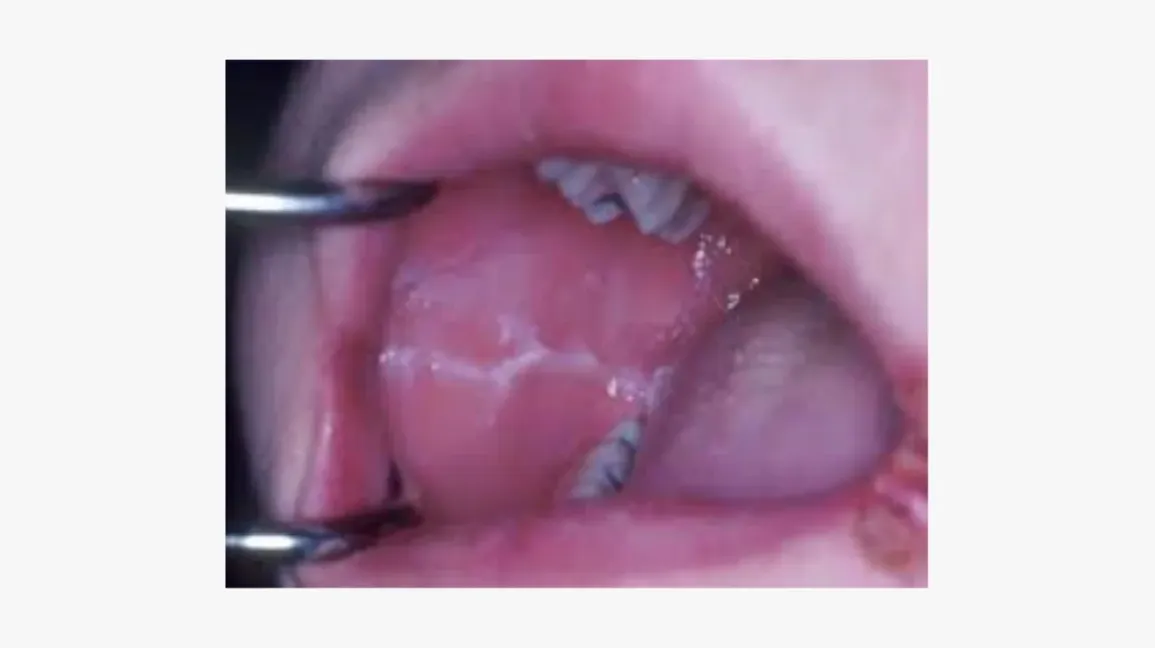
intra-oral examination 10
Oral Mucosa
Tongue
Floor of mouth
Salivary gland ducts
Frenum attachments
Gingivae
Tonsils and oropharynx
Teeth
Occlusion
Prosthesis
start by looking at lips - mucosa buccal - tongue - ventral surface last, back of the throat and hard palate
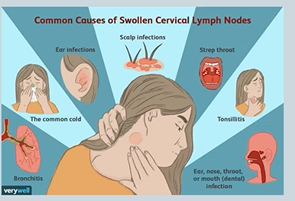
Examination - Lymph nodes
if you have a dental infection - the first place the infection will drain is the submental and submandibular NODES
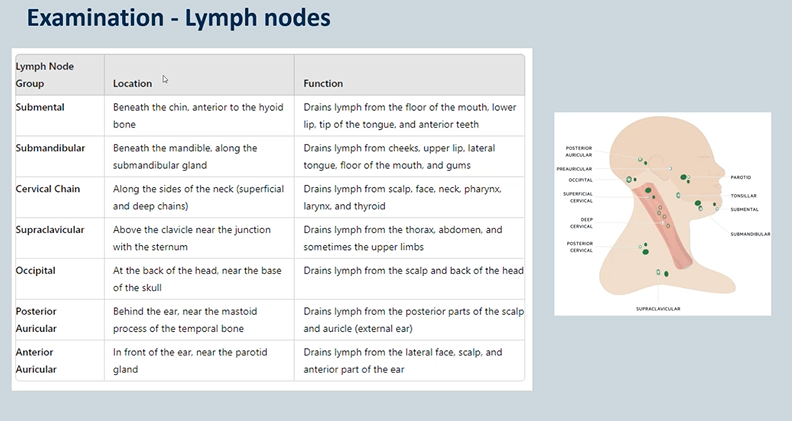
cervical lymph nodes
Head & Neck infection is the commonest cause of enlargement
May also be the first sign of systemic disease:
with infection you tend to get bilateral enlargement of lymph nodes - tenderness
with malignancies - unilateral and non tender
Glandular Fever,Lymphomas (hodgkins / non-hodgkin) ,Leukaemias ,HIV infection (Seroconversaion illness, or advanced HIV disease), Metastatic disease (usually from drainage)

what is shown here?
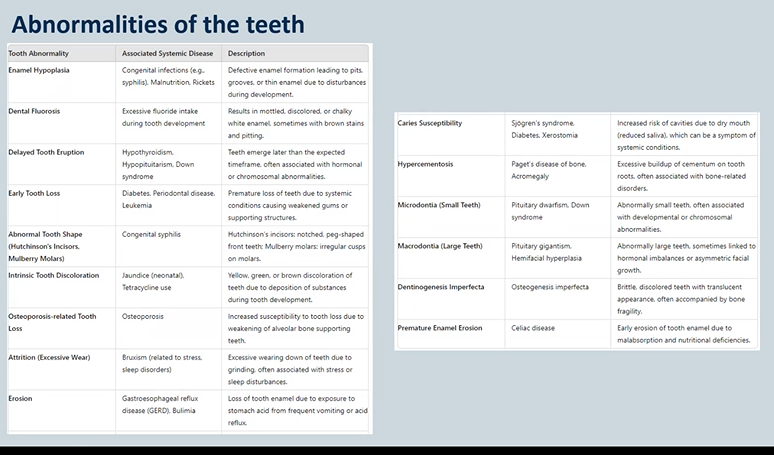
enamel hypoplasia → not the same as hypo-mineralisation
Ameloblasts affected during development – less enamel formed Pits, grooves, thinning
enamel hypoplasia vs hypomineralisation
hypo-mineralisation is when you get the correct thickness of enamel but its softer and wears away faster
hypoplasia - structure is okay - but thinner, incomplete or pitted
what could be the causes of enamel hypoplasia? 6
Nutritional deficiencies
Vitamin D / Calcium deficiency
Pre/Perinatal issues
Maternal infections e.g. rubella and syphilis
Prematurity / Low birth weight
Infectious diseases
Febrile illnesses in early childhood
Measles, chickenpox, scarlet fever
Endocrine
Hypoparathyroidism (abnormal calcium/phosphate
regulation)
Hypothyroidism – delayed tooth eruption
Chronic Renal Disease – disrupting calcium/phosphate
Coeliac Disease – nutrient malabsorption
genetics
amelogenesis imperfecta
down syndrome


what is this an example of?
abnormally shaped teeth
what causes teeth abnormalities and how can it be presented?
congenital Syphilis → vertically transmitted from the mother
Hutchinson’s incisors
Mulberry molars


abnormal colour of teeth - what causes banding?
tetracycline (antibiotic) during odontogenesis (pregnancy/ very young children)

abnormal colour of teeth - what causes mottling?
fluorosis - excess fluoride

abnormal colour of teeth - what causes olive green teeth?
childhood jaundice/liver disfunction - through its very rare

abnormal colour of teeth - what causes purple/red teeth?
prophyria - rare inherited condition where you get porphyrin build up in the body - translucent looking red/purple teeth
porphyrin is needed to make red blood cells - build up in the body

abnormal colour of teeth - what causes translucent brown/purple teeth ?
dentinogenesis imperfecta
blue sclera and brittle bones
abnormal tooth surface loss 3
Erosion
Extrinsic acids (diet) - buccal and labial
Intrinsic acid (gastric) - occlusal and palatal
GORD – risks of oesophageal metaplasia (Barret's oesophagus) and malignant conversation
Bulimia nervosa – Eating disorders
Attrition - tooth wear
Bruxism
Abrasion - mechanical forces
Toothbrushing / musical instruments / pen biting
abnormalities in the oral mucosa- changes in colour - white 4
Candidosis (thrush)
Lichenoid lesion
Leukoplakia
Linea alba
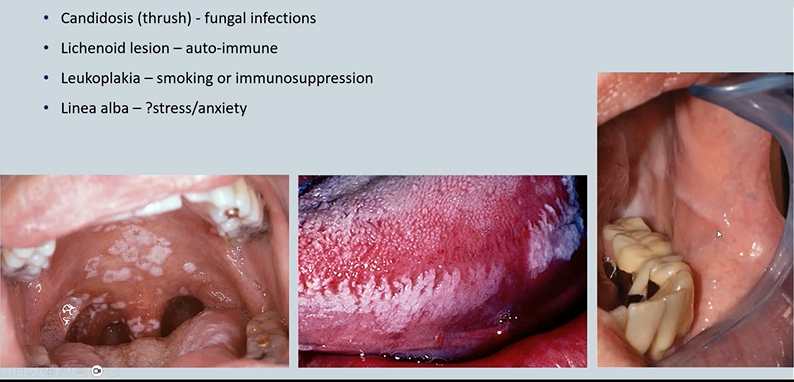

Candidosis (thrush) - fungal infections - candida is commensal fungus but can overgrow. pseudomembranous - wipes off with gauze - debris - immunocompromised eg cancer treatments

Lichenoid lesion auto-immune - don’t come off on wiping - infiltration of lymphocytes → lichen planus, lupus

Leukoplakia smoking or immunosuppression - white patch of unknown aetiology - higher risks of turning into cancers
Linea alba -stress/anxiety - in line of occlusal plane - indentation of the cheek where you are biting - forms a thickened white area
abnormalities of the oral mucosa - changes in colour - red , examples 5
(severity of) Periodontitis – Diabetes, Cardiovascular disease
Mucous membrane pemphigoid – Autoimmune
Pemphigus Vulgaris – Autoimmune
Median Rhomboid Glossitis – Candida
Erythroplakia - Smoking


(severity of) Periodontitis – Diabetes, Cardiovascular disease

Mucous membrane pemphigoid – Autoimmune

Pemphigus Vulgaris – Autoimmune

Median Rhomboid Glossitis – Candida - smoker or dry mouth

Erythroplakia (red patch) - Smoking but could be a pre cancer/cancer
abnormalities in the oral mucosa - changes in colour - yellow 3
Ulceration
Bullae (blistering) causing secondary ulceration
Drugs
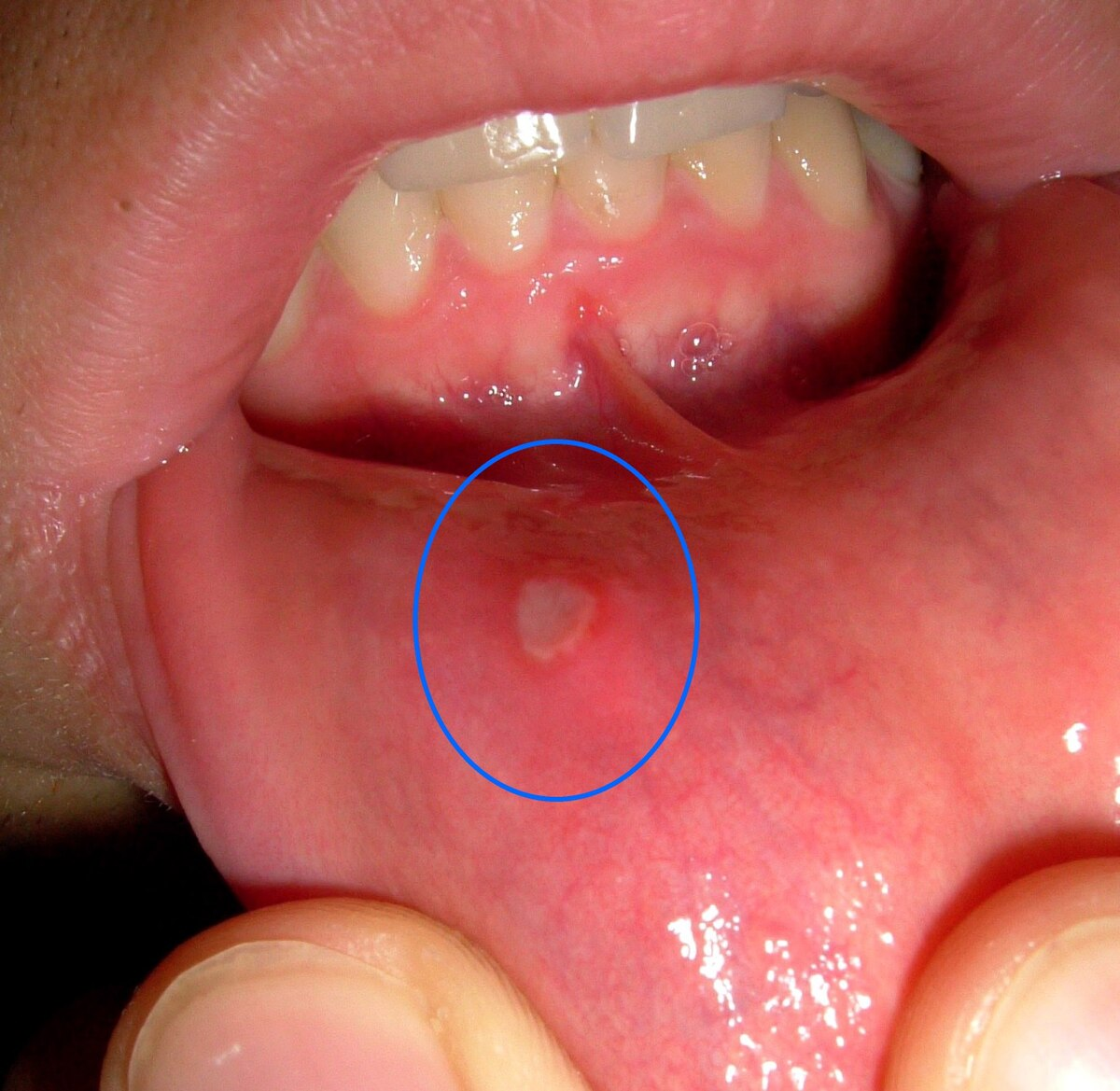
what causes yellow ulcers in the mouth?
ulceration - loss of the full thickness of epithelium
Inflammatory bowel diseases - ie chrons diseases - Chron’s is the inflammation of the GI tract - it starts with the mouth - tags,ulcers,cobblestoning
Malnutrition / deficiency states – Fe, Fo, B12
Coeliac Disease
Viral reactivations oral ulcers
Infections – Herpes, Measles etc
Bechet's Disease

what causes yellow bullae/blistering in the mouth?
blistering - loss of a bit of the thickness in the epithelium. Blister = fluid filled sac
can be because of a cancer
Bullae (blistering) causing secondary ulceration - Paraneoplastic
Chemotherapies
Drugs - hypoglycaemics

what could cause a blue/purple colour change in the oral mucosa? 4
Purpura – Idiopathic thrombocytopenia purpura and other hematological abnormalities
Haematoma – Bleeding disorders, trauma, drugs
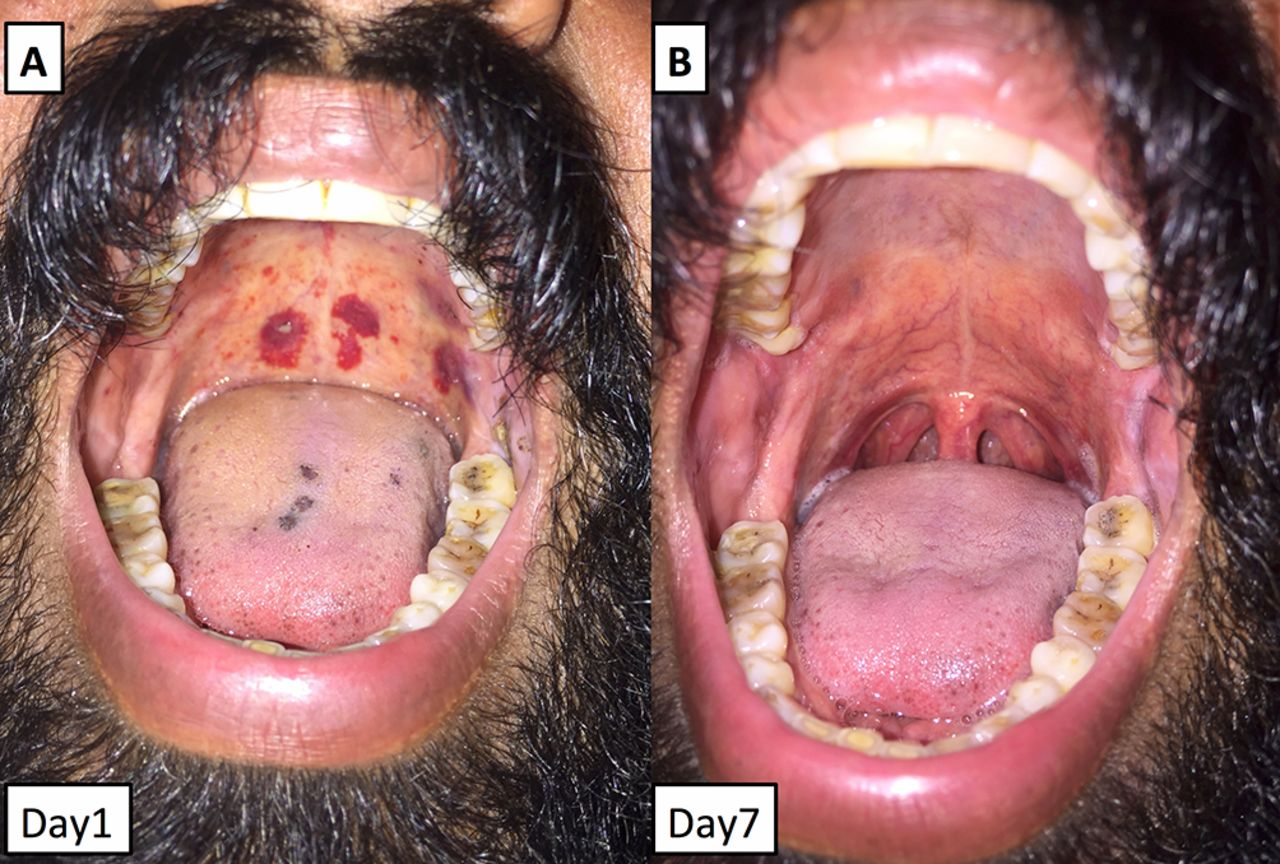
Kaposi’s Sarcoma – HIV infection
Haematological malignancy
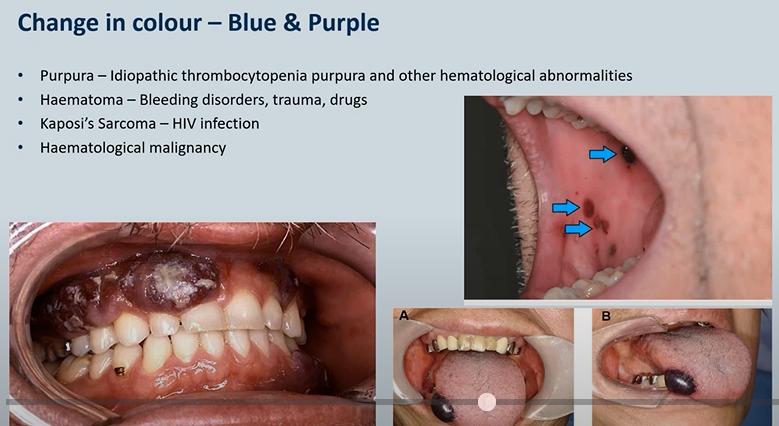
Purpura – Idiopathic thrombocytopenia purpura and other hematological abnormalities/clotting conditions - bleeding under the surface of the skin
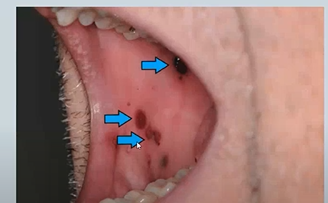
Haematoma – Bleeding disorders, trauma, drugs

Kaposi’s Sarcoma – HIV infection
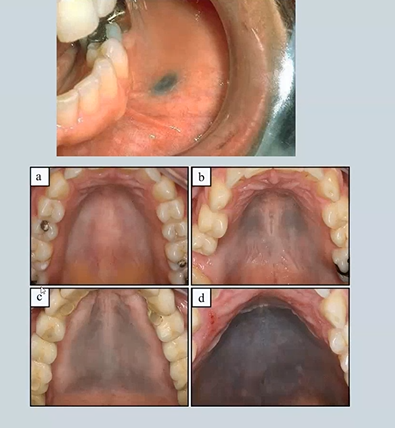
abnormalities in the oral mucosa - grey colour changes 2
Amalgam Tattoo - deposits of fine flecs of amalgam - radiopacities
Drugs – hydroxychloroquine, imatinib
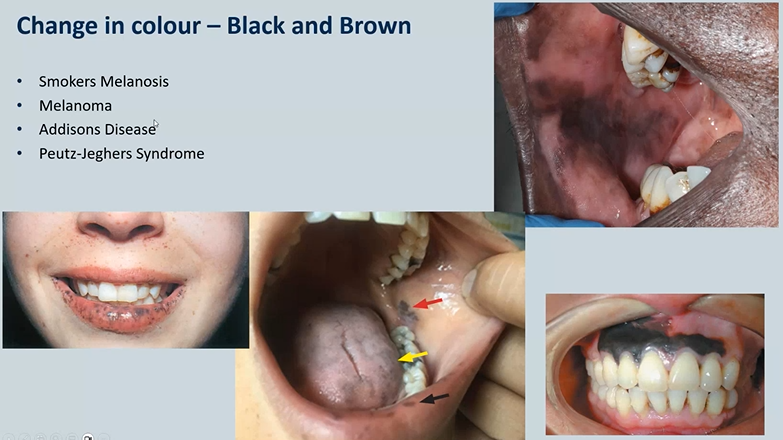
changes in colour of oral mucosa - black or brown 4
Smokers Melanosis - top right - seen in POC - physiological
Melanoma- skin cancer - rare bottom right
Addisons Disease - adrenal insufficiency
Peutz-Jeghers Syndrome - dotted - need to be seen by a GI doctor as theu may experience intestinal polyps
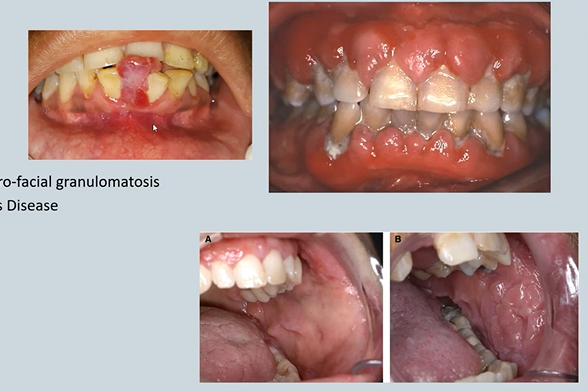
what are some examples of oral swellings? 4
Gingival Hyperplasia
Nifedipine ,Cyclosporin ,Phenytoin, Leukaemias
Lip swelling
Crohn’s Disease / Oro-facial granulomatosis (few years later affects the get)
Cobble stoning – Crohn’s Disease - trauma, endoscopy
Pregnancy - epulis
textural changes in the oral mucosa 4
keratosis – White patches
Lichen planus
Lupus
Immunosuppression
Candidosis
Syphilis
hyperkeratosis - take a biopsy to make sure its not cancer
Glossitis →Anaemia or Vitamin deficiencies (need to regenerate the surface of your mouth)→ B12 – pernicious anaemia→ Malabsorption syndromes – coeliac, short bowel syndrome (post surgical)

GI – Crohn’s Disease
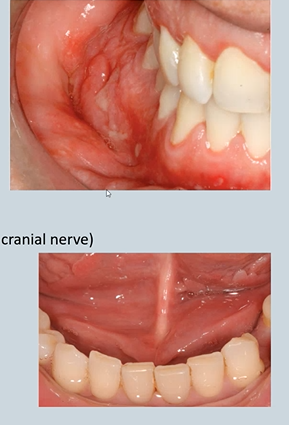
Oral Manifestations - might be the first signs
Lip swelling - bilateral
Deep linear sulcal ulceration- top
Stag-horning - bottom
Cobble stoning of the buccal mucosa
Glossitis due to secondary malabsorption
Melkersson-Rosenthal syndrome – facial nerve paralysis (7th cranial nerve)
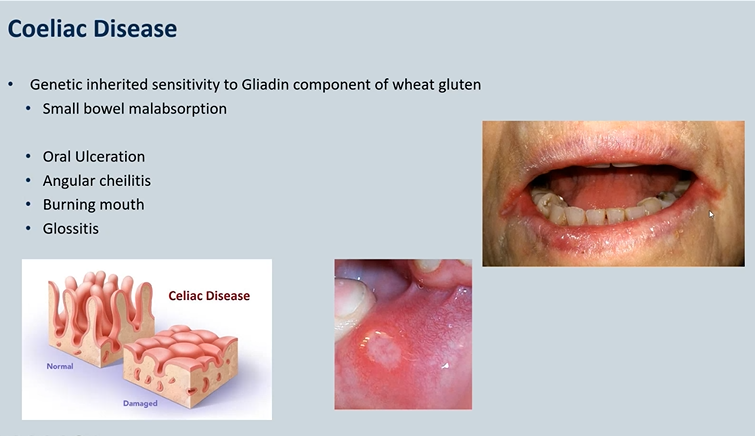
Coeliac Disease
Genetic inherited sensitivity to Gliadin component of wheat gluten Small bowel malabsorption - villus atrophy
Oral Ulceration
Angular cheilitis - candida infection
Burning mouth
Glossitis
Ulcerative Colitis
Inflammation in the colon - malabsorption
Shallow non-granulomatous ulceration
Pyoderma gangrenosum - skin
Pyostomatitis vegetans – oral - bottom

Auto-immune
Pemphigus
Pemphigoid
Lichen Planus - can be in other areas of the body

Auto-immune – Lupus
Discoid Lupus Erythematosis (DLE) - only affects the mouth/skin - no organ involvement
Systemic Lupus Erythematosis (SLE)
ANA/ENA positive – ds-DNA
Rheumatological condition
Chronic inflammation flattens cheeks
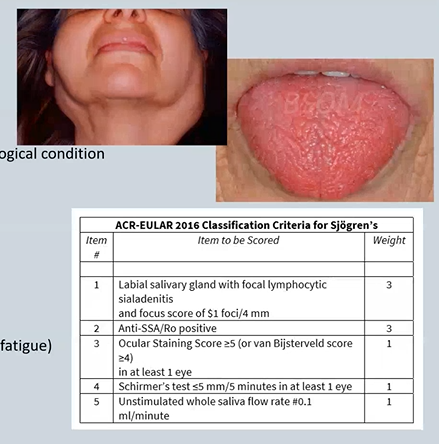
Sjogren’s Syndrome/disease
Not all dry mouths are Sjogren’s Syndrome
Primary – de novo occurrence
Secondary – Preceded by another rheumatological condition
Symptoms – Oral and ocular dryness
Extra-glandular features
MSK (Distal joint pain and myalgia)
Skin (Dryness, rashes and vasculitis)
Lungs (Interstitial lung disease)
GI (Swallowing difficulties, pancreatitis)
Nervous system (Peripheral neuropathy, fatigue)
Renal (interstitial nephritis)
Antibodies – Ro60 and La

challacombe scale
measures dry mouth
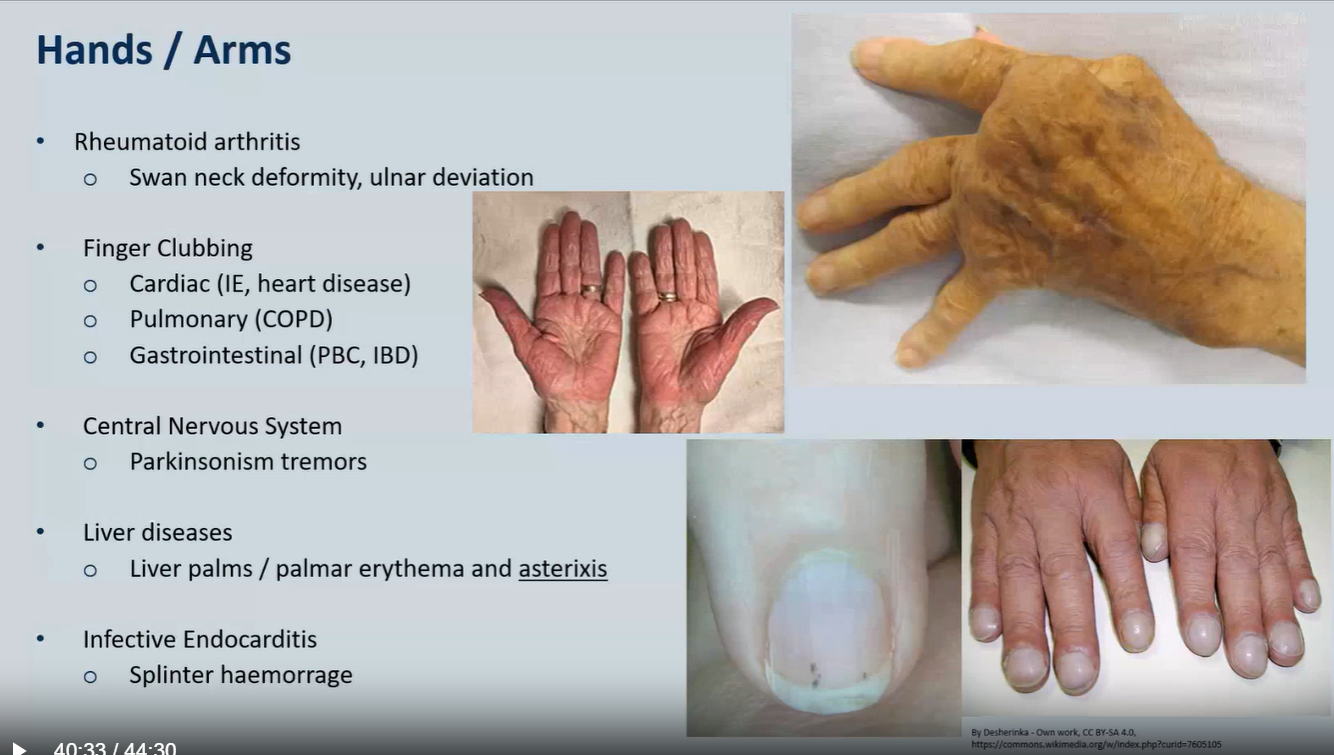
Hands / Arms
Rheumatoid arthritis
Swan neck deformity, ulnar deviation
Finger Clubbing
Cardiac (IE, heart disease)
Pulmonary (COPD)
Gastrointestinal (PBC, IBD)
Central Nervous System
Parkinsonism tremors
Liver diseases
Liver palms / palmar erythema and asterixis
Infective Endocarditis
Splinter haemorrage
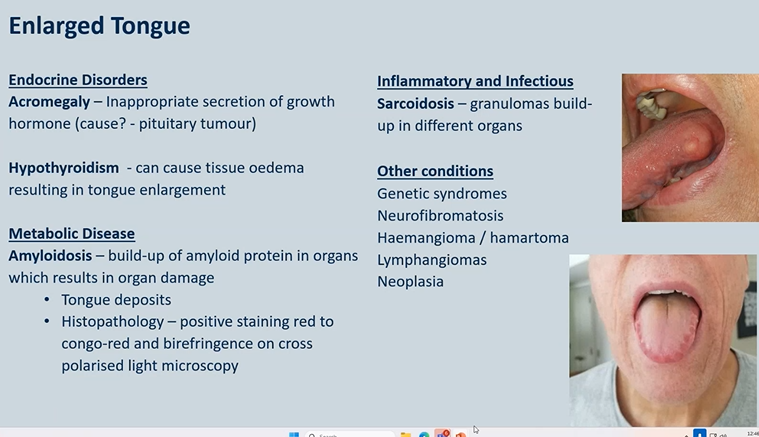
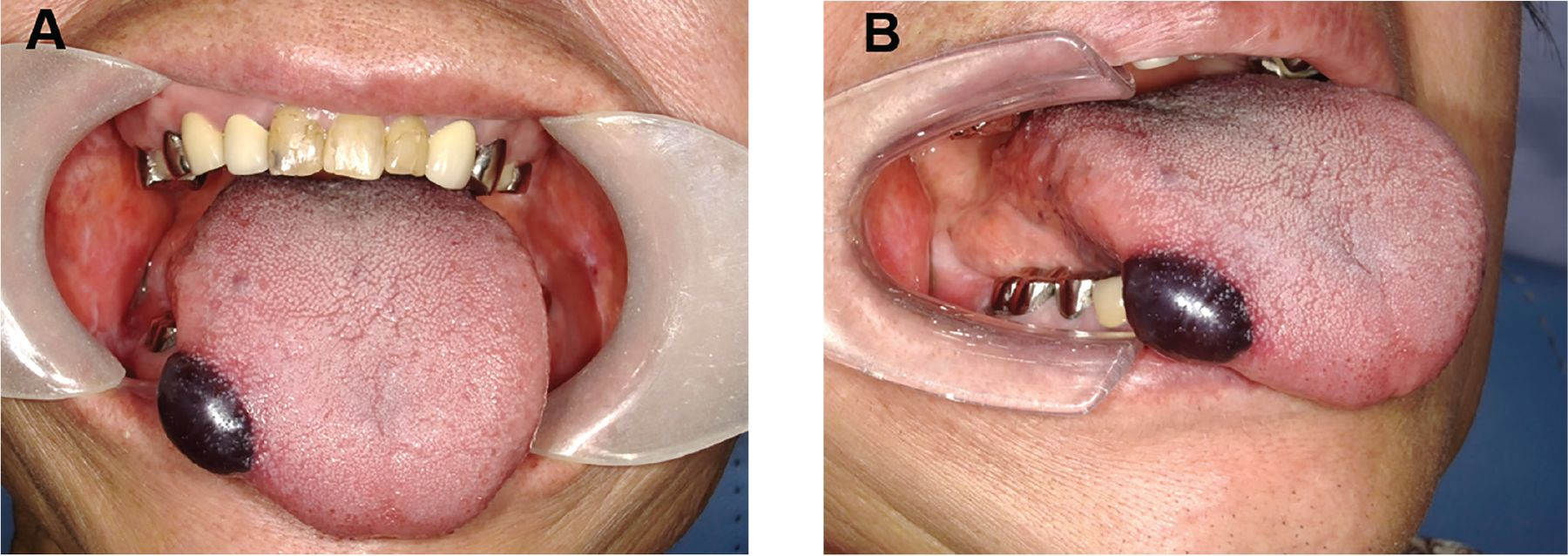
Enlarged Tongue - possible causes
Endocrine Disorders
Acromegaly – Inappropriate secretion of growth hormone (cause? - pituitary tumour)
Hypothyroidism - can cause tissue oedema resulting in tongue enlargement
Metabolic Disease
Amyloidosis – build-up of amyloid protein in
organs which results in organ damage
• Tongue deposits
• Histopathology – positive staining red to congo-red and birefringence on cross polarised light microscopy
Inflammatory and Infectious
Sarcoidosis – granulomas build-up in different organs
Other conditions
Genetic syndromes
Neurofibromatosis
Haemangioma / hamartoma
Lymphangiomas
Neoplasia
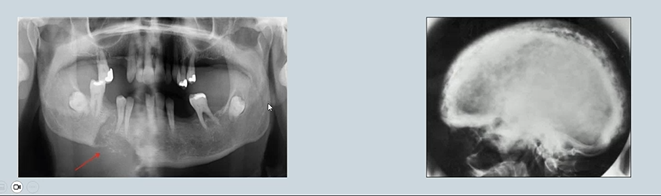
Bone changes as a result of systemic disease
Areas of resorption or patchy resorption and sclerosis in the jaws may be due to skeletal disease and associated with changes in blood chemistry.
Paget's disease →Results in excessive breakdown of bone and dysregulated remodelling.
Bony metastases - mental region in the mandible - radiolucency
Hyperparathyroidism